Urinary System
I. Main Kidney Functions:Regulation of plasma volume (contributes to blood pressure)
Regulation of osmolarity of body fluids and maintenance of ion balance (Na+, K+, etc) in the ECF (integrates with behavioral drives such as thirst)
Regulation of plasma pH. If ECF too acidic, kidneys remove H+ and conserve bicarbonate ions. If too alkaline, kidneys remove bicarbonate ions and conserve H+. Kidneys play a significant role but do not correct disturbances as rapidly as lungs.
Production of hormones:
Kidneys synthesize erythropoietin (EPO)
Kidneys secrete renin, an enzyme that regulates production of hormones involved in sodium balance and blood pressure homeostasis
Renal enzymes help convert vitamin D3 into a hormone that regulates CA++ balance.
Filters blood separating metabolic wastes (urea, creatinine, etc. and foreign substances from blood plasma and provides means to eliminate these wastes from body forms urine as a side effect
urine;
a. Clear to pale yellow fluid (depending on its concentration).b. Volume varies with fluid intake and with fluid output via other routes.
c. pH is usually 6, slightly acidic. Normal range is 4.5 to 8 and varies with diet.
d. 95% water.
e. Solutes (5%) include: uric acid (a metabolite of nucleic acids), creatinine (metabolite of creatine, a chemical used by skeletal muscle for energy storage), and urea (an end product of protein metabolism), ions such as Na+, K+, Ca2+, Mg+ and HCO3-).
f. pigments and excess drugs, hormones, toxins, Without this filtering toxic substances accumulate in the body death
Urine Formation Rate:
Normal 1 ml/min (1.5 L/day)
Normal range 0.4-2 ml/min (0.5-3 L/day)
II. Fluid/Electrolyte Homeostasis
A. Fluid CompartmentsExtracellular fluid compartments (about 1/3 of all body fluids)
Interstitial fluid—fluid between cells
Plasma—fluid portion of blood
Lymph—fluid in lymph nodes and vessels
Other: CSF, joint fluid, eyeball fluid, etc.
Intracellular fluid compartment (2/3 of all body fluids)—includes cytosol of all cells
Water constitutes average of 60% of body weight but ranges from 40-80% depending on age and amount of adipose tissue
B. Fluid Homeostasis
Balance maintained for good health, must have certain amount of water to maintain proper blood pressure and blood volumeExcesses or deficiencies of fluids in one tissue are “moved around” or “rationed” among other tissues by plasma
No tissue is very far out of balance (under or overhydrated)
Overall input and output of water to and from body can be adjusted (thirst mechanism, respiratory loss, sweating—output can be adjusted by changing volume of urine)
Fluid Balance regulated by vasopressin and thirst. Hypothalamus osmo-receptors trigger thirst and monitor ECF osmolarity and vascular fullness.
C. Electrolyte homeostasis
Electrolytes dissociate to form ions when dissolved in water
Distribution of various electrolytes differs between the intracellular fluid and ECF
Cellular mechanisms of electrolytes balance=sodium-potassium pump, calcium pump, other ion pumps
Extracellular mechanism of electrolytes balance: urinary system
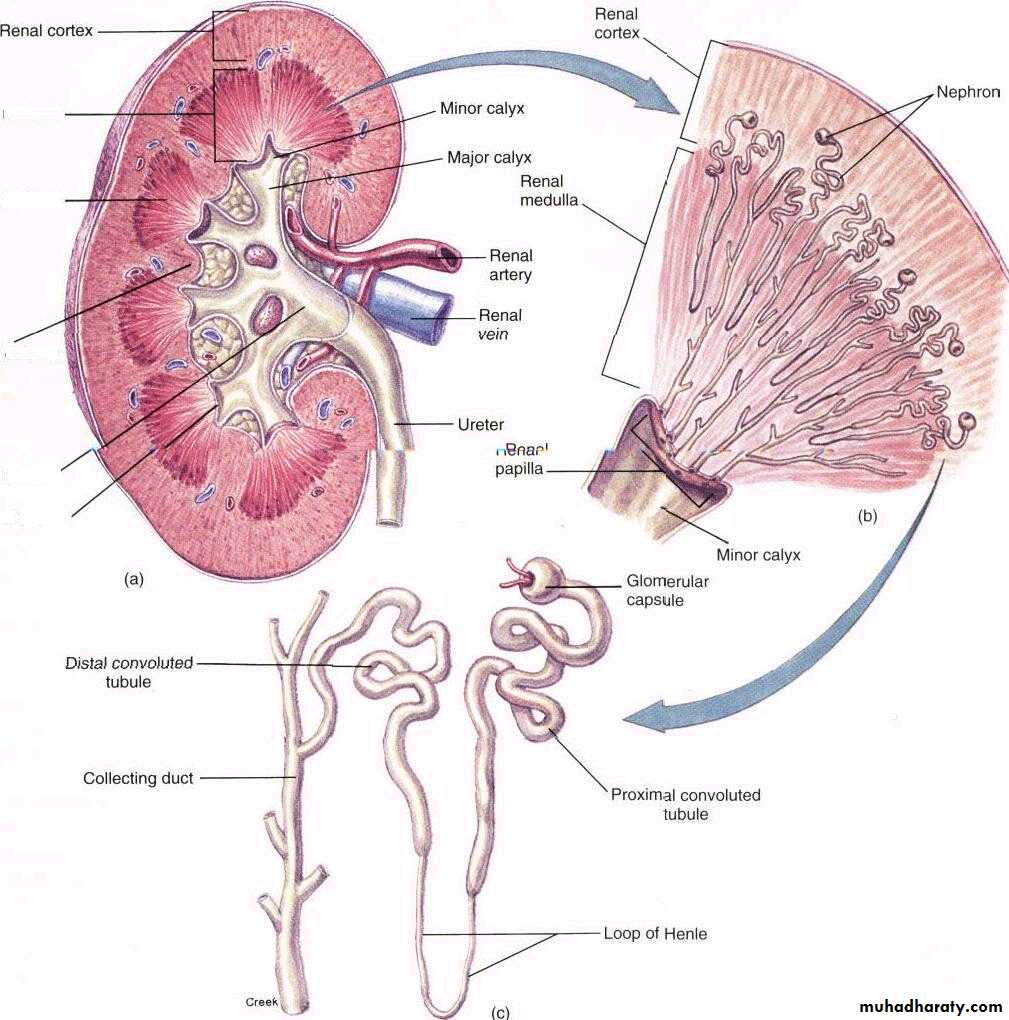
III. Anatomy of Urinary System
Kidneys
Bean-shaped paired organs covered with fibrous capsule
Interior of kidney has 2 layers: Renal cortex& Renal Medulla
Renal pyramids; cone-shaped pieces of tissue that point toward medial opening of kidney
Renal Papillae; Tips of pyramids with tiny openings for release of urine from pyramids
Renal columns; Tissue between pyramids
Urine from renal papillae empties into cuplike depression called minor calyx—unite to form major calyx.
Major calyces unite to form funnel-shaped basin called Renal Pelvis (hollow, innermost chamber of kidney)
Renal pyramid
Renal Medulla
Renal Column
Renal Pelvis
Renal Papilla
Ureters
Tube from each kidney that drains urine from pelvis of kidney to the urinary bladderSmooth muscle in wall with mucous lining
Peristalsis pumps urine away from kidney
Urinary Bladder
Stores urine until acceptable time and place to urinateIs a hollow sac lined with epithelium capable of stretching greatly
Capacity: 500ml
Detrusor muscle—generates APs in response to stretch
Urethra
Single tube continuous with neck of bladder which drains urine from bladder to outside of bodyMicturition Reflex— The process of urination –spinal reflex subject to both conscious and unconscious control from higher brain centers;
a. As >200mL of urine accumulates in the bladder, the bladder wall stretches.
b. Stretch receptors sense the stretch and signal the micturition center in the pons.
c. They also initiate a reflex response in the spinal cord resulting in increased parasympathetic outflow to the bladder.
d. It causes opening of the internal urethral sphincter and contraction of the detrusor muscle.
e. At this point, somatic activation of the external urethral sphincter can prevent urination.
f. If the external urethral sphincter is voluntarily contracted, the reflex contractions of the bladder will fall down.
g. When volume and stretch become too great, signals from the pons inhibit any motor output to the external urethral sphincter and urination arise.
Overview of Nephron Structure and Urinary Physiology
Nephrons; functional units of kidneys—responsible for formation of urineBulk of kidneys made ups of these hollow tubules (over 1 million per kidney)
Site of urine production
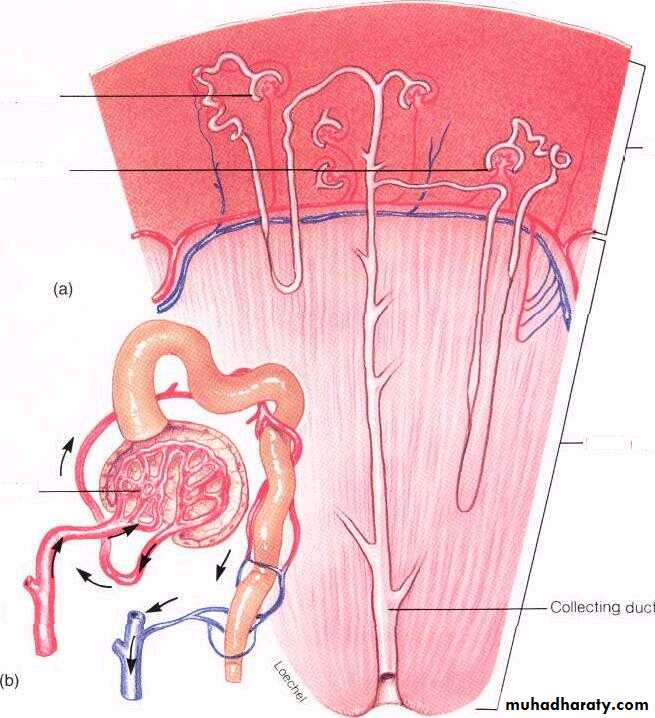
Most (80%) are contained within the cortex, about 20% dip down into medulla
Each nephron consists of tubules and associated blood vessels
Collecting duct
Cortical nephron
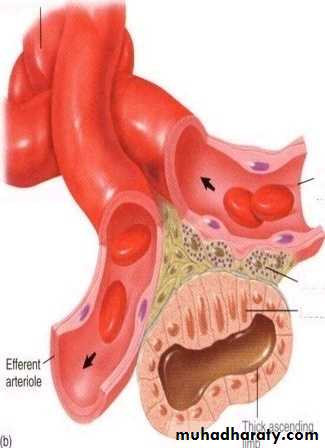
Juxtamedullary nephronEfferent arteriole
Afferent arteriole
medulla
cortex
Blood Supply to Nephron
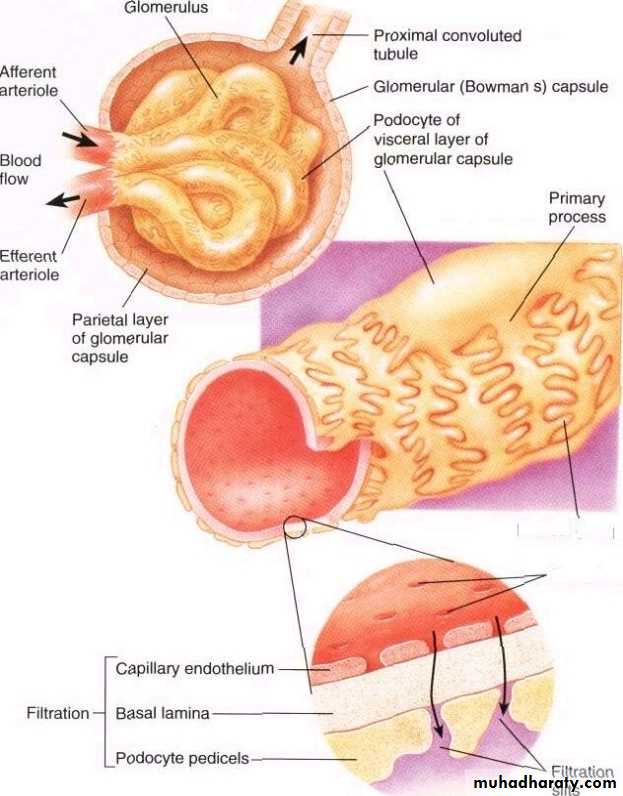
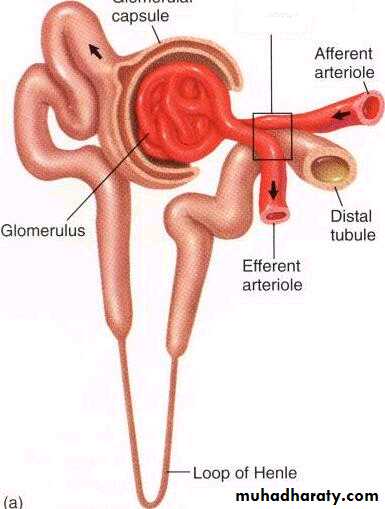
Blood flows from aorta renal artery branches (eventually) into afferent arteriole glomerulusGlomerulus = a ball-like network of blood capillaries filters water and solute from blood producing blood filtrate that enters urinary tubules
Blood leaves the glomerulus by the efferent arteriole which subdivides into a series of peritubular capillaries which surround renal tubules capillaries eventually form veins exits kidney through renal vein inferior vena cava
Other elements of Nephron
Bowman’s capsule or glomerular capsule; completely surrounds glomerulus and receives fluid that is filtered out of glomerulus. Glomerular capsule and its glomerulus make up the Renal Corpuscle.Tubular elements include: Renal tubules; Take fluid from the glomerular capsule and ends at the tip of the medullary pyramid
Glomerulus
Glomerular capsule
Efferent arteriole
Afferent arteriol
Interlobular artery
Proximal convoluted tubule
Arcuate artery& vein
Interlobular artery&vein
Distal convoluted tubuleInterlobular vein
collecting ductFour major regions:
i. Proximal convoluted tubule (PCT)Close to beginning of nephron
Highly coiled tubule extending from glomerular capsule
Contains millions of microvilli
Contains abundant mitochondria In renal cortex
ii. Nephron loop or loop of Henle
formed when the PCT straightens out and makes a hairpin loop (like a U) dipping down into medullaloops from cortex medulla cortex
iii. Distal convoluted tubule (DCT)
Drains filtrate from nephron loop
Shorter than proximal tubules and few microvilli
formed when the nephron loop returns to the cortex and winds and twists again before emptying into collecting tubule
iv. Collecting tubule or Collecting Ducts
collect urine from up to 8 different distal convoluted tubulesurine flows down the collecting tubule into calyces in the kidney to renal pelvis out the kidney through the ureter
V. Nephron function;
3 Essential Processes: 1.filtration 2. Reabsorption 3. Secretion1. Glomerular filtration
General process; passive, nonselective process in which pressure forces fluids and solutes through a membrane
High pressure in the glomerular capillaries is due to the larger diameter of the afferent arteriole compared to the efferent arteriole
Afferent arteriole carries unfiltered blood to the glomerulus (one afferent arteriole per nephron)
Glomerulus very porous (fenestrated) and very permeable to water and solutes allowing these small molecules to filter into glomerular capsule; however, blood cells normally are too big to fit through the holes
Molecules that leave blood and enter glomerular capillaries; called the glomerular filtrate and contains everything the blood contains except larger plasma proteins and RBCs
Failure to restore fluids to blood would cause death from loss of water, nutrients
Filtration pressure forces the fluids from the glomerulus into the glomerular capsule
Blood pressure, osmotic pressure, and the pressure of fluids within the Bowman’s capsule can all influence the direction of fluid movement; generally, the NET filtration pressure moves fluids from the glomerulus into Bowman’s capsule
Podocyte
Cell body
Primary process of podocyte
Branching processFiltration rate
Glomerular filtration rate ( GFR ); how much filtrate your kidneys produce each minute. The GFR averages 115 ml per minute in women and 125 ml per minute in men. This is equivalent to 7.5 L per hour or 180 L per day, since the total blood volume averages about 5.5 L, this means that the total blood volume is filtered into the urinary tubules every 40 minutes.Although typically constant, GFR can change with changing blood pressure
If blood pressure drops afferent and efferent vessels adapt (vasoconstriction or dilation) so as to increase/maintain blood flow to glomerulus
Changes in the diameter of the afferent arterioles result from both;
1. Extrinsic (sympathetic) innervation. (fight-or-flight reaction)
2. Intrinsic regulatory mechanisms (Autoregulation);
effects of locally produced chemicals on the afferent arterioles, effects on the efferent arterioles are believed to be of secondary importance).
Autoregulation is also achieved through; A negative feedback between afferent arteriole and volume of filtrate. When macula densa senses an increased flow of filtrate, it signals the afferent arterioles to constrict. This lowers the GFR, thereby decreasing the formation of filtrate in a process called tubuloglomerular feedback.
Juxtaglomerular apparatus—specialized vascular cells and specialized tubular cells called the macula densa at a point where distal tubule passes through fork formed by afferent and efferent arterioles of the same nephron.
Macula densa cells sense flow and release hormones that affect afferent arteriole diameter.
juxtaglomerular apparatus
sGlomerulous
Region of juxtaglomerular apparatus
Afferent arteriole
Granular cellMaculadensa
Glomerular Filtration is Easy to Measure From Inulin or Creatinine Clearance:
It is relatively easy to measure the GFR and it is a good way of assessing kidney functionConsider a substance, "A" which is only filtered by the kidney; it is neither reabsorbed nor secreteted:
Since no "A" is reabsorbed from or secreted into the tubule, the amount filtered into the tubule at the glomerulus must equal the amount appearing in the urine
P X GFR = U X V
P = plasma concentration of "A" in mg/mL
GFR = glomerular filtration rate of plasma, in mL/min
U = urine concentration of "A" in mg/mL
V = rate of urine production in, in mL/min
Solving the equation for GFR will give:
GFR = (U X V)/P
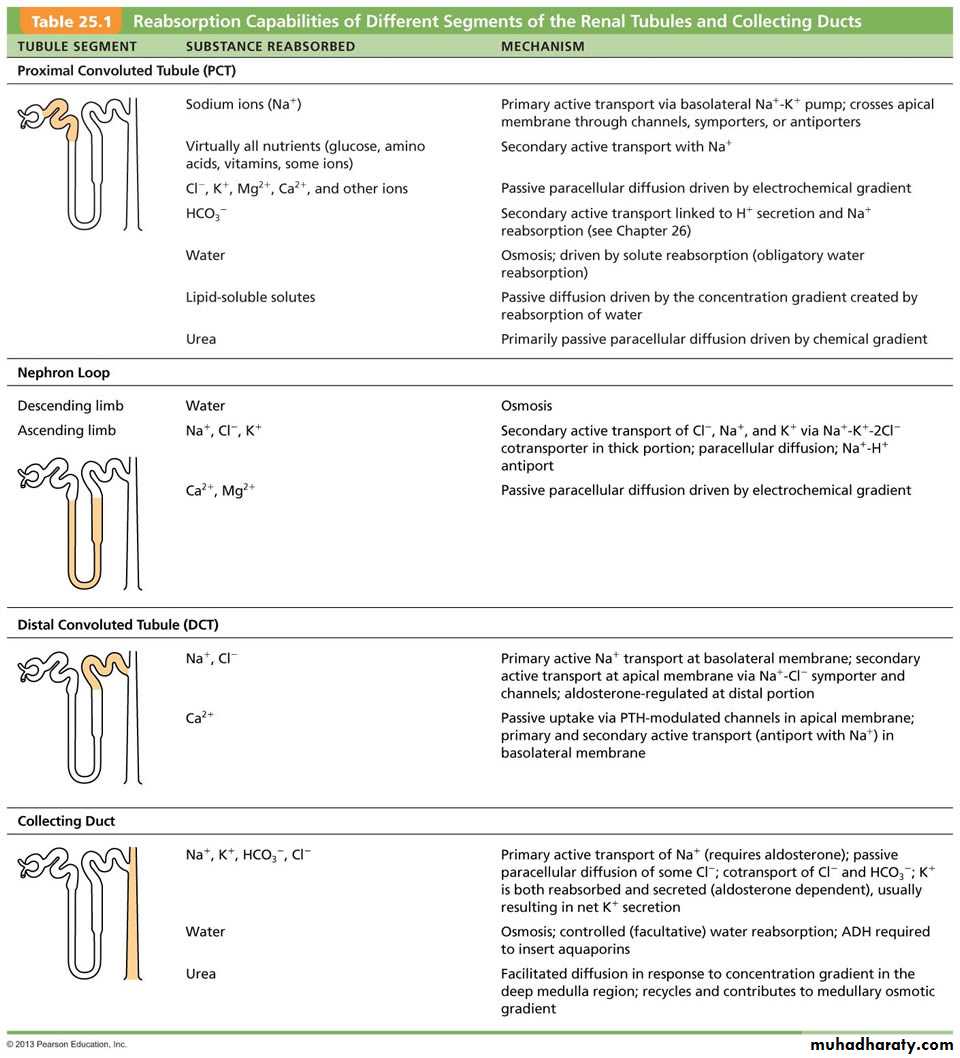
2. Reabsorption and 3. Secretion
Reabsorption ; selected materials of value to the body are removed from tubular filtrate and passed back into the blood 99% of the filtrate is returned to the body.
Secretion ; transport of solutes from plasma directly into the tubular fluid to dispose of substances not already in filtrate (drugs), to eliminate undesirable substances that have been reabsorbed, controlling blood pH, to rid body of excess K+
Tubular Reabsorption Has a Maximum Rate:
Most of the solutes filtered into the tubule are reabsorbed because they are too valuable to throw away (glucose& amino acids).1- In many cases reabsorption is by active transport, requiring ATP
Example of active transport: Na, K pump:
Most of the filtered Na is reabsorbed by the Na pump in the proximal tubule (~65%)
Na pumping in the ascending loop of Henle sets of osmotic gradients that are used to regulate water (~25%)
Fine tuning of Na is done by Na pumps in the distal tubule and collecting duct, which are controlled by the hormone, aldosterone
2-Some reabsorption is by secondary active transport- the flows are indirectly coupled to the active transport of another substance (such as Na) Example of secondary active transport: Glucose reabsorption The proximal tubule has a mechanism for cotransport of Na & glucose
The kidneys ''maximum capacity'' for reabsorption of a substance is the transport maximum( Tm ), or renal threshold.
e.g. normal blood glucose level is 2.5 to 5.3 mmol/1 (45 to 95 mg/100 ml).
If the level rises above the transport maximum of about 9 mmol/1 (160 mg/100 ml) glucose appears in the urine (Glycousuria) because all the carrier sites are occupied and the mechanism for active transfer out of the tubules is overloaded.
When that occurs, some glucose will be excreted into the urine (glucosuria) diabetes mellitus.
Note: small amounts of glucose may spill into the urine when plasma concentrations of glucose are low. This occurs because some of the nephrons have lower tubular maximum rates than others.
Maximum transport rate is limited by the number of pump or carrier molecules in the cell membrane
VI. Functions of Renal Tubules
A. PCTReabsorbs organic nutrients
Primary spot for reabsorption of water (60-70%)
The peritubular capillaries are directly adjacent to the PCT easier for transport/exchange of materials
Na+ is actively transported; sometimes is actively transported with organic nutrients (i.e. glucose) into blood stream. Chloride follows the Na+ passively by electrical attraction and water follows passively.
Glucose must have carrier
Net effect: increase in NaCl concentration of interstitial fluid and the blood plasma of the peritubular capillaries. This change in the osmolarity of the blood in the peritubular capillaries water flows into the peritubular capillaries due to osmosis because walls of proximal tubules are permeable to water.
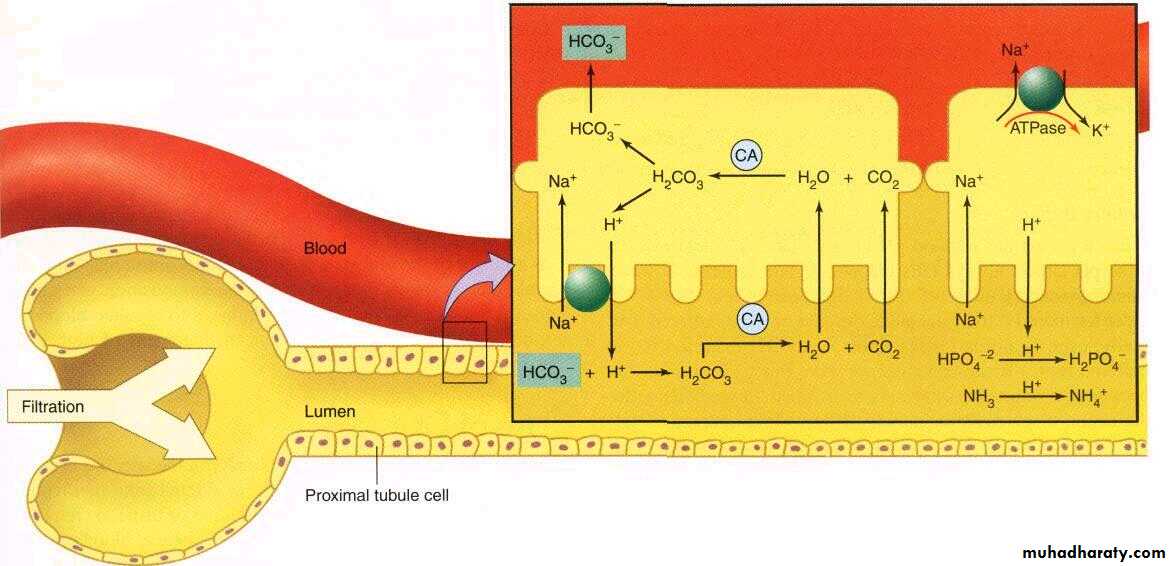
pH adjustment (H+ secretion)
About half of the urea is reabsorbed passively here
As solute in the PCT enters the loop, it is more concentrated (i.e has more solutes like urea and less water)
About 65% of Glomerular filtrate is reabsorbed in PT
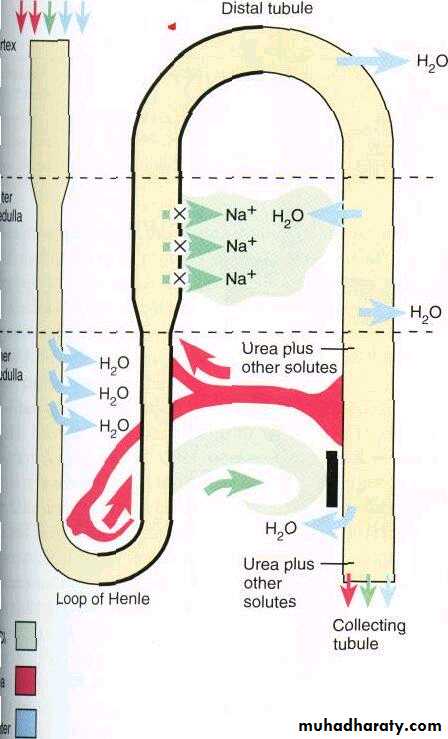
B. Loop of Henle
Reabsorption is still occurring here; products are going from the lumen to the blood—not as permeable as PCT
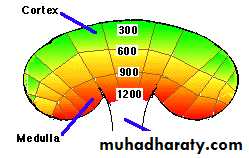
Medulla maintained at high osmolality (most body fluids isotonic at 300), Medullar about 1200-1400
Thin descending region very permeable to water
Thick ascending loop—impermeable to water
Peritubular capillaries (vasta recta) surround the loop—remove water and concentrate solutes in interstitial fluid of renal medulla
Salt (NaCL) passively diffuses out of lower portion of ascending limb but actively pumped out into interstitial fluid by thicker portion of ascending limb
Countercurrent mechanism; refers to inter-actions between the descending and ascending limbs, decreasing water concentration in descending limb encounters an increasing solute concentration → fluid flowing in opposite directions right alongside each other, (multiplies the concentration of interstitial fluid of renal medulla, very high at deepest part of medulla)
urea exiting from collecting duct adds to high osmolality (and re-enters ascending limb)
C. DCT and Collecting Duct
Both reabsorption and secretion occur here
Secretion is typically an active process (takes energy)
Products secreted from the blood into the tubular fluid include K+ and H+
by the time the tubular fluid reaches the distal convoluted tubule (DCT) the fluid is usually hypotonic to the interstitial fluids
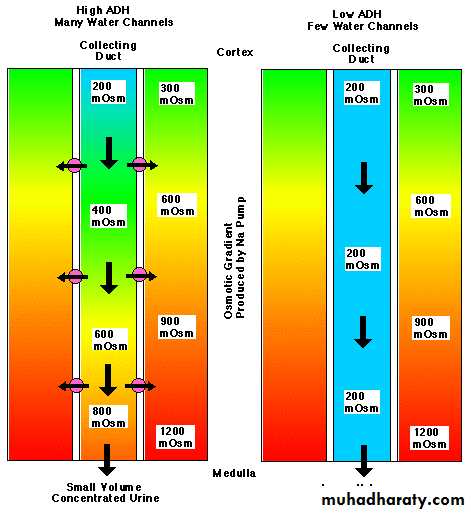
Water would normally flow from the DCT into the interstitial fluid, adjusted by hormones depending on how much water body needs to save or get rid of
the DCT are impermeable to water under normal conditions
Reabsorption of more water depends on presence of vasopressin (also called ADH or antidiuretic hormone) makes walls become permeable and water leaves the DCT, so ADH causes adjustment in final osmolarity of urine, depends of how much water the body needs to conserve or get rid of
(Vasopressin called so because it raises blood pressure when present at high concentrations; in the physiological range of concentrations, its main action is on water permeability)
Role of Urea
1. Urea trapping
a. medullary collecting duct: Some (but not all) of the urea in the collecting duct fluid is reabsorbed by passive diffusion into the interstitial fluid.
b. loop of Henle: The high interstitial concentration of urea causes some of the interstitial urea to enter the lumen of the loop. This urea is carried to the medullary collecting duct, where it again diffuses into the interstitial fluid. This process results in a high concentration of urea in the medulla
2. The urea that is not trapped is excreted in the urine
This determines whether or not your urine is dilute or concentrated with respect to water
Aldosterone;
a. Produced by the adrenal medulla.b. Acts to increase sodium reabsorption in the DCT and CD. This causes an increase in water reabsorption.
c. Also increases the secretion of potassium in the DCT.
d. The release of aldosterone is stimulated by:
i. Low plasma Na+ levels
ii. High plasma K+ levels
iii. Low blood volume and pressure.
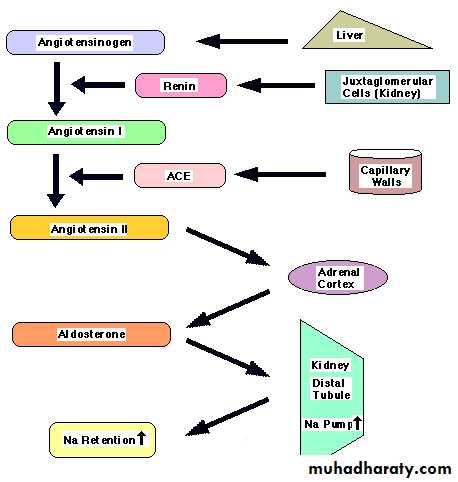
Renin-angiotensin-aldosterone system: multistep pathway for maintaining blood pressure.
renin-angiotensin mechanism;
a. Granular cells of the afferent arteriole release large amounts of the enzyme renin when:
i. BP drops (as measured by the stretch of the afferent arteriole)
ii. Stimulated by sympathetic nerve fibers (via NE).
b. Renin cleaves the plasma protein angiotensinogen (made by the liver) into a compound called angiotensin I.
c. Angiotensin I is converted to angiotensin II by the Angiotensin-Converting-Enzyme (ACE) (primarily released by pulmonary capillary endothelial cells).
d. Ag II is a vasoconstrictor so it increases resistance and thus increases BP.
e. AgII will stimulate the release of the hormone aldosterone from the adrenal cortex.
i. Aldosterone will increase the renal retention of water. This will help maintain blood volume (and thus BP).
f. AgII also prompts the pituitary to release antidiuretic hormone (ADH), which will also increase the renal retention of water.
g. AgII also promotes thirst which will maintain blood volume (and thus BP).
Mechanism of ADH;
ADH binds to collecting duct ADH receptorscausing an increase in water permeability by inducing water channels (aquaporins) stored in intracellular vesicles to fuse with the luminal membrane (major effect)
Note: The effect on water permeability is graded → the higher the ADH concentration, the more receptor sites occupied, and the greater the water permeability (up to the maximum effect)
ADH has rapid action and rapid turnover (10-20 minutes)
Example: Drink pure water??
pure ==> plasma ↓ ==> osmoreceptors ↓ ==> ADH ↓ ==> urine volume ↑ ==> plasma osmolality ↑
H2O osmolality discharge rate release urine concentration ↓ (to normal)
Example: Eat salt???
NaCl ==> plasma ↑ ==> osmoreceptor ↑ ==> ADH ↑ ==> urine volume ↓ ==> plasma osmolality↓ingest osmolality discharge rate release urine concentration ↑ (to normal)
Note: Similar homeostatic responses to dehydration (defense of fluid volume) or severe hypotension
ANH (atrial natriuretic hormone)—produced by atria of heart when cardiac cells stretch.
Blood pressure rises, releases ANH to inhibit renin secretion and release of ADH decreases blood volume and pressure
Regulation of body potassium levels is essential to health due to its effect on excitable tissues such as heart, nerve, muscle, important in RMP of all cells. Aldosterone plays critical role. K+ balance closely tied to acid-base balance
VII. Acid-Base Balance (pH homeostasis)
Acids liberate H+ ions into solutionbases bind with free H+ and remove them from solution
Hydrogen ion concentration expressed in terms of pH
Kidneys are most powerful regulator of pH
By secreting H+
Indirectly by changing rate at which HCO3 buffer is reabsorbed or excreted
In order to maintain the normal pH (acid-base balance) of the blood, the cells of the proximal convoluted tubules secrete hydrogen ions in the filtrate, they combine with buffers;
• Bicarbonate, forming carbonic acid (H+ + HCO3- H2CO3)
• Ammonia, forming ammonium ions (H+ + NH3 NH4+)
•Hydrogen phosphate, forming dihydrogen phosphate(H++HPO42- H2PO4).
Carbonic acid is converted to carbon dioxide (CO2) and water (H2O), and the CO2 is reabsorbed maintaining the buffering capacity of the blood.
Hydrogen ions are excreted in the urine as ammonium salts and hydrogen phosphate.
The normal pH of urine varies from 4.5 to 7.8 depending on diet, time of day and a number of other factors.
Individuals whose diet contains a large amount of animal proteins tend to produce more acidic urine (lower pH) than vegetarians do.
VII. Urinary System Disorders
1. Dysuria; difficulty or pain in urination. Possibly from kidney or bladder stones caused by “precipitation” of chemicals in the urine to form crystals2. Polyuria; frequent urination
3. Nocturnal enuresis; bed-wetting—vasopression (hormone that decreases
urine production) secretion does not increase at night as it should
Diabetes insipidus :
A disease associated with the inadequate secretion or action of ADH.
Without proper ADH secretion or action, the collecting ducts are not very permeable to water, and so a large volume (5 to 10 L / day) of dilute urine is produced.
The dehydration that results causes severe thirst.
Diuretics
a. Chemicals that enhance urine output.
b. An osmotic diuretic is a substance that is filtered but not reabsorbed. It will increase the osmolality of the filtrate and prevent water from flowing out.
c. Alcohol is a diuretic ,it inhibits pituitary ADH release.
d. Caffeine is a diuretic , it inhibits renal sodium reabsorption.