د. راف
ع
عالوي الفياض
Body fluids physiology
كلية طب الفلوجة
2016-2017
*******************************************************************************
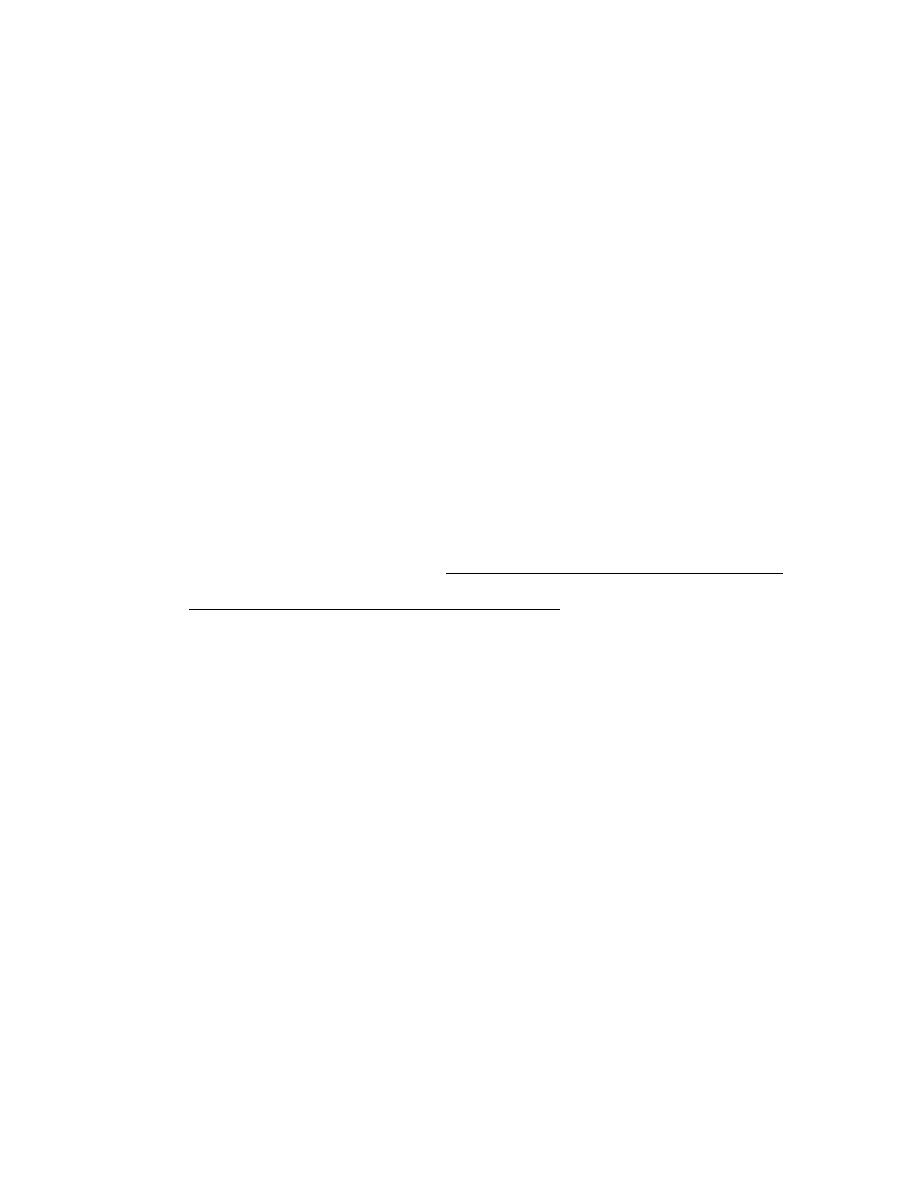
Body Fluid in Human Body
cells can't live without water; they can't survive or perform their functions
without being in a solution. That's why 60% of our body weight is water,
and that’s about 42 liters in human body (in adult male (70) kg). It is located
in different areas or regions:
1- Extracellular body fluid (ECF): located outside the cell, either
inside the vessels which is intravascular or outside the vessels which
is interstitial. The amount of ECF is about the third of the total body
water, so about 12 liters outside the cells. They are located in the
plasma and interstitial compartments. The barrier between
intravascular and interstitial is the capillaries (the layer of the
epithelial cells of the capillaries) endothelial cells.
2- Intracellular body fluid (ICF): It makes the major compartment of
body fluid and is located inside the cells. Even though the cell is very
tiny but we are talking about trillions of cells, so if you collect the
amount of water inside the cells you'll get about 28 liters in average.
The barrier between ECF & ICF is the cytoplasmic membrane of the
cells.
د. راف
ع
عالوي الفياض
Body fluids physiology
كلية طب الفلوجة
2016-2017
*******************************************************************************
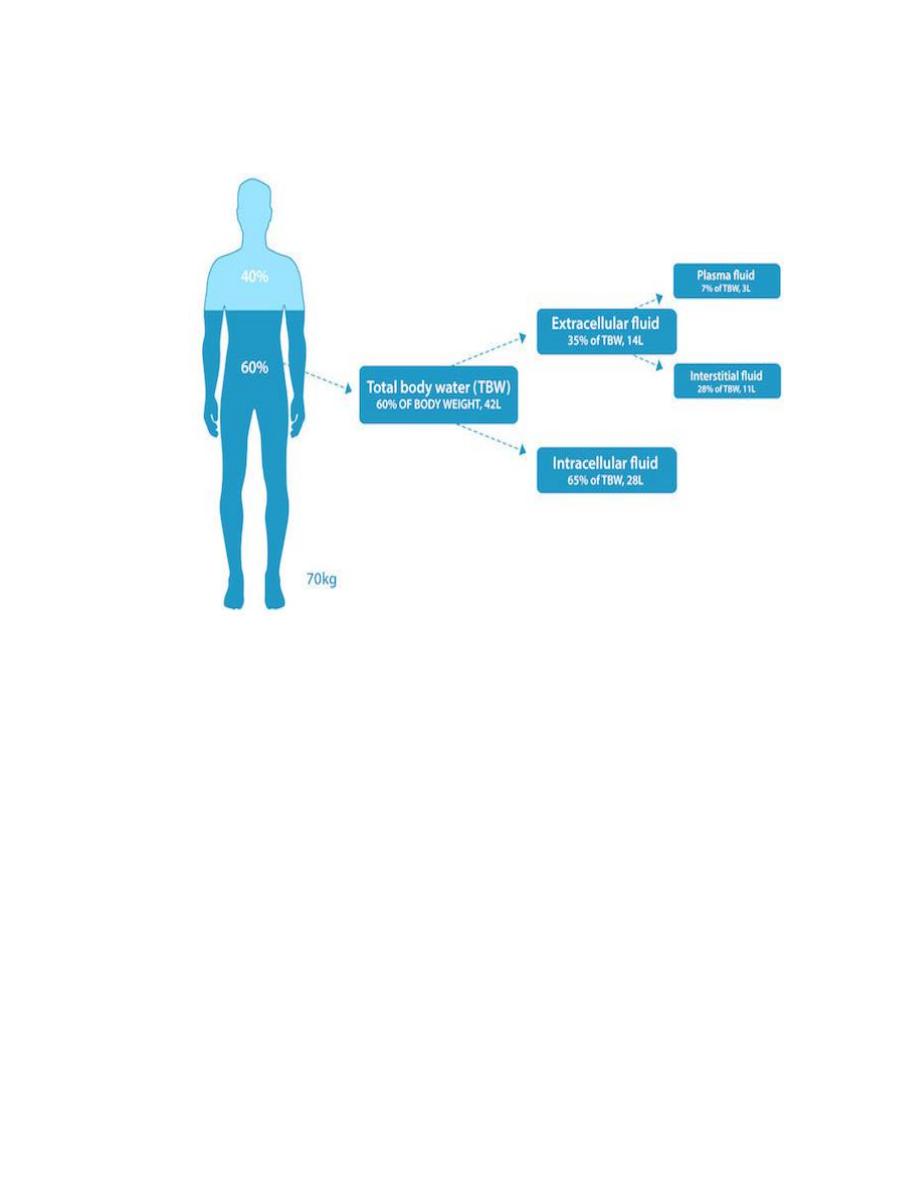
What's the tonicity of the body fluid? The normal tonicity of body fluid is
called isotonic or normotonic, the isotonic means the concentration or the
osmolarity of the solution which keeps the cell in its normal volume. one of
the major functions of the plasma membrane is to keep cell fluidity, so if we
put the cell in isotonic solution its volume will remain the same, but if we
changed the osmolarity, and that's possible just by adding a little bit of NaCl
or glucose or fatty acid to that solution we will change the osmolarity. The
normal osmolarity of plasma which is called isotonic is equal to (280-300)
milli osmole/ liter (memorize this number it’s very important).
د. راف
ع
عالوي الفياض
Body fluids physiology
كلية طب الفلوجة
2016-2017
*******************************************************************************
If we add particles to the solution, we will change that solution from
isotonic to hypertonic. Hyper means more particles so the hypertonic
solution is the solution which has more than 300 milli osmole/liter. If we put
the cell in that hypertonic solution it will be shrunken, because it will suck
the water from ICF. However, if we take particles from the solution we will
create a hypotonic solution, if we put the cell in this hypotonic solution the
cell will be swollen, because the extra water outside will enter the cell, so
more water will get inside the cell. The swelling and shrinking of the cell is
a killer change for brain & other tissues.

د. راف
ع
عالوي الفياض
Body fluids physiology
كلية طب الفلوجة
2016-2017
*******************************************************************************
That's why the medical concept called dehydration isn't acceptable in
medicine, if you have a dehydrated child for example, you should seek help
in hospitals, on the other hand if you have what's called water intoxication
which is really swelling of the whole body, it's very dangerous for the brain
and the body functions. So the target of homeostasis is to maintain the cell's
normal function and performance by keeping it in isotonic solution.
Let's take an example… If you eat a sugary meal the level of glucose in
your body will be increased in an unacceptable way because u can't burn that
glucose immediately so it will remain in your body and that is not
acceptable, the normal plasma glucose level in blood is 70 mg/dL to 99
mg/dL but that normal level changes all the time because of eating or
drinking glucose-rich foods so what happens inside our body?
There are special hormones that take the glucose and put it in the storage
places of our body to keep it away from the plasma (to keep the vital sign
which is the glucose level normal), and whenever we need that glucose we
don't have need to take it from outside sources, a signal is released telling
the stored glucose that we need it and so it is released and utilized especially
when we are hungry.
So the osmolarity of the body fluid keeps changing all the time but that
doesn’t cause a dangerous situation for the cells, how is that possible? First
of all we have 42 liters of water in our body, but every day we all take
some amount of water in by drinking and some amounts are created by

د. راف
ع
عالوي الفياض
Body fluids physiology
كلية طب الفلوجة
2016-2017
*******************************************************************************
synthesizing processes inside the body, this amount is about 2.3 liter /day
(majority of it will be taken as drinking water) but because we have 42 liters
we don't need these 2.3, they are extra because it's higher than the normal
volume so by the end of the day we will lose them back by different routes,
the main one is the urine which excrete about 1.4 liter/day of water, also
you excrete some water with feces and sweat and there is a significant
amount of water that will be lost as insensible loss of water about (500-700 )
ml/ day, that means you lose water without feeling it (in contrast you do feel
it when you sweat or urinate) you lose that insensibly whether you are
sleeping or walking or sitting, by doing so; the extra amount of water we
took per day will be lost. So, normal volume of body fluid will be
maintained.
What if we have only 40 liters of water in our body in a given day you
will not drink 2.3 liters, instead you will drink 4.3 liters, 2 liters will replace
the loss and 2.3 liters will do whatever their job is; which is washing the
internal environment, giving extra nutrition and oxygen to the tissues, taking
the waste back and washing everything inside your body.
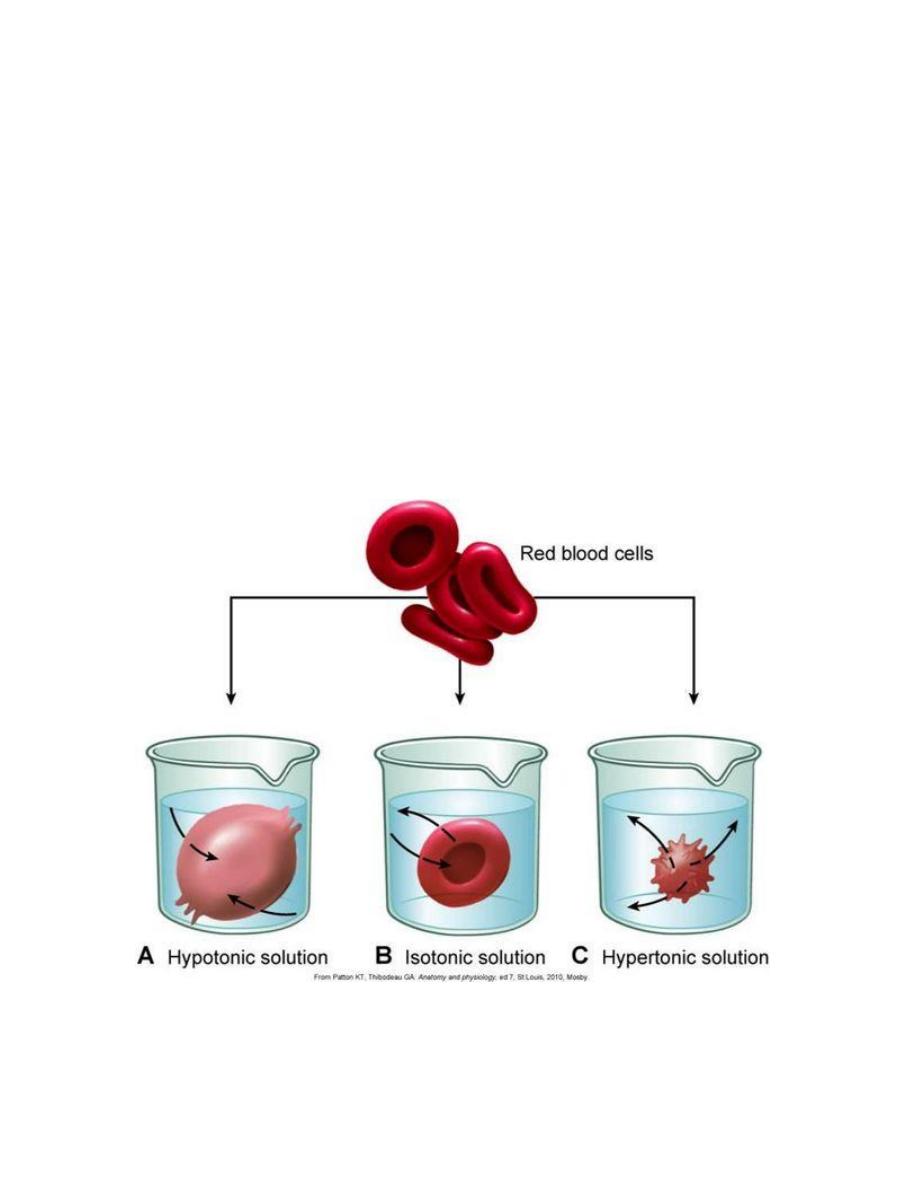
How does the intravascular and extravascular fluid communicate?
This process is called the starling capillary circulation. It means that the
plasma moves out from capillaries to interstitial compartment then
interstitial fluid move back to capillaries.
د. راف
ع
عالوي الفياض
Body fluids physiology
كلية طب الفلوجة
2016-2017
*******************************************************************************
This is a capillary (the figure) it has only one layer of endothelial cells,
but if we look carefully between those cells there are pores in which water
passes through. The more pores the vessel has the more the water can get
out, this criteria is called the permeability of the capillaries. If we compare
the permeability of capillaries with the permeability of arteries and arterioles
(it is 100 times more); so these small tiny capillaries are the end of vascular
system, and they are huge in network and their surface area is huge and the
pores in them are huge in numbers; so the flow from the plasma outside is
easy but it's not that simple.
We have a driving force that determines which way the water will go. We
have:
1- Hydrostatic pressure
2- Osmotic pressure.

د. راف
ع
عالوي الفياض
Body fluids physiology
كلية طب الفلوجة
2016-2017
*******************************************************************************
What kind of hydrostatic pressure and osmotic pressure are in the
capillaries?
Let's take a capillary, we know that there is blood pressure created by the
heart pump which pumps the blood, it will create the pressure inside the
vascular system and this pressure is the highest in the aorta, then it goes
down till it reaches almost zero. This is a capillary (look at the figure);
before the capillary we have an arteriole, this capillary is divided in two
halves: the first one is called the arterial part and the other one is the
venous part. What's the difference? There are pores all over the capillary, if
we count these in the arterial part compared to the venous part, we will find
that it's more in the venous part. So in other words, the permeability of the
venous part is higher.
when the plasma goes through these capillaries, it has a hydrostatic
pressure, if you measure the hydrostatic pressure in the capillaries in the
arterial part it is almost 30 mmHg, but if you measure the hydrostatic
pressure at the venous end of the capillary it's only 10 mmHg. Hydrostatic
pressure is a pushing force, so the pushing force of plasma located in 30
mmHg (arterial end) is higher than 10 mmHg (venous part), so if we look
carefully, this kind of pressure will force the plasma to go through these
pores outside the capillaries, so there is a force that causes the water to go
out by 30 mmHg where as in the other end the plasma will go out by force of
10 mmHg.

د. راف
ع
عالوي الفياض
Body fluids physiology
كلية طب الفلوجة
2016-2017
*******************************************************************************
There are special proteins in the plasma called plasma proteins (8% of
plasma), and when we say proteins we know that they are big particles, they
can't go through these pores, only one type of protein can go through which
is very small, only a small particle of it. Now because we have these protein
particles inside the capillaries they create osmotic pressure, if we measure
the osmotic pressure inside the capillary created by these proteins (this
pressure has a special name called (oncotic colloid pressure) if we measure
it, it is 28 mmHg osmotic pressure. This force will not push the water out it
will try to suck the water from outside; because if you look at the interstitial
compartment, it has a solution and if we look at intravascular compartment it
also has a solution, they are almost identical in composition with one
exception is that the proteins are not present in the interstitial fluid; so the
osmosis inside the capillary is more than the osmosis outside the capillary so
this 28 mmHg try to pull water back.
Some small particles of proteins can leave the capillary but not all, so
when they are out they will create an osmotic pressure outside the capillary;
the amount of osmotic pressure outside the capillary (in the interstitial fluid)
is around 8 mmHg.
However, as we said that we need to keep the plasma volume constant
in the interstitial compartment and in the intracellular fluid. So this amount
of plasma, which left the capillary to give the oxygen and nutrition to cells
and to wash this area from toxic materials, when it is close to the venous part
there is a force to suck it back, this force is equal to -7 mmHg, and we
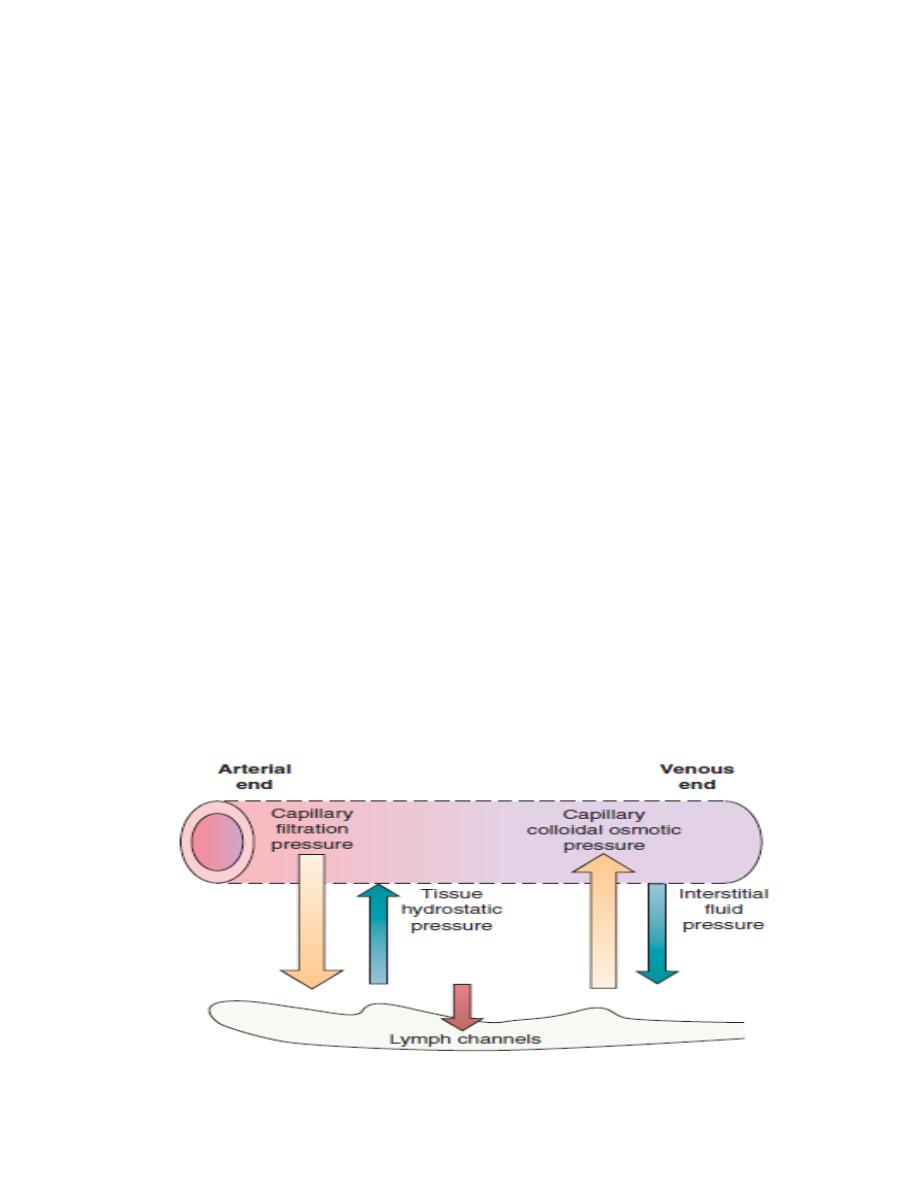
د. راف
ع
عالوي الفياض
Body fluids physiology
كلية طب الفلوجة
2016-2017
*******************************************************************************
mentioned that the permeability of the venous part is more than the arterial
part. So we don’t need the same force to get the water back in so the -7
mmHg is enough to get most of the plasma back.
There is another special structure inside the capillary circulation, in all
these capillary in your body there is special lymph structure going side by
side with capillaries. The function of this lymph vessel is not to keep any
amount of plasma accumulated in the interstitial compartment, so it will
suck it back and it will eventually return it to the plasma.
Another function of lymph vessels is that it doesn’t allow these small
particles of protein to be accumulated more and more and increase the
pressure outside capillaries, if it is more than 8 mmHg it will cause a
disaster. So this lymph vessel will take the extra water which was left from
the capillary back to the plasma circulation and it will take the extra amount
of protein which was left outside the capillary.

د. راف
ع
عالوي الفياض
Body fluids physiology
كلية طب الفلوجة
2016-2017
*******************************************************************************
Adjustment of water balance:
Under normal conditions the osmolality of the body fluids is regulated
extremely tightly to within about ± 2% of the mean plasma osmolality of
290 mosmol/kg H2O. This is achieved by adjustment of water intake by
means of the thirst center and by urinary output by means of kidney.
[1] Thirst center: It is located in the hypothalamus of the brain.
Stimulation of the thirst center can be achieved by osmoreceptor areas
located also in the hypothalamus. An increase in the electrolytes
concentration inside the neurons of osmoreceptor areas or in the allied areas
of hypothalamus (as a result of increase ECF osmolarity) stimulates thirst
center and the subject developed an intense desire to drink water until the
electrolyte concentration of the osmoreceptors center neurons return to
normal. It should be noted that if the plasma osmolality is raised by the
presence of a substance such as urea, which rapidly equilibrates between the
ECF and ICF, the osmoreceptors and consequently the thirst center are not
simulated.
The thirst center can be stimulated also by a decrease in ECF volume,
by a pathway which is independent of the osmolality of the plasma. The
effect of ECF volume depletion on thirst center is mediated in part via renin–
angiotensin system in which angiotensin II acts on a specialized receptor
area in hypothalamus to stimulate the neural areas concerned with thirst.

د. راف
ع
عالوي الفياض
Body fluids physiology
كلية طب الفلوجة
2016-2017
*******************************************************************************
The results of the stimulation of thirst center and other osmoreceptor
areas of the hypothalamus (paraventricular and suprachiasmatic nuclei of the
hypothalamus) are: (A) the creation the sensation of thirst and the desire to
drink water. (B) the stimulation of the hypothalamus to secrete ADH
(antidiuretic hormone, vasopressin) through the posterior pituitary gland.
This hormone is absorbed into the blood and acts on the collecting ducts of
the kidneys to cause massive reabsorption of water, thereby decreasing the
loss of water into the urine.
[2] Urinary output: The kidney can adjust the urinary output through
its autoregulatory mechanisms, through the activation of renin-angiotensin
system, and through the effect of ADH on the kidney.

د. راف
ع
عالوي الفياض
Body fluids physiology
كلية طب الفلوجة
2016-2017
*******************************************************************************
Clinical applications:
[A] Dehydration (volume contraction) states: They are of three types:
[1] Isosmotic dehydration: which is primarily caused by loss of
isotonic fluid from ECF compartment. It can be caused by haemorrhage,
plasma exudation through burned skin, and gastrointestinal fluid loss (as in
vomiting and diarrhea). In this type of dehydration:
ECF volume decreases while the osmolarity of the ECF is kept
constant.
Because osmolarity of ECF is unchanged, water does not shift
between the ECF and ICF compartments.
Therefore, the ICF volume and osmolarity do not change.
Arterial blood pressure is decreased.
[2] Hyperosmotic dehydration: which is primarily caused by loss
hypotonic fluid (water) from ECF compartment. It can be caused by diabetes
insipidus, diabetes mellitus, alcoholism, fever, and excessive evaporation
from skin through heavy loss of sweat (which is hypotonic). In this type of
dehydration:
ECF volume decreases while the osmolarity of ECF is increased.
Because osmolarity of ECF is decreased, water shifts from ICF to the
ECF.
As a result of this shift, ICF volume decreases while ICF osmolarity
increases until it equals the ECF osmolarity.
The plasma protein concentration is increased.

د. راف
ع
عالوي الفياض
Body fluids physiology
كلية طب الفلوجة
2016-2017
*******************************************************************************
[3] Hyposmotic dehydration: which is primarily caused by loss of
hypertonic fluid from ECF compartment. It can be caused by renal
loss of NaCl because of adrenal insufficiency as in Addison's disease.
In this type of dehydration:
The osmolarity of ECF decreases.
Consequently, water shifts from ECF to ICF.
As a result of this shift, ECF volume is decreased while the ICF
volume is increased with ICF osmolarity equals ECF osmolarity.
Plasma protein concentration increases because of the decrease in
ECF volume.
[B] Overhydration (volume expansion) states: They are of three types:
[1] Isosmotic overhydration which is primarily caused by addition of
isotonic fluid to the ECF compartment. It can be caused by any condition
that is responsible to cause edema and also can be caused by oral or
parenteral administration of large volume of isotonic NaCl (150 mmol/L). In
this type of overhydration:
The ECF volume is increased while the osmolality of the ECF is kept
constant. Because osmolarity of ECF is unchanged, water does not
shift between the ECF and ICF compartments.

د. راف
ع
عالوي الفياض
Body fluids physiology
كلية طب الفلوجة
2016-2017
*******************************************************************************
Therefore, the ICF volume and osmolarity do not change.
The plasma protein concentration is decreased because the ECF
volume is increased.
Arterial blood pressure is increased.
[2] Hyperosmotic overhydration which is primarily caused by
addition of hypertonic fluid to the ECF compartment. It can be caused by
oral or parenteral intake of large amounts of hypertonic fluid. In this type of
overhydration:
The ECF osmolarity is increased.
Consequently, water shifts from ICF to ECF.
As a result of this shift, ECF volume is increased while the ICF
volume is decreased with ICF osmolarity equals ECF osmolarity.
The plasma protein concentration is decreased because of the increase
in ECF volume.
[3] Hyposmotic overhydration which is primarily caused by addition
of hypotonic fluid to the ECF compartment. It is caused by ingestion of a
large volume of water or renal retention of water due to the syndrome of
inappropriate antidiuretic hormone secretion (SIADH). In this type of
overhydration:
The volume of ECF increases because of water retention while ECF
osmolarity is decreased.
Consequently, water shifts from ECF to ICF.
As a result of this shift, ICF volume increases and ICF osmolarity
decreases until it equals ECF osmolarity.
د. راف
ع
عالوي الفياض
Body fluids physiology
كلية طب الفلوجة
2016-2017
*******************************************************************************
The plasma protein concentration decreases because of the increase in
ECF volume.
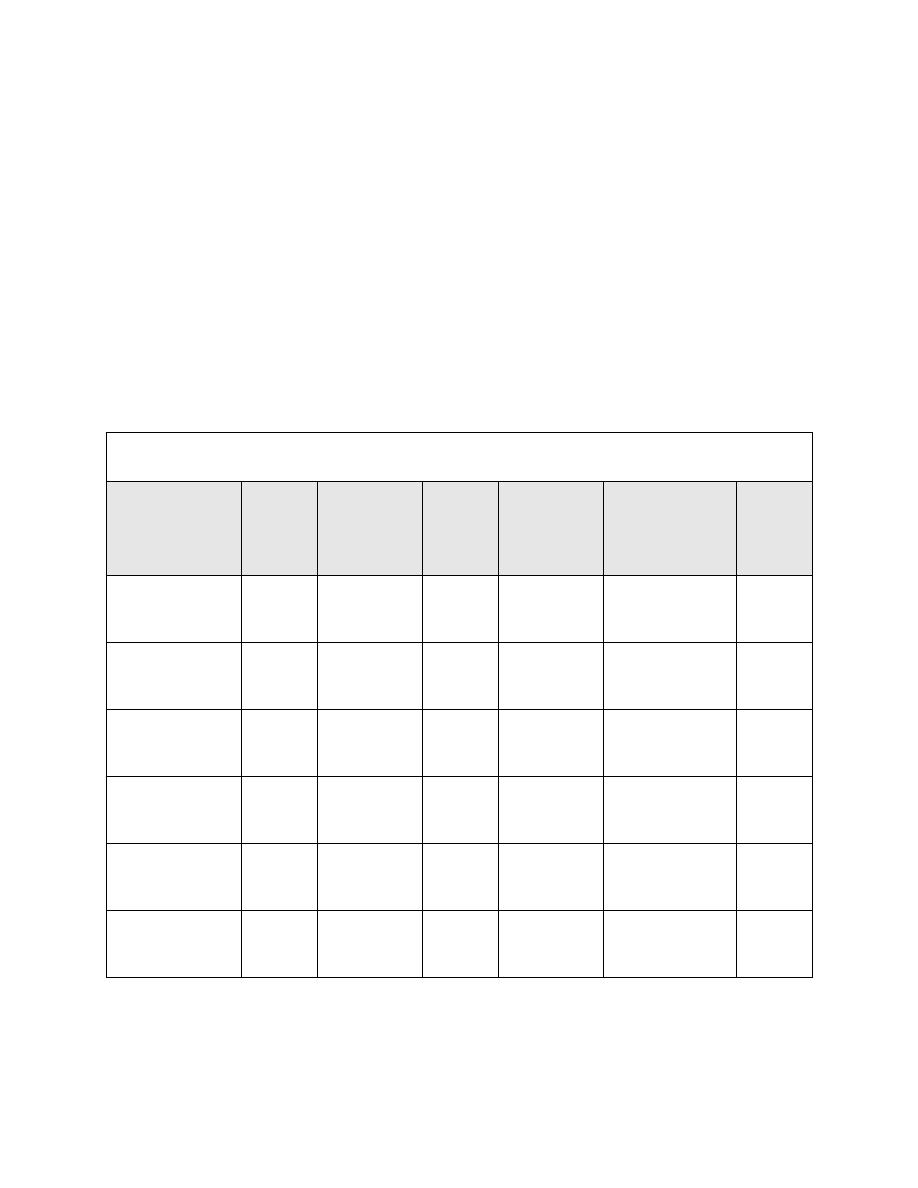
Changes in volume and osmolarity of body fluids
Type
ECF
volume
ECF
osmolarity
ICF
volume
ICF
osmolarity
Plasma
protein
concentration
ECF
[Na]
Isosmotic
dehydration
↓ =
=
=
↑
=
Hyperosmotic
dehydration
↓
↑
↓
↑
↑
↑
Hyposmotic
dehydration
↓
↓
↑
↓
↑
↓
Isosmotic
overhydration
↑
=
=
=
↓
=
Hyperosmotic
overhydration
↑
↑
↓
↑
↓
↑
Hyposmotic
overhydration
↑
↓
↑
↓
↓
↓
