1
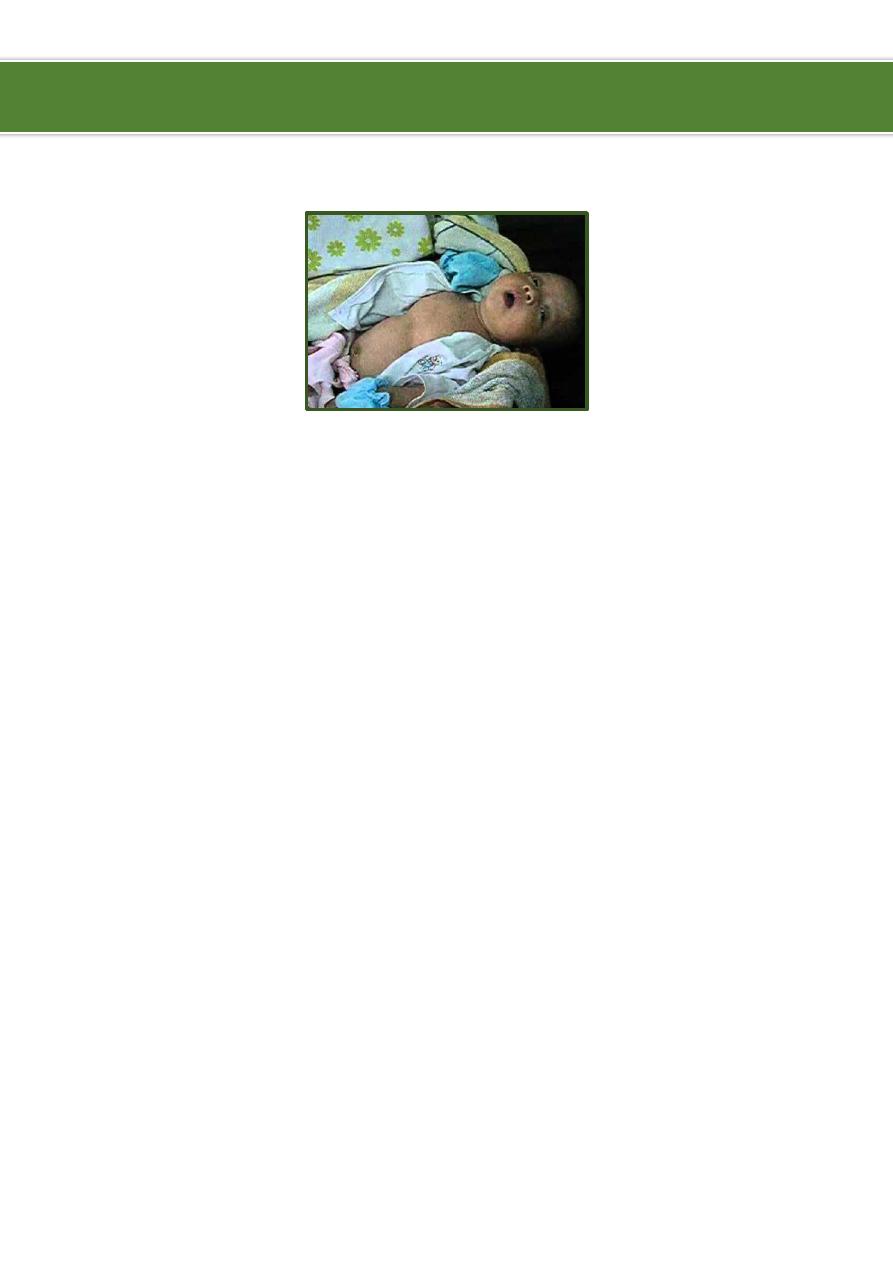
Respiratory distress
Degree:
Mild: flaring of ala nasi and tachypnea.
Moderate: use of accessory muscles.
Severe: Grunting.
More severe: all of above + cyanosis + conscious level (irritability).
Main signs:
Breathing rate Tachypnea (increased O2 wash alkalosis retention of CO2
acidosis).
Increased heart rate Low oxygen levels may cause an increase in heart rate.
Color changes A bluish color seen around the mouth, on the inside of the lips, or on
the fingernails, the color of the skin may also appear pale or gray.
Grunting A grunting sound can be heard each time the person exhales. This
grunting is the body's way of trying to keep air in the lungs so they will stay open.
Nose flaring The openings of the nose spreading open while breathing.
Retractions The chest appears to sink in just below the neck and/or under the
breastbone with each breath (suprasternal, supraclavicular, intercostal, subcostal) --
one way of trying to bring more air into the lungs.
Sweating There may be increased sweat on the head, but the skin does not feel
warm to the touch. More often, the skin may feel cool or clammy. This may happen
when the breathing rate is very fast.
Wheezing A tight, whistling or musical sound heard with each breath can indicate
that the air passages may be smaller, making it more difficult to breathe.
Stridor An inspiratory sound heard in the upper airway.
Accessory muscle use muscles of the neck appear to be moving when child breathes
in. This can also be seen under the rib cage or even the muscles between the ribs.
Changes in alertness child is more tired and may indicate respiratory fatigue.
Ibnlatef
Notes
Pediatrics

2
Other signs:
Asymmetrical movement of the chest.
Harrison's sulcus permanent indentation of chest wall along the costal margins
where diaphragm inserts, due to chronic dyspnea in asthma, COPD, bronchiolitis
obliterans, heart diseases, also occur in rickets.
Tracheal Tag pulling of thyroid cartilage towards the sternal notch in inspiration.
Associated symptoms:
Nasal discharge (rhinorrhea), Sneezing.
Otalgia, Ear discharge (otorrhea).
Dysphagia.
Chest pain (if child can explain).
Pulsus paradoxus fall in systolic BP > 15 mmHg during inspiration.
Ask about: activity, sleeping pattern, feeding.
General information:
RDS is a condition that need admission postnatally and its effect is long-lived.
Surfactant formation starts at 28 weeks and complete at 37 weeks.
For maturity of lung of the baby dexamethasone is replaced by betamethasone
(one injection/ 24 hours before delivery).
Causes of respiratory distress:
Reparatory: pneumonia, bronchiolitis, bronchitis, asthma, plural effusion,
pneumothorax relieved by O2.
Cardiac not respond to O2.
Metabolic: diabetic ketoacidosis, acute renal failure, dehydration.
Neurological, drugs (opioids), severe anemia.
Differential diagnosis of chronic cough + respiratory distress syndrome:
Infections Pertussis (most common), TB.
Asthma, Bronchiectasis.
Sinusitis, Foreign body.
Bronchiolitis obliteration.
Congenital anomaly.
----------------------------------------------------------------------------------------------
www.facebook.com/ibnlatef
https://goo.gl/RpvNsl
