Malabsorption syndromes
Dr. Ban AdilMBChB,FICMS,MRCPCh
Malabsorption syndromes:
are conditions that affect the digestion or the absorption of nutrients.Clinical feature
Classification : Based on the Predominant Nutrient Which Is Malabsorbed
CLINICAL APPROACH TO A CHILD WITH SUSPECTED MALABSORPTION
History:Onset:
• In congenital chloride diarrhea and microvillus inclusion disease, the stool is watery since birth and can be mistaken for urine.
• Onset of symptoms after introduction of a particular food into a child's diet may provide diagnostic clues, such as seen with gluten in gluten-sensitive enteropathy
Nature :
• explosive watery diarrhea suggests carbohydrate malabsorption;
• loose, bulky stools are associated with celiac disease; and
• pasty and yellowish offensive stool suggests an exocrine pancreatic insufficiency.
Stool color is usually not helpful; green stool with undigested “peas and carrots” may suggest rapid intestinal transit in toddler's diarrhea.
Dietary history A common example is the child with chronic, nonspecific diarrhea (toddler's diarrhea) generally presents in well-appearing toddlers between 1 and 3 yr of age (toddler's diarrhea). The diarrhea is often brown and watery, at times containing undigested food particles. If the child's fluid intake is >150 mL/kg/24 hr, fluid intake should be reduced to no more than 90 mL/kg/24 hr.
• Appetite
• very good appetites(voraceous) as in exocrine pancreatic insufficiency(cystic fibrosis)
• anorexia celiac disease
• Food avoidance CHO malabsorption due to abdominal distension &abdominal pain.
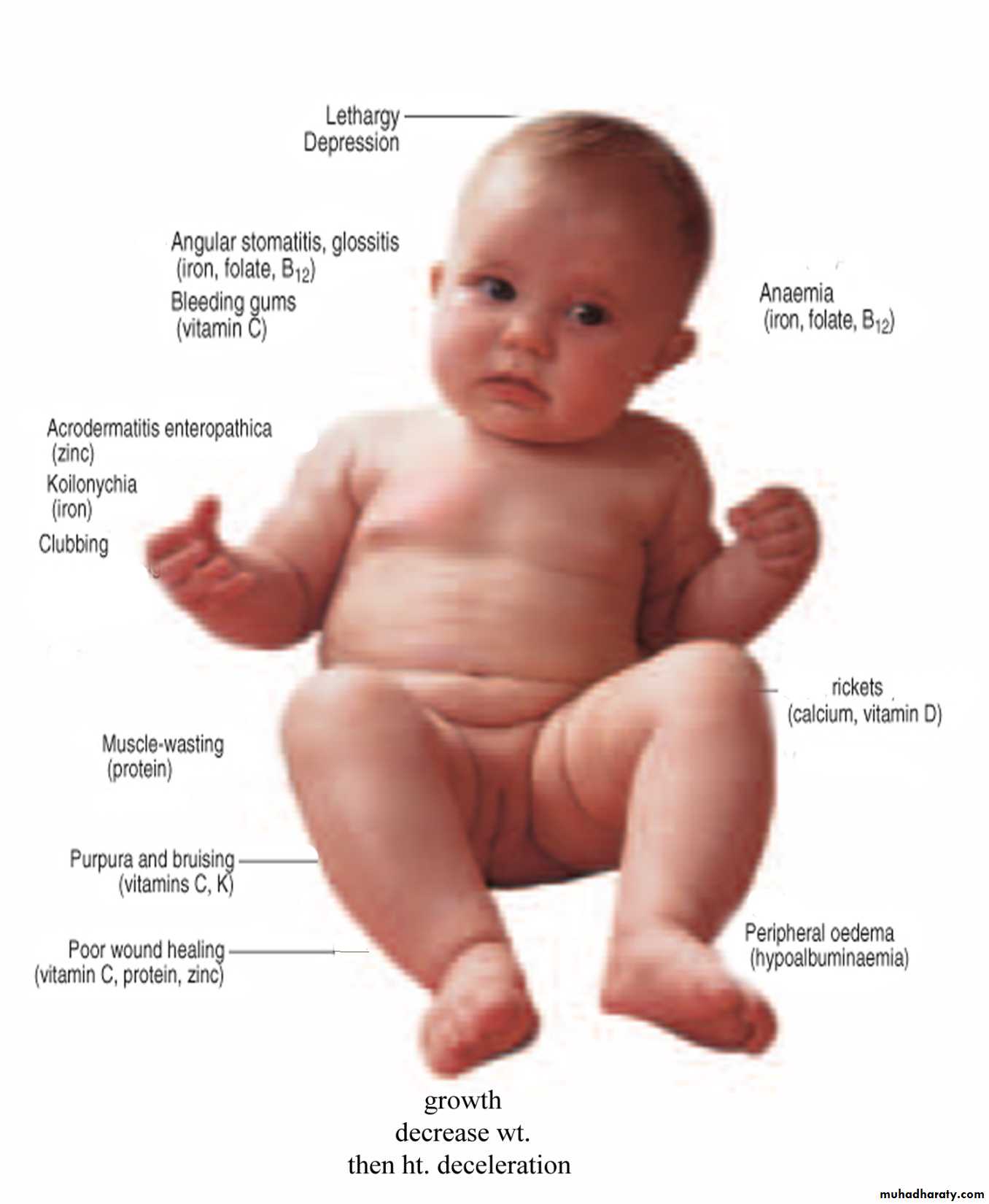
Change in weight, then ↓ht. the OFC will be compromised when malnutrition become chronic.
Abnormal hair
(Meknes hair)Abdominal distention
Perianal excoriation
Physical findings:
signs of malnutrition: include the disappearance of the subcutaneous fat, muscle wasting, and the appearance of skin being too loose for the child .
Specific findings may guide toward a particular disorder;
• edema protein-losing enteropathy,
• digital clubbing cystic fibrosis and celiac disease,
• perianal excoriation and gaseous abdominal distention carbohydrate malabsorption,
• perianal and circumoral rash acrodermatitis enteropathica,
• abnormal hair Menkes syndrome
• Long-term calcium and vitamin D malabsorption can lead to reduced bone mineral density and metabolic bone disease with increased risk of bone fractures.
• Vitamin K malabsorption, irrespective of the underlying mechanism (fat malabsorption, mucosal atrophy), can result in coagulopathy.
• Other nutrient deficiencies include iron malabsorption causing microcytic anemia and low reticulocyte count,
• low serum folate levels in conditions associated with mucosal atrophy,
• and low serum vitamin A and vitamin E concentration in fat malabsorption.
Investigation
carbohydrate malabsorptionClinitest reagent for reducing substances is a simple screening test and can be performed at the bedside. The test is easily performed by combining 10 drops of water with 5 drops of stool and then adding a Clinitest tablet. The color change can be quantified as trace to 4+ using a color sheet provided by the manufacturer. Only 2+ or higher should raise the possibility of sugar malabsorption. Sucrose is not a reducing sugar and requires hydrolysis with hydrochloric acid before analysis.
Stool pH, obtained easily with pH paper, lower than 5.6 is also suggestive of carbohydrate malabsorption.
The breath hydrogen test can also be used to evaluate carbohydrate malabsorption. The gas produced by bacterial degradation of carbohydrates is largely absorbed in the colon, enters the portal and systemic venous return, goes to the lung, and is then released in the breath
Protein malabsorption
Protein loss cannot be evaluated directly because bacterial protein accounts for such a large proportion of the stool nitrogen.
Measurement of spot stool α1 -antitrypsin levels is helpful in establishing a diagnosis of protein-losing enteropathy. This serum protein is resistant to digestion and therefore can be measured in stool in contrast to albumin.
Gluten-Sensitive Enteropathy (Celiac Disease)
Celiac disease is an immune-mediated enteropathy caused by permanent sensitivity to gluten in genetically susceptible individuals which lead to mucosal damage.
It is now estimated that the frequency of celiac disease in the United States is around 1:300
PATHOGENESIS.
Celiac disease develops only after dietary exposure to the protein gluten, which is found in wheat, rye, oat and barley.
The activity of gluten resides in the gliadin fraction
PATHOGENESIS:
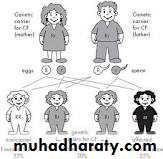
• A genetic predisposition• monozygotic twins approaching 100%.
• Two to 5% of first-degree relatives have symptomatic gluten-sensitive enteropathy
• Individuals with HLA-DQ2 and –DQ8 tissue type are at higher risk.
Celiac disease occurs at a higher frequency in children with
• type 1 diabetes and is 50 times more common
• Down syndrome.
• selective IgA deficiency.
• Turner syndrome,
• thyroiditis.
Environmental factors such as viruses may also play a role
The inflammatory response results in :
Total or subtotal villus atrophy,crypt hyperplasia,
increased number of intraepithelial lymphocytes,
damage to the surface epithelium in the small bowel.
The injury is greatest in the proximal small bowel and extends distally for a variable distance.
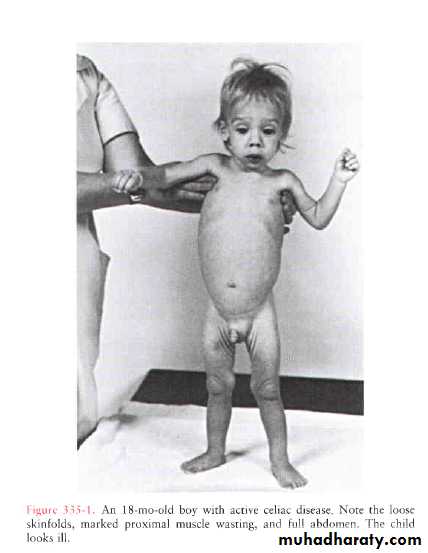
A. SYMPTOMS AND SIGNS
• 6. Constipation, vomiting, and abdominal pain—This triad of symptoms may in a small number of patients dominate the clinical picture and suggest a diagnosis of intestinal obstruction. Constipation generally results from a combination of anorexia, dehydration, muscle weakness, and bulky, fatty stools• 7.Short stature and delayed puberty are characteristic in older children
•
Nongastrointestinal Manifestations of Celiac Disease
• Dermatitis herpetiforms• Dental enamel hypoplasia
• Osteopenia/osteoporosis
• Short stature
• Delayed puberty
• Anemia (nonresponsive to iron therapy, seen in adults only)
• Hepatitis
• Arthritis
• Brain calcifications
• Neurologic symptoms
LABORATORY FINDINGS
1.increase Fat content of stools—A 3-day collection of stools usually reveals excessive fecal fat.2. Impaired carbohydrate absorption
3. Hypoproteinemia —Hypoalbuminemia
SEROLOGIC TESTS
Antigliadin and antireticulin antibodies are often present in celiac disease. However, there is a 10% false-positive rate for the IgG antigliadin antibody among healthy individuals.Endomysial or tissue transglutaminase antibody assays are the most sensitive and specific screening tests for celiac disease. As both of these antibodies are of the IgA class, screening for them in a patient who is IgA deficient may yield a falsely negative screen result.
The best available serologic screening test, therefore, is a quantitative IgA level with a transglutaminase or endomysial antibody assay.
Genetic tests
have an increasing role in the diagnosisLess than 2% of celiac patients lack both HLA specificities;
at the same time, approximately one third of the “normal” population has one or the other marker;
that means that the measurement of HLA DQ2 and/or DQ8 has a strong negative predictive value but a very weak positive predictive value for the diagnosis of celiac disease.
With these limitations the test can prove useful to exclude celiac disease when the genetic studies are negative in subjects on a gluten-free diet or in subjects belonging to an at-risk group (e.g., 1st-degree relatives, insulin-dependent diabetics, patients with Down syndrome) to avoid long-term follow-up.
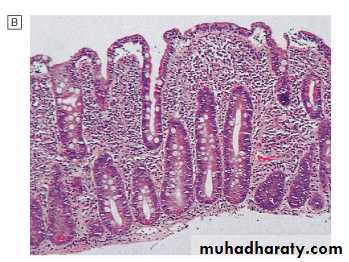
D. BIOPSY FINDINGS
Total or subtotal villus atrophy,crypt hyperplasia,
increased number of intraepithelial lymphocytes,
damage to the surface epithelium in the small bowel.
The ultimate diagnosis of celiac disease relies on the demonstration of specific, though not pathognomonic, histopathologic abnormalities in the small bowel mucosa .
According to The European Society for Pediatric Gastroenterology, Hepatology and Nutrition (ESPGHAN) current criteria
, the 2 requirements mandatory for the diagnosis of celiac disease are:
the finding of villous atrophy with hyperplasia of the crypts and abnormal surface epithelium, while the patient is eating adequate amounts of gluten,
and a full clinical remission after withdrawal of gluten from the diet.
The finding of circulating IgA celiac disease–associated antibodies at the time of diagnosis and their disappearance on a gluten-free diet adds weight to the diagnosis.
A control biopsy to verify the consequences of the gluten-free diet on the mucosal architecture is considered mandatory only in patients with an equivocal clinical response to the diet.
Gluten challenge is not considered mandatory except in situations where there is doubt about the initial diagnosis, for example, when an initial biopsy was not performed or when the biopsy specimen was inadequate or atypical of celiac disease.
Treatment
A. DIETTreatment consists of dietary gluten restriction for life. All sources of wheat, rye, barley, and oat gluten must be eliminated during the initial treatment.
Clinical improvement is usually evident within a week, and
histologic repair is complete after 3–12 months.
Tissue transglutaminase titers may decrease on a gluten free diet, but usually do not disappear.
B. CORTICOSTEROIDS
are indicated only in very ill patients with signs and symptoms of celiac crisis (profound malnutrition, diarrhea, edema, abdominal distention, and hypokalemia).
Prognosis
Clinical and histologic recovery is the rule but may be slow.Malignant lymphoma of the small bowel occurs with increased frequency in adults with long-standing disease.
Dietary treatment seems to decrease the risk of this complication.
Cystic Fibrosis ETIOLOGY AND EPIDEMIOLOGY
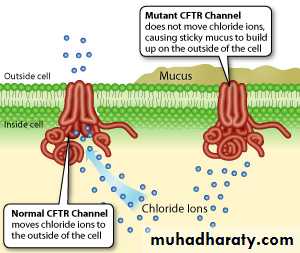
CF, an autosomal recessive disorder, In the U.S., 1 in 3200 white newborns is born with CFThe gene for CF, localized to the long arm of chromosome 7, termed cystic fibrosis transmembrane regulator (CFTR) The secretory and absorptive characteristics of epithelial cells are affected.
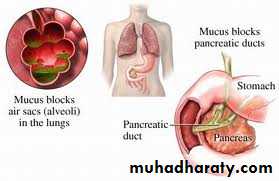
the respiratory epithelium exhibits marked impermeability to chloride and an excessive reabsorption of sodium. These lead to a relative dehydration of the airway secretions, resulting in impaired mucociliary transport and airway obstruction
The classic hallmark of CF:
Most patients are colonized with Haemophilus influenzae, Staphylococcus aureus, or Pseudomonas aeruginosa or Burkholderia cepacia
cough (the most common initial pulmonary manifestation), sputum production, hyperinflation, bronchiectasis, and pulmonary insufficiency and death.
Digital clubbing is common, even without significant lung disease.
Chronic sinusitis is nearly universal, and nasal polyposis is common.
Other potential pulmonary complications of CF include atelectasis, progressive bronchiectasis, hemoptysis, and pneumothorax
• Chronic bronchial infection
pancreatic insufficiency
Most patients with CF have exocrine pancreatic insufficiency early in life (if not at birth) as a result of inspissation of mucus in the pancreatic ducts.
Maldigestion with secondary malabsorption results in steatorrhea (large, fatty, floating, foul-smelling stools) and
many secondary deficiency states (vitamins A, D, E, and K) in untreated patients.
Nutrient malabsorption also results in failure to thrive despite a ravenous appetite.
In adolescent or adult patients, relative insulin deficiency may develop. Hyperglycemia and CF-related diabetes may become symptomatic; ketoacidosis is rare.
Secondary amenorrhea Women with CF have given birth, however. Males are almost universally azoospermic, with atrophy or absence of the vas deferens.
The failure of the sweat ducts to conserve salt may lead to heat exhaustion or to unexplained hypochloremic alkalosis in infants.
Diagnostic Criteria for Cystic Fibrosis (CF)
OROR
OR
OR
plus
sweat test
sweat test
The sweat test, which involves using pilocarpine iontophoresis to collect sweat and performing chemical analysis of its chloride content, is the standard approach to diagnosis of CF. The procedure requires care and accuracy. An electric current is used to carry pilocarpine into the skin of the forearm and locally stimulate the sweat glands. If an adequate amount of sweat is collected, the specimens are analyzed for chloride concentration. Testing may be difficult in the 1st 2 wk of life because of low sweat rates but is recommended any time after the 1st 48 hr of life. Positive results should be confirmed; for a negative result, the test should be repeated if suspicion of the diagnosis remains.a positive result obtained from a sweat test on two or more occasions (positive if >60 mEq/L with adequate sweat collection of at least 75 mg,
borderline if 40 to 60 mEq/L, and
negative if <40 mEq/L
Non-CF conditions associated with elevated concentrations of sweat electrolytes(false +ve) include
• untreated adrenal insufficiency,
• ectodermal dysplasia,
• hereditary nephrogenic diabetes insipidus,
• hypothyroidism,
• hypoparathyroidism,
• familial cholestasis,
• pancreatitis,
• mucopolysaccharidoses, and
• malnutrition. Most of these conditions can be easily distinguished from CF by clinical criteria
False-negative test results may be encountered in children with hypoproteinemic edema.
Treatment :