Fructose metabolism
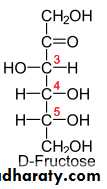
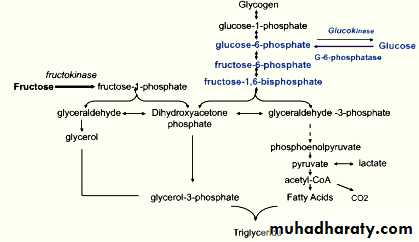
While virtually absent in our diet a few hundred years ago, fructose has now become a major constituent of our modern diet. Our main sources of fructose are sucrose from beet or cane, high fructose corn syrup, fruits, and honey. Fructose has the same chemical formula as glucose (C(6)H(12)O(6)), but its metabolism differs markedly from that of glucose due to its almost complete hepatic extraction and rapid hepatic conversion into glucose, glycogen, lactate, and fat.
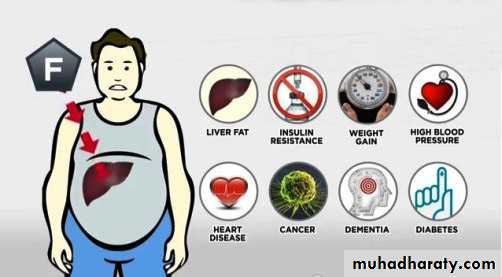
Fructose was initially thought to be advisable for patients with diabetes due to its low glycemic index. However, chronically high consumption of fructose in rodents leads to many metabolic problems. Hepatic de novo lipogenesis and lipotoxicity, oxidative stress, and hyperuricemia have all been proposed as mechanisms responsible for these adverse metabolic effects of excess fructose.
Results of excess fructose consumption
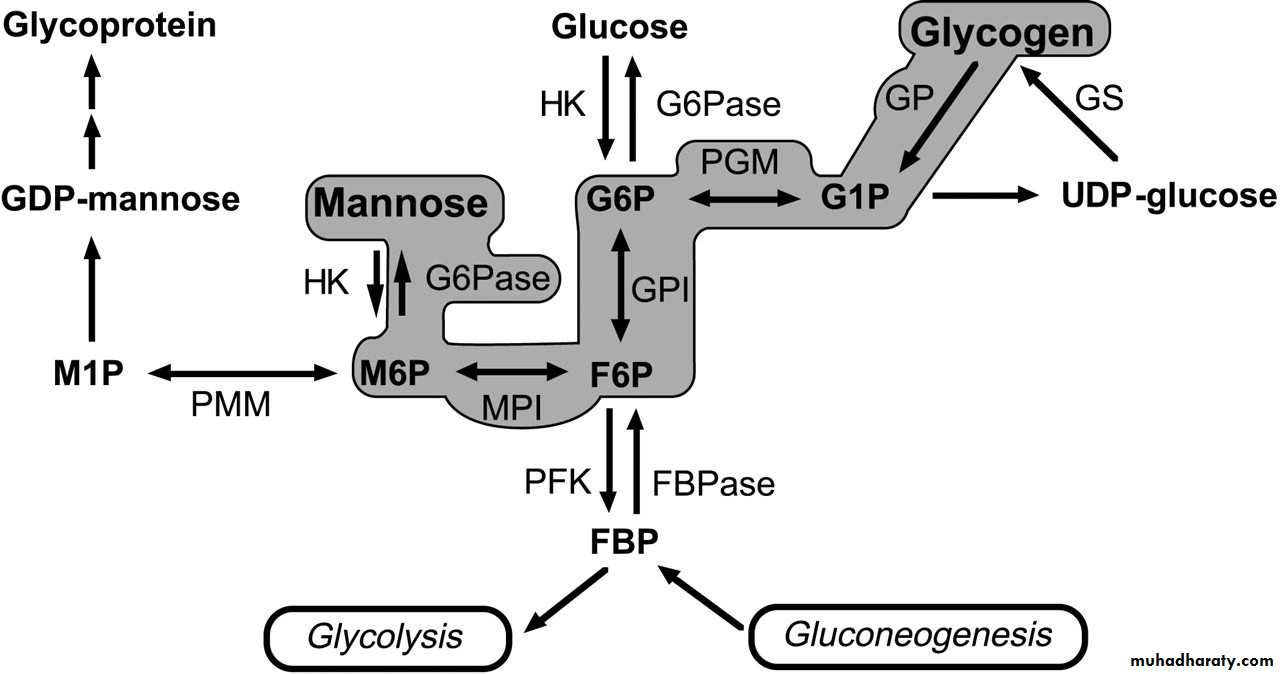
Mannose metabolism
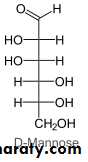
Mannose is a sugar monomer of the HYPERLINK "https://en.wikipedia.org/wiki/Hexose" \o "Hexose" aldohexose series of carbohydrates. Mannose is a C-2 HYPERLINK "https://en.wikipedia.org/wiki/Epimer" \o "Epimer" epimer of glucose. Mannose is important in human metabolism, especially in the HYPERLINK "https://en.wikipedia.org/wiki/Glycosylation" \o "Glycosylation" glycosylation of certain proteins. Several congenital disorders of glycosylation are associated with mutations in enzymes involved in mannose metabolism.
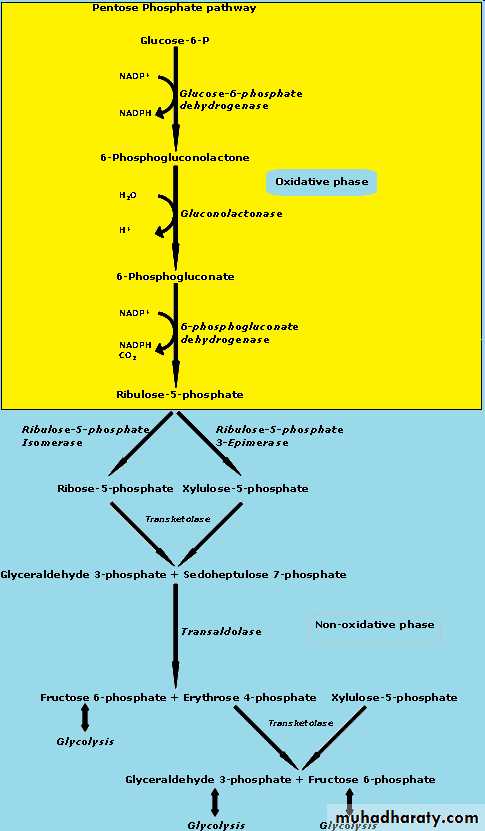
Pentose Phosphate Pathway
The pentose phosphate pathway (also called the hexose monophosphate pathway, or 6-phosphogluconate pathway) occurs in the cytosol of the cell. It includes two, irreversible oxidative reactions, followed by a series of reversible sugar–phosphate interconversions . No ATP is directly consumed or produced in the cycle. Carbon 1 of glucose 6-phosphate is released as CO2, and two NADPH are produced for each glucose 6-phosphate molecule entering the oxidative part of the pathway. The rate and direction of the reversible reactions of the pentose phosphate pathway are determined by the supply of and demand for intermediates of the cycle. The pathway provides a major portion of the body’s NADPH, which functions as a biochemical reductant.It also produces ribose 5-phosphate, required for the biosynthesis of nucleotides and provides a mechanism for the metabolic use of five-carbon sugars obtained from the diet or the degradation of structural carbohydrates in the body.
There are three distinct phases each of which has a distinct outcome. Depending on the needs of the organism the metabolites of that outcome can be fed into many other pathways.Gluconeogenesis is directly connected to the pentose phosphate pathway. As the need for glucose-6-phosphate (the beginning metabolite in the pentose phosphate pathway) increases so does the activity of HYPERLINK "http://chemwiki.ucdavis.edu/Biological_Chemistry/Metabolism/Gluconeogenisis" \o "Gluconeogenesis" gluconeogenesis.
The main molecule in the body that makes anabolic processes possible is NADPH. Because of the structure of this molecule it readily donates hydrogen ions to metabolites thus reducing them and making them available for energy harvest at a later time. The PPP can also be used to produce glyceraldehyde-3-phosphate which can then be fed into the TCA and ETC cycles allowing for the harvest of energy. Depending on the needs of the cell certain enzymes can be regulated and thus increasing or decreasing the production of desired metabolites. The enzymes reasonable for catalyzing the steps of the PPP are found most abundantly in the liver more specifically in the cytosol. The cytosol is where fatty acid synthesis takes place which is a NADPH dependent process.
Oxidation Phase
The beginning molecule for the PPP is glucose-6-P which is the second intermediate metabolite in glycolysis. Glucose-6-P is oxidized in the presence of glucose-6-P dehydrogenase and NADP+. This step is irreversible and is highly regulated. NADPH and fatty acyl-CoA are strong negative inhibitors to this enzyme. The purpose of this is to decrease production of NADPH when concentrations are high or the synthesis of fatty acids is no longer necessary.
The metabolic product of this step is gluconolactone which is hydrolytrically unstable. Gluconolactonase causes gluconolactone to undergo a ring opening hydrolysis
6-phospho-D-gluconate is oxidized by NADP+ in the presence of 6-phosphogluconate dehydrogenase which yields ribulose-5-phosphate.
The oxidation phase of the PPP is solely responsible for the production of the NADPH to be used in anabolic processes.
Non-oxidation ( Isomerization) Phase
Ribulose-5-phosphate can then be isomerized by phosphopentose isomerase to produce ribose-5-phosphate. Ribose-5-phosphate is one of the main building blocks of nucleic acids and the PPP is the primary source of production of ribose-5-phosphate.
If production of ribose-5-phosphate exceeds the needs of required ribose-5-phosphate in the organism, then phosphopentose epimerase catalyzes a chiralty rearrangement about the center carbon creating xylulose-5-phosphate.
The products of these two reactions can then be rearranged to produce many different length carbon chains. These different length carbon chains have a variety of metabolic fates as shown in the figure above .
GLUCOSE 6-P DEHYDROGENASE DEFICIENCY
Glucose 6-phosphate dehydrogenase (G6PD) deficiency is an inherited disease characterized by hemolytic anemia caused by the inability to detoxify oxidizing agents. G6PD deficiency is the most common disease- producing enzyme abnormality in humans, affecting more than 400 million individuals worldwide. This deficiency has the highest prevalence in the Middle East, tropical Africa and Asia, and parts of the Mediterranean.
G6PD deficiency is, in fact, a family of deficiencies caused by more than 400 different mutations in the gene coding for G6PD. Only some of these mutations cause clinical symptoms.[Note: In addition to hemolytic anemia, a clinical manifestation of G6PD deficiency is neonatal jaundice appearing 1–4 days after birth.The jaundice, which may be severe, typically results from increased production of unconjugated bilirubin . The life span of individuals with a severe form of G6PD deficiency may be somewhat shortened as a result of complications arising from chronic hemolysis.
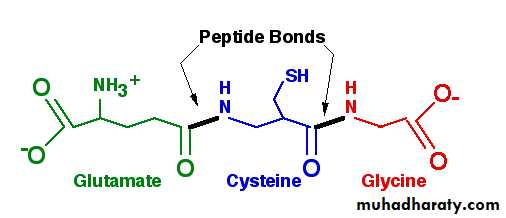
A. Role of G6PD in red blood cells
Diminished G6PD activity impairs the ability of the cell to form the NADPH that is essential for the maintenance of the reduced glutathione pool. This results in a decrease in the cellular detoxification of free radicals and peroxides formed within the cell . Glutathione also helps maintain the reduced states of sulfhydryl groups in proteins, including hemoglobin. Oxidation of those sulfhydryl groups leads to the formation of denatured proteins that form insoluble masses (called Heinz bodies) that attach to the red cell membranes . Additional oxidation of membrane proteins causes the red cells to be rigid (less deformable), and they are removed from the circulation by macrophages in the spleen and liver. Although G6PD deficiency occurs in all cells of the affected individual, it is most severe in erythrocytes, where the pentose phosphate pathway provides the only means of generating NADPH. Other tissues have alternative sources for NADPH production (such as NADP+-dependent malate dehydrogenases) that can keep glutathione reduced.
The erythrocyte has no nucleus or ribosomes and cannot renew its supply of the enzyme. Thus, red blood cells are particularly vulnerable to enzyme variants with diminished stability.
B. Precipitating factors in G6PD deficiency
Most individuals who have inherited one of the many G6PD mutations do not show clinical manifestations, that is, they are asymptomatic. However, some patients with G6PD deficiency develop hemolytic anemia if they are treated with an oxidant drug, ingest fava beans, or contract a severe infection.
1. Oxidant drugs: Commonly used drugs that produce hemolytic anemia in patients with G6PD deficiency are best remembered from the mnemonic AAA—Antibiotics Antimalarials and Antipyretics .
2. Favism: Some forms of G6PD deficiency, for example the Mediterranean variant, are particularly susceptible to the hemolytic effect of the fava (broad) bean, a dietary staple in the Mediterranean region. Favism, the hemolytic effect of ingesting
fava beans, is not observed in all individuals with G6PD deficiency, but all patients with favism have G6PD deficiency.
3. Infection: Infection is the most common precipitating factor of hemolysis in G6PD deficiency. The inflammatory response to infection results in the generation of free radicals in macro phages, which can diffuse into the red blood cells and cause oxidative damage.