PEPTIC ULCER DISEASETUCOMInternal Medicine 4th class Dr Hassan. I. Sultan
Functional anatomy and physiology of stomach and duodenum:Stomach: The stomach acts as a 'hopper', retaining and grinding food, then actively propelling it into the upper small bowel.
it’s divided into four regions; the cardia, the fundus, the body, and the antrum: which end by pyloric channal.
The mucosa, is formed by a layer of columnar epithelium. The submucosa, immediately deep to the mucosa, provides a dense connective tissue in which lymphocytes, plasma cells, arterioles, venules, lymphatics, and the myenteric plexus are contained. The third tissue layer, the muscularis propria, is a combination of an inner oblique, a middle circular, and an outer longitudinal smooth muscle layer. The serosa, a thin, transparent continuation of the visceral peritoneum.
The gastric epithelial lining consists of rugae that contain microscopic gastric pits.
Gastric glands: made up of highly specialized epithelial cells:
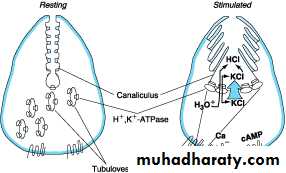
1- Parietal cells, which secrete both acid and intrinsic factor. Acid is secreted in response to the activity of the hydrogen-potassium ATPase ('proton pump') .2- Chief cells, which secrete pepsinogen .
3- ECL cells, which secrete histamine .
4- G cells, which secrete gastrin .
5- D cells, which secrete somatostatin.
6- Mucus, secreting cells.
Duodenum: The most proximal portion of the small intestine, forms a C-shaped loop around the head of the pancreas and is in continuity with the pylorus proximally and the jejunum distally.
Angular changes in course divide the duodenum into four portions. The first part of the duodenum is the duodenal bulb or cap.
The submucosal Brunner's glands that produce bicarbonate-rich secretions involved in acid neutralization.
The mucosal defense system
1- The first line of defense is a mucus-bicarbonate layer.
2- The next line of defense is the epithelial cells, intracellular tight junctions, cells 3- migration, and cell proliferation and renewal.
4- Prostaglandins are important in maintaining mucosal blood flow.
PEPTIC ULCER DISEASE
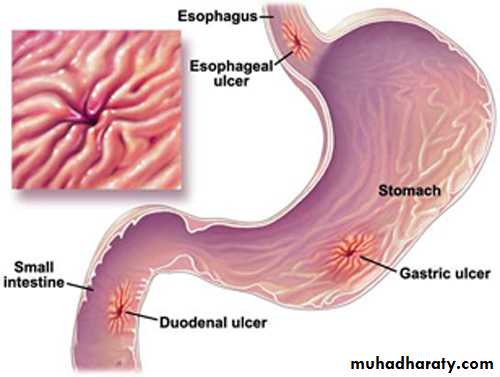
Peptic ulcer: refers to an ulcer in the lower oesophagus, stomach or duodenum, in the jejunum after surgical anastomosis to the stomach or, rarely, in the ileum adjacent to a Meckel's diverticulum, which penetrate the muscularis mucosae. Erosions; do not penetrate it.Ulcer may be acute or chronic, but acute ulcer show no evidence of fibrosis.
Gastric and duodenal ulcer
The prevalence of peptic ulcer is decreasing in Western communities as a result of widespread use of H. pylori eradication therapy.It remains high in developing countries.
Male to female ratio for duodenal ulcer varies from 5:1 to 2:1 .
whilst that for gastric ulcer is 2:1 or less.
Pathophysiology and aetiology of PUD:
1- H. pylori infection; the prevalence of H. pylori infection in developed world approxim. 50% of those over the age of 50 yrs while 90% of the adult population in developing world are infected.The vast majority of colonised people remain healthy and asymptomatic.
90% of duodenal ulcer patients and 70% of gastric ulcer patients are infected with H. pylori.
H. pylori: is Gram-negative, spiral and has multiple flagella at one end which make it motile, allowing it to burrow and live deep beneath the mucus layer closely adherent to the epithelial surface.
production of the enzyme urease, this produces ammonia from urea and raises the pH around the bacterium.
It spread by person-to-person contact via gastric refluxate or vomit.
H. pylori exclusively colonises gastric-type epithelium, in duodenum in assoctation of gastric metaplasia.
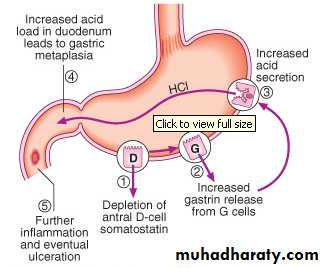
In most people H. pylori causes antral gastritis --depletion of somatostatin (from D cells)---hypergastrinaemia --- increase acid production ---DU
role of H. pylori in GU is less clear but H. pylori may be due to reduced gastric mucosal resistance to acid and pepsin.
1% of infected people---pangastritis ---gastric atrophy ---hypochlorhydria ---gastric cancer .
The end result of H pylori infection
1- Gastritis2- PUD
3- Gastric MALToma
4- Gastric cancer
NSAIDs: NSAIDs induce ulcer by reducing mucosal resist.– decrease Prostaglandin– mucous Injury.
RISK FACTORS FOR NSAID-INDUCED ULCERS
1- Age > 60 years
2- Past history of peptic ulcer
3- Past history of adverse event withNSAIDs
4- Concomitant corticosteroid use
5- High-dose or multiple NSAIDs
6- Individual NSAID-highest with azapropazone, piroxicam, ketoprofen; lower with ibuprofen
Zollinger-Ellison syndrome (ZES): gastrin-secreting tumors, accounts for 0.1% of causes of PUD.
should be considered in patients with ulcers in unusual sites (e.g., distal duodenum or jejunum); multiple, recurrent, or complicated duodenal ulcers; or ulcers associated with chronic diarrhea.
Smoking: increased risk of GU and, to a lesser extent DU, more complications , less healing .
Pathology of PUD:
Duodenal Ulcers mostly in the first portion of duodenum (>95%), Ulcers are sharply demarcated,the base of the ulcer often consists of a zone of eosinophilic necrosis with surrounding fibrosis. Malignant DUs are extremely rare.GUs can represent a malignancy, bening GUs are histologically similar to DUs.
Clinical features
1- PUD chronic condition with a history of spontaneous relapse and remission lasting for decades.The most common presen.---recurrent abdominal pain ---three charact.
A-Localization to the epigastrium.
B- Relationship to food.
C- Episodic occurrence.
2- Epigastric pain described as a burning or gnawing discomfort , hunger pain, relieved by antacids or food, awakes the patient from sleep ,Wt gain.
3- Vomiting occurs in about 40%; persistent daily vomiting suggests gastric outlet obstruction.
In some patients --silent ulcer; anaemia from chronic undetected blood loss.
4- Complications:
haematemesis, or acute perforation.
5- The pain pattern in GU patients may be different from that in DU patients, where discomfort may actually be precipitated by food. Nausea and weight loss occur more commonly in GU patients.
Investigations of PUD
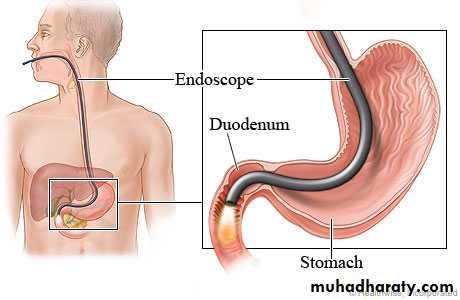
1- Endoscopy is the preferred investigation. Gastric ulcers must always be biopsied .
2- Barium studies DU appears as a well-demarcated crater, most often seen in the bulb. Benign GU also appears as a discrete crater with radiating mucosal folds originating from the ulcer margin. Ulcers >3 cm in size or associ. with a mass are more often malignant.
3- Tests for Detection of H. pylori infection
Test
AdvantagesDisadvantages
NON-INVASIVE
Serology
Rapid kits availableLacks sensitivity and specificity
Urea breath tests
High sensitivi and specifi
expensive
Faecal antigen test
Cheap, accurate
Acceptability
INVASIVE (ANTRAL BIOPSY)
Histology
Sensitivity and specificityFalse negatives occur
Rapid urease tests
Cheap, quick, specifi.
Lack sensitivity
Microbiological culture
'Gold standard'
Slow and laborious
Management
The aims of management are to relieve symptoms, induce healing and prevent recurrence.1- H. pylori eradication.
2- General measures.
3- Short-term management.
4- Maintenance treatment.
5- Surgical treatment.
1- REGIMENS FOR H. PYLORI ERADICATION :
A- 'First-line therapy is a proton pump inhibitor (12-hourly), clarithromycin 500 mg 12-hourly, and amoxicillin 1 g 12-hourly or metronidazole 400 mg 12-hourly, for 7 days.B- Second-line therapy is a proton pump inhibitor (12-hourly), bismuth 120 mg 6-hourly, metronidazole 400 mg 12-hourly, and tetracycline 500 mg 6-hourly, for 7 days.‘
2- General measures Cigarette smoking, aspirin and NSAIDs should be avoided.
3- Short-term management : after H pylori eradication ,followed by continuous acid suppression drugs ( H2 RB or PPI) for 4-6 wks.
4- Maintenance treatment: GU need 8-12wks to complete healing , with repeated endoscopy and biopsy.
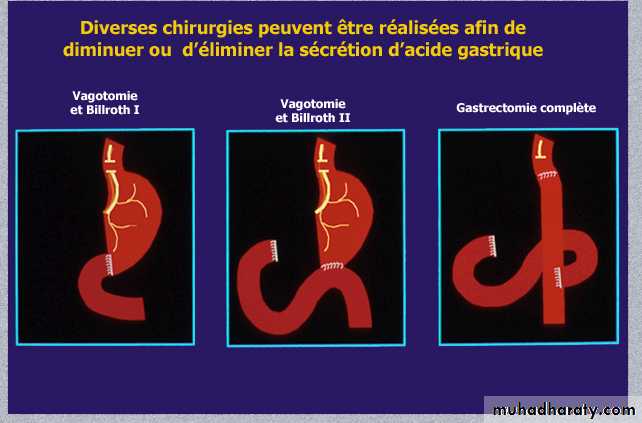
5- Surgical treatment:
A- Emergency: Perforation, Haemorrhage.
B- Elective: Complications, e.g. gastric outflow obstruction . Recurrent ulcer following gastric surgery .
Refractory ulcer
A GU that fails to heal after 12 weeks or DU after 8 weeks of therapy should be considered refractory.Common causes:
poor compliance , persistent H. pylori infection, NSAID use, cigarette smoking , GU malignancy and ZES .
Complications of peptic ulcer disease:
A- Complications of gastric resection or vagotomy:1- Dumping
2- Bile reflux gastritis
3- Diarrhoea and maldigestion
4- Weight loss
5- Anaemia
6-Metabolic bone disease
7- Gastric cancer
B- Complications of PUD itself:
1- Perforation
2- Bleeding
3- Gastric outlet obstruction
IDEAL GROUP
A.H.M.YAHIA
ما كل ما يتمنى المرئ يدركه رب امرء حتفه فيما تمناه