Lecture(4). Lecturer name: Dr. Sa`ad Y. Sulaiman
Chronic Sinusitis
Definition:
is defined as 8 weeks of persistent symptoms and signs of sinusitis that
does not respond to appropriate and aggressive medical therapy. In this case the long-
standing infection of the sinus will lead to irreversible change in the mucosa even
when the original cause of infection is removed.
The most commonly affected sinus
is the maxillary sinus because its osteum is
high and not gravity dependant.
Chronic Maxillary Sinusitis
Predisposing factors;
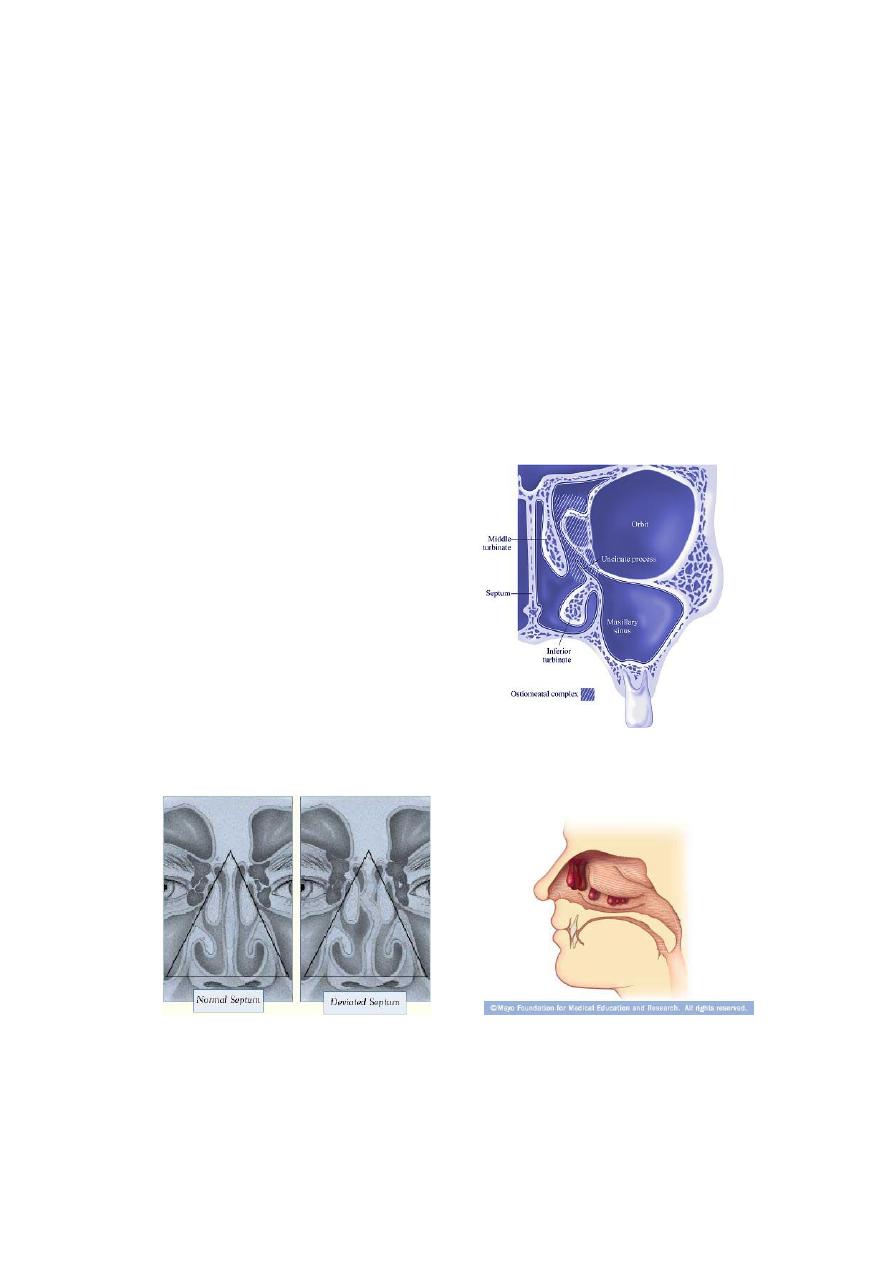
1) Nasal:
o Obstruction
of
the
drainage ostia due to
long-standing
blockage
(with
e.g.;
deviated
nasal
septum,
nasal
polyposis and enlarged
inferior turbinates).
o Recurrent acute
infection leads to
chronic state.
o Chronic irritation from
environmental gases.
,
th
5
.
(i.e
molar
nd
and 2
st
and the 1
upper 2nd premolar
) The
of cases
%
(10
2) Dental
illary antrum and may
impinge closely on the floor of the max
teeth)
upper
th
and 7
th
6
indeed penetrate it. Root infection or dental abscesses are commonly the cause of
unresolved maxillary sinus infections. The organism here are mainly anaerobes, and
2
the secretion is characteristically fetid . Healing of this form of sinusitis is impossible
without dental treatment.
Pathology:
chronic sinusitis can be divided pathologically into
:
1. Chronic hypertrophic sinusitis: there is hypertrophy of mucosa due to
increase vascular permeability.
2. Chronic atrophic sinusitis: (less common) there is generalized flattening of
the epithelium due to endarteritis obliterans of the arterioles.
Diagnosis:
Symptoms:
Major symptoms
Minor symptoms
Nasal discharge (copious greenish,
yellowish post nasal discharge)
Fever
Nasal obstruction (due to swelling
of inferior turbinate )
Halitosis (bad mouth odor )
Headache and facial pain
(due
to blockage of drainage ostea and
build up of secretion)
Anosmia( because air not reach the
olfactory region) and cacosmia (i.e.
unpleasant smell, due to chronic
odiferous sepsis).
In addition to the above symptoms, chronic irritation in side the nose may
produce; vestibulitis due to chronic use of handkerchief, nose bleeds, otitis
media due to oedema of eustachian tube , granular pharyngitis and chronic
laryngitis.
Signs:
Examination is often unhelpful, but we may see;
o Generalized inflammation of the mucosa.
o Purulent secretion or crusts.
o If a vasoconstrictor is used to shrink the nasal mucosa, pus may be seen
emanating from the middle meatus.
o Otitis media and granular pharyngitis may be present in the absence of any
specific nasal symptoms.
3
Investigation
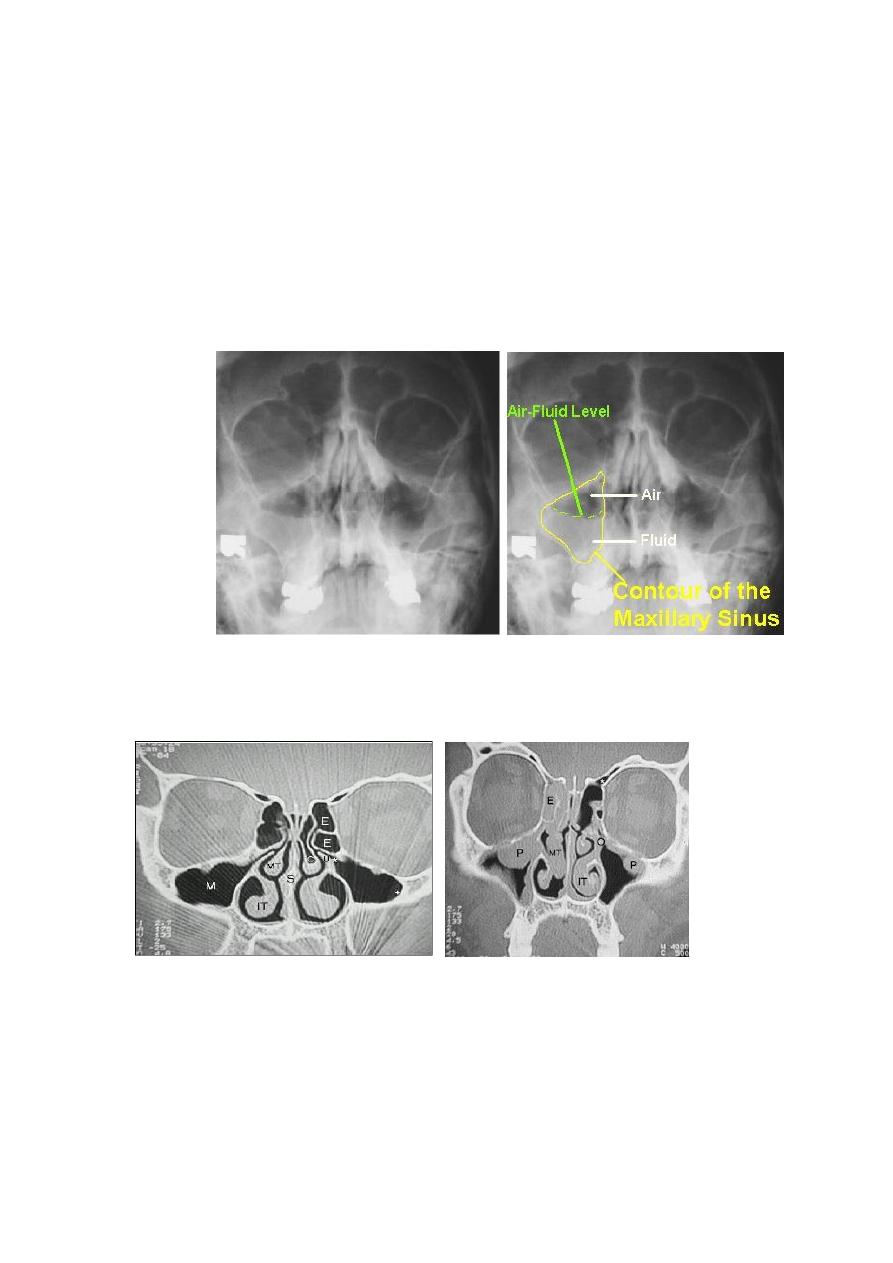
1)Radiography:
X-Ray of paranasal sinus
is helpful in
the
diagnosis
sinusitis
(mucosal
thickening, polyps and fluid level may
present).
2)
CT scan:
Coronal CT scan provide most information about the osteo-meatal
complex. Axial CT is indicated mainly for defining disease in the sphenoid or frontal
sinus.
Abnormal CT scan (P=polyp E=ethmoid
Normal CT scan MT= middle turbinate IT inferior
turbin
3) Endoscopic assessment
Endoscopic assessment has now become routine in the examination of the
nose and paranasal sinuses. There are several important features to be looked
for;
a) The presence of pus in the
middle meatus.
b)The cause of osteal obstruction
.
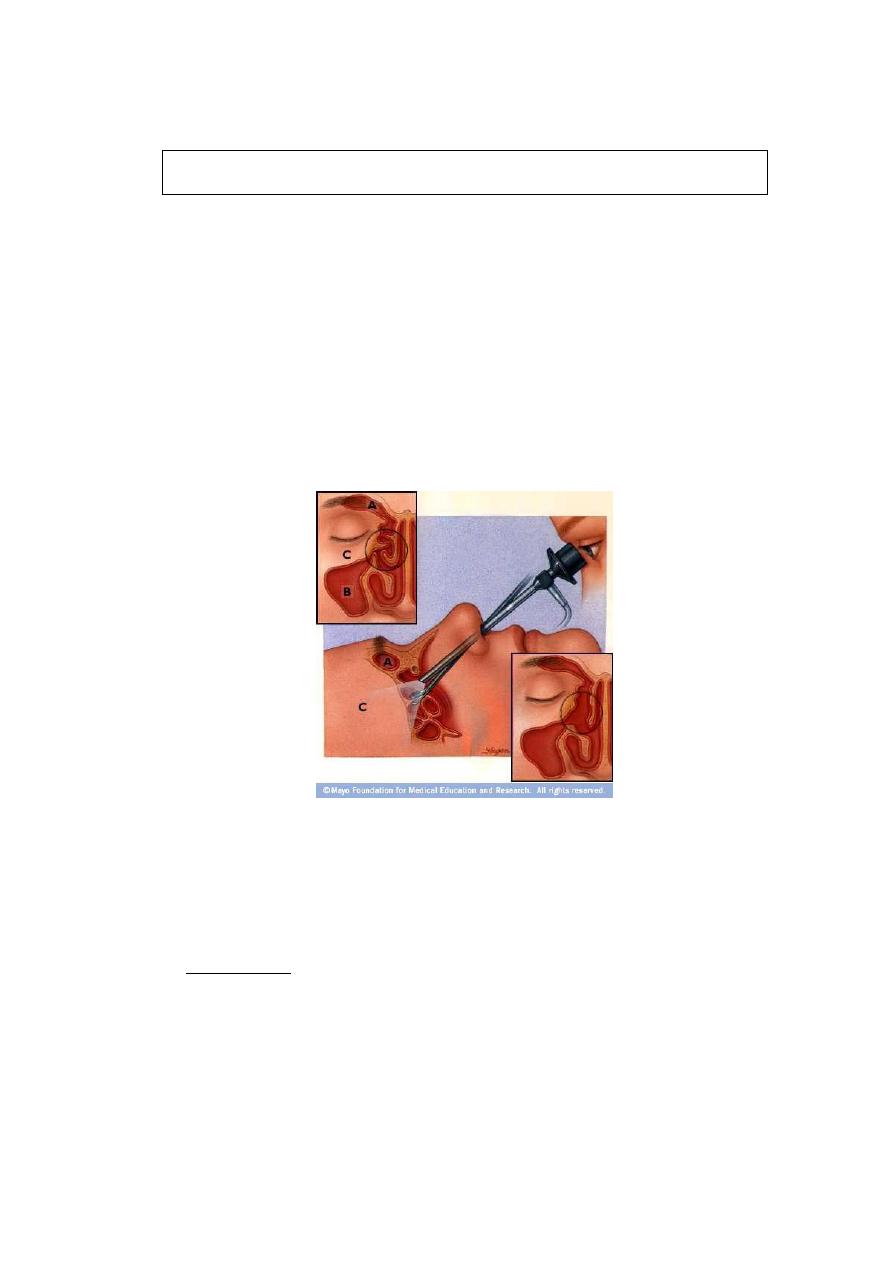
4
c) Sometimes biopsy is taken to confirm the diagnosis.
The key elements in the diagnosis are the history, the endoscopic assessment and the
findings on coronal CT.
Treatment:
The principle of treatment is to restore the normal mucosa to the sinus lining.
If this is not possible, i.e. when the mucosa has been irreversibly changed, then the
mucosa may need to be removed.
At the stage of chronic changes, medical treatment has been tried and is of no
value.
Surgical treatments of the chronic maxillary sinusitis include;
1) FESS (functional endoscopic sinus surgery ) is considered nowadays as the
procedure of choice for the treatment of chronic sinusitis. The basic
philosophy of FESS is to remove only the diseased areas in order to relieve
the obstruction and so restore natural sinus drainage, ventilation and
physiology.
2) Antral lavage.
3) Intranasal antrostomy.
4) Caldwell-Luc procedure.
Complication of chronic sinusitis;
Mucoceles:
Definition; A
mucocele
is a
mucous-containing cyst completely filling a sinus and
capable of expansion. They arise in order of frequency in the frontal, ethmoidal,
maxillary and sphenoidal.
Aetiology;
polyps, trauma, tumours and previous surgery particularly in the frontal
recess. Over 30 years can elapse between the traumatic event and the clinical
presentation of a mucocele.
5
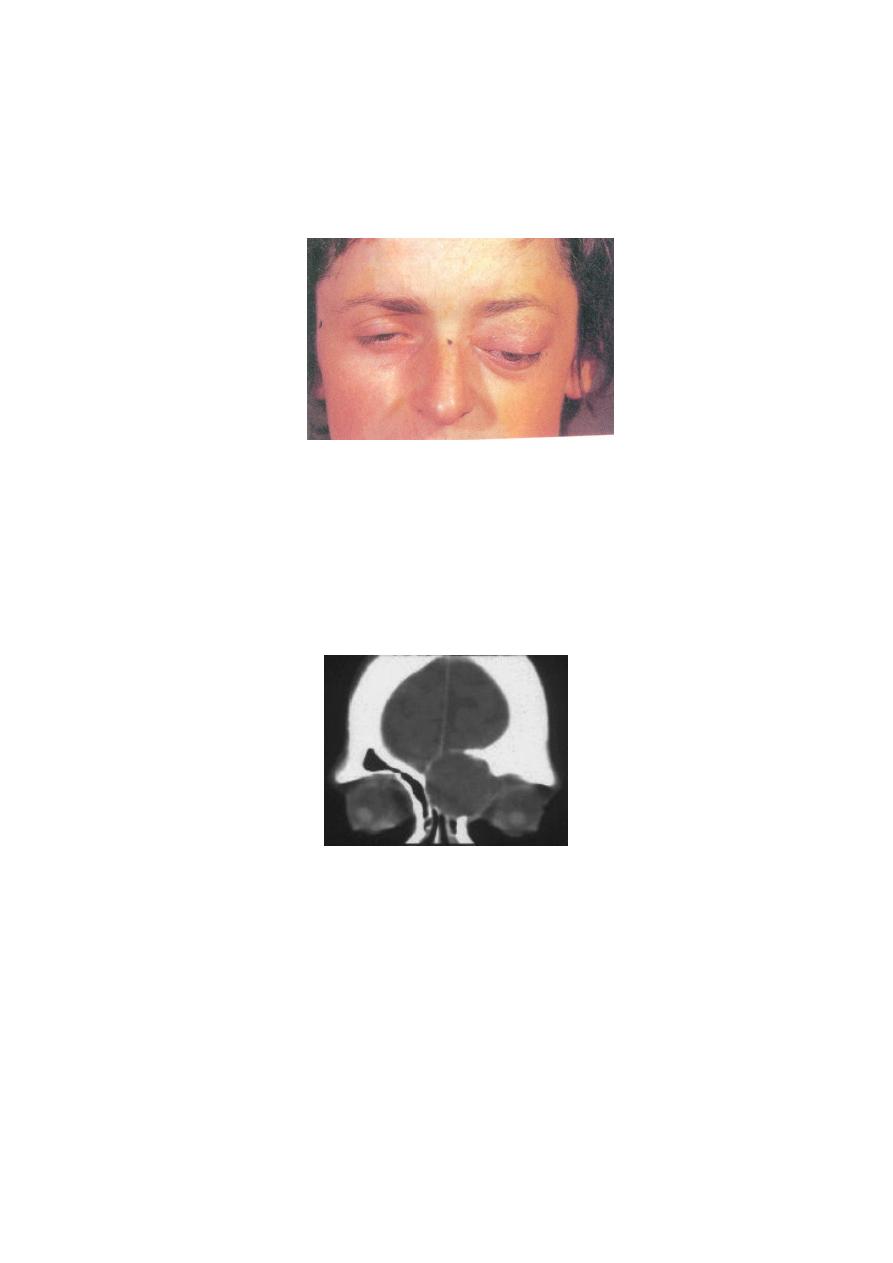
Frontoethmoidal mucocele
Clinical presentation
;
o In the early stages the patient is asymptomatic but, particularly in the frontal
type, a dull ache develops and a swelling appears at the supramedial aspect of
the orbit.
o The swelling is tender and feels rubbery, not as firm a consistency as bone.
o Increase in size thins the bone more and pressure may damage the optic nerve
or vasculature causing blindness.
o If infection supervenes it is called a pyocoele and has more sinister
consequences.
o With increase enlargement the eye may proptose.
Radiography of the sinus;
Thinning of the bone.
Displacement of the medial frontal sinus floor downwards.
Loss of scalloping of the superior border of the sinus.
The intersinus septum may be displaced or eroded.
CT scan is important in determining the anatomy and extent of the lesion.
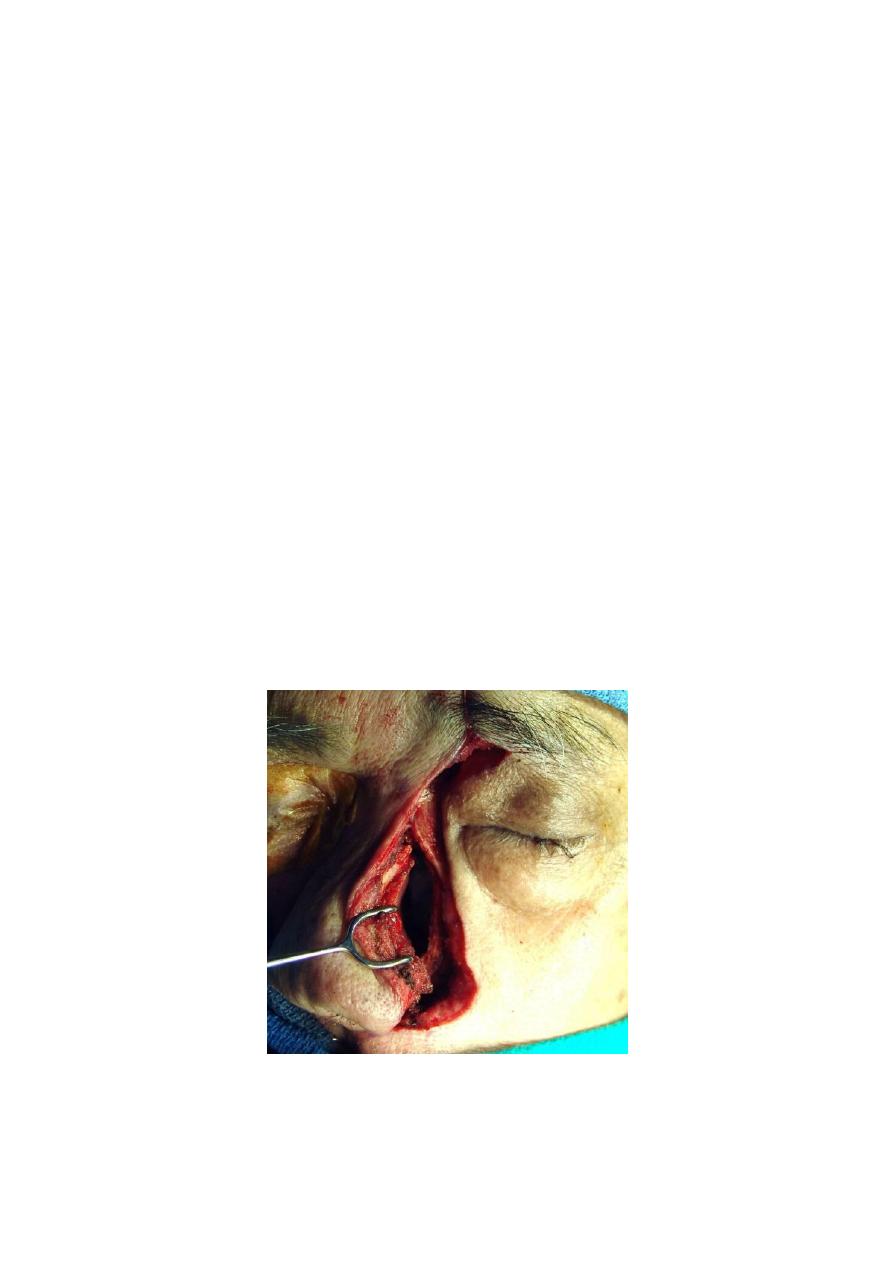
Treatment;
Is by evacuation of the contents of the sinus by ;
1) Endoscopic technique.
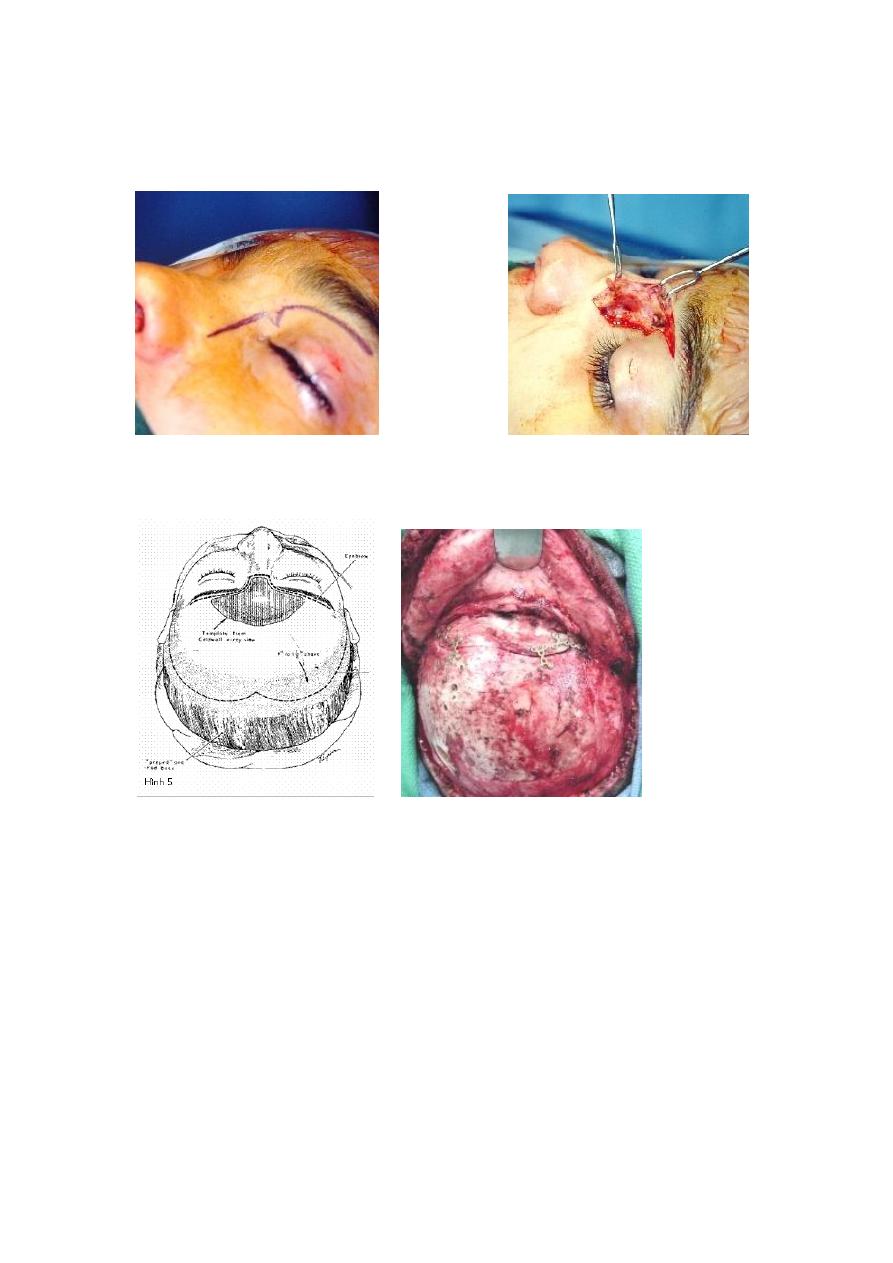
6
2) Radical frontal sinus operation.
3) Osteoplastic flap operation.
______________________________________________________
Tumors of the nose and paranasal sinuses
Tumors of the nose and paranasal sinuses can be subdivided into;
A.
Benign; e.g. Squamous papilloma (in the vestibule), osteoma (in frontal,
ethmoidal and maxillary sinus), Haemangiomas (on nasal septum) angiofibroma and
inverted papilloma.
B.
Malignant tumours (uncommon); Squamous carcinoma is the most common
followed by adenocarcinoma, malignant melanoma, ethesioneuroblastoma, sarcoma
and lymphoma. The maxillary sinus is the most common site for development of
malignancy.
*Malignant tumours, unlike most of the other head and neck cancers, do not usually
occur in heavy smoking or heavy drinking population. They may occasionally result
from exposure to environmental carcinogens (e.g. adenocarcinoma in woodworkers)
7
* The chief symptoms of nasal malignancy are unila teral obstruction with
haemorrhage (men > woman, average age at presentation is 60)
*Tumours of the skin of the nose are probably the most common of the facial cancer.
Inverted papilloma
(Transitional cell papilloma or Schneiderian papilloma)
;
This lesion represents about 4% of all nasal neoplasms. It is the most common
benign neoplasm of the nose and sinuses.
Aetiology; unknown.
Sex; Male-female ratio 5-1.
Age; most commonly in the 5
th
decade.
Site of origin; lateral wall of the nose (occasionally from the septum) with extension
to the ethmoid and maxillary sinus.
Clinical presentation; Unilateral nasal polyp → unilateral nasal obstruction and
sinusitis of all groups. The tumour is soft and friable and may become detached or
bleed with hard nose blowing.
X-Ray and CT scan of the sinuses; unilateral sinus opacity with bony erosion.
Histopathological examination; the surface of the tumour is covered by alternating
layers of Squamous and columnar epithelium, i.e. transitional type of epithelium.
The lesion is characterized by;
1) Being locally aggressive and causing bony erosion.
2) Tendency to undergo malignant change in about 2-5% of patient.
3) There may be coincidental malignancy elsewhere in the upper respiratory
tract.
4) It has high propensity for recurrence after removal.
Treatment; by adequate local excision usually through lateral rhinotomy approach.

8
Disorders of smell
The olfactory cleft occupies the upper third of the nasal cavity in the area between the
superior turbinate, cribriform plate and corresponding area of the septum and is lined
by
specialized
olfactory
epithelium
(this
is
a
specialized
pseudostratified
neuroepithelium containing the primary olfactory receptors and has a golden yellow
color).
Terminology;
Anosmia; Inability to detect odors.
Hyposmia; Decreased ability to detect odors.
Parosmia; Altered perception of smell in the presence of an odor.
Phantosmia; Smelling of nonexistent odor.
(Both parosmia and phantosmia are associated with epilepsy and olfactory
hallucination of schizophrenia).
Cacosmia; Unpleasant smell, due to chronic odiferous sepsis.
Classification of olfactory dysfunction:
1. Conductive anosmia; is due to impaired transport of airborne
odorants to the olfactory cleft.
2. Neuronal anosmia; is due to impairment of olfactory epithelial
function or disrupted neuronal pathway.
Causes of olfactory dysfunction;
1. Obstructive nasal disease (23%): Include nasal polyposis, mucosal disease,
tumours and nasal deformity.
2. Postviral anosmia (19%): Due to viral injury to olfactory epithelium and more
common in those above age of 40.Hyposmia is more common than frank
anosmia. About one third recover some function over 3-6 months. No specific
treatment
3. Head trauma (15%): Due to shearing force on olfactory filaments, olfactory
bulb contusion or frontal lobe injury.
4. Toxins, drugs (3%): Aminoglycosides, formaldehyde, alcohol, nicotine,
organic solvents and direct application of zinc salts.
5. Miscellaneous (21%): Aging, neoplastic, psychologic, nutritional deficiencies
(e.g. vitamin A, thiamine) and other causes.
6. Idiopathic (21%).
……………………………………………………………………………..

9
