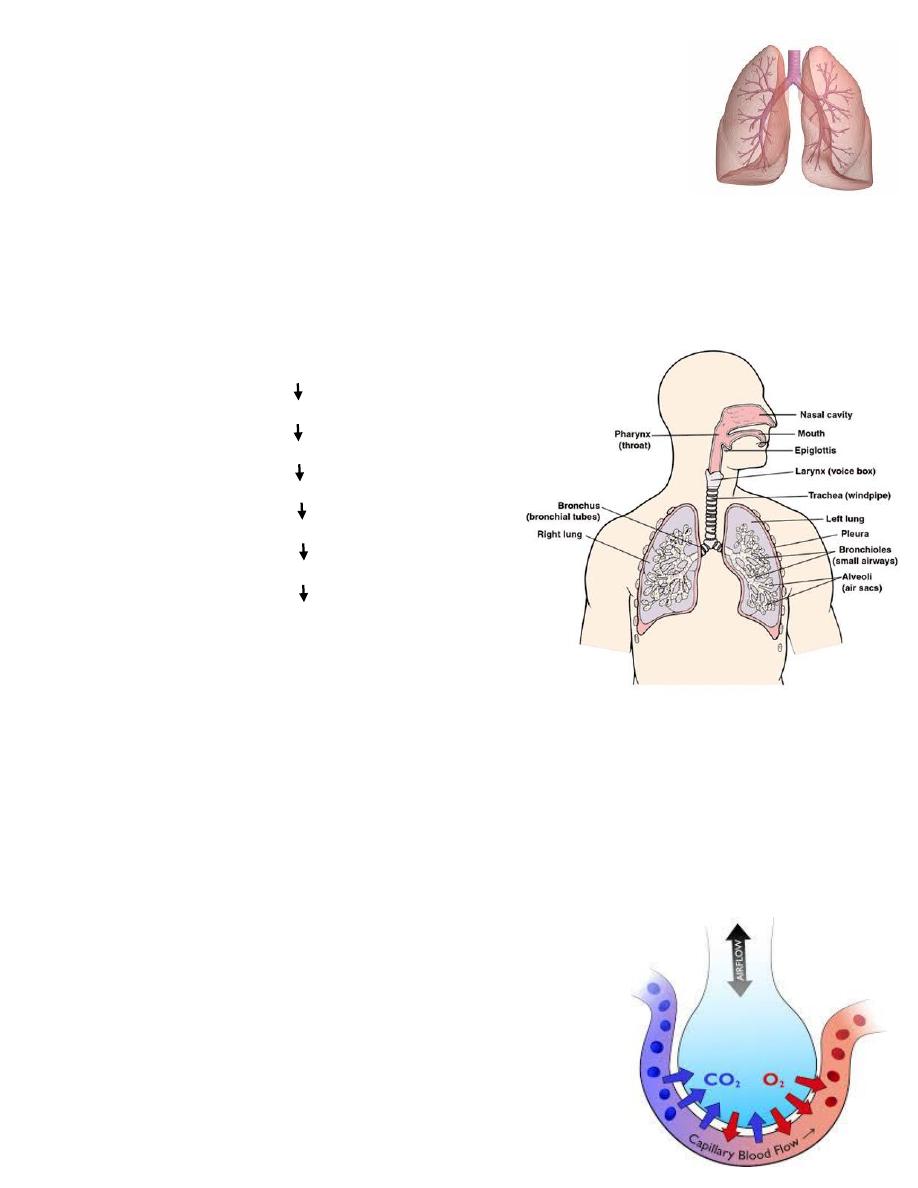
Figure: Gas exchange in an alveoli
Respiratory system (Respiratory rate and volumes)
Introduction
- The three main functions of respiratory system are:
- Supplies with O
2
- Helps to maintain the pH of the blood plasma
- Takes important role in the regulation of body temperature
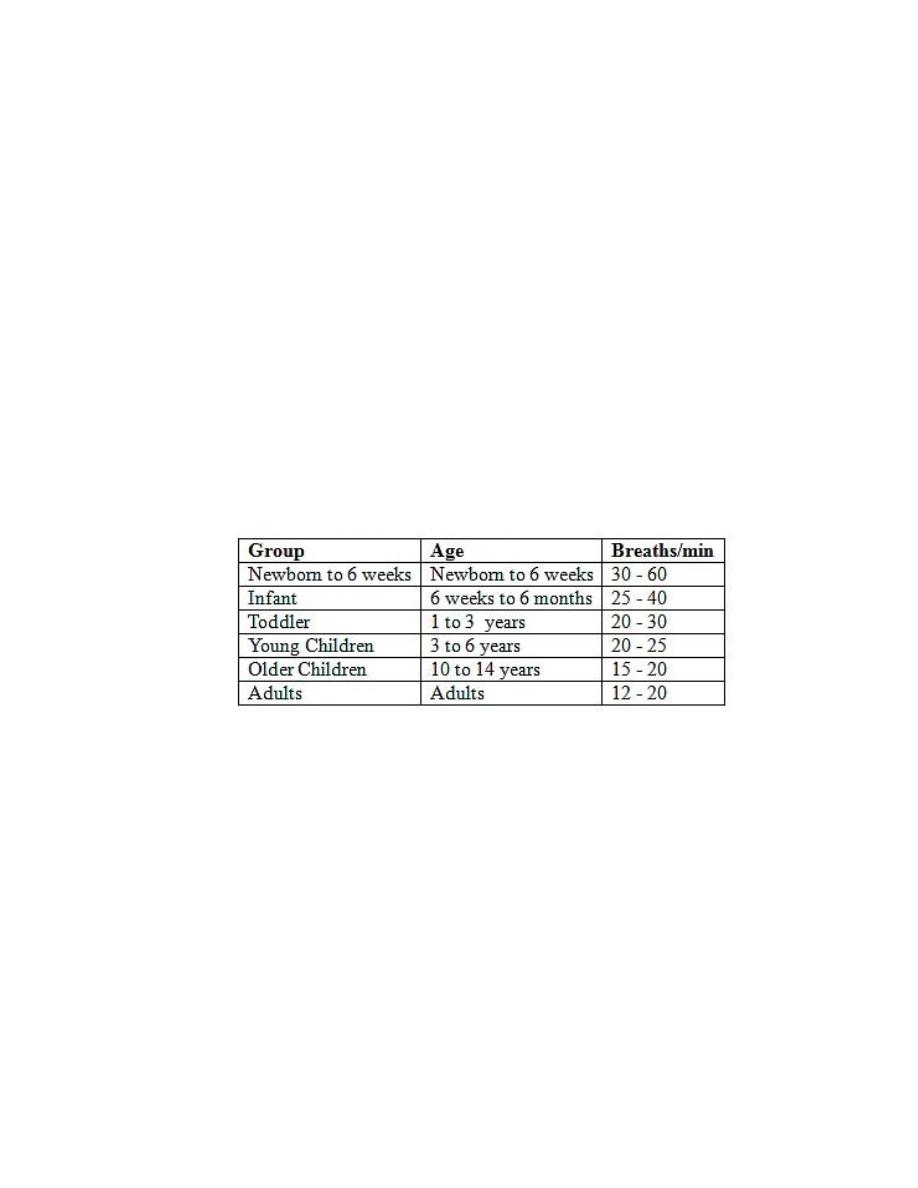
- Pathway of air: nasal cavities (or oral cavity)
Pharynx
Larynx
Trachea
Bronchi
Bronchioles
Alveoli (site of gas exchange)
The exchange of gases (O
2
& CO
2
) between the alveoli & the blood occurs by simple
diffusion:
- O
2
diffusing from the alveoli into the blood & CO
2
from the blood into the
alveoli. Diffusion requires a concentration gradient.
So, the concentration (or pressure) of O
2
in the alveoli must be kept at a higher
level than in the blood
& the concentration (or pressure) of CO
2
in the alveoli must be kept at a lower
level than in the blood.
Respiratory rate
The number of breaths per minute (the number of inspiration and expiration
together per minute)
Measured by counting the number of times the chest rises or falls (breath) per
minute
The aim of measuring respiratory rate is to determine whether the respirations
are: - normal,
- abnormally fast (tachypnea),
- abnormally slow (bradypnea), or
- nonexistent (apnea).
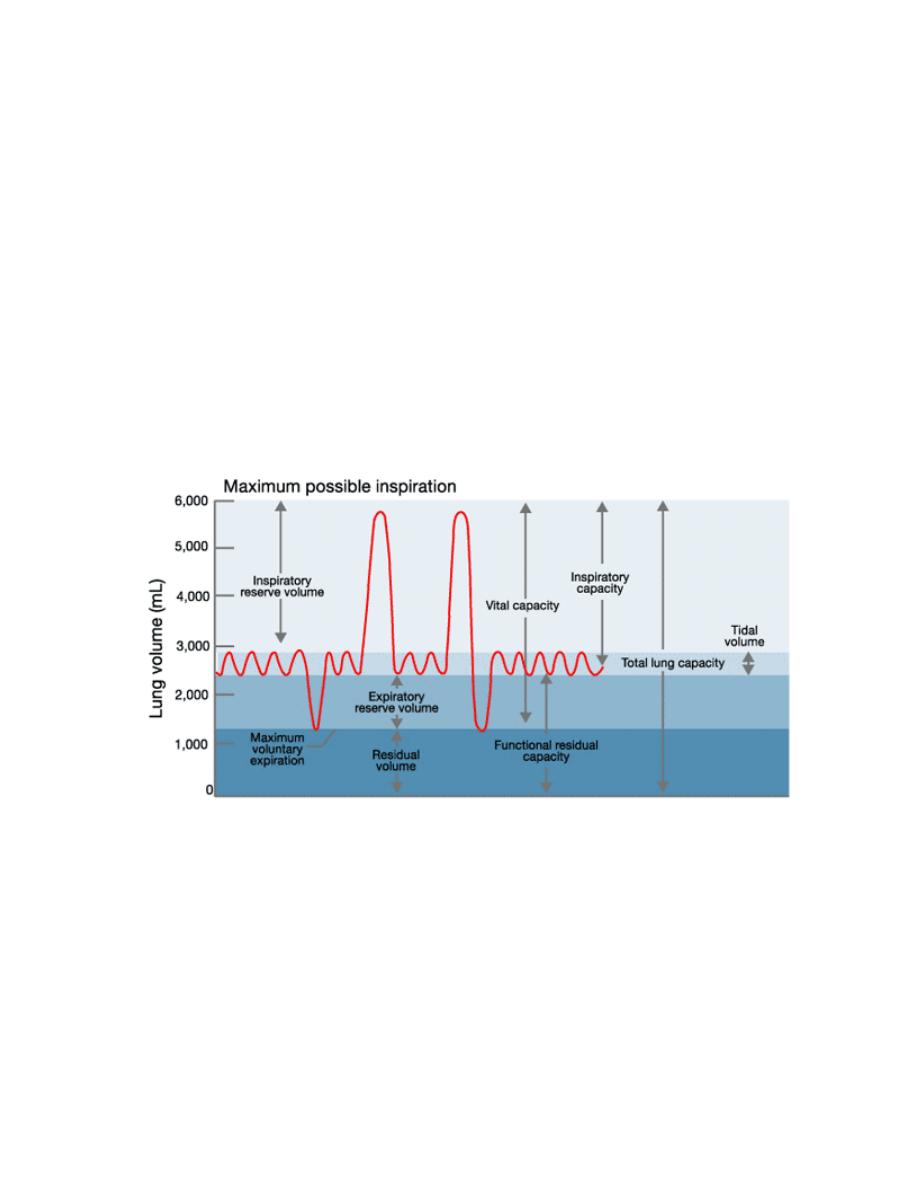
Normal values:

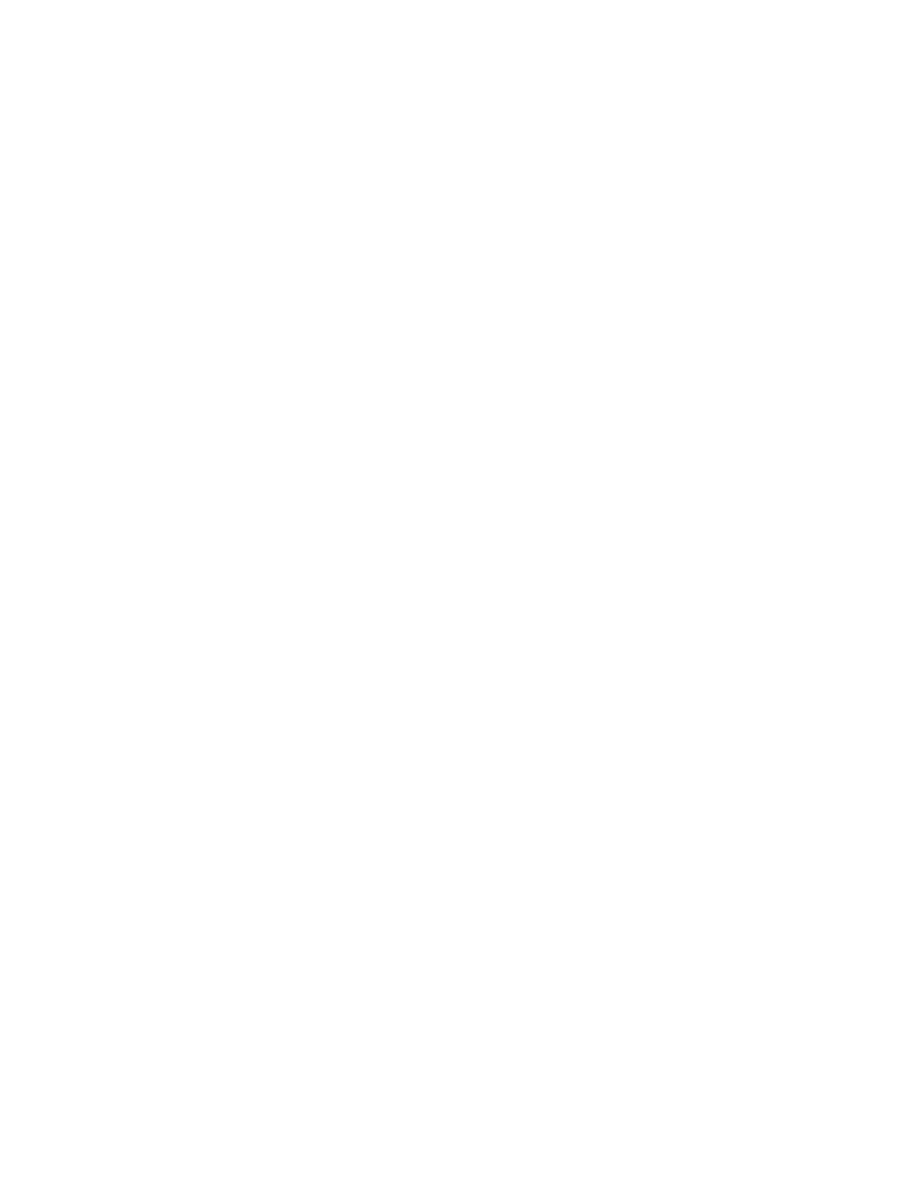
Figure: Spirometer
Measuring the respiratory function (volume)
An important quantitation of human respiratory function is the measurement of
lung volumes and capacities together with the rate of airflow by the spirometer
The static lung volumes are independent from time, reflecting:
- The amount of inspired and expired air, and
- providing information about the strength of the respiratory muscles and
other aspects of pulmonary functions
These volumes include:
-
Tidal volume (TV): The amount of air that moves into the lungs with each
inspiration (or the amount that moves out with each expiration) during breathing
Normal value: 500–750 ml at rest (during exercise can be more than 3L)
-
Inspiratory reserve volume (IRV): The amount of air inspired with a maximal
inspiratory effort at the end of a tidal inspiration at rest
Normal value: 3100 ml for males
1900 ml for females
-
Expiratory reserve volume (ERV): The volume exhaled by an active expiratory
effort at the end of a passive tidal expiration
Normal value: 1200 ml for males
900 ml for females
- Residual volume (RV): The amount of air left in the lungs after an expiration
with maximal effort (Static value which is not measured by spirometer)
Normal average in adults: 1100-1200 ml
- Vital capacity (VC): refers to the maximum amount of air expired from the fully
inflated lung, or maximum inspiratory level (TV + IRV + ERV).
VC is depending on the height (H), age (A) and sex of the investigated person
- Inspiratory capacity (IC, ∼2.5 L), which is the maximum amount of air that can
be inspired from the resting end-expiratory level (IRV + TV).
- Functional residual capacity (FRC; ∼2.5 L) represents the volume of the air
remaining in the lungs after expiration of a normal, resting breath (RV + ERV)
-
Total lung capacity (TLC) = (TV+ IRV + ERV +RV)
Normal value =
∼5 L
Speed of the volume changes in forced breathing can also be measured by the
following parameters:
- Forced vital capacity (FVC), the largest amount of air that can be expired after a
maximal inspiratory effort, is a frequently measured index.
It gives useful information about the strength of the respiratory muscles and
other aspects of pulmonary function
- FEV1 (forced expiratory volume in 1 sec): The major fraction of VC is already
exhaled in the first second of forced exhalation maneuver.
Since FEV depends on the personal physical abilities, the FEV1 to FVC ratio
(FEV1/FVC) is used in practice to: - compare FEV values of different persons and
- recognize the classes of airway disease.
- Maximal voluntary ventilation (MVV) is the largest volume of gas that can be
moved into and out of the lungs in 1 min by voluntary effort
Interpretation of the above values
Static pulmonary volumes and capacities are generally measured to assess the
health of the respiratory system because pulmonary diseases can fundamentally
affect these values.
- Low vital capacity (VC) can reflect a restrictive pulmonary diseases that
decreases the ability of a lung to inflect and deflect, which could be caused by:
- Reduction in the respiratory surface and increase rigidity
(e.g., alveolitis, pulmonary fibrosis)
- Reduction in the elastic properties of the lung tissue
(Reflects various interstitial lung disease)
- Changes or inhibitions of the respiratory movements
(e.g. Guillain-Barre syndrome)
- Low FVC (Forced vital capacity) means there is a resistance in the airway
passages, which could indicate the presence of obstructive airway disease, such
as:
- Chronic bronchitis
- Asthma (inflammation of the lining of the airways)
- Emphysema (destruction of lung tissue around alveoli makes these
air sacs unable to hold their functional shape upon exhalation)
- Low MVV (Maximal voluntary ventilation) Diseases of the respiratory muscles
