Parasitic Infestationsof the Skin
ScabiesHuman scabies is a highly contagious disease caused by the mite Sarcoptes scabiei var. hominis which is an obligate parasite to humans.
Scabies is not primarily a sexually transmitted disease but sexual transmission does occur.
Scabies spreads in households and neighborhoods in which there is a high frequency of intimate personal contact or sharing of inanimate objects.
Dogs and cats may be infested by almost identical organisms; these sometimes may be a source for human infestation.
Scabies is endemic in many developing countries and is usually associated with overcrowding, low socioeconomic standards, and poor hygiene.
ANATOMIC FEATURES
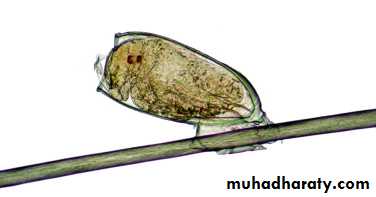
The adult mite is ⅓-mm long and has a flattened, oval body with wrinklelike, transverse corrugations and eight legs.
The digestive tract fills a major portion of the body.
Infestation and life cycle
Infestation begins when a fertilized female mite arrives on the skin surface.Within an hour, the female excavates a burrow in the stratum corneum.
During the mite’s 30-day life cycle, the burrow extends from several mms to few cms in length.
The burrow does not enter the underlying epidermis except in the case of hyperkeratotic Norwegian scabies.
Eggs are laid at the rate of 2-3 a day and fecal pellets (scybala) are deposited in the burrow.
Scybala are dark, oval masses that are seen easily when burrow scrapings are examined under a microscope.
Scybala may act as an irritant and may be responsible for some of the itching.
The larvae hatch, leaving the egg casings in the burrow, and reach maturity in 2-3 weeks.
Immunology
A hypersensitivity reaction rather than a foreign
body response may be responsible for the
lesions.
Clinical manifestations
The disease begins insidiously.Symptoms are minor at first?
Scratching destroys burrows (and other primary lesions) and removes mites, providing initial relief.
Scratching also spreads mites to other areas and after 6 to 8 weeks the once localized area of minor irritation has become a widespread, intensely pruritic eruption.
Lesions are pleomorphic and tend to remain discrete and small.
Lesions of scabies
PRIMARY LESIONSBurrow
VesiclesPapules
Mites are found in burrows and at the edge of vesicles but rarely in papules.
SECONDARY LESIONS
Pinpoint erosionsPustules
Eczematous changes
Nodules
Symptoms and signs of scabies
Rash present for 4 to 8 weeks has suddenly become
worse.
Generalized, severe itching
Nocturnal itching
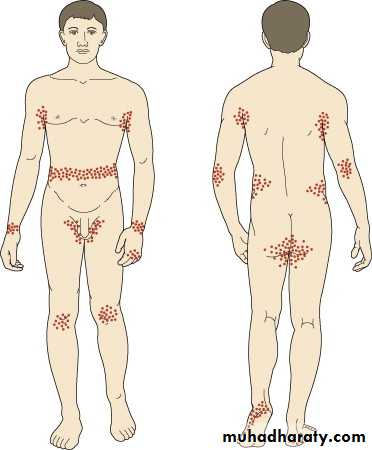
Pinpoint erosions and crusts on the buttocks
Vesicles in the finger webs
Diffuse eruption sparing the face
Nodules on the penis and scrotum
Patient becomes better, then worse, after treatment
with topical steroids.
Rash is present in several members of the same
family.
• Distribution
Scabies in infants
Widespread involvement usually due to misdiagnosis and Rx.Sometimes the face and scalp are affected.
Vesicles are common on the palms and soles (characteristic).
Secondary eczematization and impetiginization are common.
Burrows are difficult to find.
Nodules may be seen in the axillae and diaper area.
Scabies in the elderly
The decreased immunity associated with advanced age may allow the mites to multiply and survive in great numbers.Therefore, few cutaneous lesions (other than excoriations, dry skin, and scaling) are present.
Eventually papules and nodules appear and may become numerous.
Itching is intense.
Treatment and management
Permethrin (cream)Is the drug of choice for the treatment of scabies in children and adults of all ages including pregnant and lactating women.
Two applications 1 week apart, apply from head/neck to toe and wash after 8-12 hours (for permethrin and lindane).
Lindane (cream, shampoo, and lotion)
Is a central nervous system stimulant that produces seizures and death in the scabies mite.It accumulates in fat and binds to brain tissue, therefore excessive use can be dangerous.
No pre-bathing in lindane.
BENZYL BENZOATE
The 25% lotion is the most common preparation.Application is just like sulfur
CROTAMITON
Once-a-day application for 2 to 5 days.It has antipruritic properties.
SULFUR
The pharmacist mixes 5% to 10% precipitated sulfur in petrolatum.
The compound is applied to the entire body below the neck once each day for 3 days and the patient is instructed to bathe 24 hours after each application.
These preparations are messy, have an unpleasant odor, stain, and cause dryness.
Sulfur in petrolatum is thought to be safe for infants <2 months old and pregnant and nursing women.
Ivermectin
Indications?Dose: 200µg/kg, two doses, 2 weeks apart.
Cure rate=95%
MANAGEMENT OF COMPLICATIONS
ECZEMATOUS INFLAMMATIONPYODERMA
POST-SCABIETIC PRURITUS
Pruritus may persist for weeks after treatment (may be due to
hypersensitivity response to remaining dead mites and mite
products).
NODULAR SCABIES
ENVIRONMENTAL MANAGEMENT
Intimate contacts and all family members in the same household should be treated.
Mites can live in dust , chairs, and bed linens for several days.
Wash all clothing, towels, and bed linen (in a normal washing machine cycle) that have touched the skin.
Pediculosis
Lice are obligate human parasites that cannot survive off their host.Three kinds of lice infest humans:
Pediculus humanus var. capitis (head louse)Pediculus humanus var. corporis (body louse)
Phthirus pubis (pubic or crab louse)
Lice feed approximately five times each day by piercing the skin with their claws, injecting irritating saliva, and sucking blood that makes them rust colored (characteristic).
Lice feces appear on the skin as small, rust-colored flecks.
Saliva and fecal material can induce a hypersensitivity reaction and inflammation.
Lice are active and can travel quickly, which explains why they can be transmitted so easily.
The life cycle from egg to egg is approximately 1 month.
Transmission is by close personal contact and contact with objects such as combs, hats, clothing, and bed linen.
Nits
The female lays approximately six eggs, or nits, each day for up to 1 month, and then dies.
Nits are 0.8 mm long and are firmly cemented to the bases of hair shafts close to the skin to acquire adequate heat for incubation.
Nits are very difficult to remove from the hair shafts.
Clinical manifestations of Pediculosis capitis
Lice infestation of the scalp is most common in children.More girls than boys are afflicted.
Commonly seen on the back of the head and neck and behind the ears.
The average patient carries less than 20 adult lice.
Scratching causes inflammation and secondary bacterial infection, with pustules, crusting, and cervical lymphadenopathy.
Posterior cervical adenopathy without obvious disease is characteristic of lice.
Sensitization to the lice toxin, feces, or body parts lasts for 3 - 8 months and is a cause of pruritus.
Eyelashes may be involved, causing blepharitis.
Head lice can survive away from the human host for about 3 days, and nits can survive for up to 10 days.
Transmission is by direct contact and also by fomite transmission.
Head lice do not carry any human disease.
Diagnosis
Scalp will be apparent to those who carefully examine individual hairs.
Finding nits does not indicate active infestation and may persist for months after successful treatment
Combing the hair with a fine-toothed comb.
Lice and nits can be seen easily under a microscope.
Nits fluoresce and can be detected easily by Wood’s light examination. Nits that contain an unborn louse fluoresce white. Nits that are empty fluoresce gray.
Treatmant
Permethrin (1% and 5%) is the most effective treatment. It paralyzes the nerves that allow the lice to breathe.Remains active for 2 weeks.
Only apply to dry hair.
It is insecticidal and ovicidal.
Two applications (10 min. each) one week apart.
Permethrin has a clinical efficacy of 95%.
Lindane and pyrethrin have cure rates less than 90%.
Malathion
Malathion is rapidly pediculicidal and ovicidal and is useful for lice resistant to pyrethrins and permethrin.
It binds to hair and has residual activity.
A 1% shampoo is applied to the scalp and washed out 10 minutes later and repeated in 1 week.
It is not recommended for infants and neonates.
Other measures
IvermectinCo-trimoxazole (480mg twice daily for 3 days), and repeated after 1 week.
Shaving the head
Nit removal (Combing)
Fomite control
Eye infestation: Baby shampoo or Vaseline; Ivermectin.
Cutaneous Leishmaniasis
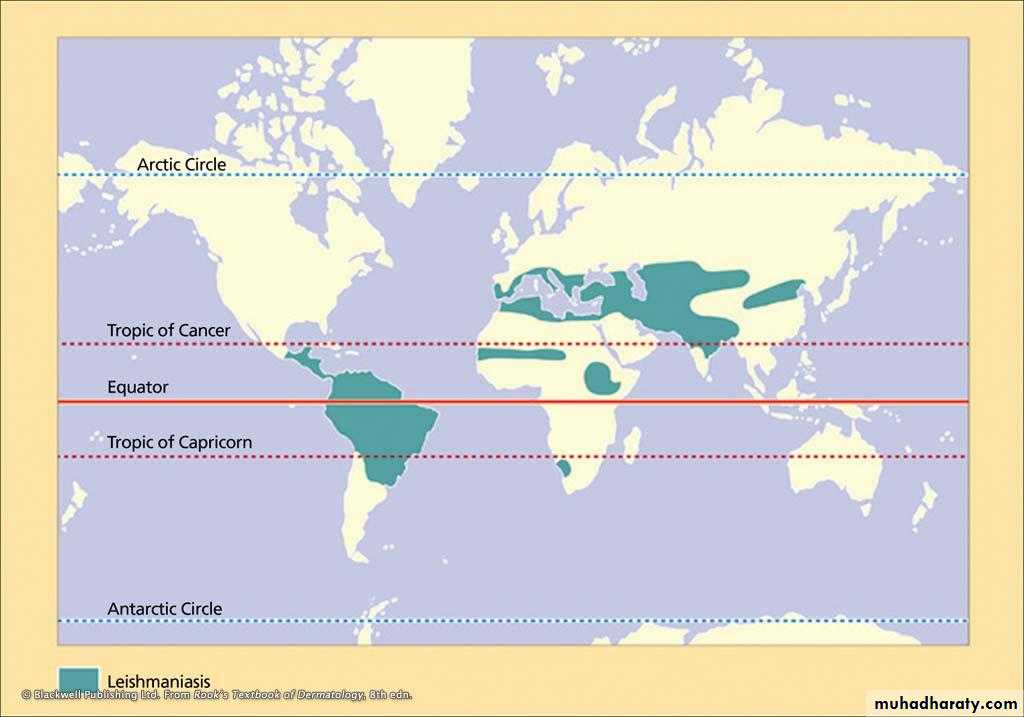
The leishmaniases are a group of diseases caused by several species of the genus Leishmania.Each species tends to occupy a particular zoogeographical zone and the disease is endemic in 88 countries.
It has been estimated that 1.5 million new cases of cutaneous leishmaniasis occur annually and >80% of the total of cases are in developing countries.
Brazil, Iran, Syria, Iraq, Afghanistan and Sudan suffer the highest prevalence.
Leishmania spp. undergo a cycle of development in the gut of female sandflies, of the genera Phlebotomus in the Old World.
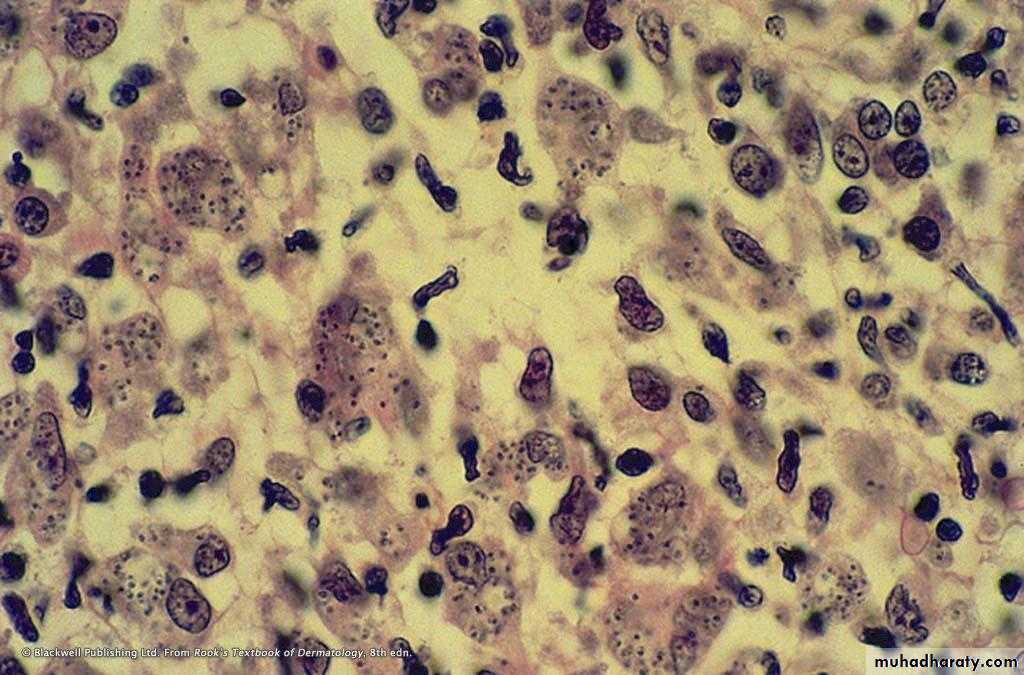
In its vertebrate host (Dogs, Gerbils, Humans), the amastigote form of the parasite is found in cells of the reticuloendothelial system or in the dermis following infection.
It is round or oval, 2–3 µm in diameter, with no protruding flagellum.
While in the sandfly and in culture media, Leishmania spp. are the elongated promastigote stage, motile with an anterior flagellum.
Old World cutaneous leishmaniasis
SynonymsOriental sore
Delhi boil
Baghdada boil
Aleppo boil
Cutaneous leishmaniasis of the Old World is due to L. major, L. tropica,
L. aethiopica and L. donovani infantum.
Pathogenesis
Sandflies inoculate the infective promastigotes when taking a blood meal into the dermis, then promastigotes are taken up by histiocytes, in which they multiply.Only a minority of parasite inoculations result in localized or disseminated cutaneous leishmaniasis.
After a period of time, the overlying epidermis becomes hyperkeratotic and breaks down, causing an ulcer covered with a crust.
Clinical features
The incubation period is usually measured in months, but ranges from a few days to over a year.
One or more lesions occur on unclothed body parts, particularly the face, neck and arms.
The natural history of the lesions caused by the four spp. is different but there is much overlap and the sequence of nodule, crusting, ulceration and healing with scar formation is common to all.
Diagnosis
History of travel (or living) to an endemic area in the previous weeks or months.
History of insect (sandfly) bites in the previous weeks or months.
History of high-risk activities such as sleeping outdoors.
Non-healing chronic nodular, violaceous ulcer/nodule for 4–6 weeks or longer.
Demonstration of amastigotes in Giemsa-stained smears from infected skin by direct microscopy.
Demonstration of intracellular amastigotes in the dermis of H & E skin sections.
Growth of promastigotes in Nicolle–Novy–MacNeal (NNN) culture medium from lesional specimens
Demonstration of leishmanial DNA by PCR.
Treatment
Try topical treatment methods for simple sores.Reserve the systemic use of pentavalent antimonials for problematic sores: these include:
• Sores where scarring would be disabling or severely disfiguring.
• Sores that will not heal easily (on shin or over a joint).
• Sores involving mucosa or cartilage.
Weekly intralesional sodium stibogluconate PLUS daily oral itraconazole 100 mg (or allopurinol) for 6 to 8 weeks.
IM sodium stibogluconate in a single daily dose of 20 mg/kg for 15–21 days.
Severe scarring may require plastic repair.
After healing, patients are normally immune to reinfection with the same species.