The Pancreas
Assistant Professor Aqeel Shakir MahmoodFRCS – London
Consultant General and Laparoscopic SurgeonPan-creas!
Greek:“pan” = all;
“creas” = flesh
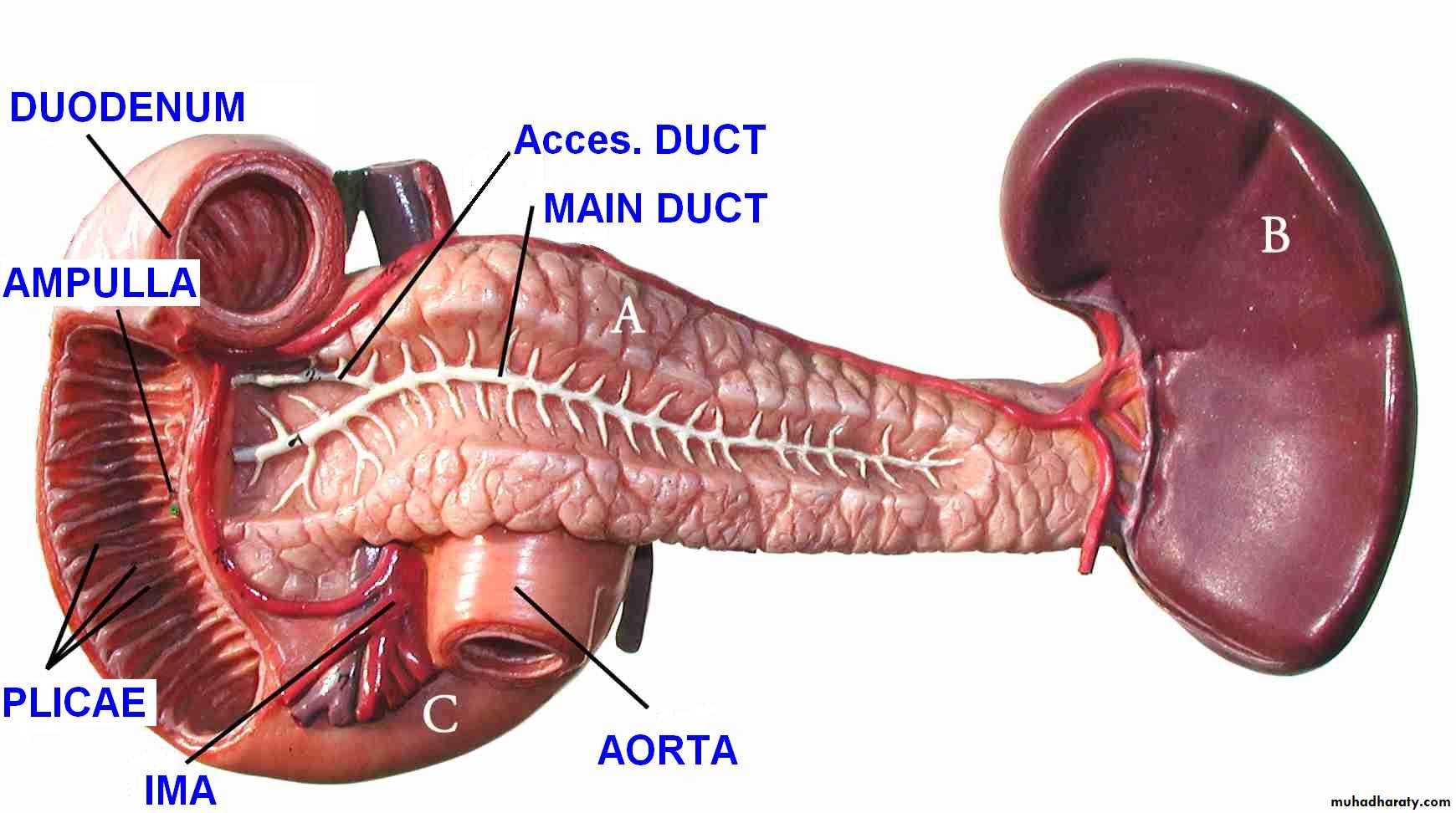
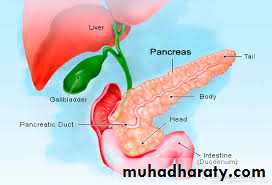
Pancreas is like a fish! Head, body, and tail.
Important anatomical relationships
The Pancreas
pancreas anatomy
Made up of head, neck body and tailRetroperitoneal
Head lies in the ‘C’ of the duodenum
also overlies IVC, L2 vertebra, medial aorta and superior mesenteric vessels
Behind the neck splenic veins joins superior mesenteric vein to form portal vein
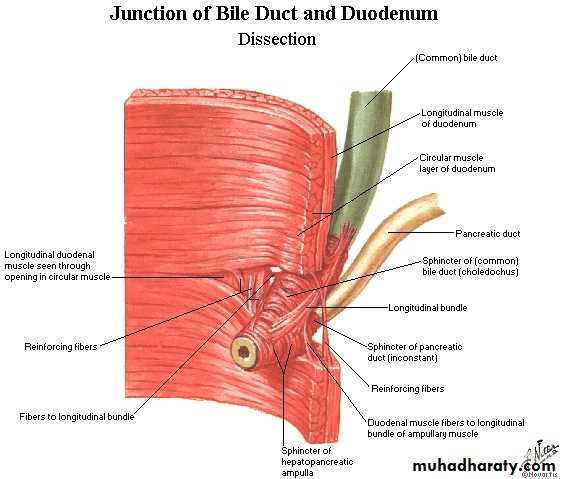
Pancreatic duct closely related to common bile duct
Arterial supply and venous drainage of the pancreas and spleen
Hepaticopancreatic ampulla(Ampulla of Vater)
L2
PANCREAS DISEASES
CongenitalInflammatory
Acute
Chronic
Cysts
Neoplasms
Congenital
Agenesis (very rare)Pancreas Divisum (failure of 2 ducts to fuse) (common)
Annular Pancreas (pancreas encircles duodenum) (rare)
Ectopic Pancreas (very common)
Importance of the pancreas?
The diseased pancreas can cause a LOT of trouble
Diabetes:
In the United States, 25.8 million adults and children (8.3% of population) have diabetes
Systemic disease
Pancreatitis is an emergency situation and common problem
Pancreatic cancer – 4th most common cause of cancer-related death, extremely poor prognosis
Pancreas: two major roles
Control the sugar levels in the body• Produce enzymes that digest food
• 1) Exocrine• 2) Endocrine
Endocrine Pancreatic cells
Islets of Langerhans has FOUR major cell types:
1) Alpha cell
2) Beta cell
3) Gamma cell (PP cell)
4) Delta cell
Islets of Langerhans!!!
Endocrine Pancreatic cells• Alpha cells glucagon
• Beta cells insulin
• Gamma cells pancreatic polypeptide
• Delta cells somatostatin
•
Alpha cells
Alpha cells make up 33-46% of the human islet cellsMake and secrete glucagon to elevate glucose levels in blood
Clinical correlation:
Too much glucagon – glucagonoma
-rare tumor of the alpha cells that cause up to 1000-fold overproduction of glucagon
-blood glucose raises via gluconeogenesis and lipolysis
-causes diabetes mellitus
Beta cells
Make up 65-80% of the cells in the isletsPathology:
Type 1 diabetes mellitus• Insulin-dependent diabetes
• Autoimmune disease
• Body cannot make insulin
Type 2 diabetes mellitus
• Non insulin-dependent diabetes
• Body can still make insulin, but tissues are insensitive to its actions
Gamma cells
Predominantly reside in the head of the pancreasMakes and releases pancreatic polypeptide (PP) in response to ingestion of food
Inhibitory functions
Found to be elevated in anorexia nervosa
Clinical correlation:
-too much PP – Pancreatic polypeptidoma
-can cause weight loss, diabetes mellitus
Delta Cells
Produce somatostatin INHIBITORYProduced in multiple tissues, antigrowth effects
Suppress the release of insulin and glucagon
Clinical correlation:
Too much somatostatin – somatostatinoma
-extreme reduction in secretion of insulin and cause diabetes.
Pancreas and Glucose Homeostasis
Clinical correlation: glucose test
Normal fasting blood sugar: 80 to 120 mg/dLAfter a meal: less than 180 mg/dL 90 minutes after eating is normal
Learning Point
Insulin gets glucose into cells (so that they can use it or store it)
Glucagon is for when the glucose is gone
• (and you need to mobilize storage)Fact
Blood glucose must be tightly regulatedNormally, insulin and glucagon work together
Problems arise when this regulation failsHyperglycemia
Too much glucose in bloodOften suggests malfunction in insulin pathway
Often seen in diabetes mellitus
Chronic hyperglycemia carries several long term effects:Increased risk of cardiovascular disease and stroke
Frequent hunger, thirst, and need for urination
Tissue damage (e.g., retinopathy, nephropathy, neuropathy)
Ketoacidosis
(Sneak preview for your 11/11 lecture)
Importance of the pancreas?The diseased pancreas can cause a LOT of trouble
Diabetes:
In the United States, 25.8 million adults and children (8.3% of population) have diabetes
Systemic disease
Pancreatitis is an emergency situation and common problem
Pancreatic cancer – 4th most common cause of cancer-related death, extremely poor prognosis
pancreatitis
PANCREATITIS
ACUTE (VERY SERIOUS)CHRONIC (Calcifications, Pseudocyst)
CONSEQUENCES of ACUTE and CHRONIC pancreatitis
Acute pancreatitisSpectrum of:
mild
severe
Mild inflammation of pancreas
Extensive pancreatic necrosis
Multi-organ failure
75% cases seen in ED
25% cases seen in ED
Mortality 20-30%
Mortality <1%
causes
Gallstones (35-40%)ETOH (2nd most frequent cause) Ethyl Alcohol (Ethanol)
Tumours
pancreas, ampulla, choledochocele
Scorpion sting
Microbiological – infection
Autoimmnune (SLE, crohn’s)
Surgery/trauma (blunt trauma, cardiac surgery, ERCP)
Hyperlipidaemia (<11mmol, 3rd most freq cause), hypocalcemia, hypothermia
Emboli/ischemia
Drugs (carbamazepine, valproate, frusemide, opiates, estrogens, erythromycin, enalapril, rifampicin)
Cause is unknown in 15-20% of cases.
Clinical presentation acute pancreatitis
HistoryAny severe acute pain in the abdomen or back should suggest acute pancreatitis.
The diagnosis is usually made when a patient presents with
Severe and constant abdominal pain (classically in epigastrium, radiating through to back)
Nausea
Vomiting
Fever
Tachycardia
Clinical presentation acute pancreatitis
ExaminationFever (76%), sinus tachycaria (65%)
Dehydration
Upper abdomen tenderness/epigastric tenderness (68%)
Clinical presentation acute pancreatitis
in severe pancreatitis…Pulmonary signs (effusions, tachypnea secondary to diaphragmatic irritation)
Cullen’s sign (bluish/red discolouration periumbilical wall
Grey-turner’s sign (bluish/red discolouration of flanks)
peritonitis
Cullen’s + Grey Turner’s sign
laboratory testing
No gold standard for diagnosis (apart from histopathological testing of the pancreas)Lipase and amylase
↑ amylase
fallopian tubes, ovaries,
• testes, adipose tissue,
• small bowel, lung, thyroid,
• skeletal muscle,
• and certain neoplasms.
↑ lipase
more specific, but still in small intestineRule out all valid differentials
Differential Diagnosis for upper Abdominal Pain and Tenderness
Perforated Viscus, especially peptic ulcerErect CXR
Acute Cholecystitis and Biliary Colic
LFTs, liver/biliary ultrasound, ERCPAcute Intestinal Obstruction
Abdo XR
Mesenteric Vascular Occlusion
CT angiogram of intestinal vesselsRenal Colic
Urinanalysis, hourly urine output, serum creatinine, CT uretersMyocardial Infarction
ECG, troponinDissecting Aortic Aneurysm
CT angiogramConnective Tissue Disorders with vasculitis
ESRPneumonia
CXRDiabetic Ketoacidosis
serum glucose, ABG
Assessing severity
Ranson’s criteriaAt admission
age in years > 55 yearswhite blood cell count > 16000 cells/mm3
blood glucose > 10 mmol/L (> 200 mg/dL)
serum AST > 250 IU/L
serum LDH > 350 IU/L
At 48 hours
Calcium (serum calcium < 2.0 mmol/L (< 8.0 mg/dL)Hematocrit fall > 10%
Oxygen (hypoxemia PO2 < 60 mmHg)
BUN increased by 1.8 or more mmol/L (5 or more mg/dL) after IV fluid hydration
Base deficit (negative base excess) > 4 mEq/L
Sequestration of fluids > 6 L
...many severity scores
Score 0 to 2 : 2% mortality
Score 3 to 4 : 15% mortalityScore 5 to 6 : 40% mortality
Score 7 to 8 : 100% mortality
Radiology of acute pancreatitis
U/S
useful for biliary pathology, 70-80% sensitive for pancreatitisCT more useful for judging severity and regional effects
Try to wait >12 hours as early CT is usually unhelpfulTreating Acute Pancreatitis
Mild to Moderate Pancreatitis:usually requires treatment with IV fluids and fasting.
clear liquid diet is frequently started on the third to sixth day
regular diet by the fifth to seventh day
The decision to reintroduce oral intake is usually based on the following criteria:
a decrease in or resolution of abdominal pain;
the patient is hungry; and
Organ dysfunction, if present, has resolved
Antibiotics – controversial, but currently recommended
Treating Acute Pancreatitis
Unremitting Fulminant Pancreatitis:usually requires inordinate amounts of fluid
close attention to complications
cardiovascular collapse, respiratory insufficiency, and pancreatic infection, as well as possible surgical debridement or drainage.
Treating Acute Pancreatitis
Conservative TreatmentOperative Treatment
Treating Acute Pancreatitis Conservative
((R)) Regimen include• Relieve the pain
• Rest of pancreas
• Rest of bowel
• Resuscitation
• Resist enzymatic activity
Treating Acute Pancreatitis Conservative
((R)) Regimen include
• 6. Resist infection
• 7. Repeated examinations
• 8. Repeated blood tests
• 9. Respiratory support
• 10. Renal output
Operative Treatment
• 1. Endoscopic papillotomy• 2. Pancreatic debridment
• 3. Internal drainage of pancreatic pseudocyst
• 4. Subsequent treatment