DIAGNOSIS OF TB
Dr.Redha 2013Specimens required
Pulmonary• Sputum* (induced with nebulized hypertonic saline if not expectorating)
• Bronchoscopy with washings or BAL
• Gastric washing* (mainly used for children)
Extrapulmonary
• Fluid examination (cerebrospinal, ascitic, pleural,
pericardial, joint): yield classically very low
• Tissue biopsy (from affected site); also bone marrow/liver
may be diagnostic in patients with disseminated disease
Diagnostic tests
• Circumstantial (ESR, CRP, anaemia etc.)• Tuberculin skin test (low sensitivity/specificity; useful only in
primary or deep- seated infection)
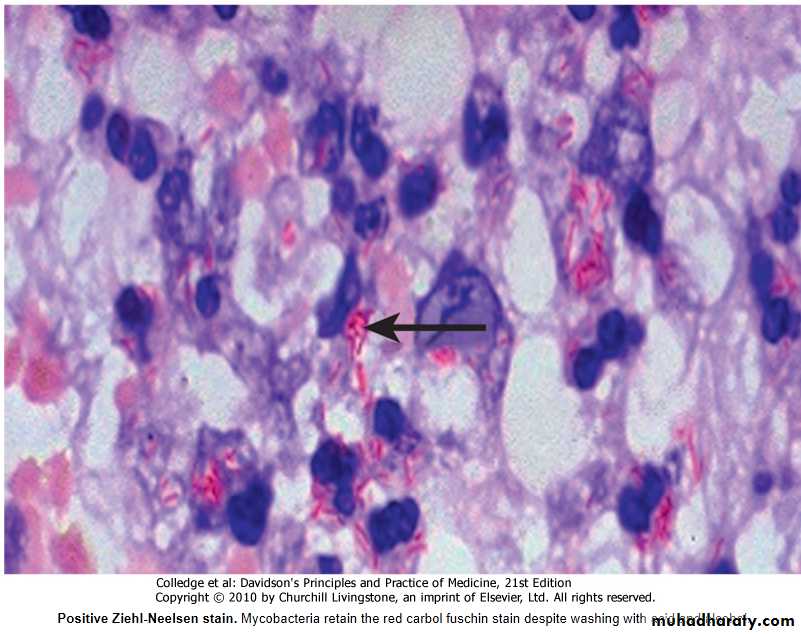
• Stain
o Ziehl-Neelsen
o Auramine fluorescence
• Nucleic acid amplification
• Culture
o Solid media (Löwenstein-Jensen, Middlebrook)
o Liquid media (e.g. BACTEC or MGIT)
• Response to empirical antituberculous drugs (usually seen after 5-10 days)
• The presence of an otherwise unexplained cough for more than 2-3 weeks, particularly in an area where TB is highly prevalent, or typical chest X-ray changes should prompt further investigation Box above).
• Direct microscopy of sputum is the most important first step.
• The probability of detecting acid-fast bacilli is proportional to the bacillary burden in the sputum (typically positive when 5000-10 000 organisms are present).
• By virtue of their substantial lipid-rich wall, tuberculous bacilli are difficult to stain.
• The most effective techniques are the Ziehl-Neelsen and rhodamine-auramine (Fig.) stains.
• The latter causes the tuberculous bacilli to fluoresce against a dark background and is easier to use when numerous specimens need to be examined; however, it is more complex and expensive, limiting applicability in resource-poor regions.
•
• A positive smear is sufficient for the presumptive diagnosis of TB but definitive diagnosis requires culture.
• Smear-negative sputum should also be cultured, as only 10-100 viable organisms are required for sputum to be culture-positive.
• A diagnosis of smear-negative TB may be made in advance of culture if the chest X-ray appearances are typical of TB and there is no response to a broad-spectrum antibiotic.
• MTB grows slowly and may take between 4 and 6 weeks to appear on solid medium such as Löwenstein-Jensen or Middlebrook.
• Faster growth (1-3 weeks) occurs in liquid media such as the radioactive BACTEC system or the non-radiometric mycobacteria growth indicator tube (MGIT).
• The BACTEC method is commonly used in developed nations and detects mycobacterial growth by measuring the liberation of 14CO2, following metabolism of 14C-labelled substrate present in the medium.
• New strategies for the rapid confirmation of TB at low cost are being developed; these include the nucleic acid amplification test (NAT), designed to amplify nucleic acid regions specific to MTB such as IS6110, and the MPB64 skin patch test, in which immunogenic antigen detects active but not latent TB, and has the potential to provide a simple, non-invasive test which does not require a laboratory or highly skilled personnel.
• Drug sensitivity testing is particularly important .
• If a cluster of cases suggests a common source, confirmation may be sought by fingerprinting of isolates with restriction-fragment length polymorphism (RFLP) or DNA amplification.
• The diagnosis of extrapulmonary TB can be more challenging.
• There are generally fewer organisms (particularly in meningeal or pleural fluid), so culture or histopathological examination of tissue is more important.
• In the presence of HIV, however, examination of sputum may still be useful, as subclinical pulmonary disease is common.
Management
Chemotherapy
• A variety of highly effective short-course regimens are available; choice depends on local health resources and infrastructure (Box 19.61).
• They are based on the principle of an initial intensive phase (which rapidly reduces the bacterial population), followed by a continuation phase to destroy any remaining bacteria.
• Treatment should be commenced immediately in any patient who is smear-positive, or who is smear-negative but with typical chest X-ray changes and no response to standard antibiotics.
• Quadruple therapy has become standard in the UK, although ethambutol may be omitted under certain circumstances.
• Fixed-dose tablets combining two or three drugs are generally favoured: for example, Rifater (rifampicin, isoniazid and pyrazinamide) daily for 2 months, followed by 4 months of Rifinah (rifampicin and isoniazid).
• Streptomycin is an important component of short-course treatment regimens in developing nations.
Treatment of TB (World Health Organization recommendations)
1New cases of smear-positive pulmonary TB
2 months H3R3Z3E3 or 2 months H3R3Z3S3
4 months H3R3
Severe extrapulmonary TB
2 months HRZE or 2 months HRZS4 months HR
Severe smear-negative pulmonary TB
6 months HE†
Severe concomitant HIV disease
2§Previously treated smear-positive pulmonary TB
2 months H3R3Z3E3 or 1 month H3R3Z3E
5 months H3R3E3
Relapse
2 months HRZES or 1 month HRZE5 months HRE
Treatment failure
Treatment after default3‡
New cases of smear-negative pulmonary TB2 months H3R3Z3E3
4 months H3R3
Less severe extrapulmonary TB
2 months HRZE
4 months HR
6 months HE†
• Six months of therapy is appropriate for all patients with new-onset, uncomplicated pulmonary disease.• However, 9-12 months of therapy should be considered if the patient is HIV-positive, or if drug intolerance occurs and a second-line agent is substituted.
• Meningitis should be treated for a minimum of 12 months.
• Pyridoxine should be prescribed in pregnant women and malnourished patients to reduce the risk of peripheral neuropathy with isoniazid.
• Where drug resistance is not anticipated, patients can be assumed to be non-infectious after 2 weeks of appropriate therapy.
• Most patients can be treated at home.
• Admission to a hospital unit with appropriate isolation facilities should be considered where there is :
• uncertainty about the diagnosis,
• intolerance of medication,
• questionable compliance,
• adverse social conditions or
• a significant risk of multidrug-resistant TB (MDR-TB: culture-positive after 2 months on treatment, or contact with known MDR-TB).
• In choosing a suitable drug regimen, underlying comorbidity (renal and hepatic dysfunction, eye disease, peripheral neuropathy and HIV status), as well as the potential for drug interactions, must be considered.
• Baseline liver function and regular monitoring are important for patients treated with standard therapy including rifampicin, isoniazid and pyrazinamide, as all of these agents are potentially hepatotoxic.
• Mild asymptomatic increases in transaminases are common but serious liver damage is rare.
• Ethambutol should be used with caution in patients with renal failure, with appropriate dose reduction and monitoring of drug levels.
• Adverse drug reactions occur in about 10% of patients, but are significantly more common in the presence of HIV co-infection (Box Below).
Corticosteroids : reduce inflammation and limit tissue damage, and are currently recommended when treating :
• Pericardial
• Meningeal disease
• Children with endobronchial disease.
• TB of the ureter
• Pleural effusions and
• Extensive pulmonary disease, and
• Can suppress hypersensitivity drug reactions.
Surgery :
• Is still occasionally required (e.g. for massive haemoptysis, loculated empyema, constrictive pericarditis, lymph node suppuration, spinal disease with cord compression), but usually only after a full course of antituberculosis treatment.• The effectiveness of therapy for pulmonary TB may be judged by a further sputum smear at 2 months and at 5 months.
• A positive sputum smear at 5 months defines treatment failure.
• Extrapulmonary TB must be assessed clinically or radiographically as appropriate.
Main adverse reactions of first-line antituberculous drugs
IsoniazidRifampicin
Pyrazinamide
Streptomycin
Ethambutol
Mode of action
Cell wall synthesis
DNA transcription
Unknown
Protein synthesis
Cell wall synthesis
Major adverse reactions
Peripheral neuropathy1Hepatitis2Rash
Febrile reactionsHepatitisRashGastrointestinal disturbance
HepatitisGastrointestinal disturbanceHyperuricaemia
8th nerve damageRash
Retrobulbar neuritis3Arthralgia
Less common adverse reactions
Lupoid reactionsSeizuresPsychoses
Interstitial nephritisThrombocytopeniaHaemolytic anaemia
RashPhotosensitisationGout
NephrotoxicityAgranulocytosis
Peripheral neuropathyRash
1The risk of peripheral neuropathy may be reduced by prescribing pyridoxine.2Hepatitis is more common in patients with a slow acetylator status and in alcoholics.3Reduced visual acuity and colour vision may be reported with higher doses and are usually reversible.
Control and prevention
• The WHO is committed to reducing the incidence of TB by 2015.
• Important components of this goal include supporting the development of laboratory and health-care services to improve detection and treatment of active and latent TB.
Detection of latent TB
• Contact tracing is a legal requirement in many countries.
• It has the potential to identify the probable index case, other cases infected by the same index patient (with or without evidence of disease), and close contacts who should receive BCG vaccination (see below) or chemotherapy.
• Approximately 10-20% of close contacts of patients with smear-positive pulmonary TB and 2-5% of those with smear-negative, culture-positive disease have evidence of TB infection.
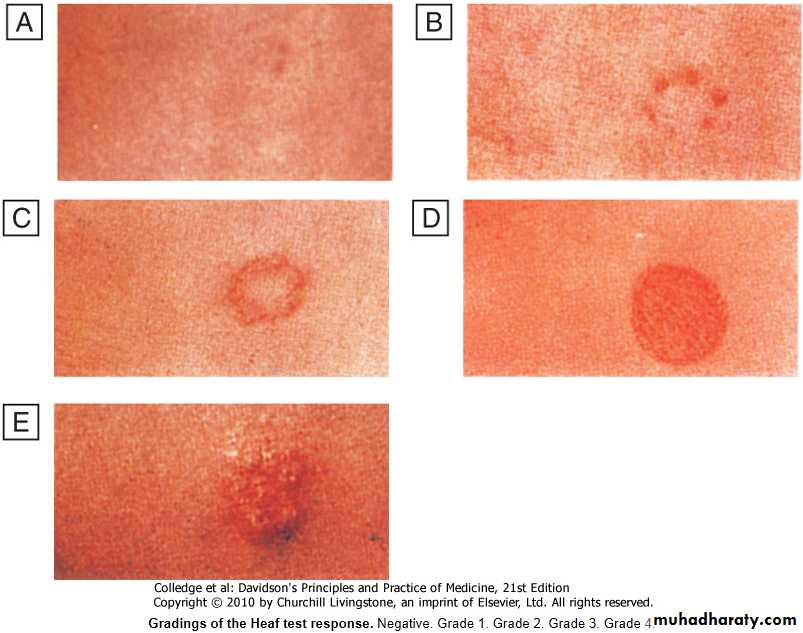
• Cases are commonly identified using the tuberculin skin test (Box and Fig.).
Heaf testRead at 3-7 days
• Multipuncture method
o Grade 1: 4-6 papules
o Grade 2: Confluent papules forming ring
o Grade 3: Central induration
o Grade 4: > 10 mm induration
Mantoux test
Read at 2-4 days
• Using 10 tuberculin units
o Positive when induration 5-14 mm (equivalent to Heaf grade 2) and > 15 mm (Heaf grade
3-4)
False negatives
• Severe TB (25% of cases negative)
• Newborn and elderly
• HIV (if CD4 count < 200 cells/mL)
• Malnutrition
• Recent infection (e.g. measles) or immunization
• Immunosuppressive drugs
• Malignancy
• Sarcoidosis
• An otherwise asymptomatic contact with a positive tuberculin skin test but a normal chest X-ray may be treated with chemoprophylaxis to prevent infection progressing to clinical disease.
• Chemoprophylaxis is also recommended for children aged less than 16 years identified during contact tracing to have a strongly positive tuberculin test, children aged less than 2 years in close contact with smear-positive pulmonary disease, those in whom recent tuberculin conversion has been confirmed, and babies of mothers with pulmonary TB.
• It should also be considered for HIV-infected close contacts of a patient with smear-positive disease.
• Rifampicin plus isoniazid for 3 months or isoniazid for 6 months is effective.
Gradings of the Heaf test response.
• Negative.• Grade 1.
• Grade 2.
• Grade 3.
• Grade 4.
• Tuberculin skin testing may be associated with false-positive reactions in those who have had :
• A BCG vaccination and
• In areas where exposure to non-tuberculous mycobacteria is high.
• These limitations may be overcome by employing interferon-gamma release assays (IGRAs).
• These tests measure the release of IFN-γ from sensitised T cells in response to antigens such as early secreted antigenic target (ESAT)-6 or culture filtrate protein (CFP)-10 that are encoded by genes specific to the MTB and are not shared with BCG or opportunistic mycobacteria.
• The greater specificity of these tests, combined with the logistical convenience of one blood test, as opposed to two visits for skin testing, suggests that IGRAs will replace the tuberculin skin test in low-incidence, high-income countries.
Directly observed therapy (DOT)
• Poor adherence to therapy is a major factor in prolonged infectious illness, risk of relapse and the emergence of drug resistance.
• DOT involves the supervised administration of therapy thrice weekly and improves adherence.
• It has become an important control strategy in resource-poor nations.
• In the UK, it is currently only recommended for patients thought unlikely to be adherent to therapy: those who are homeless, alcohol or drug users, drifters, those with serious mental illness and those with a history of non-compliance.
TB and HIV/AIDS
• The close links between HIV and TB, particularly in sub-Saharan Africa, and the potential for both diseases to overwhelm health-care funding in resource-poor nations have been recognised with the promotion of programmes that link detection and treatment of TB with detection and treatment of HIV.
• It is recommended that all patients with TB should be counselled and tested for HIV disease.
• Mortality is high and TB is a leading cause of death in HIV patients.
Drug-resistant TB
• Drug-resistant TB is defined by the presence of resistance to any first-line agent. Multidrug-resistant (MDR) TB is defined by resistance to at least rifampicin and isoniazid, with or without other drug resistance.• Extensively drug-resistant (XDR) TB is defined by resistance to at least rifampicin and isoniazid, in addition to any quinolone and at least one injectable second-line agent.
• The prevalence of MDR-TB is rising, particularly in the former Soviet Union, Central Asia and Africa.
• It is more common in those with a prior history of TB, particularly if treatment has been inadequate, and those with HIV infection (Box 19.64).
• Diagnosis is challenging, especially in developing countries, and although cure may be possible, it requires prolonged treatment with less effective, more toxic and more expensive therapies.
• Mortality rate from MDR-TB is high and that from XDR-TB higher still.
Factors contributing to emergence of drug-resistant TB
• Drug shortages• Poor-quality drugs
• Lack of appropriate supervision
• Transmission of drug-resistant strains
• Prior anti-tuberculosis treatment
• Treatment failure (smear-positive at 5 months)
Vaccines
• BCG (the Calmette-Guérin bacillus), a live attenuated vaccine derived from M. bovis, is the most established TB vaccine.
• It is administered by intradermal injection and is highly immunogenic. BCG appears to be effective in preventing disseminated disease, including tuberculous meningitis, in children, but its efficacy in adults is inconsistent and new vaccines are urgently needed.
• Current vaccination policies vary world-wide according to incidence and health-care resources, but usually target children and other high-risk individuals.
• BCG is very safe with the occasional complication of local abscess formation.
• It should not be administered to those who are immunocompromised (e.g. by HIV) or pregnant.
Prognosis
• Following successful completion of chemotherapy, cure should be anticipated in the majority of patients.• There is a small (< 5%) and unavoidable risk of relapse, which usually occurs within 5 months and has the same drug susceptibility.
• In the absence of treatment, a patient with smear-positive TB will remain infectious for an average of 2 years; in 1 year, 25% of untreated cases will die.
• Death is more likely in those who are smear-positive and those who smoke.
• A few patients die unexpectedly soon after commencing therapy and it is possible that some have subclinical hypoadrenalism that is unmasked by a rifampicin-induced increase in steroid metabolism.
• HIV-positive patients have higher mortality rates and a modestly increased risk of relapse.