Chronic kidney disease (chronic renal failure)TUCOMInternal Medicine 4th classDr. Hasan I. Sultan
Chronic kidney disease (CKD); refers to an irreversible, progerssive deterioration in renal function which classically develops over a period of years, end in loss of the excretory, metabolic and endocrine functions of the kidney leads to the clinical symptoms and signs of renal failure, which are referred to as uraemia.
When death is likely without renal replacement therapy, it is called end-stage renal disease/failure (ESRD or ESRF).
The incidence of CKD is much higher in some countries due to differences in regional and racial incidences of disease, as well as differences in medical practice.
Chronic Kidney Disease (CKD)
Classification of Chronic Kidney Disease
StageDescription
GFR, (mL/1.73 m2/min)
1
Kidney damage with normal or increased GFR
≥90
2
Kidney damage with mildly decreased GFR
60-89
3
Moderately decreased GFR
30-59
4
Severely decreased GFR
15-29
5
Kidney failure
<15 or dialysis
GFR= glomerular filtration rate, It is proportionate to body size and the normal reference range is usually expressed after correction for body surface area as 120 +/- 25 mL/1.73 m2/min.
Common causes of end-stage renal failure
Disease
Proportion
Comments
Congenital and inherited
5%
E.g. polycystic kidney disease, Alport's syndrome
Renal artery stenosis
5%
Hypertension
5-20%
Glomerular diseases
10-20%
IgA nephropathy is most common
Interstitial diseases
20-30%
Systemic inflammatory diseases
5-10%
e.g. SLE, vasculitis
Diabetes mellitus
20-40%
Large racial and geographical differences
Unknown
5-20%
Clinical features
Chronic kidney disease may present as a raised blood urea and creatinine found during routine examination, often accompanied by hypertension, proteinuria or anaemia.
The great majority of patients with slowly progressive disease are asymptomatic until GFR falls below 30 mL/min/1.73 m2 (stage 4 or 5).
Nocturia, due to the loss of concentrating ability and increased osmotic load per nephron, can be an early symptom. Oliguria occur in the late stages of CKD.
Thereafter, symptoms and signs may develop in almost every body system as described in the next slides, with including tiredness or breathlessness.
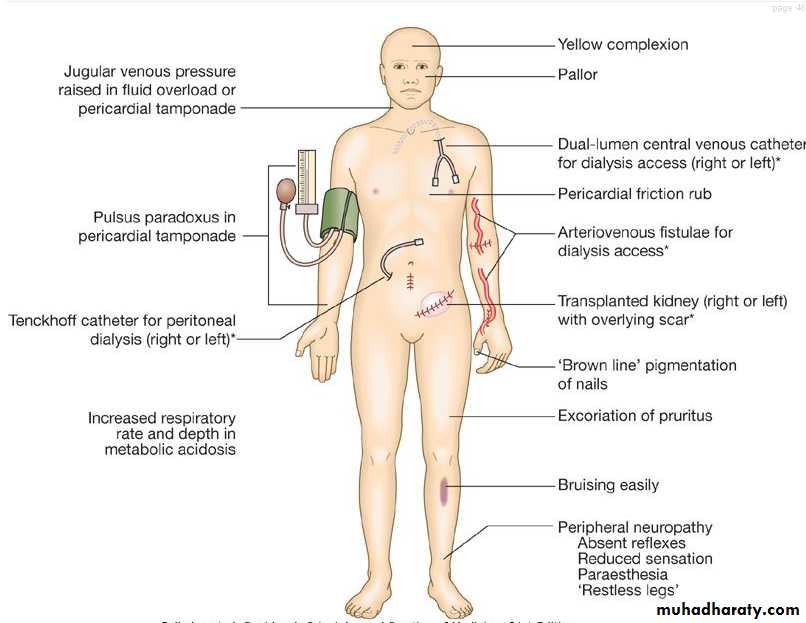
In ESRD (stage 5) there may be pruritus, anorexia, nausea and vomiting. Later, hiccups, unusually deep respiration related to metabolic acidosis (Kussmaul's respiration), muscular twitching, fits, drowsiness and coma ensue.
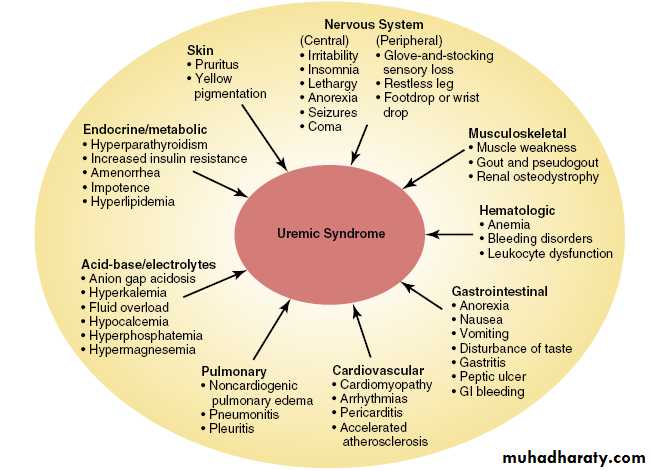
Signs and Symptoms of Uremia
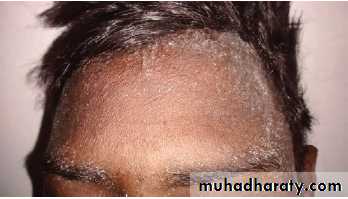
1- Skin; Pruritus. Pigment alteration (pallor due anemia. Yellowish color, due to retained urochromes and carotene. Brownish hyperpigmentation is common mostly in a sun-exposed distribution, these gives the earthy colour face). Dryness of the skin. Half-and-half nails (The distal part of fingernails become brownish in color). Uremic frost (increase evaporation of urea through sweat glands results in the deposition of urea crystals on the skin). Alopecia.2- Gastrointestinal; are among the earliest and most common signs of the uremia. Metallic taste, loss of appetite, anorexia, nausea, vomiting, and weight loss. Severe uremia may also experience stomatitis, enteritis or GI bleeding.
3- Cardiovascular; Hypertension, left ventricular hypertrophy and congestive heart failure. Accelerated atherosclerosis and IHD. Metastatic calcification in the myocardium, cardiac valves, and arteries. Arrhythmias, and sudden cardiac death. Pericarditis, pericardial tamponade or constrictive pericarditis.
4- Pulmonary; pulmonary edema. Pneumonitis. Pleuritis. Pleural effusion.
5- Neurologic; Central nervous system (CNS); Impaired cognitive function and memory. Disturbances of sleep. Encephalopathy; Lethargy, irritability, asterixis, seizures, and later on coma. Peripheral nervous system; progressive symmetrical sensory neuropathy in a glove-and-stocking distribution. Decreased distal tendon reflexes and loss of vibratory perception. Restless legs, foot drop, or wrist drop.
6- Muscle; Generalised myopathy may occur due to a combination of poor nutrition, hyperparathyroidism, vitamin D deficiency and disorders of electrolyte metabolism. Gout and pseudogout.
7- Endocrine/metabolic; Hyperparathyroidism. Increased insulin resistance. Amenorrhea. Impotence. Hyperlipidemia.
8- Acid- base/electrolyte; Metabolic acidosis (Kussmaul’s breathing). Hyperkalemia. Fluid overload. Hypocalcemia. Hyperphosphatemia. Hypermagnesemia.
9- Immune dysfunction; Cellular and humoral immunity is impaired in advanced CKD. Which is the second most common cause of death in dialysis patients, after cardiovascular disease.
10- Haematological; There is an increased bleeding tendency in advanced CKD, which manifests as cutaneous ecchymoses and mucosal bleeds, due to platelet dysfunction or coagulopathy. Causes of anaemia in chronic kidney disease are:
• Deficiency of erythropoietin
• Toxic effects of uraemia on marrow precursor cells
• Reduced red cell survival
• Increased blood loss due to capillary fragility and poor platelet function
• Reduced intake, absorption and utilisation of dietary iron
11- Metabolic bone disease; Disturbances of calcium and phosphate metabolism are almost universal in advanced CKD, and various types of metabolic bone disease may also occur, including osteitis fibrosa cystica, osteomalacia and osteoporosis.
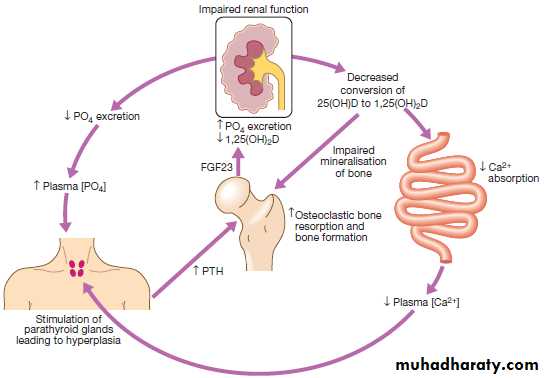
There is impaired conversion of 25-hydroxyvitamin D to its active metabolite, 1,25-dihydroxyvitamin D, thereby causing hypocalcaemia, and increased PTH production by the parathyroid glands and hyperphosphataemia develops.
In some cases, tertiary hyperparathyroidism supervenes, due to autonomous production of PTH by the enlarged parathyroid glands; this presents with hypercalcaemia.
Pathogenesis of renal osteodystrophy. Low 1,25(OH)2D levels cause hypocalcaemia, which increases PTH production by the parathyroid glands. The raised level of PTH increases osteoclastic bone resorption and bone formation. Although production of FGF23 from osteocytes also increases, promoting phosphate excretion, this is insufficient to prevent hyperphosphataemia in advanced CKD.
The major manifestations of uremia
Earthy colour face
Half-and-half nail
Uremic frostInvestigations
Their main aims are:to identify the underlying cause where possible, since this may influence the treatment
to identify reversible factors that may worsen renal function, such as hypertension, urinary tract obstruction, nephrotoxic drugs, and salt and water depletion
to screen for complications of CKD, such as anaemia and renal osteodystrophy
to screen for cardiovascular risk factors.
Suggested investigations in chronic kidney disease
Urea and creatinin; to assess stability/progression of CKDUrinalysis and quantification of proteinuria; indicates risk of progressive CKD requiring preventive ACE inhibitor or ARB therapy
Electrolytes; hyperkalaemia and acidosis
Calcium, phosphate, parathyroid hormone; renal osteodystrophy
Albumin; Low albumin: consider malnutrition
Full blood count (± Fe, ferritin, folate, B12); as renal causes of anaemia
Lipids, glucose ± HbA1c; Cardiovascular risk factors
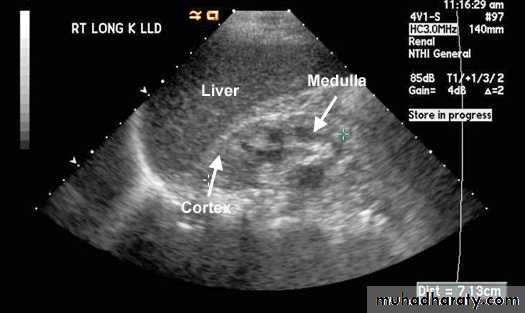
• Renal ultrasound; to exclude obstruction, progressive CKD, Small kidneys suggest chronicity. Normal size kidneys suggest (APKD, diabetic nephropathy, hydronephrosis or amyledosis). Asymmetric renal size suggests renovascular or developmental disease.
• Hepatitis and HIV serology; If dialysis or transplant is planned. Hepatitis B vaccination recommended if seronegative
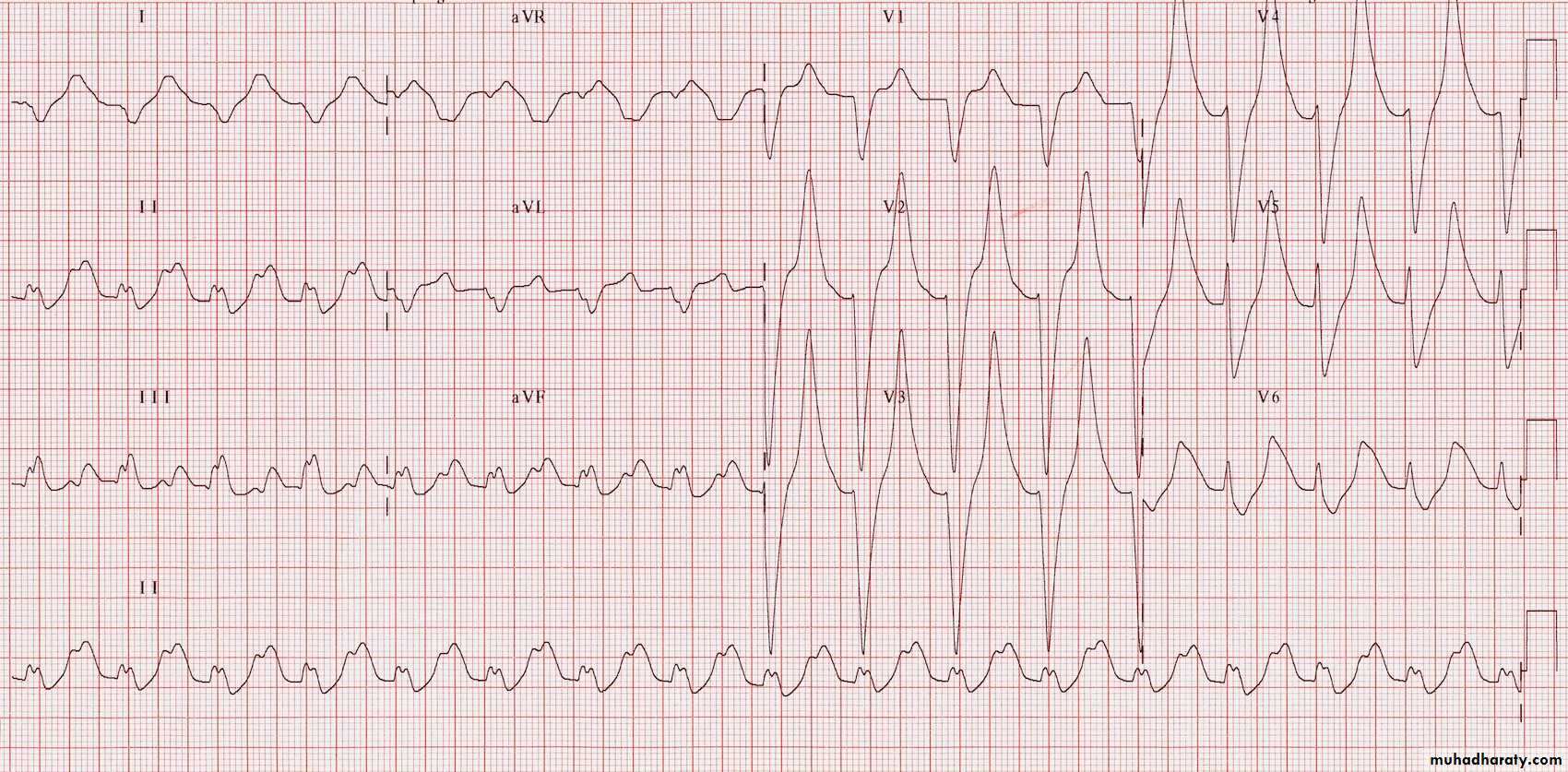
ECG; hyperkalaemic, or there are risk factors for cardiac disease
Hyperkalaemia ECG findings; Prolonged PR interval. Broad and bizarre QRS complexes. Peaked T waves.
Normal Kidney; Normal kidney measures between 10.5 to 12.5 cms. Cortex is about 2.5 cms and has the same kind of echoes as liver. Medulla is hypoechoic and appears dark.
Chronic Renal Failure; Kidneys are smaller than normal. Surface may be irregular. Cortex is thinned and is hyperechoic than liver due to scar tissue. Medulla is hypoechoic and appears dark.
Management of Chronic Kidney Disease
Management goals include• Prevention of progression of CKD
• Identifying and treating symptoms and complications of CKD
• Preparing patients for renal replacement therapy (RRT).
PREVENTION OF PROGRESSION:
Include optimal control of hypertension, diabetes, and other cardiovascular disease risk factors (i.e. tobacco cessation), use of medications that block the RAAS pathway, diet modifications, avoidance of nephrotoxins, and addressing potentially reversible causes of acute kidney injury in the setting of CKD.
1- Dietary and lifestyle interventions;
The recommended dietary protein intake in advanced CKD (stage 4 or 5) is 0.60 g/kg per day and, if this is not accepted or tolerated, can be increased to 0.75 g/kg per day, with at least 50% of the protein being of high biologic value. Severe protein restriction is not recommended. Restriction of sodium, potassium and phosphorus are recommended. stop smoking, improve exercise and weight loss have beneficial effects on cardiovascular risk profile.
2- Antihypertensive therapy;
Angiotensin-converting enzyme inhibitors and angiotensin II receptor blockers reduce proteinuria and slow the progression of CKD in hypertensive patients to a greater extent than can be explained by the reduction in blood pressure alone. and has additional benefits in lowering risk of hypertensive heart failure, stroke and peripheral vascular disease.
3- Reduction of proteinuria;
ACE inhibitors and ARBs inhibit the angiotensin-induced vasoconstriction of the efferent arterioles of the glomerular microcirculation. This inhibition leads to a reduction in both intraglomerular filtration pressure and proteinuria in diabetic and nondiabetic renal failure.4- Maintaining fluid and electrolyte balance;
fluid retention; dietary sodium intake limited to about 100 mmol/day, but often loop diuretics may also be required to treat fluid overload.
Hyperkalaemia; reduce or stop potassium-sparing diuretics, ACE inhibitors and ARBs. Correction of acidosis, limiting potassium intake and use of potassium-binding resins, such as calcium resonium.
5- Treatment of diabetes mellitus;
It is recommended that fasting plasma glucose be kept in the 5.0–7.2 mmol/L (90–130 mg/dL) and hemoglobin A1C should be < 7%.Some antidiabetic drugs should be avoided with with progressive renal impairment;
Chlorpropamide may be associated with prolonged hypoglycemia
Metformin may cause lactic acidosis
Thiazolidinediones (e.g., rosiglitazone, pioglitazone, and others), may increase renal salt and water absorption and aggravate volume-overloaded states.
Finally, as renal function declines, renal degradation of administered insulin will also decline, so that less insulin may be required for glycemic control.
6- Lipid-lowering therapy;
Hypercholesterolaemia is almost universal in patients with significant proteinuria. There is some evidence that control of dyslipidaemia with statins may slow the rate of progression of renal disease.7- Renal bone disease;
Treatment should be initiated with active vitamin D metabolites (either 1-α-hydroxyvitamin D or 1,25- dihydroxyvitamin D) in patients who are found to have hypocalcaemia. Hyperphosphataemia should be treated by dietary restriction of foods with high phosphate content (milk, cheese, eggs and protein-rich foods) and by the use of phosphate-binding drugs, like calcium carbonate or aluminium hydroxide.
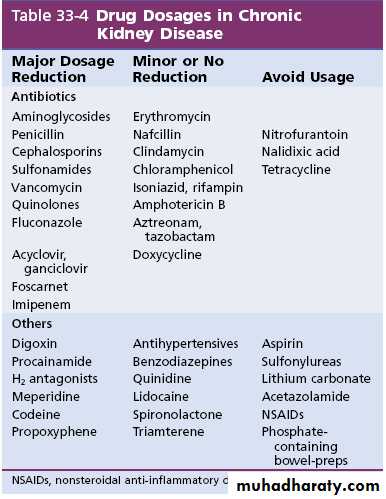
8- Avoiding Toxic Drug Effects;
Many drugs that are excreted by the kidney should be avoided, or their doses should be reduced, in patients with renal insufficiency, as shown in the table below.
9- Avoidance and treatment of reversible factors of acute kidney injury in the setting of CKD. These factors are;
Decreased renal perfusion: Intravascular volume depletion, Heart failure
Obstruction
Infection
Nephrotoxins
Endogenous: myoglobulin, hemoglobin, uric acid, calcium, phosphorus
Exogenous: contrast media, drugs
Poorly controlled hypertension: malignant or accelerated hypertension
9- Treatment of anaemia;
Recombinant human erythropoietin (EPO), Eprex; is effective in correcting the anaemia of CKD.EPO side effects; Hypertension and thrombosis (including thrombosis of the AV fistulae used for haemodialysis).
The target haemoglobin is usually between 100 and 120 g/L (10–12 g/dL).
EPO is less effective in the presence of iron deficiency, active inflammation or malignancy, and in patients with aluminium overload, which may occur in dialysis.
Iron supplementation is usually essential to ensure an adequate response to EPO.
Treatment of End-Stage Renal Disease Renal Replacement Therapy
A plan for a modality of RRT should be discussed with the patient early in the course of kidney failure and before the appearance of uremic symptoms.
The two primary treatments for ESRD are dialysis and transplantation.
There are two types of dialysis, hemodialysis and peritoneal dialysis.
Kidney transplants may be from either deceased or living donors.
In medically eligible patients, kidney transplantation is encouraged because it allows a better quality of life, increased survival rate, and greater chance for rehabilitation.
Indications for dialysis in patients with CKD include the following:
• Severe metabolic acidosis• Hyperkalemia
• Pericarditis
• Encephalopathy such as confusion, asterixis, or seizures
• Fluid overload or pulmonary edema refractory to diuretics
• Malnutrition
• Intractable gastrointestinal symptoms
• Bleeding diathesis attributable to uremia
• The GFR is 15 mL per minute or less and there are no apparent reversible causes of kidney failure.
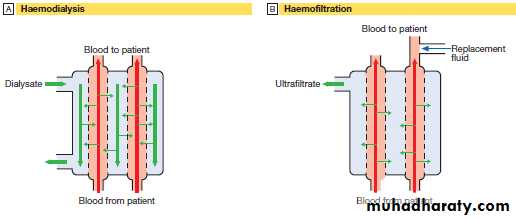
Hemodialysis (HD)
In CKD, vascular access for HD is gained by formation of an arteriovenous fistula, usually in the forearm, up to a year before dialysis is contemplated. After 4–6 weeks, increased pressure transmitted from the artery to the vein leading from the fistula causes distension and thickening of the vessel wall (arterialisation). Large-bore needles can then be inserted into the vein to provide access for each HD treatment.HD is usually carried out for 3–5 hours three times weekly. Efficient HD achieve reduction in urea during dialysis (urea reduction ratio) of over 65%, improvement of symptoms and better fluid and electrolytes balance.
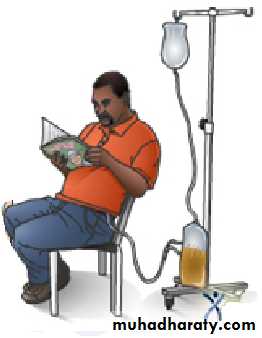
Haemodialysis. A patient receiving haemodialysis through a forearm subcutaneous (Brescia–Cimino) fistula.
A In haemodialysis, there is diffusion of solutes from blood to dialysate across a semipermeable membrane allowing exchange of small molecules across the concentration gradient by diffusion. B In haemofiltration, both water and solutes are filtered across a porous semipermeable membrane by a pressure gradient, allowing removing excess fluid. Replacement fluid is added to the filtered blood before it is returned to the patient.
A
B
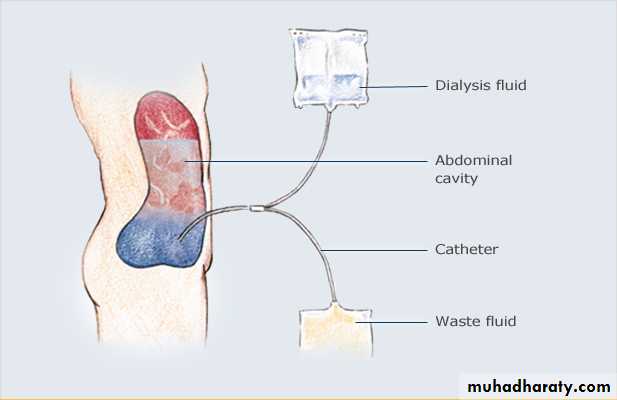
Peritoneal dialysis
The peritoneum acts as a semipermeable membrane similar to a hemodialysis filter. This technique has several advantages because it allows independence from the long time spent in dialysis units, it does not require stringent dietary restrictions as in hemodialysis, and rehabilitation rates are better than those observed in hemodialysis, with more patients returning to full-time employment.In continuous ambulatory peritoneal dialysis, dialysate fluid of 2.0- to 3.0-L volumes is instilled in the peritoneal cavity for varying amounts of time, to be exchanged four to six times daily. In continuous cyclic peritoneal dialysis, the patient is connected to a machine referred to as a cycler that allows inflow of smaller volumes of dialysate with shorter dwell time through the night.
In peritoneal dialysis, fluid is introduced into the abdominal cavity using a catheter. Solutes diffuse from blood across the peritoneal membrane to PD fluid down a concentration gradient and water diffuses through osmosis
Renal transplantation
offers the best chance of long-term survival and complete rehabilitation, and is the most cost-effective treatment in patients with ESRD. It can restore normal kidney function and correct all the metabolic abnormalities of CKD. All patients should be considered for transplantation unless there are active contraindications:Absolute contraindica.
Active malignancy
Active vasculitis or recent anti-GBM disease
Severe heart disease
Severe occlusive aorto-iliac vascular disease
Relative contraindication
Age: very young children (< 1 yr) or older people (> 75 yrs)
High risk of disease recurrence in the transplant kidney
Disease of the lower urinary tractan ileal conduit may be considered
Significant comorbidity
Kidney grafts may be taken from a cadaver in the UK after brain death (51%) or circulatory death (11%), or from a living donor (38%).