لثة \ خامس اسنان
د. رؤى (م2)2\1\2017
لثة \ خامس اسنان
د. رؤى (م2)
2\1\2017
Periodontal flaps
Periodontal flap is a section of gingiva and/or mucosa surgically separated from the underlying tissues to provide visibility of and access to the bone and root surface. The flap also allow the gingiva to be displaced to a different location in patients with mucogingival involvement.Classification of flaps
Periodontal flap can be classified based on the following:
Bone exposure after flap reflection
Placement of flap after surgery
Management of papilla
Based on bone exposure after reflection
Full thickness (mucoperiosteal flap): this indicated when respective osseous surgery is contemplated.
Partial thickness (mucosal flap): also called split thickness flap is indicated when flap is to be positioned apically or when the operator does not to desire to expose bone.
Based on flap placement after surgery they are classified as
Nondisplaced flaps
Displaced flaps
Based on management of papilla
Conventional flap, is used when:The interdental spaces are too narrow
When the flap is to be displaced
Conventional flaps include:
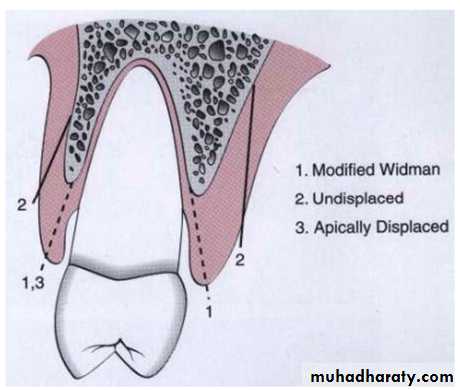
The modified widman flap
The undisplaced flap
The apically displaced flap
Flap for regenerative procedure
Papilla preservation flap
Design of the flap
The design of the flap is dictated by the surgical judgement of the operator and may depend on the objectives of the operation. The entire surgical procedure should be planned in every detail before the intervention is begun.
Incisions
Horizontal incisions
Two type of horizontal incision have been recommended:
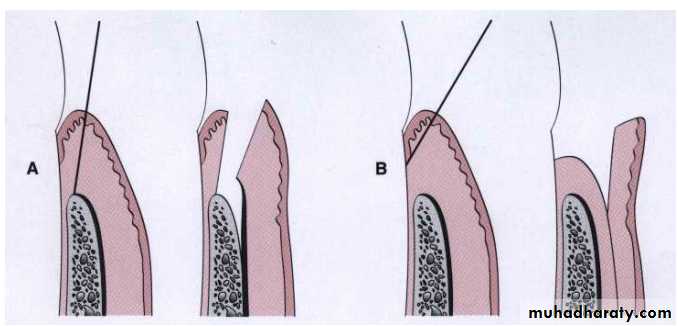
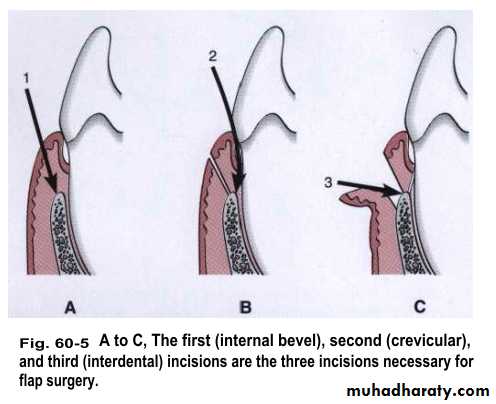
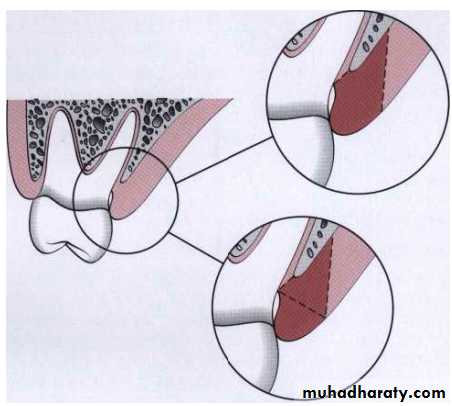
The internal bevel incision which is aimed at the bone crest:
it accomplishes three important objectives
It removes the pocket lining
It conserves the relatively uninvolved outer surface of the gingiva, which, if apically positioned, becomes attached gingiva
It produces a sharp, thin flap margin for adaptation to the bone-tooth junction.
The #11 or #15 surgical scalpel is used most commonly.
Cervicular incision which is starts at the bottom of the pocket and is directed to the bone margin
The interdental incision which is performed after the flap is elevated. The orban knife is usually used for this incision.
That portion of the gingiva left around the tooth contains the epithelium of the pocket lining and the adjacent granulomatous tissue. It is discarded after the cervicular and interdental incisions are performed. A curette or a large scaler can be used for this purpose.
Flaps can be reflected using only the horizontal incision if sufficient access can be obtained by this means. If no vertical incisions are made, the flap is called an , envelope flap.
Vertical flap
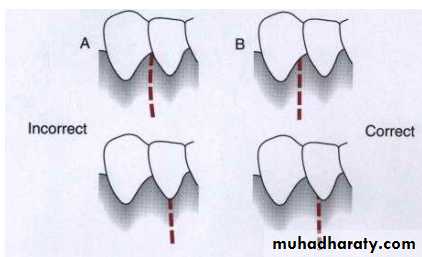
It is necessary if the flap is to be apically displaced. Vertical incisions must extend beyond the mucogingival line reaching the alveolar mucosa to allow for the release of the flap to be displaced. In general, vertical incisions in the lingual and palatal areas are avoided. Facial vertical incisions should not be made in the center of an interdental papilla or over the radicular surface of a tooth. Incisions should be made at the line angels of a tooth either to include the papilla in the flap or to avoid it completely.
Flap technique for pocket therapy
Several techniques can be used for treatment of periodontal pockets. The periodontal flap is one of the most commonly employed procedures, particularly for moderate and deep pockets in posterior areas.Flaps are used for pocket therapy to accomplish the following:
Increase accessibility to root deposits
Eliminate or reduce pocket depth by resection of the pocket wall
Expose the area to perform regenerative methods
The modified Widman flap
Facilitate meticulous instrumentation and for removal of the pocket lining but does not attempt to reduce pocket depth except for the reduction that occurs in healing by tissue shrinkage. It starts with internal bevel incision close to the gingival margin (not more than 1 to 2 mm apically) and follows the normal scalloping of the gingival margin.
Modified Widman flap is unrepositioned mucoperiosteal flap. This technique offers the possibility of establishing an intimate postoperative adaptation of healthy collagenous connective tissue to tooth surfaces and provides access for adequate instrumentation of the root surfaces and immediate closure of the area. The following is an outline of this technique:
Step 1: the initial incision is an internal bevel incision to alveolar crest starting 0.5 to 1 mm away from the gingival margin. Care should be taken to insert the blade in such away that the papilla is left with a thickness similar to that of the remaining facial flap. Vertical relaxing incisions are usually not needed.
Step 2: the gingiva is reflected with a periosteal elevator.
Step 3: crevicular incision is made from the bottom of the pocket to the bone, circumscribing the triangular wedge of tissue containing the pocket lining.
Step 4: after the flap is reflected, a third incision is made in the interdental spaces coronal to the bone with a curette or an interproximal knife, and the gingival collar is removed.
Step 5:granulation tissue are removed with curette, the root surfaces are scaled and planed if needed.
Step 6: bone architecture is not corrected except if it prevents good tissue adaptation to the necks of the teeth.
Step 7: interrupted direct sutures are placed in each interdental space and covered eith tetracycline ointment and with a periodontal surgical pack.
The undisplaced flap
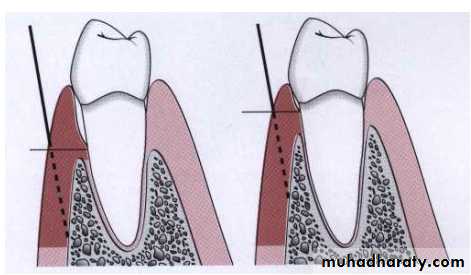
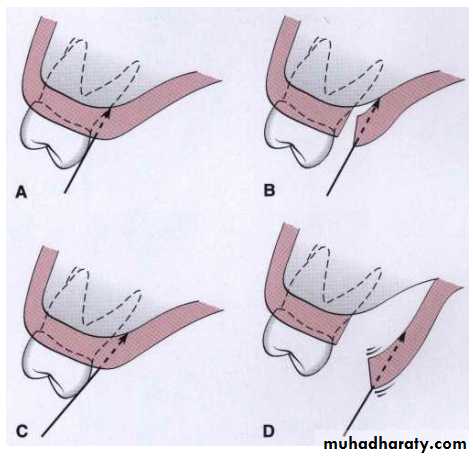
In addition to improving accessibility for instrumentation, removes the pocket wall, reducing or eliminating the pocket. This is essentially an excisional procedure of gingiva. The internal bevel incision is initiated at or near a point just coronal to the projection of the bottom of the pocket on the outer surface of the gingiva. This incision can be accomplished only if there is sufficient attached gingiva remaining apical to the incision. There are two anatomical landmarks to evaluate the amount of attached gingiva that remains, pocket depth and location of the mucogingival junction. If the incision is made too close to the tooth, it will not eliminate the pocket wall and may result in the recreation of a soft tissue pocket. If the tissue is thick it should also be thinned by the initial incision to cover the bone properly during flap closure. Proper placement of the flap during closure is essential to prevent either recurrence of pockets or bone exposure; placement is determined by where this first incision is placed. If the surgeon contemplates osseous surgery, the first incision should be placed in such a way as to compensate for removal of bone tissue so that the flap ends at the tooth-bone junction.
The techniques used for regenerative purposes are the papilla preservation flap and the flap using only crevicular or pocket incisions, to retain the maximum amount of gingival tissue, including the papilla, for graft or membrane coverage.
It is the most commonly performed type of periodontal surgery. It differs from the modified Widman flap in that the soft tissue pocket wall is removed with the initial incision; thus it may be considered an internal bevel gingivectomy. The undisplaced flap and gingivectomy are the two techniques that surgically removed the pocket wall. To perform this technique without creating a mucogingival problem it should be determined that enough attached gingiva will remain after after removal of pocket wall. The following outline of this technique:
Step 1: the pockets are measured with periodontal probe, and a bleeding point is produced on the outer surface of the gingiva to mark the pocket bottom.
Step 2: internal bevel incision is made on bleeding points. In addition, thinning of the flap should be done with the initial incision because at this time, it is easier to accomplish than later with loose reflected flap that is difficult to manage.
Step 3: the crevicular incision is made from the bottom of the pocket to the bone to detach the connective tissue from the bone.
Step 4: the flap is reflected with a periosteal elevator. No need for vertical incision.
Step 5: the interdental incision is made with an interdental knife.
Step 6: the triangular wegde of tissue created is removed with curette.
Step 7: after the necessary scaling and root planning, the flap edge should be rest on the root-bone junction.
Step 9: a continuous sling suture is used to secure the facial and lingual or palatal flaps. The area covered with a periodontal pack.
Apically displaced flap
Improves accessibility and eliminate or reduce the pocket depth. It preserves to be positioned apically while its lining is removed and/or increases the width of the attached gingiva by transforming the previously unattached keratinized pocket wall into attached tissue. The purpose of this surgical technique is to preserve the maximum amount of keratinized gingiva. For this reason, the internal bevel incision should be made as close to the tooth as possible (0.5 to 0.1 mm).
This type of flap can be used for pocket eradication or widening the zone of attached gingiva. So, according to the purpose it can be a full thickness ( mucoperiosteal) or split thickness (mucosal) flap. The split thickness flap requires more precision and time, and gingival tissue thick enough to split, but it can be more accurately positioned and sutured in an apical position using a periosteal suture technique, as follow:
Step 1: an internal bevel incision is made, to preserve tissue as much as possible, it should be no more than about 1 mm from the crest of the gingiva.
Step 2: crevicular incisions are made, followed by initial elevation of the flap, and then interdental incisions are performed and the wedge of tissue is removed.
Step 3: vertical incisions are made extending beyond the mucogingival junction.
Step 4: after removal of all granulation tissue, scaling and root planning, and osseous surgery if needed, the flap is apically displaced.
Step 5: if a full thickness flap was performed, a sling suture done and periodontal pack is placed, while a partial thickness flap is sutured to the periosteum. A dry foil is placed over the flap before covering it with the dressing to prevent the introduction of pack under the flap.
After 1 week, dressings and sutures are removed. The area is usually repacked for another week, after which the patient is instructed to use chlorhexidine mouth rinse or to apply chlorhexidine topically with cotton-tipped applicators for another 2 to 3 weeks.
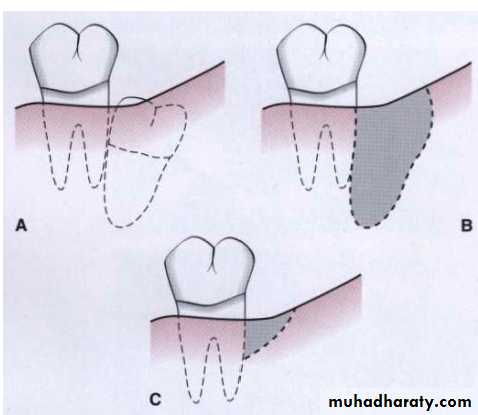
The palatal flap
The surgical approach to the palatal area differ from that for other areas because of the character of the palatal tissue and the anatomy of the area. The palatal tissue is all attached, keratinized tissue and has none of elastic properties associated with other gingival tissues. Therefore the palatal tissue cannot be apically displaced, nor can a partial thickness flap be accomplished. It cannot be moved apically or coronally to adapt to the root-bone junction, as can be done with the flaps in other areas. Therefore the location of the initial incision as important for final placement of the flap.The initial incision for a flap varies with the anatomic situation. The initial incision may be the usual internal bevel incision, followed by crevicular and interdental incisions. If the tissue is thick, a horizontal gingivectomy incision may be made, followed by internal bevel incision that starts at the edge of this incision and ends on the lateral surface of the undelying bone. The placement of the internal bevel incision must be done in such a way that the flap fits around the tooth without exposing the bone.
Before the flap is reflected to the final position for scaling and management of the osseous lesion, its thickness must be checked. Its best to thin the flaps before their complete reflection, because a free, mobile flap is difficult to hold for thinning.
The purpose of the palatal flap should be considered before the incision is made. If it done for debridement, the internal bevel incision is planned so that the flap adapts at the root-bone junction when sutured. If osseous resection is necessary, the incision should be planned to compensate for the lowered level of the bone when the flap is closed.
Flaps for regenerative surgery
The flap design for regenerative surgery should be set up the maximum amount of gingival tissue and papilla are retained to cover the materials placed in the pocket.Two flap designs are available for regenerative surgery:
The papilla preservation flap
The technique for employing a papilla preservation flap is as follows:
Step 1: a crevicular incision is made around each tooth with no incisions across the interdental papilla.
Step 2: the papilla can be incorporated into the facial or lingual/palatal flap, although it is most commonly integrated into the facial flap.
Step 3: the papilla is then dissected from the lingual or palatal aspect and elevated intact with the facial flap.
Step 4: the flap is reflected without thinning the tissue.
The conventional flap with only crevicular
The technique for employing a conventional flap for regenerative surgery is as follows:
Step 1: incise the tissue at the bottom of the pocket and to the crest of the bone, splitting the papilla below the contact point. Every effort should be made to retain as much tissue as possible to subsequently protect the area.
Step 2: reflect the flap maintaining it as thick as possible, not attempting to thin it as is done for respective surgery. The maintenance of a thick flap is necessary to prevent exposure of the graft or the membrane due to necrosis of the flap margins.
To use papilla preservation flap, there must be adequate interdental space to allow the intact papilla to be reflected with the facial or lingual/palatal flap. When the interdental space is very narrow, making it impossible to perform a papilla preservation flap, a conventional flap with only crevicular incisions is made.
Distal molar surgery
Treatment of periodontal pockets on the distal surface of terminal molars is often complicated by the presence of bulbous fibrous tissue over the maxillary tuberosity or prominent retromolar pads in the mandible. Deep vertical defects are also commonly present. Some of these osseous lesions may result from incomplete repair after the extraction of impacted third molars.