The Spinal Cord
The spinal cord lies in the vertebral canal it is about 42 to 45 cm in length, it extends from the foramen magnum at the base of the skull to a cone-shaped termination, the conus medullaris, usually at the level of the first or second lumbar vertebra (L1 or L2). The dorsal and ventral roots of the more caudal portions of the cord elongate during development and angle downward from the cord, forming what is called the cauda equine (“horse’s tail”). The filum terminale, which is composed of nonneural tissues and the pia mater, continues caudally and attaches to the second sacral vertebra (S2).Spina bifida
About one baby in 1,000 is born with spina bifida, a congenital defect resulting from the failure of one or more vertebrae to form a complete vertebral arch for enclosure of the spinal cord. Its only external sign is a dimple or hairy pigmented spot. Spina bifida cystic is more serious. A sac protrudes from the spine and may contain meninges, cerebrospinal fluid, and parts of the spinal cord and nerve roots.Structure of spinal cord
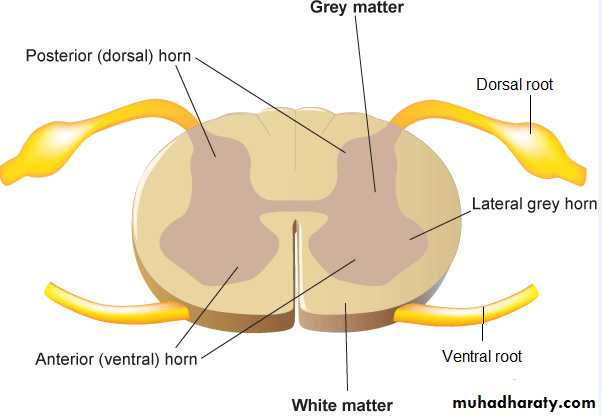
Cross-Sectional AnatomyLike the brain, the spinal cord is covered by meninges and bathed in CSF within bony vertebral canal. The spinal cord is divided into segments that correspond to the segments of the bony vertebral column (cervical, thoracic,lumber….).The spinal nerve fibers of the spinal nerves enter and exit the cord at each segment. The spinal cord is somewhat oval on transverse section and consist of
I. gray matter, the spinal cord has a central core of gray matter that looks
somewhat butterfly- or H-shaped in cross sections. The core consists mainly of two dorsal (posterior) horns, and two thicker ventral (anterior) horns. The right and left sides are connected by a gray commissure. In the middle of the
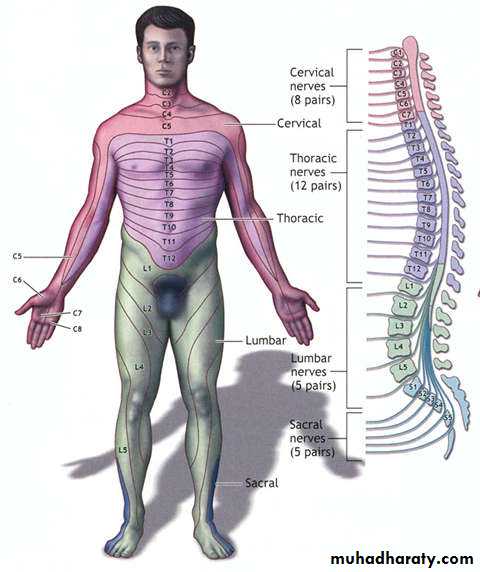
commissure is the central canal, lined with ependymal cells, and filled with CSF. As a spinal nerve approaches the cord, it branches into a dorsal root and ventral root. The dorsal root carries sensory nerve fibers, which enter the dorsal horn of the cord. The ventral horns contain the large somas of the somatic motor neurons mainly (α). Axons from these neurons exit by way of the ventral root of the spinal nerve and lead to the skeletal muscles. There are 32 or more pairs of spinal nerves (i.e., 8 cervical, 12 thoracic, 5 lumbar, 5 sacral, and 2 or more coccygeal). Spinal nerves do not go directly to skin and muscle fibers; instead, they form complicated nerve networks called plexuses. Nerves emerging from a plexus form progressively smaller branches that supply the skin and muscles of the various parts of the body. The major nerve plexuses are: the cervical plexus, the brachial plexus, the lumbar plexus, and the sacral plexus.
Figure: Cross-Section of spinal cord
In the thoracic and lumbar regions, an additional lateral horn is visible on each side of the gray matter. It contains neurons of the sympathetic nervous system, which send their axons out of the cord by way of the ventral root along with the somatic efferent fibers.II.The white matter, contains bundles of myelinated nerve fibers ascending and descending through the spinal cord:
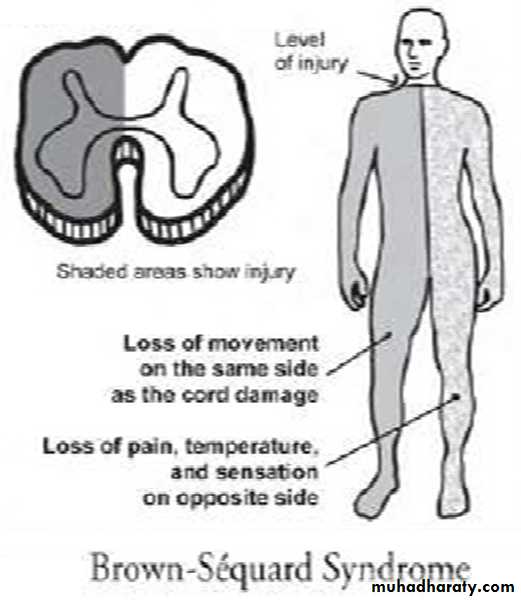
1. Ascending tracts
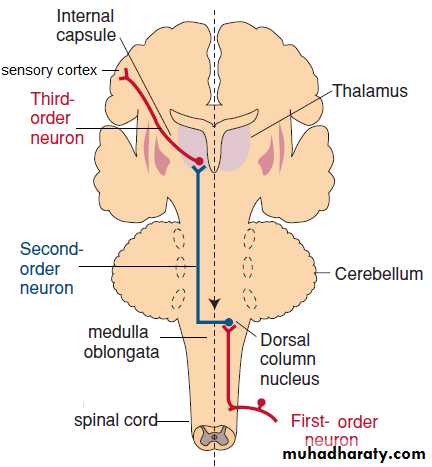
Dorsal column, it carry sensory signals of vibration, visceral pain, deep and discriminative touch, and proprioception. it consist of Gracile fasciculus and Cuneate fasciculus. The gracile fasciculus carries signals from the midthoracic and lower parts of the body. At T6, it is joined by the cuneate fasciculus, carries the same type of sensory signals, originating from level T6 and up (from the upper limb and chest). Its fibers end in the cuneate nucleus on the ipsilateral side of the medulla oblongata. In the medulla, second-order fibers of the gracile and cuneate systems decussate and form the medial lemniscus, a tract of nerve fibers that leads the rest of the way up the thalamus. Third-order fibers go from the thalamus to the cerebral cortex.
Figure: Neural pathway for discriminative touch and vibration. The pathway is a three-neuron chain. The fi rst-order neuron ascends in the dorsal column of the spinal cord; the second-order neuron crosses over the midline in the medulla, and the third-order neuron ascends from the thalamus to the somatosensory cortex..
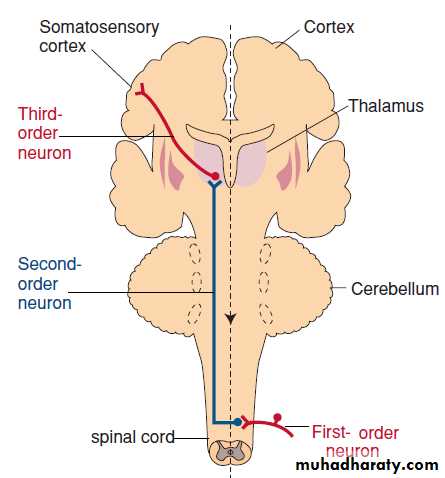
The spinothalamic tract, which passes up the anterior and lateral columns of the spinal cord. The spinothalamic tract carries signals for pain, temperature, pressure, tickle, itch, and light or crude touch. The first-order neurons end in the dorsal horn of the spinal cord near the point of entry. Second-order neurons decussate to the opposite side of the spinal cord and there form the ascending spinothalamic tract. These fibers lead all the way to the thalamus.Third-order neurons continue from there to the cerebral cortex.
The dorsal and ventral spinocerebellar tracts travel through the lateral column and carry proprioceptive signals from the limbs and trunk to the cerebellum. the tracts provide the cerebellum with feedback needed to coordinate muscle action.
figure: Neural pathway for pain and temperature. The pathway is a three-neuron chain. The first-order neuron synapses in the dorsal horn of the spinal cord; the second-order neuron immediately crosses the midline and ascends to the brainstem in the anterolateral white matter of the spinal cord; and the third-order neuron ascends from the thalamus to the somatosensory cortex.
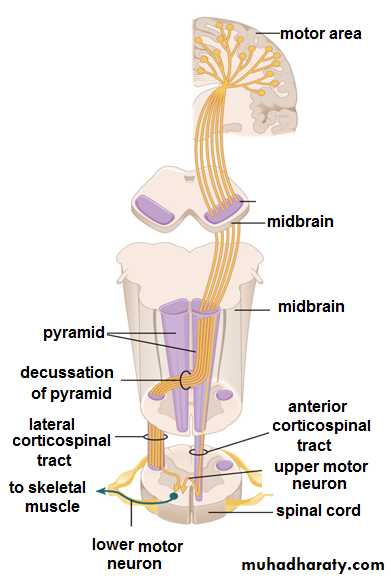
2.Descending Tracts
Descending tracts carry motor signals down the brainstem and spinal cord. A descending motor pathway typically involves two neurons called the upper and lower motor neuron. The upper motor neuron begins with a soma in the cerebral cortex or brainstem and has an axon that terminates on a lower motor neuron in the brainstem or spinal cord. The axon of the lower motor neuron then leads the rest of the way to the muscle or other target organ. The major descending tracts areThe corticospinal tracts carry motor signals from the cerebral cortex for precise, finely coordinated limb movements. The fibers of this system form ridges called pyramids on the ventral surface of the medulla oblongata, so these tracts were once called pyramidal tracts. Most corticospinal fibers decussate in the lower medulla and form the lateral corticospinal tract on the contralateral side of the spinal cord. A few fibers remain uncrossed and form the ventral corticospinal tract on the ipsilateral side. Fibers of the ventral tract decussate lower in the spinal cord, however, so even they control contralateral muscles.
Figure:descending tracts
The tectospinal tract begins in a midbrain region called the tectum and crosses to the contralateral side of the brainstem. In the lower medulla, it branches into lateral and medial tectospinal tracts of the upper spinal cord. These are involved in reflex movements of the head, especially in response to visual and auditory stimuli.
The lateral and medial reticulospinal tracts originate in the reticular formation of the brainstem. They control muscles of the upper and lower limbs, especially to maintain posture and balance.
The vestibulospinal tract begins in a brainstem vestibular nucleus that receives impulses for balance from the inner ear. The tract passes down the ventral column of the spinal cord and controls limb muscles that maintain balance and posture.
Poliomyelitis and Amyotrophic Lateral Sclerosis
Poliomyelitis and amyotrophic lateral sclerosis (ALS) are two diseases that involve destruction of motor neurons. In both diseases, the skeletal muscles atrophy from lack of innervations:
Poliomyelitis is caused by the poliovirus, which destroys motor neurons in the brainstem and ventral horn of the spinal cord.
Amyotrophic lateral sclerosis , in most cases of ALS, neurons are destroyed by an inability of astrocytes to reabsorb glutamate from the tissue fluid, allowing this neurotransmitter to accumulate to a toxic level.
Functions of spinal cord
The spinal cord serves three principal functions:
1. conduct information up and down between the brain and periphery.
2. Locomotion, motor neurons in the brain initiate walking and determine its speed, distance, and direction, but the simple repetitive muscle contractions that put one foot in front of another, over and over, are coordinated by groups of neurons called central pattern generators in the cord.
3. Reflexes. Reflexes are involuntary stereotyped responses to stimuli.
Spinal control of movement
There are three inputs to alpha motor neurons that determine which muscle fibers will contract: upper motor neurons, spinal interneurons, and sensory neurons.1. Upper motor neurons from the cortex or brainstem are important mediators of voluntary movements and are mainly inhibitory in nature.
2. Spinal interneurons may be excitatory or inhibitory and form an extensive circuitry within the spinal cord. Basic motor programs (e.g., walking) are encoded in spinal circuits known as central pattern generators, which include many spinal interneurons. Spinal circuits are accessed and modulated by higher centers as appropriate.
3. Sensory neurons from muscle proprioceptors provide feedback about muscle length and tension.
PROPRIOCEPTORS
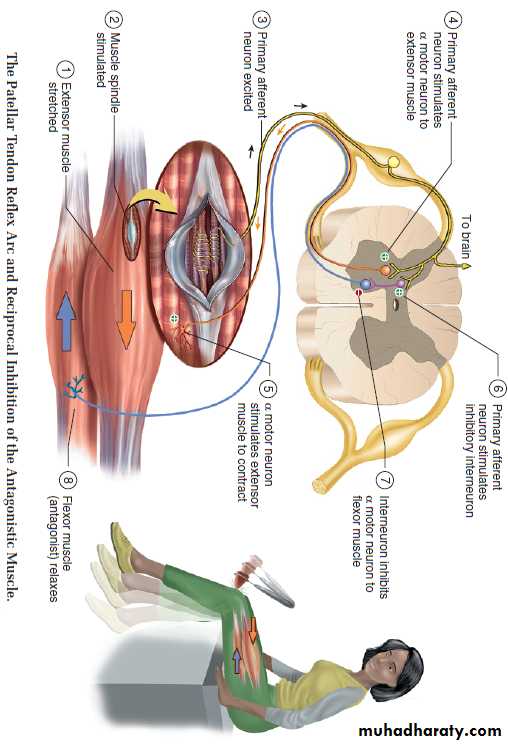
Sensory information about body position and its relationship to the environment is relayed from the vestibular, visual, and auditory systems. A large amount of somatosensory information comes from receptors (e.g., Pacinian corpuscles) in the skin and joint capsules. In addition, muscles contain two types of proprioceptors that provide feedback about muscle length and tension:1. Muscle spindles
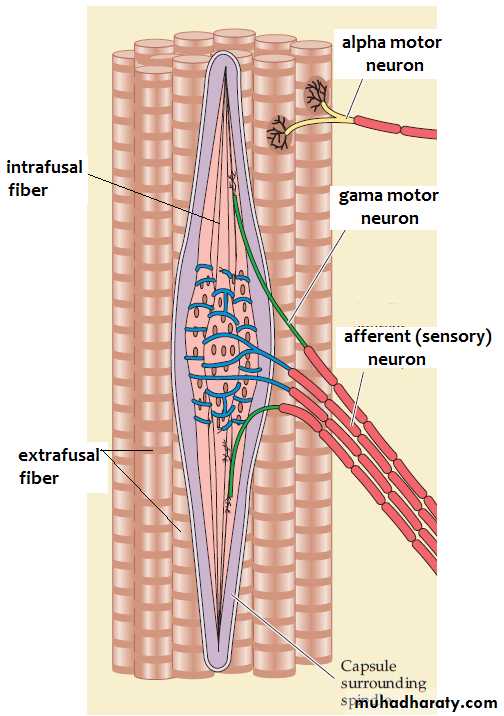
Muscle spindles provide information to the CNS about muscle (length) and the speed with which muscle length is changing. Muscle spindles are especially abundant in muscles that require fine control. each spindles are about 4 to 10 mm long, tapered at the ends, and scattered throughout the fleshy part of a muscle. A spindle contains 3 to 12 modified muscle (intrafusal) fibers and a few nerve fibers. There are two classes of intrafusal fibers: nuclear chain fibers, and nuclear bag fibers. Muscle spindles have three types of nerve fibers:
1. Primary afferent fibers(Ia), which end in annulospiral endings that coil around the middle of nuclear chain and nuclear bag fibers. These respond mainly to the onset of muscle stretch.
2. Secondary afferent fibers, which have flower-spray endings,(II) , wrapped primarily around the ends of the nuclear chain fibers. These respond mainly to prolonged stretch.
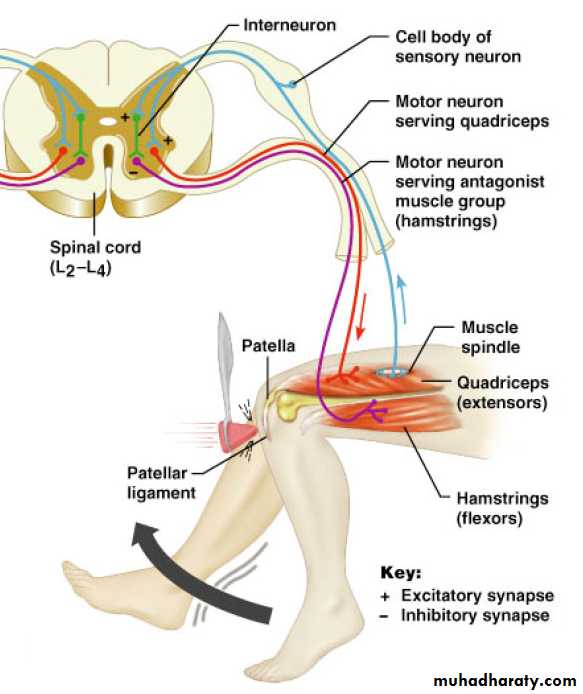
increased activity in afferent fibers of muscle spindle due to stretch of muscle activate the α motor neuron of same muscle and other synergistic muscles leading to contraction of these muscles, it also decrease the activity in α motor neuron of antagonist muscle leading to relaxation of these muscles.
3. Gamma (γ) motor neurons, which originate in the ventral horn of the spinal cord and lead to the contractile ends of the intrafusal fibers. The name distinguishes them from the alpha (α) motor neurons, which innervate the extrafusal fibers. Gamma motor neurons adjust the tension in a muscle spindle to variations in the length of the muscle. When a muscle shortens(contract by activity in α motor neurons) , the γ motor neurons stimulate the ends of the intrafusal fibers to contract slightly, this keeps the intrafusal fibers taut and responsive at all times and the process of simultaneous discharge of in α and γ motor called Alpha-Gamma Coactivation..
The stretch reflex arc of spindle is a negative feedback loop used to maintain muscle length at a desired value. The appropriate muscle length is specified by the activity of descending upper motor neuron pathways that influence the motor neuron pool. Deviations from the desired length are detected by the muscle spindles, since increases or decreases in the stretch of the intrafusal fibers alter the level of activity in the sensory axons that innervate the spindles. These changes lead in turn to adjustments in the activity of the α motor neurons, returning the muscle to the desired length by contracting the stretched muscle and relaxing the opposed muscle group, and by restoring the level of spindle activity to what it was before.
figure; Muscle spindles provide information to the CNS about muscle stretch
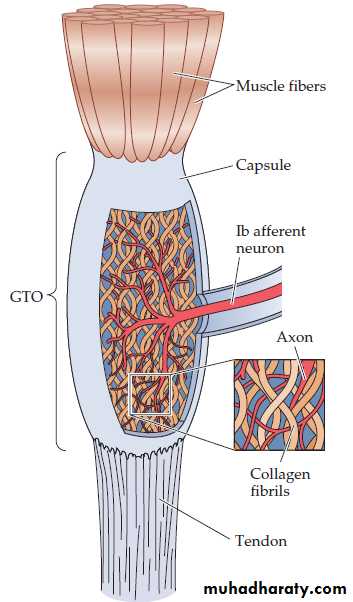
(length) and the speed with which muscle length is changing.2. Golgi tendon organs It is about 1 mm long and consists of an encapsulated tangle of knobby nerve endings entwined in the collagen fibers of the tendon. They are arranged in series with extrafusal muscles fibers. The sensory (afferent) fiber of golgi tendon are of type Ib fibers . When muscle contraction pulls on the tendon, the collagen squeeze the nerve endings between them. The nerve fiber sends signals to the spinal cord that provide the CNS with feedback on the degree of muscle tension at the joint. The Golgi tendon reflex is a response to excessive tension on the tendon. It inhibits α motor neurons to the muscle so the muscle does not contract as strongly to prevent tearing of muscle. The Golgi tendon reflex also functions when some parts of a muscle contract more than others. It inhibits the fibers connected with overstimulated tendon organs so that their contraction is more comparable to the contraction of the rest of the muscle. This reflex spreads the workload more evenly over the entire muscle, which is beneficial in such actions as maintaining a steady grip on a tool.
figure: Golgi tendon organs
ReflexReflexes are sudden, unlearned, involuntary, subconscious response to changes within or outside the body. Reflexes include glandular secretion and contractions of all three types of muscle. They also include some learned responses, such as the salivation of dogs in response to a sound they have come to associate with feeding time( conditioned reflexes). Reflexes are essential for
maintain homeostasis (autonomic reflexes) – heart rate, breathing rate, blood pressure, and digestion.
Reflexes also carry out the automatic action of swallowing, sneezing, coughing, and vomiting.
Reflexes maintain balance & posture. ex. Spinal reflexes – control trunk and limb muscles.
Spinal Reflexes
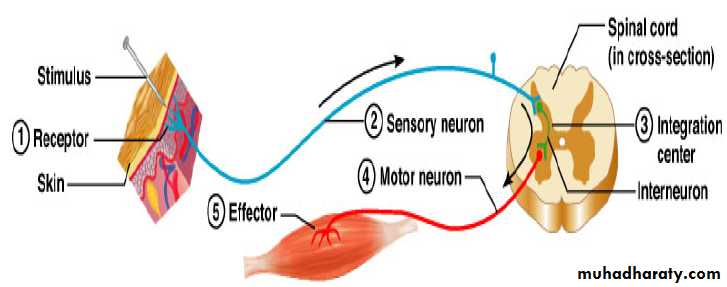
Spinal reflexes concerned with unlearned skeletal muscle reflexes that are mediated by the brainstem and spinal cord. They result in the involuntary contraction of a muscle—for example, the quick withdrawal of your hand from a hot stove or the lifting of your foot when you step on something sharp. They are somatic reflexes, and traditionally called spinal reflexes A somatic reflex employs a reflex arc, in which signals travel along the following pathway:1. somatic receptors in the skin, a muscle, or a tendon.
2. afferent nerve fibers, which carry information from these receptors into the dorsal horn of the spinal cord.
3. interneurons, which integrate information; these are lacking from some reflex arcs.
4. efferent nerve fibers, which carry motor impulses to the skeletal muscles.
5. effector, like skeletal muscles, the somatic effectors that carry out the response..
Figure: Reflex Arc.
Types of spinal motor reflexesI.The (flexor )withdrawal reflex and Crossed Extensor Reflex
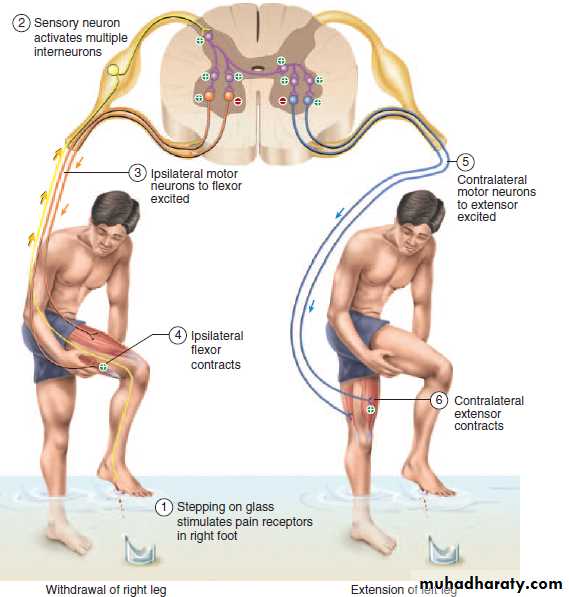
A flexor reflex is the quick contraction of flexor muscles resulting in the withdrawal of a limb from an injurious stimulus. For example, suppose you are wading in a lake and step on a broken bottle with your right foot. Even before you are consciously aware of the pain, you quickly pull your foot away before the glass penetrates any deeper. This action involves contraction of the flexors and relaxation of the extensors in that limb; the relaxation of the extensors is a case of reciprocal inhibition. The steps of the flexor withdrawal reflex response include:
1.Pain receptors are activated at the site of stimulation.
2. Afferent pain fibers enter the dorsal root and send collaterals to
Excitatory interneurons that synapse with alpha motor neurons serving flexors are stimulated. Contraction of flexors removes the limb from the aversive stimulus.
Reciprocal inhibition suppresses contraction of the extensors of the affected limb.
In this example, where one leg would suddenly be lifted, the person would rarely fall down because the postural support of the other limb would be simultaneously increased. This occurs due to an additional component of the flexorwithdrawal reflex, called the crossed extensor reflex. Spinal interneurons crossing the midline orchestrate the crossed extensor response in which extensors on the opposite side of the body contract and flexors relax.
Figure: The flexor withdrawal reflex pathway. If a painful stimulus is applied to one side of the body, flexors contract and extensors relax on that side to rapidly remove the body part from the stimulus. The opposite response occurs on the contralateral side of the body to maintain posture; this crossed extensor reflex is mediated by spinal interneurons.
II. The myotatic or stretch reflex
The myotactic (muscle stretch) reflex is demonstrated by tapping a tendon with a reflex hammer; for example, when testing the knee jerk reflex:1. Tapping the patellar tendon causes a small degree of stretch in the quadriceps muscle, which results in the generation of action potentials in Ia afferents from muscle spindles.
2. A monosynaptic reflex arc is formed when sensory afferents enter the spinal cord, via the dorsal root, and synapse directly on the alpha motor neurons; reflex contraction of the quadriceps causes the knee jerk response.
Figure: knee-jerk (patellar) reflex.
There are many other tendon reflexes:1.Biceps jerk reflex: the examiner places finger on the inside of the extended elbow over the tendon of the biceps muscle and the finger is tapped. The biceps contracts in response, and the forearm flexes at the elbow.
2.Triceps jerk reflex: tapping the short tendon of the triceps muscle
close to its insertion near the tip of the elbow extends the forearm.
3.Ankle – jerk reflex (plantar reflex): tapping the Achilles tendon just above its insertion on the Calcaneous lead to plantar flexion, produced by contraction of the gastrocnemius and the solues muscles.
Clinical significance
Testing somatic reflexes is valuable in diagnosing many diseases that cause exaggeration, inhibition, or absence of reflexes, such as neurosyphilis, diabetes mellitus, multiple sclerosis, alcoholism, electrolyte imbalances, andlesions of the nervous system. A lesion in any part of the myotactic reflex circuit will result in areflexia. The following deep tendon reflexes (and their associated spinal segments) are important to know when performing a neurologic examination:
■ Brachioradialis (C5–C6)
■ Biceps (C5–C6)
■ Triceps (C6–C7)
■ Knee (L2–L4)
■ Ankle (S1).
Cutaneous Innervation and Dermatomes
Each spinal nerve except C1 receives sensory input from a specific area of skin called a dermatome. A dermatome map is a diagram of the cutaneous regions innervated by each spinal nerve. Such a map is oversimplified, however, because the dermatomes overlap at their edges by as much as 50%. Therefore, severance of one sensory nerve root does not entirely deaden sensation from a dermatome. It is necessary to sever or anesthetize three successive spinal nerves to produce a total loss of sensation from one dermatome. Spinal nerve damage is assessed by testing the dermatomes with pinpricks and noting areas in which the patient has no sensation.Figure: A dermatome map
Spinal Cord TraumaComplete transection (severance) of the spinal cord causes immediate loss of motor control at and below the level of the injury. Transectio superior to segment C4 presents a threat of respiratory failure. Victims,also lose all sensation from the level of injury and below.In the early stage, victims exhibit a syndrome called spinal shock. The muscles below the level of injury
exhibit flaccid paralysis and an absence of reflexes because of the lack of stimulation from higher levels of the CNS. the patient typically lacks bladder and bowel reflexes and thus retains urine and feces. Lacking sympathetic stimulation to the blood vessels, a patient may exhibit neurogenic shock in which the vessels dilate and blood pressure drops dangerously low.Spinal shock can last from a few days to 3 months, but typically lasts 7 to 20 days. As spinal shock subsides, somatic reflexes begin to reappear, autonomic reflexes also reappear. Contrary to the earlier urinary and fecal retention, a patient now has the opposite problem, incontinence, as the rectum and bladder empty reflexively in response to stretch. Both the somatic and autonomic nervous systems typically exhibit exaggerated reflexes, a state called hyperreflexia or the mass reflex reaction.