CEMENTUMDr. Bassam ELGHARABLY
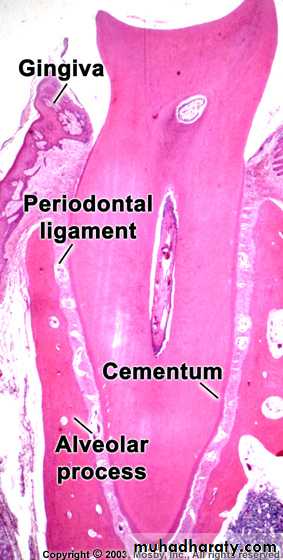
Cementum
The other boneIt is a hard avascular connective tissue that covers the roots of teeth
Role of Cementum
• It covers and protects the root dentin (covers the opening of dentinal tubules)• It provides attachment of the periodontal fibers
• It reverses tooth resorption
Varies in thickness: thickest in the apex and
In the inter-radicular areas of multirootedteeth, and thinnest in the cervical area
10 to 15 m in the cervical areas to
50 to 200 m (can exceed > 600 m) apicallyCementum simulates bone
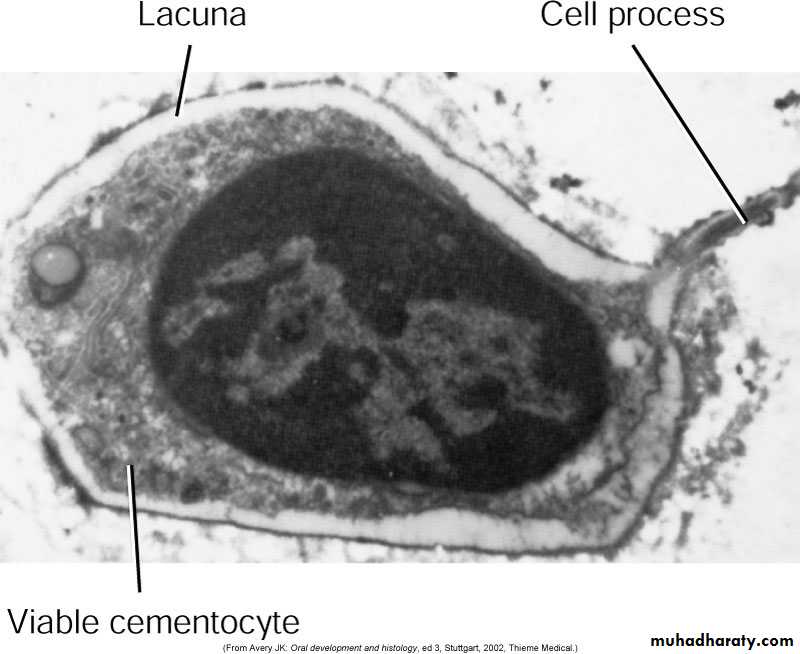
Organic fibrous framework, ground substance, crystal type, developmentLacunae
Canaliculi
Cellular component
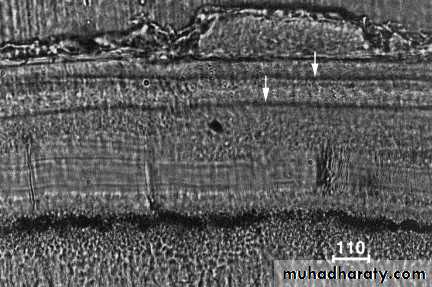
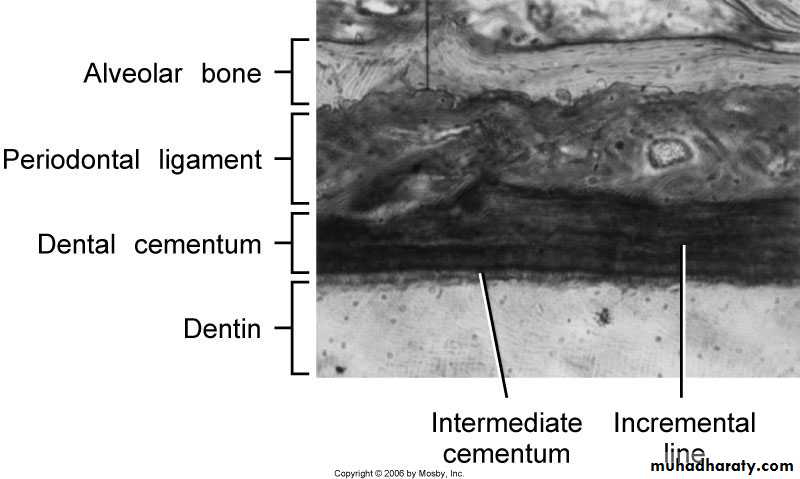
Incremental lines (also known as “resting” lines; they are produced by continuous but phasic, deposition of cementum)
Incremental lines
Under the light microscope alternating light and dark lines are visible in ground sections of human root cementum. These lines are believed to be incremental lines and to repeat at an annual rhythm. With different microscopical techniques we examine the ultra structural nature of this light microscopical phenomenon and the distribution of these lines in the rootDifferences between cementum and bone
• Not vascularized• Minor ability to remodel
• More resistant to resorption compared to bone
• Lacks neural component – so no pain
• 70% of bone is made by inorganic salts while cementum only 45-50%
• Contains unique (specific) proteoglycan interfibriler substance
Clinical Correlation
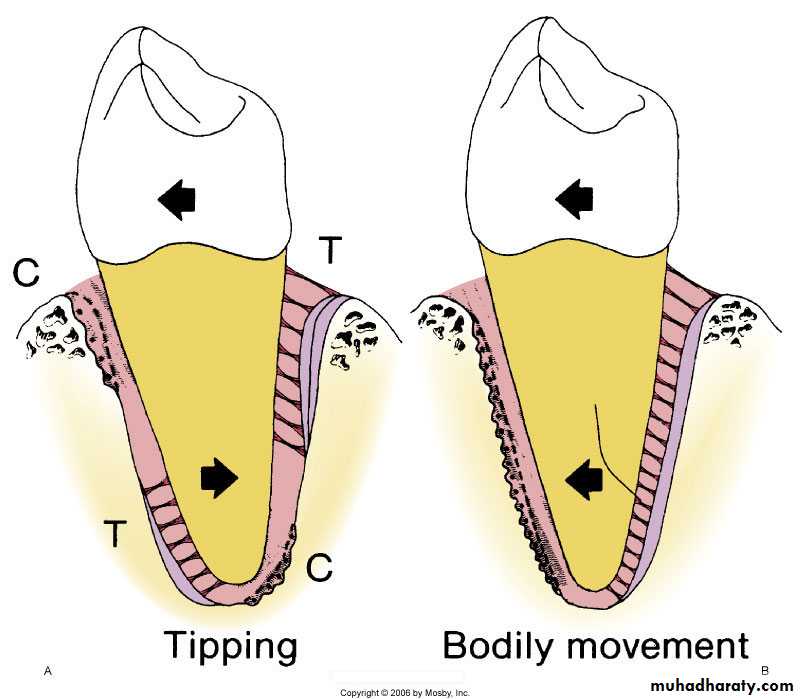
Cementum is more resistant to resorption: Important in permittingorthodontic tooth movement
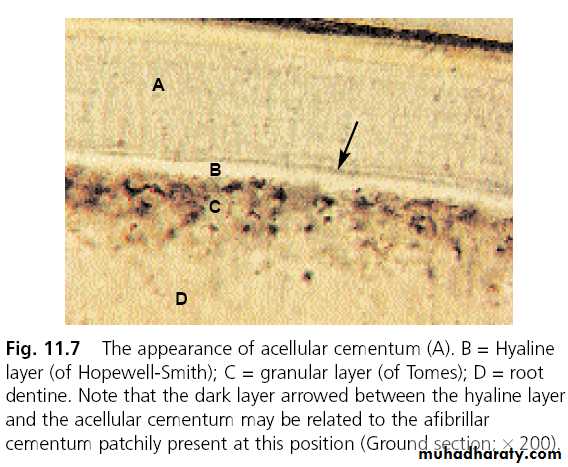
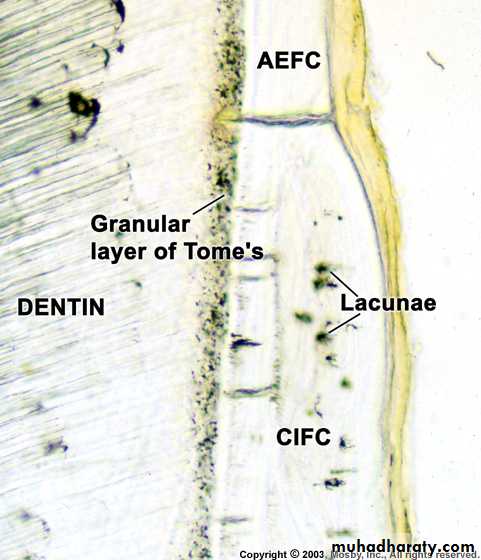
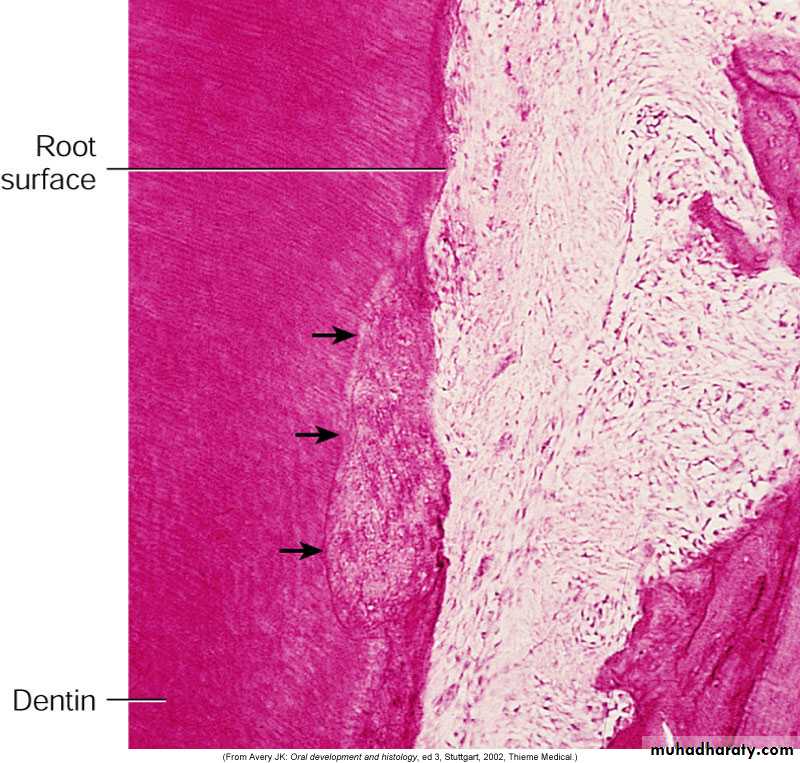
First layer of cementum is called intermediate cementum or Hyaline layer of Hopewell-Smith
Intermediate cementum is situated between the granular layer of dentin and the secondary cementum that is formed by the cementoblasts
Approximately 10 m thick and mineralizes greater than the adjacent dentin or the secondary cementum
Hyaline layer of Hopewell-Smith (Intermediate Cementum)
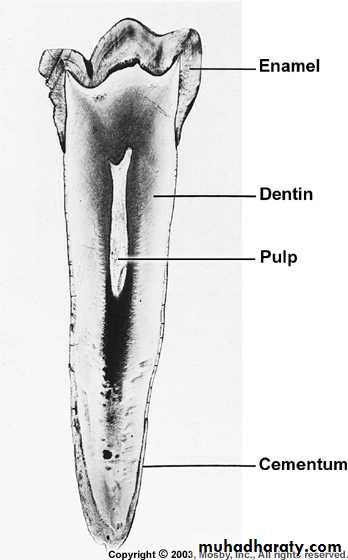
Properties of Cementum
Physical:Cementum is light yellow with a dull surface
Cementum is more permeable than other dental tissues
Relative softness and the thinness at the cervical portion means
that cementum is readily removed by the abrasion when gingival
recession exposes the root surface to the oral environment
Chemical Composition of Cementum
Similar to bone45% to 50% hydroxyapatite (inorganic)
50% to 55% collagenous and noncollagenous matrix proteins
(organic)Collagenous component
TYPE ITYPE III
TYPE XII
TYPE V
TYPE XIV
Classification of Cementum
• 1. Presence or absence of cells• 2. Origin of collagenous fibers
• of the matrix
• FORMATİON TİME
• Prefunctional and functional
CELLULAR
ACELLULARExtrinsic fibers
Intrinsic fibers
PRİMER
SECONDER
MİXED
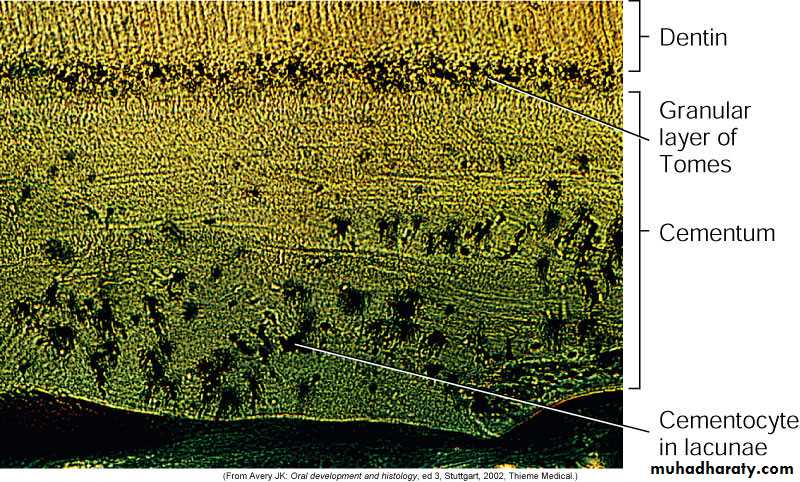
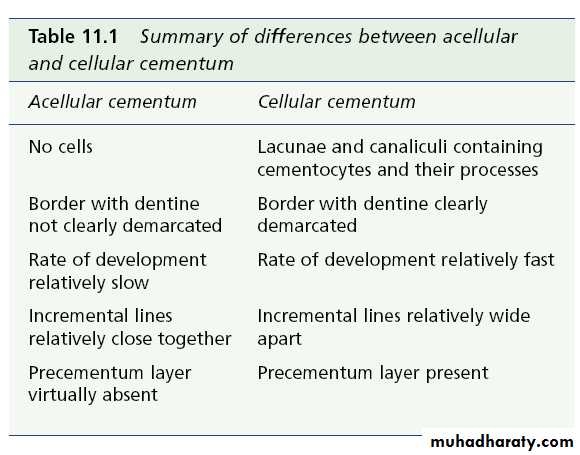
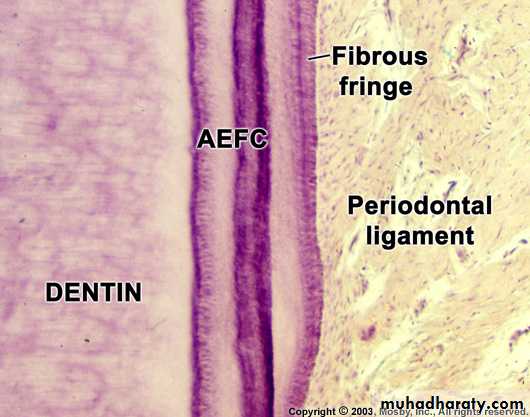
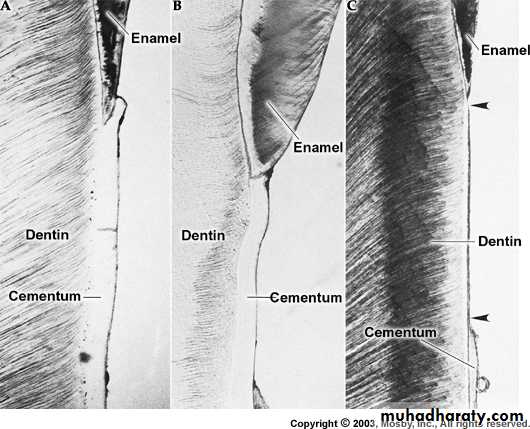
Cellular and Acellular Cementum
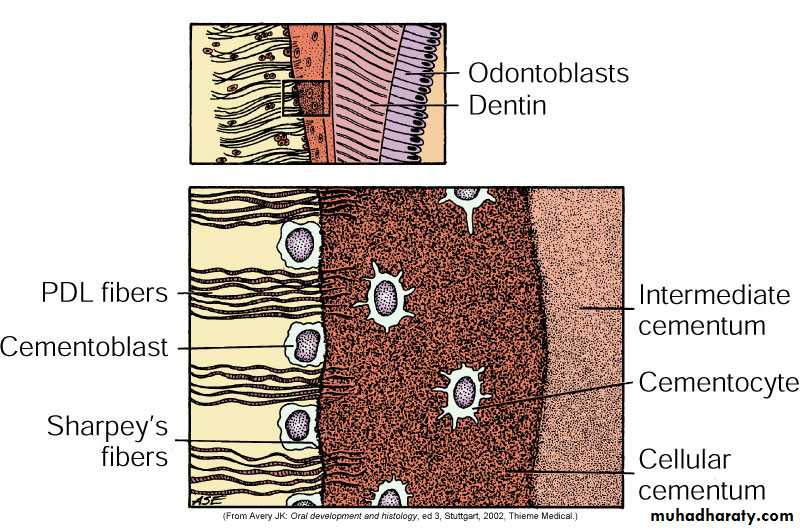
A: Acellular cementum (primary cementum)B: Cellular Cementum (secondary cementum)
Acellular cementum: covers the root
adjacent to dentin whereas cellular
cementum is found in the apical area
Cellular: apical area and overlying
acellular cementum. Also common ininterradicular areas
Cementum is more cellular as the
thickness increases in order to maintainViability
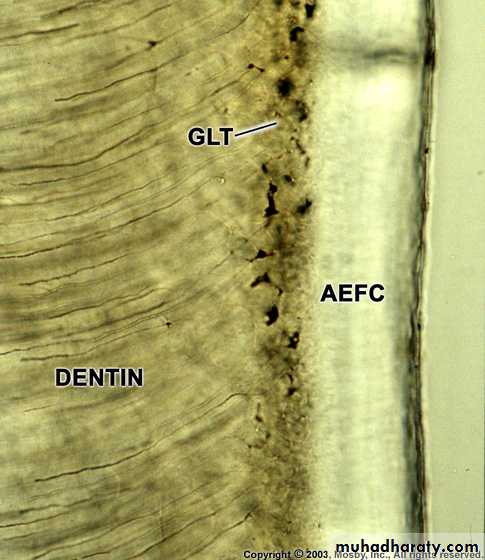
A: Acellular cementum
B: Hyaline layer of Hopwell-SmithIntermediate Cementum
C: Granular layer of Tomes
D: Root dentin
Cellular: Has cells
Acellular: No cells and has no structure
Cellular cementum usually overlies acellular cementumAcellular
CellularVariations also noted where acellular and cellular reverse in position
and also alternateDentin
GTLacuna of cementocyte
Canaliculus
CEMENTUM
Cellular cementum
Acellular cementum
Intermediate CementumGranular layer of tomesd
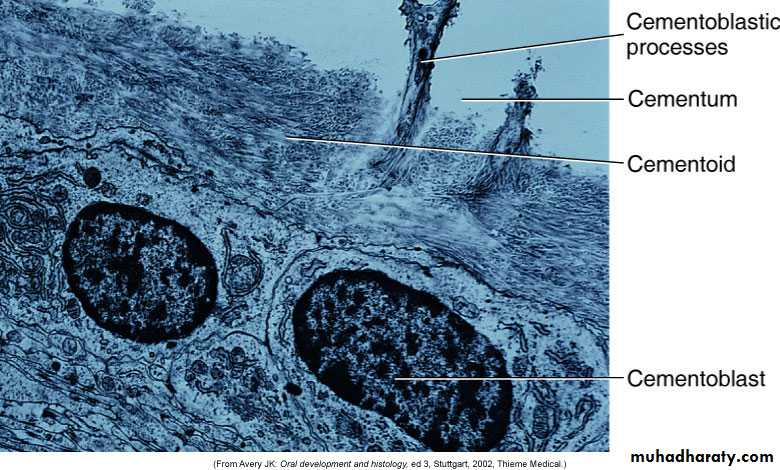
Dentin with tubulesCementoblast and cementocyte
Cementocytes in lacunae and the channels that their processes extend arecalled the canaliculi
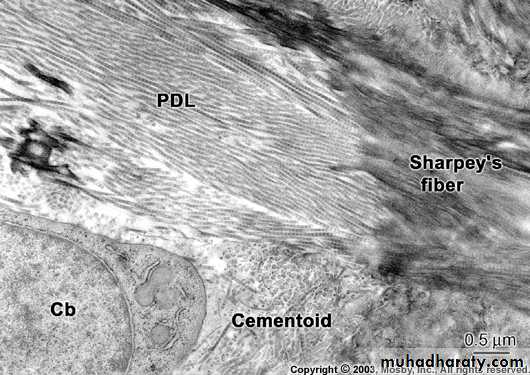
Cementoid: Young matrix that becomes secondarily mineralized
Cementum is deposited in increments similar to bone and dentinAre acellular and cellular cementum formed from two different sources?
One theory is that the structural differences between acellular and cellularcementum is related to the faster rate of matrix formation for cellular
cementum. Cementoblasts gets incorporated and embedded in the tissue
as cementocytes.
Different rates of cementum formation also reflected in more widely
spaced incremental lines in cellular cementumClassification Based on the Nature and Origin of Collagen Fibers
• Periodontal ligament (Sharpey’s fibers)• Cementoblasts
Extrinsic fibers if derived from PDL. These are in the same
direction of the PDL principal fibers i.e. perpendicular oroblique to the root surface
Intrinsic fibers if derived from cementoblasts. Run parallel to
the root surface and at right angles to the extrinsic fibersThe area where both extrinsic and intrinsic fibers is called
mixed fiber cementumCombined classification
• Primary Acellular Extrinsic Fiber Cementum (PAEF - Cementum)• Primary Acellular İntrinsic Fiber Cementum (PAİF - Cementum)
• Secondary Cellular İntrinsic Fiber Cementum (SCİF – Cementum)
• Secondary Cellular Mixed Fiber Cementum (SCMF - Cementum)
• Acellular afibrillar cementum
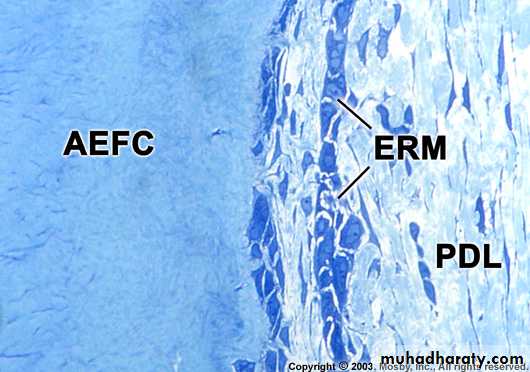
A. Primary Acellular Extrinsic Fiber Cementum (PAEF- Cementum)
• Located in cervical half of the root and constitutes the bulk of cementum
• The collagen fibers derived from Sharpey’s fibers and ground substance from cementoblasts• Covers 2/3rds of root corresponding with the distribution of primary acellular Cementum
• Principal tissue of attachment
• Function in anchoring of tooth
• Fibers are well mineralized
B. Primary acellular intrinsic fiber cementum (PAİFC)
First cementum - Primary cementumAcellular
Before PDL forms
Cementoblasts
15-20μm
C. Secondary Cellular intrinsic fiber cementum (SCIF- Cementum )
Starts forming after the tooth is in occlusionIncorporated cells with majority of fibers organized parallel to the root surface
Cells have phenotype of bone forming cells
Very minor role in attachment (virtually absent in incisors and canine teeth)
İt is seen in middle to apical third and intrer radicular
Adaptation
Repair
D. Secondary Cellular Mixed Fiber Cementum
Both intrinsic and extrinsic fibers[Extrinsic (5 – 7 m) and Intrinsic (1 – 2 m)]
Bulk of secondary cementum
CementocytesLaminated structure
Cementoid on the surfaceApical portion and intrerradicular
AdaptationE. Acellular afibrillar cementum
Limited to enamel surfaceClose to the CE junction
Lacks collagen so plays no role in attachmentDistribution of Cementum on the Root
Acellular afibrillar: cervical enamelAcellular extrinsic: Cervix to practically the whole root (incisors, canines) increasing in thickness towards the apical portion 50200μm
Cellular: Apical third, furcations
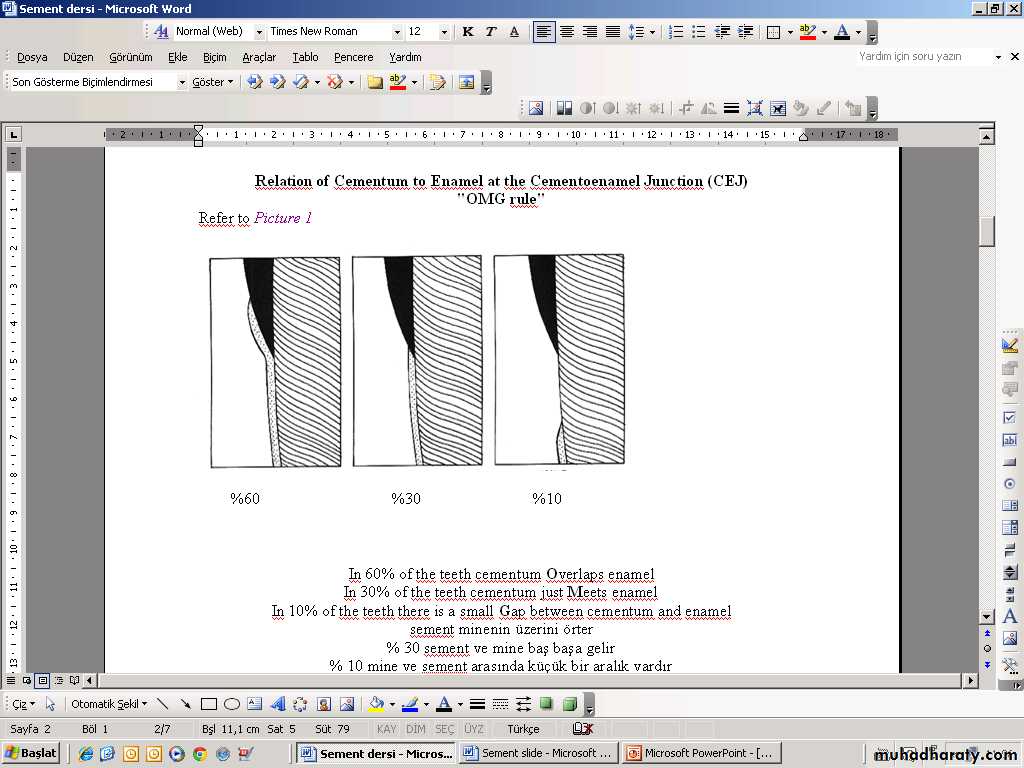
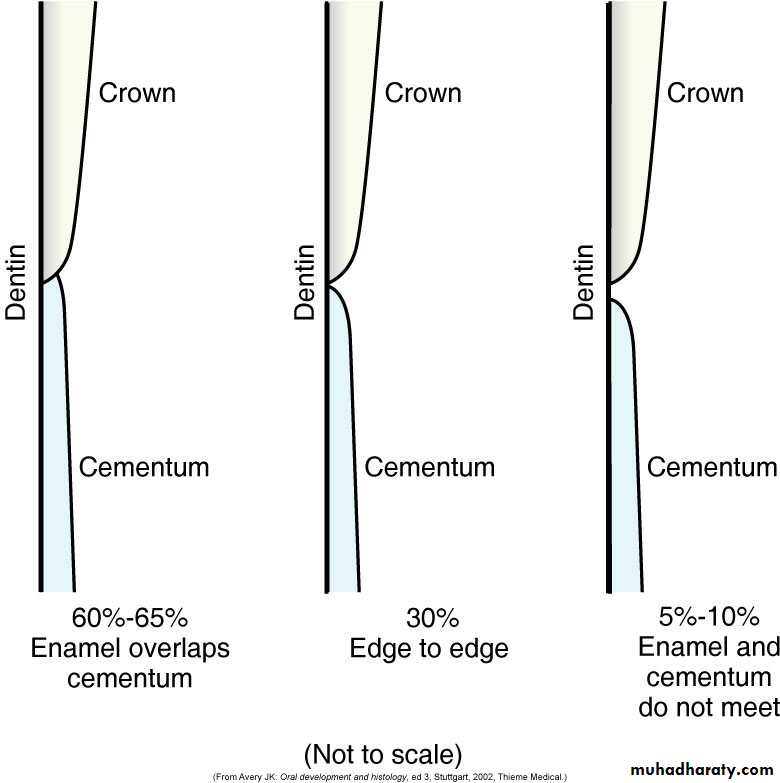
Cementum overlaps enamel 60%Cementum just meets enamel 30%
Small gap between cementum and enamel 10%
RELATION OF CEMENTUM TO ENAMEL AT THE CEMENTOENAMEL JUNCTION
Aging of Cementum
• Smooth surface becomes irregular due to calcification of ligament fiber bundles where they are attached to cementum
• Continues deposition of cementum occurs with age in the apical area.
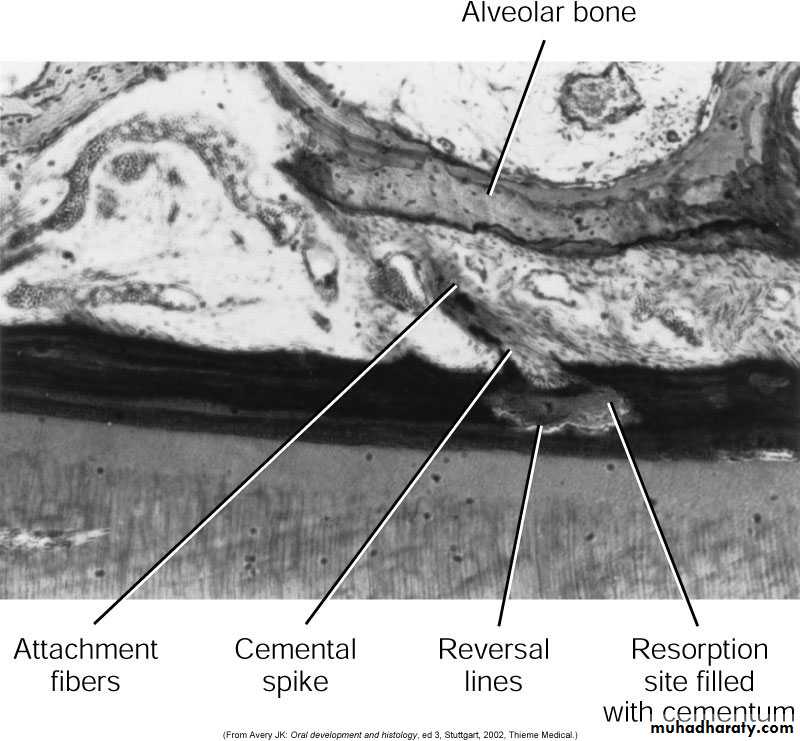
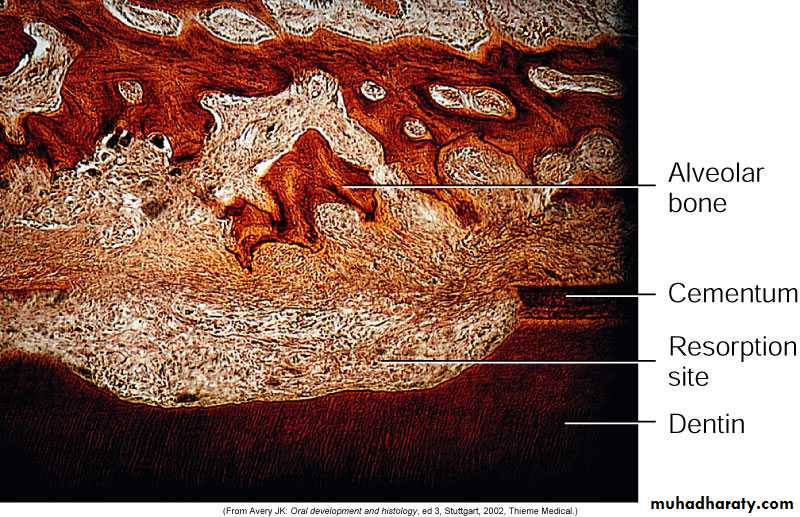
• Cementum resorption.Active for a period of time and then stops for cementum deposition creating reversal lines
• Resorption of root dentin occurs with aging which is covered by cemental repair
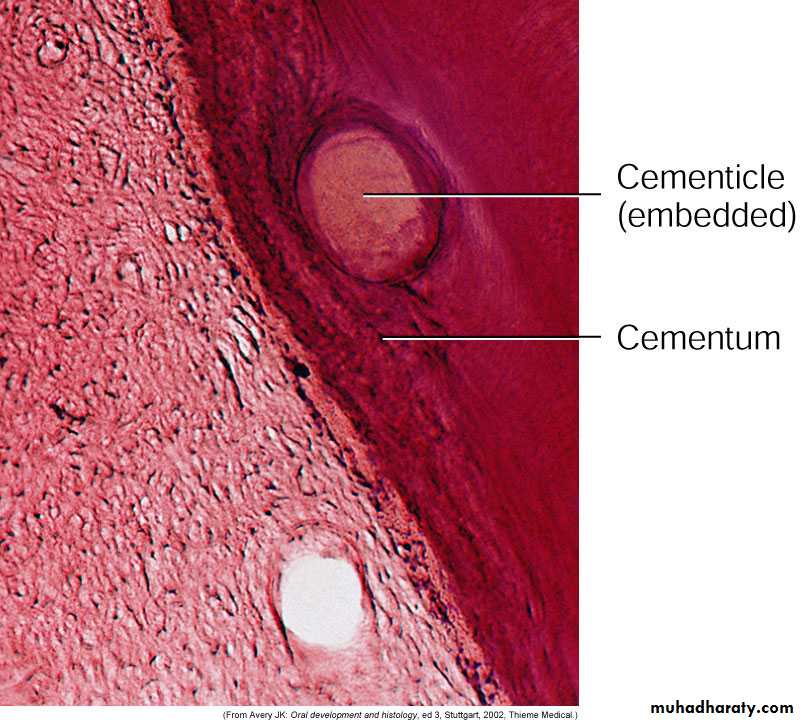
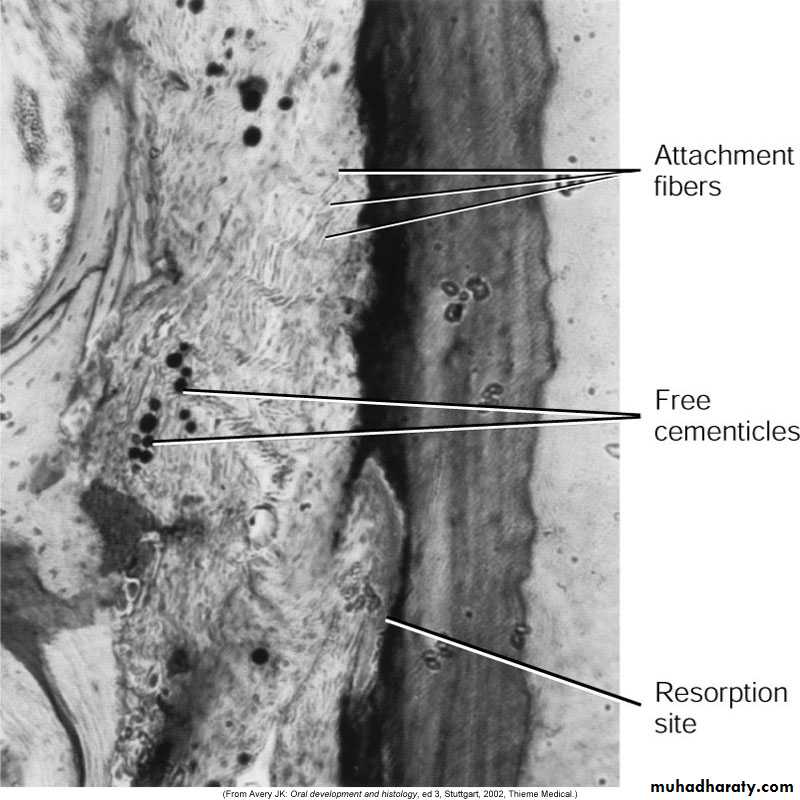
Cementicles
Calcified ovoid or round nodule foundin the PDL
Single or multiple near the cemental surface
Free in ligament; attached or embedded
in cementumAging and at sites of trauma
Origin: Nidus of epithelial cell that arecomposed of calcium phosphate and
collagen to the same amount as
cementum (45% to 50% inorganic
and 50% to 55% organic)
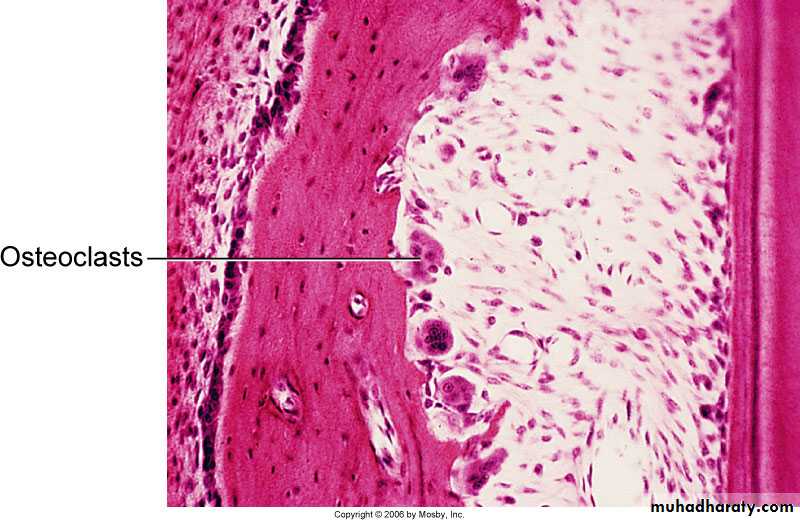
Cemental Repair
Protective function of cementoblasts afterresorption of root dentin or cementum
Resorption of dentin and cementum due
to trauma (traumatic occlusion, tooth
movement, hypereruption)
Loss of cementum accompanied by loss
of attachmentFollowing reparative cementum
deposition attachment is restoredClinical Correlation
Cellular cementum is similar to bone but has no nerves.Therefore it is non-sensitive to pain. Scaling produces no pain, but if cementum is removed, dentin is exposedcauses sensitivityCementum is resistant to resorption especially in younger
Patients, Thus, orthodontic tooth movement causes alveolar bone resorption and not tooth root loss• In most cases of repair, there is a tendency to re-establish the former outline of the root surface by cementum. This is called anatomic repair.
• However, if only a thin layer of cementum is deposited on the surface of a deep resorption, the root outline is not reconstructed, & a bay like recess remains.
• In such areas the periodontal space is restored to its normal width by formation of a bony projection, so that a proper functional relationship will result. the outline of the alveolar bone in these cases follows that of the root surface. This is called functional repair.
42
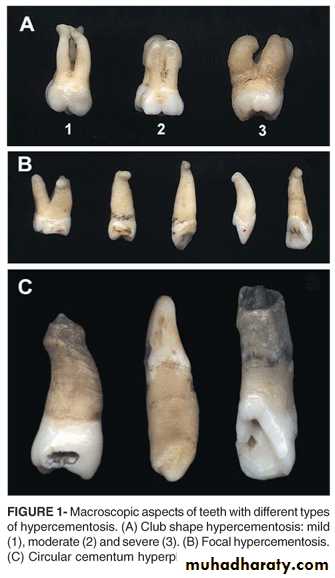
HYPERCEMENTOSIS
• Is an abnormal thickening of cementum.
• May affect all teeth of the dentition, be confined to a single tooth, or even affect only parts of one tooth.
• If the overgrowth improves the functional qualities of the cementum, it is termed cementum hypertrophy.
• If the overgrowth occurs in non-functional teeth or if it is not correlated with increased function, its termed hyperplasia.
43
Extensive hyperplasia of cementum is occasionally associated with chronic periapical inflammation.
Hyperplasia of cementum in non-functioning teeth is characterized by a reduction in the number of Sharpey’s fibers embedded in the root.
This may cause problems during tooth extraction.
Hypercementosis affecting all the teeth may be associated with Paget’s disease.44
HYPERCEMENTOSIS