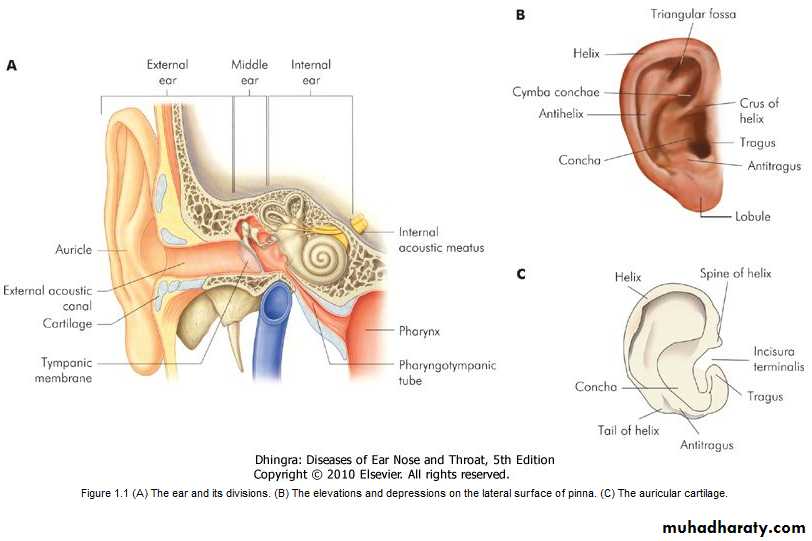
Anatomy of Ear THE EXTERNAL EAR The external ear consists of the (i) auricle or pinna, (ii) external acoustic canal and (iii) the tympanic membrane
1. Auricle or Pinna
The entire pinna, except its lobule, and the outer part of external acoustic canal are made up of a framework of a single piece of yellow elastic cartilage covered with skin. The latter is closely adherent to the perichondrium on its lateral surface while it is slightly loose on the medial surface.There is no cartilage between the tragus and crus of the helix, and this area is called the incisura terminalis . Cartilage from the tragus, perichondrium from the tragus or concha, and fat from the lobule are frequently used for reconstructive surgery of the middle ear.
2. External Acoustic (Auditory) Canal
It extends from the bottom of the concha to the tympanic membrane and measures about 24 mm along its posterior wall. It is not a straight tube; its outer part is directed upwards, backwards and medially while its inner part is directed downwards, forwards and medially.
The canal is divided into two parts: (a) cartilaginous and (b) bony.
(a) Cartilaginous PartIt forms outer one-third (8 mm) of the canal. Cartilage is a continuation of the cartilage which forms the framework of the pinna. The skin, covering the cartilaginous canal is thick and contains ceruminous and pilosebaceous glands which secrete wax. Hair is only confined to the outer canal and therefore furuncles (staphylococcal infection of hair follicles) are seen only in the outer one third of the canal.
(b) Bony Part
It forms inner two-thirds (16 mm). Skin lining the bony canal is thin and continuous over the tympanic membrane. It is devoid of hair and ceruminous glands. About 6 mm lateral to tympanic membrane, the bony meatus presents a narrowing called the isthmus. Foreign bodies lodged medial to the isthmus, get impacted, and are difficult to remove. Antero-inferior part of the deep meatus, beyond the isthmus, presents a recess called the anterior recess which acts as a cesspool for discharge and debris in cases of external and middle ear infections.3. Tympanic Membrane or the Drumhead
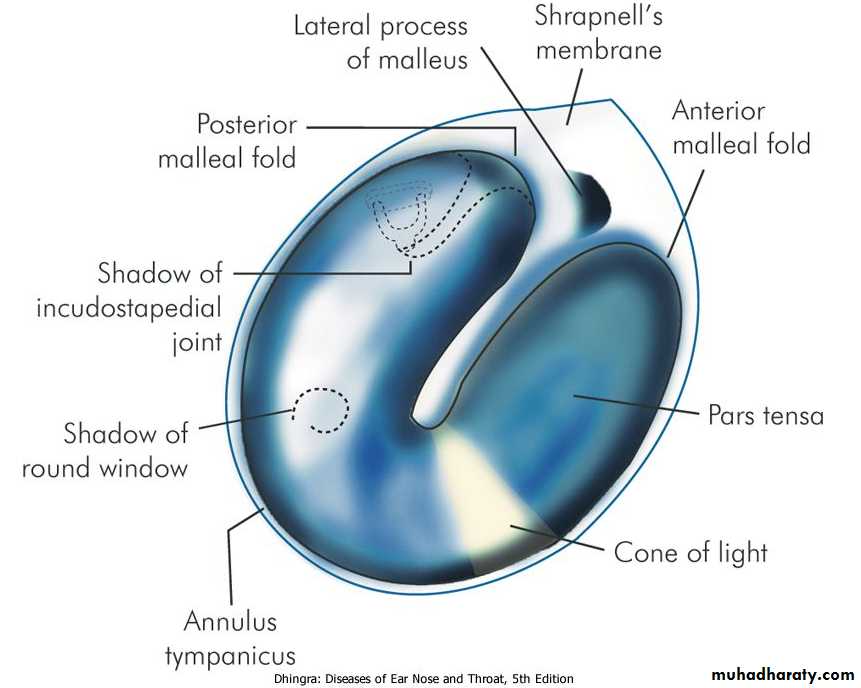
It forms the partition between the external acoustic canal and the middle ear. It is obliquely set and as a result, its posterosuperior part is more lateral than its antero-inferior part. It is 9-10 mm tall, 8-9 mm wide and 0.1 mm thick. Tympanic membrane can be divided into two parts:(a) Pars Tensa
It forms most of tympanic membrane. Its periphery is thickened to form a fibrocartilaginous ring called the annulus tympanicus which fits in the tympanic sulcus. The central part of pars tensa is tented inwards at the level of the tip of malleus and is called the umbo. A bright cone of light can be seen radiating from the tip of malleus to the periphery in the anteroinferior quadrant .(b) Pars Flaccida (Shrapnell's Membrane)
This is situated above the lateral process of malleus between the notch of Rivinus and the anterior and posterior malleal folds . It is not so taut and may appear slightly pinkish.
Tympanic membrane consists of three layers:
(i) Outer epithelial layer, which is continuous with the skin lining the meatus.(ii) Inner mucosal layer, which is continuous with the mucosa of the middle ear.
(iii) Middle fibrous layer, which encloses the handle of malleus.
Fibrous layer in the para flaccida is thin and not organised into various fibres as in pars tensa.
Figure 1.2 Landmarks of a normal tympanic membrane of right side.
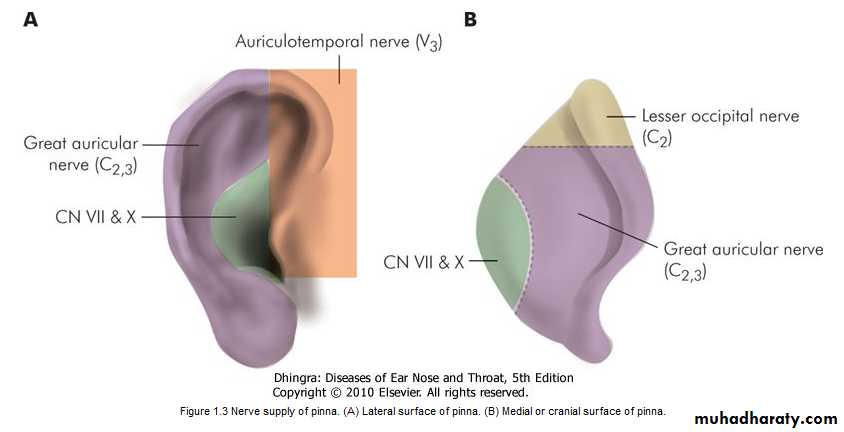
Nerve Supply of the External Ear
(i) Greater auricular nerve (C2,3) supplies most of the medial surface of pinna and only posterior part of the lateral surface .(ii) Lesser occipital (C2) supplies upper part of medial surface.
(iii) Auriculotemporal (V3) supplies tragus, crus of helix and the adjacent part of the helix with anterior wall of the EAC.
(iv) Auricular branch of vagus (CN X), also called Arnold's nerve, supplies the concha and corresponding eminence on the medial surface with the posterior wall of the EAC.
(v) Facial nerve, which is distributed with fibres of auricular branch of vagus, supplies the concha and retroauricular groove.
Figure 1.3 Nerve supply of pinna. (A) Lateral surface of pinna. (B) Medial or cranial surface of pinna.
THE MIDDLE EAR
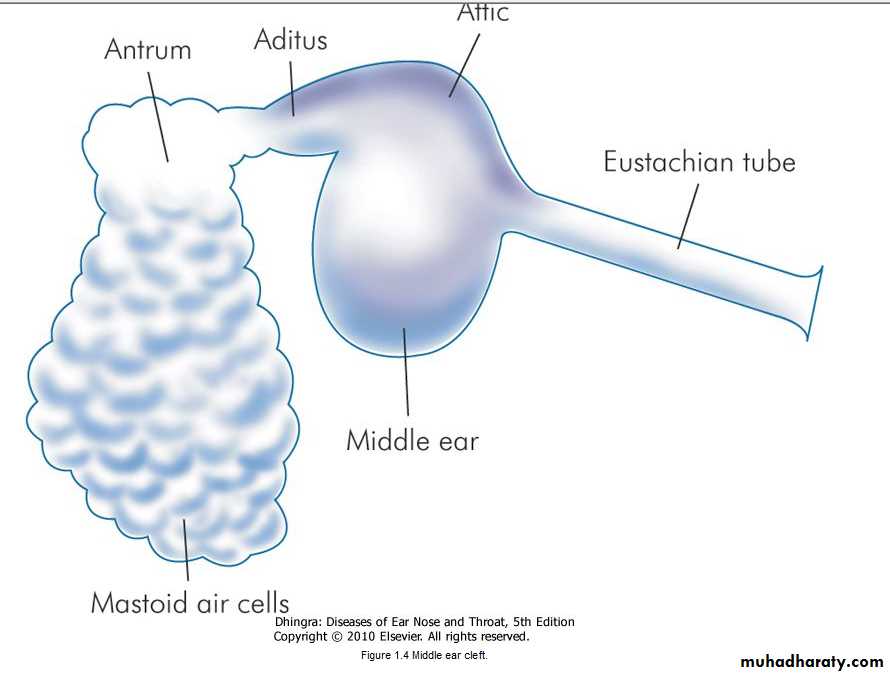
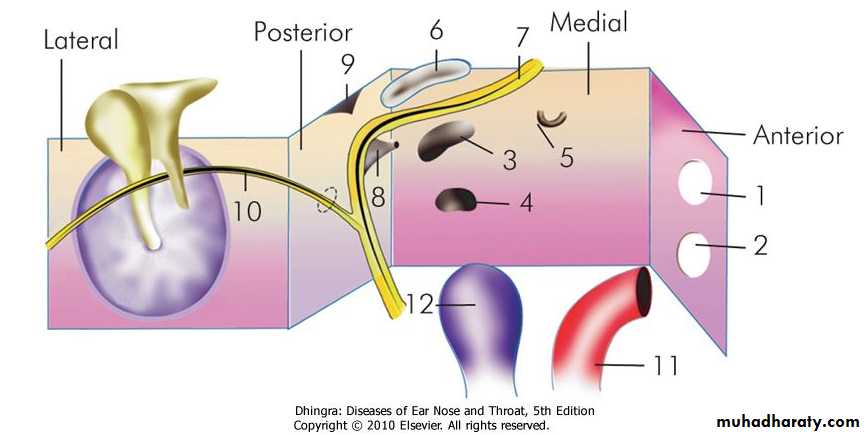
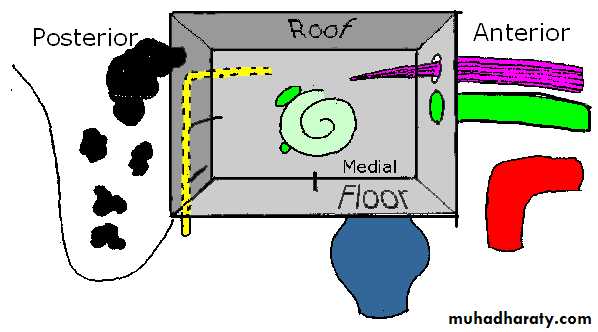
The middle ear together with the eustachian tube, aditus, antrum and mastoid air cells is called the middle ear cleft. It is lined by mucous membrane and filled with air.Middle ear can be likened to a six-sided box with a roof, a floor, medial, lateral, anterior and posterior walls .
The roof
is formed by a thin plate of bone called tegmen tympani. It also extends posteriorly to form the roof of the aditus and antrum. It separates tympanic cavity from the middle cranial fossa.The floor
is also a thin plate of bone which separates tympanic cavity from the jugular bulb. Sometimes, it is congenitally deficient and the jugular bulb may then project into the middle ear; separated from the cavity only by the mucosa.
The anterior wall
has a thin plate of bone which separates the cavity from internal carotid artery. It also has two openings; the lower one for the eustachian tube and the upper one for the canal of tensor tympani muscle.Figure 1.6 Walls of middle ear and the structures related to them.
Canal for tensor tympaniOpening of eustachian tube
Oval window
Round window
Processus cochleariformis
Horizontal canal
Facial nerve
Pyramid
Aditus
Chorda tympani
Carotid artery
Jugular bulb
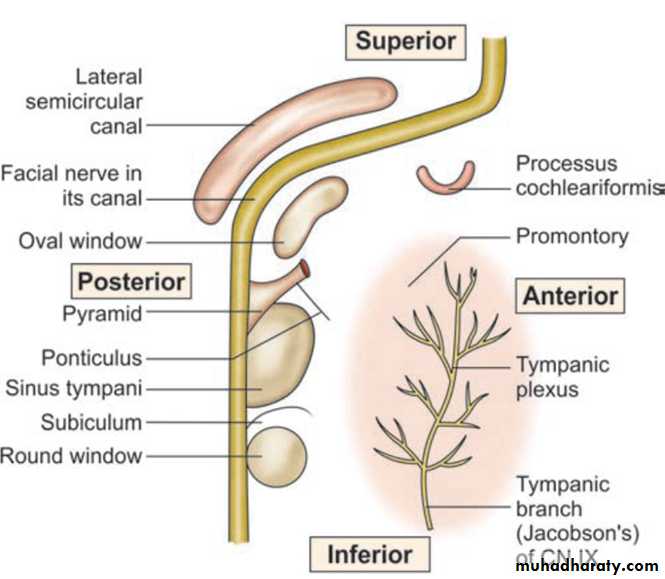
The posterior wall
lies close to the mastoid air cells. It presents a bony projection called the pyramid through the summit of which appears the tendon of the stapedius muscle to get attachment to the neck of stapes. Aditus, an opening through which attic communicates with the antrum, lies above the pyramid. Facial nerve runs in the posterior wall just behind the pyramid.
The medial wall
is formed by the labyrinth. It presents a bulge called promontory which is due to the basal coil of cochlea; oval window into which is fixed the footplate of stapes; round window or the fenestra cochleae which is covered by the secondary tympanic membrane. Above the oval window is the canal for facial nerve. Its bony covering may sometimes be congenitally dehiscent and the nerve may lie exposed making it very vulnerable to injuries or infection. Above the canal for facial nerve is the prominence of lateral semicircular canal. Just anterior to the oval window, the medial wall presents a hook-like projection called the processus cochleariformis. The tendon of tensor tympani takes a turn here to get attachment to the neck of malleus.The lateral wal
is formed largely by the tympanic membrane and to a lesser extent by the bony outer attic wall called the scutum..Mastoid Antrum
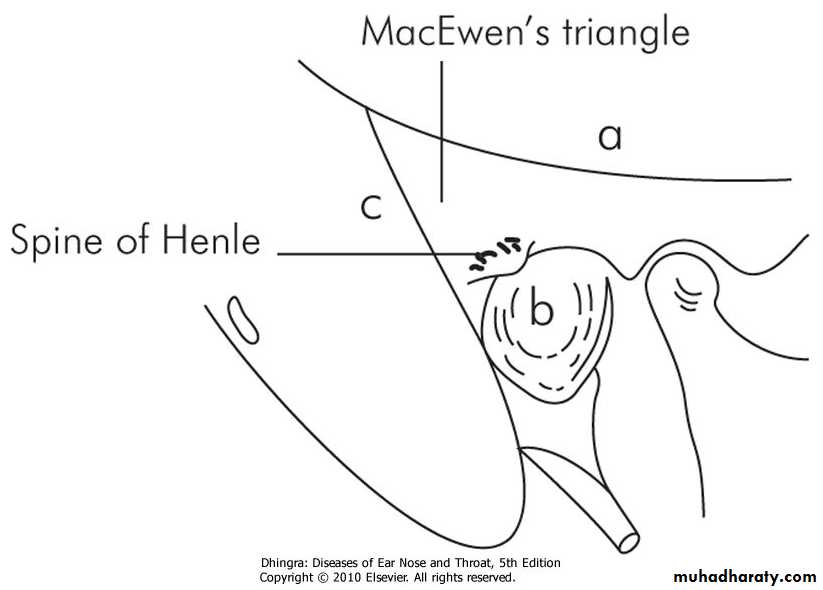
It is a large, air-containing space in the upper part of mastoid and communicates with the attic through the aditus. Its roof is formed by the tegmen antri which is a continuation of the tegmen tympani and separates it from the middle cranial fossa. The lateral wall of antrum is formed by a plate of bone which is on an average 1.5 cm thick in the adult. It is marked externally on the surface of mastoid by suprameatal (MacEwen's) triangle .Ossicles of the Middle Ear
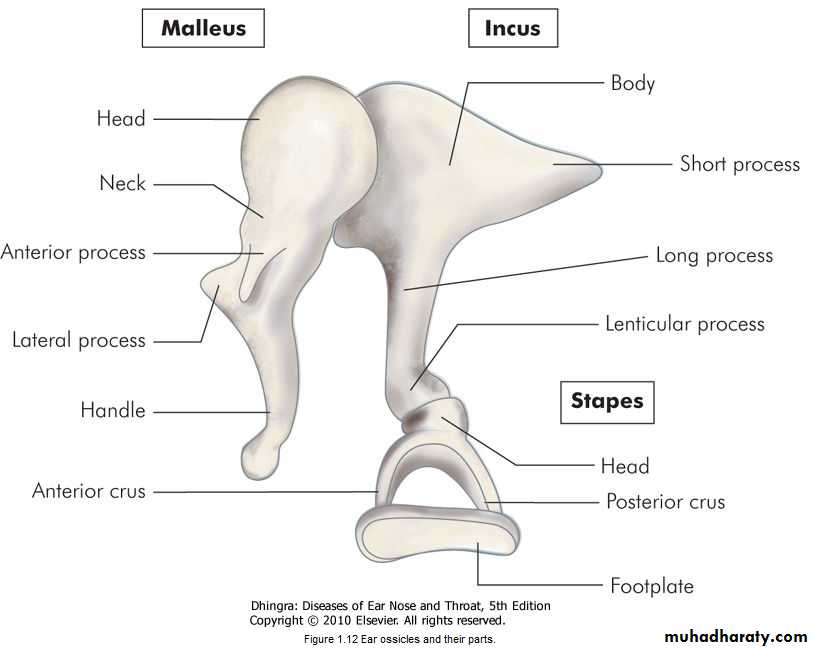
There are three ossicles in the middle ear-the malleus, incus and stapes.Intratympanic Muscles
There are two muscles-tensor tympani and the stapedius; the former attaches to the neck of malleus and tenses the tympanic membrane while the latter attaches to the neck of stapes and helps to dampen very loud sounds thus preventing noise trauma to the inner ear. Stapedius is a 2nd arch muscle and is supplied by a branch of CN VII while tensor tympani develops from the 1st arch and is supplied by a branch of mandibular nerve (V3).Tympanic Plexus
It lies on the promontory and is formed by (i) tympanic branch of glossopharyngeal and (ii) sympathetic fibres from the plexus round the internal carotid artery. Tympanic plexus supplies innervation to the medial surface of the tympanic membrane, tympanic cavity, mastoid air cells and the bony eustachian tube. It also carries secretomotor fibres for the parotid gland. Section of tympanic branch of glossopharyngeal nerve can be carried out in the middle ear in cases of Frey's syndrome.Chorda Tympani Nerve
It is a branch of the facial nerve which enters the middle ear through posterior canaliculus, and runs on the medial surface of the tympanic membrane between the handle of malleus and long process of incus, above the attachment of tendon of tensor tympani. It carries taste from anterior two-thirds of tongue and supplies secretomotor fibres to the submaxillary and sublingual salivary glands.Lining of the Middle Ear Cleft
Histologically, the eustachian tube is lined by ciliated epithelium which is pseudostratified columnar in the cartilaginous part, columnar in the bony part with several mucous glands in the submucosa. Tympanic cavity is lined by ciliated columnar epithelium in its anterior and inferior part which changes to cuboidal type in the posterior part. Epitympanum and mastoid air cells are lined by flat, nonciliated epithelium.
Blood Supply of Middle Ear
Middle ear is supplied by six arteries, out of which two are the main,(i) Anterior tympanic branch of maxillary artery which supplies tympanic membrane. (ii) Stylomastoid branch of posterior auricular artery which supplies middle ear and mastoid air cells.
Four minor vessels are:
(i) Petrosal branch of middle meningeal artery (runs along greater petrosal nerve). (ii) Superior tympanic branch of middle meningeal artery traversing along the canal for tensor tympani muscle. (iii) Branch of artery of pterygoid canal (runs along eustachian tube). (iv) Tympanic branch of internal carotid.Veins drain into pterygoid venous plexus and superior petrosal sinus
Lymphatic Drainage of Ear
AreaNodes
Concha, tragus, fossa triangularis and external cartilaginous canal
Preauricular and parotid nodes
Lobule and antitragus
Infra-auricular nodes
Helix and antihelix
Post-auricular nodes, deep jugular and spinal accessory nodes
Middle ear and eustachian tube
Retropharyngeal nodes → upper jugular chain
Inner ear
THE INTERNAL EAR
No lymphatics
Bony Labyrinth
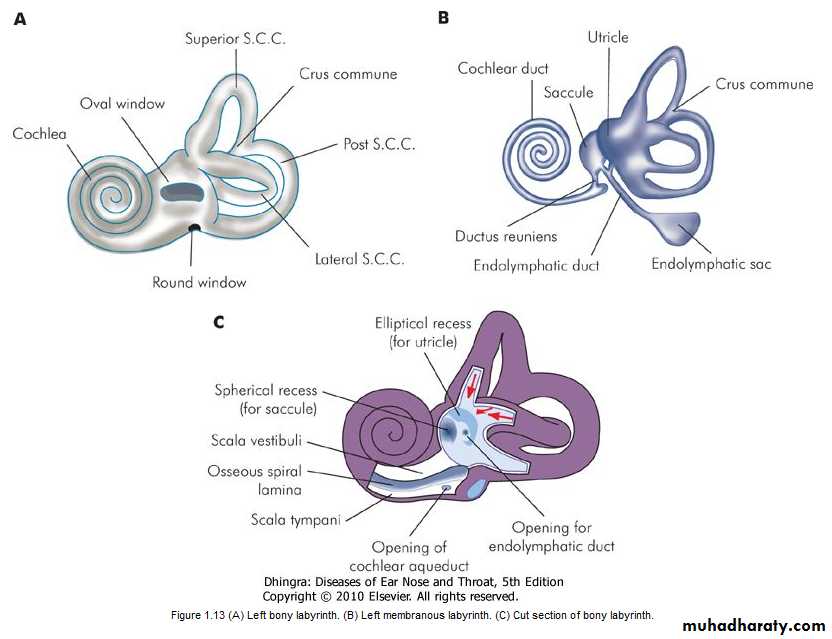
It consists of three parts: the vestibule, the semicircular canals and the cochlea.1. Vestibule
is the central chamber of the labyrinth. In its lateral wall lies the oval window. The inside of its medial wall presents two recesses, a spherical recess, which lodges the saccule and an elliptical recess which lodges the utricle. Below the elliptical recess is the opening of aqueduct of vestibule through which passes the endolymphatic duct. In the posterosuperior part of vestibule are the five openings of semicircular canals .2. Semicircular canals
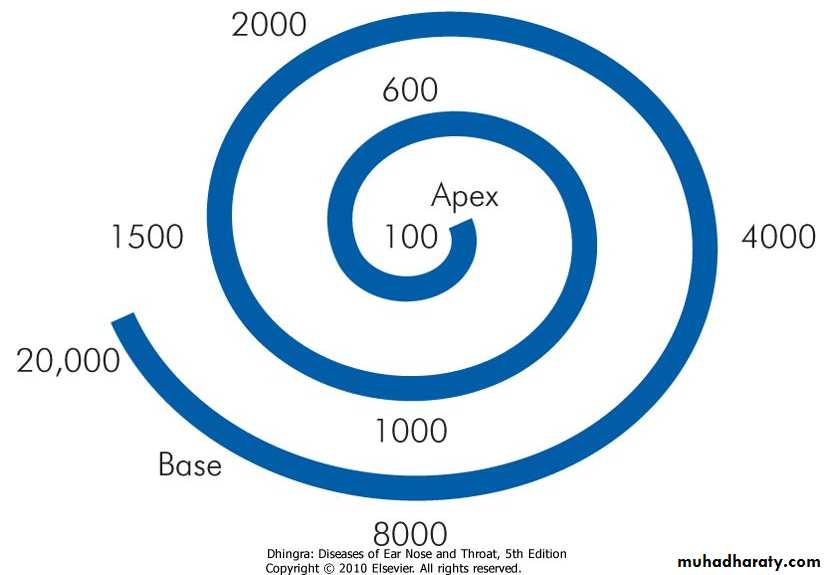
They are three in number, the lateral, posterior and superior, and lie in planes at right angles to one another. Each canal has an ampullated end which opens independently into the vestibule and a nonampullated end. The non-ampullated ends of posterior and superior canals unite to form a common channel called the crus commune. Thus, the three canals open into the vestibule by five openings.3. Cochlea
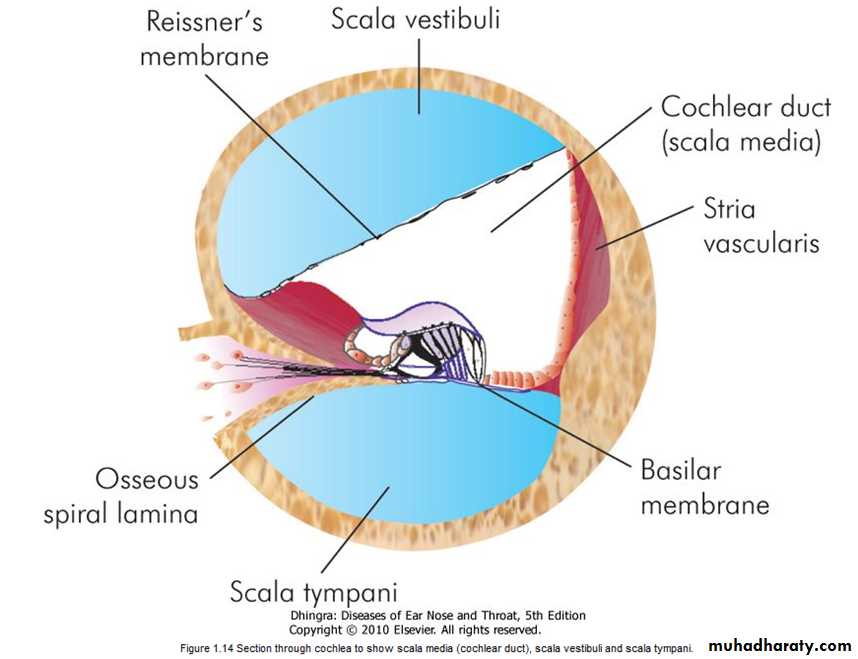
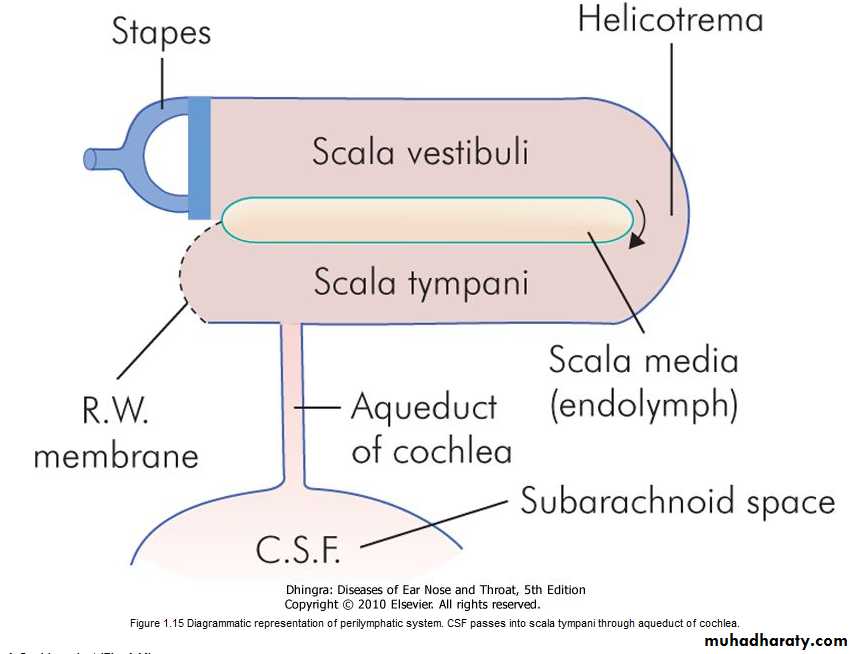
The bony cochlea is a coiled tube making 2.5 to 2.75 turns round a central pyramid of bone called the modiolus. The base of modiolus is directed towards internal acoustic meatus and transmits vessels and nerves to the cochlea. The bony bulge in the medial wall of middle ear-the promontory, is due to the basal coil of the cochlea. The bony cochlea contains three compartments: (a) scala vestibuli, (b) scala tympani, (c) scala media or the membranous cochlea .
The scala vestibuli and scala tympani are filled with perilymph and communicate with each other at the apex of cochlea through an opening called helicotrema. Scala vestibuli is closed by the footplate of stapes which separates it from the air-filled middle ear. The scala tympani is closed by secondary tympanic membrane; it is also connected with the subarachnoid space through the aqueduct of cochlea .
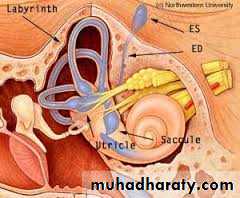
Membranous Labyrinth
It consists of the cochlear duct, the utricle and saccule, the three semicircular ducts, and the endolymphatic duct and sac.
1. Cochlear duct
Also called membranous cochlea or the scala media. It is a blind coiled tube. It appears triangular on cross-section and its three walls are formed by: (a) the basilar membrane, which supports the organ of corti,
(b) the Reissner's membrane which separates it from the scala vestibuli, (c) the stria vascularis, which contains vascular epithelium and is concerned with secretion of endolymph.
Cochlear duct is connected to the saccule by ductus reuniens
2. Utricle and saccule
The utricle lies in the posterior part of bony vestibule. It receives the five openings of the three semicircular ducts. It is also connected to the saccule through utriculosaccular duct. The sensory epithelium of the utricle is called the macula and is concerned with linear acceleration and deceleration. The saccule also lies in the bony vestibule, anterior to the utricle and opposite the stapes footplate. Its sensory epithelium is also called the macula. Its exact function is not known. It probably also responds to linear acceleration and deceleration. In Meniere's disease, the distended saccule lies against the stapes footplate and can be surgically decompressed by perforating the footplate.3. Semicircular ducts
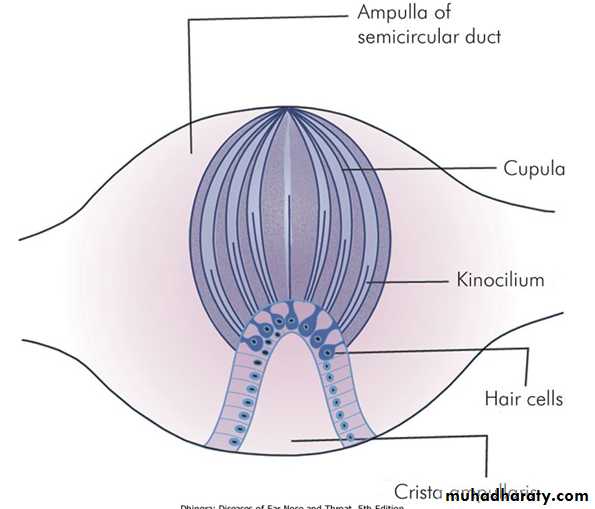
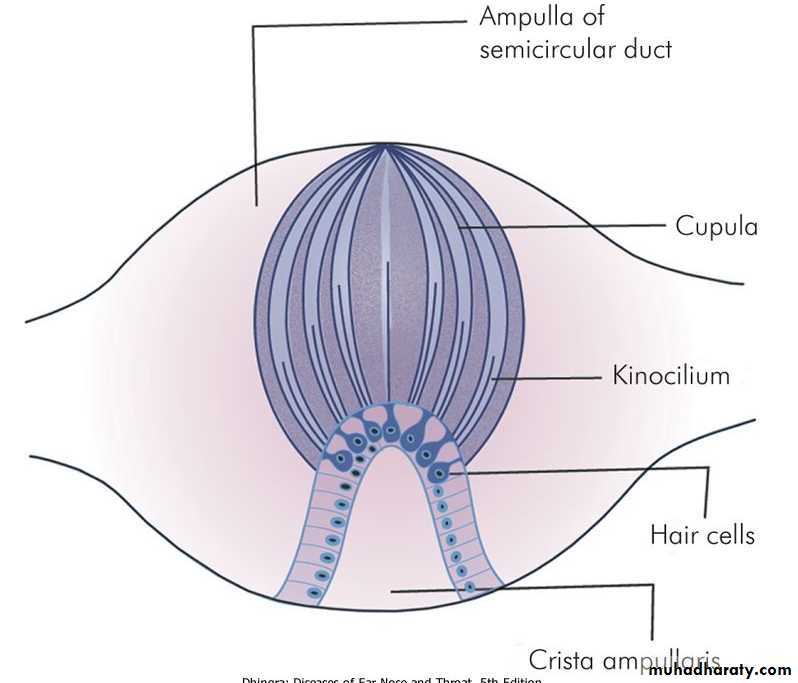
They are three in number and correspond exactly to the three bony canals. They open in the utricle. The ampullated end of each duct contains a thickened ridge of neuroepithelium called crista ampullaris.4. Endolymphatic duct and sac
Endolymphatic duct is formed by the union of two ducts, one each from the saccule and the utricle. It passes through the vestibular aqueduct. Its terminal part is dilated to form endolymphatic sac which lies between the two layers of dura on the posterior surface of the petrous bone.Endolymphatic sac is surgically important. It is exposed for drainage or shunt operation in Meniere's disease.
Inner Ear Fluids and their Circulation
There are two main fluids in the inner ear, perilymph and endolymph.Perilymph
resembles extracellular fluid and is rich in Na ions. It fills the space between the bony and the membranous labyrinth. It communicates with CSF through the aqueduct of cochlea which opens into the scala tympani near the round window.
Endolymph
fills the entire membranous labyrinth and resembles intracellular fluid, being rich in K ions. It is secreted by the secretory cells of the stria vascularis of the cochlea and by the dark cells of the vestibule.Blood Supply of Labyrinth
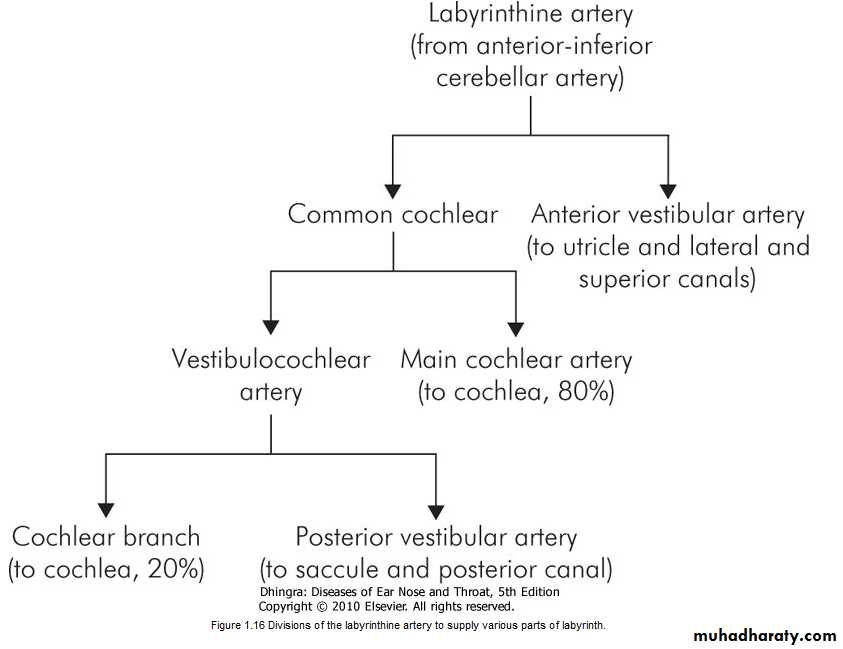
The entire labyrinth receives its arterial supply through labyrinthine artery which is a branch of anterior-inferior cerebellar artery but sometimes from the basilar.Venous drainage is through three veins, namely internal auditory vein, vein of cochlear aqueduct and vein of vestibular aqueduct which ultimately drain into inferior petrosal sinus and lateral venous sinus.
Figure 1.16 Divisions of the labyrinthine artery to supply various parts of labyrinth.
Eustachian Tube
Anatomy
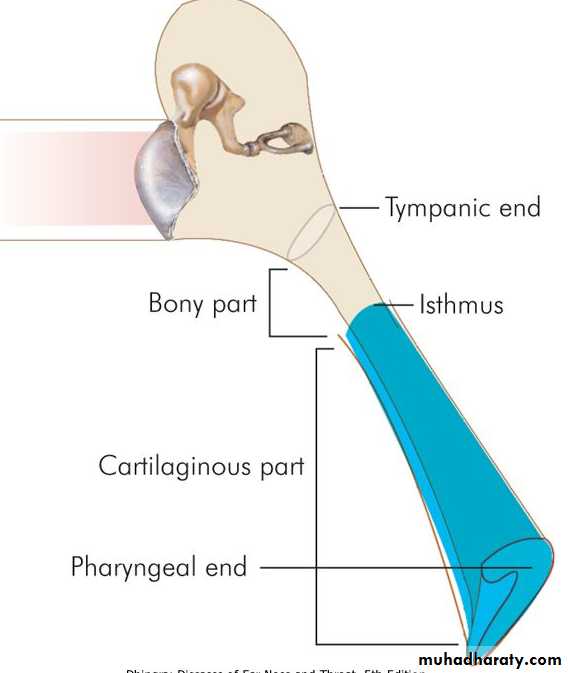
Eustachian tube, also called the auditory or the pharyngotympanic tube, connects nasopharynx with the tympanic cavity. In an adult, it is about 36 mm long and runs downwards, forwards and medially from its tympanic end, forming an angle of 45° with the horizontal. It is divided into two parts: The bony, which is posterolateral, forms one third (12 mm) of the total length and fibrocartilaginous, which is anteromedial, forms two-thirds (24 mm). The two parts meet at isthmus which is the narrowest part of the tube .The tympanic end of the tube is bony is situated in the anterior wall of middle ear, a little above the level of floor. The pharyngeal end of the tube is slit-like, vertically. The cartilage at this end raises an elevation called torus tubarius which is situated in the lateral wall of the nasopharynx, 1-1.25 cm behind the posterior end of inferior turbinate
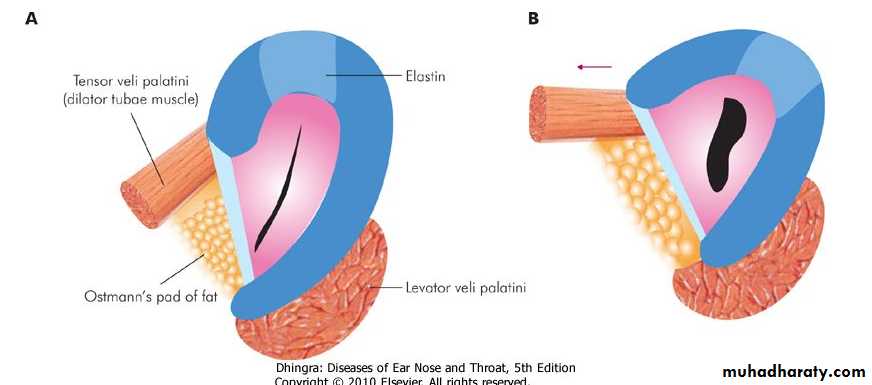
Muscles Related to Eustachian Tube
Three muscles are related to the tube: Tensor veli palatini, Levator veli palatini and the Salpingopharyngeus. The tensor veli palatine is attached to the lateral lamina of the tube, and help to open the tubal lumen. The exact role of the levator veli palatini and the Salpingopharyngeus muscles to open the tube is uncertain.Lining of the Eustachian Tube
Histologically, the mucosa shows pseudostratified ciliated columnar epithelium interspersed with mucous secreting goblet cells. The cilia beat in the direction of nasopharynx and thus helps to drain secretions and fluid from the middle ear into the nasopharynx.Nerve Supply
Tympanic branch of CN IX supplies sensory as well as parasympathetic secretomotor fibres to the tubal mucosa. Tensor veli palatini is supplied by mandibular branch of trigeminal (V3) nerve. Levator veli palatini and salpingopharyngeus receive motor nerve supply through pharyngeal plexus (Cranial part of CN XI through vagus).
Differences Between the Infant and Adult Eustachian Tube
The eustachian tube of infants is wider, shorter and more horizontal; thus infections from the nasopharynx can easily reach the middle ear. Even the milk may regurgitate into the middle ear if the infants are not fed in head-up positionFunctions
Physiologically, eustachian tube performs three main functions:1. Ventilation and thus regulation of middle ear pressure.
2. Protection against (a) Nasopharyngeal sound pressure and (b) Reflux of nasopharyngeal secretions.
3. Middle ear clearance of secretions
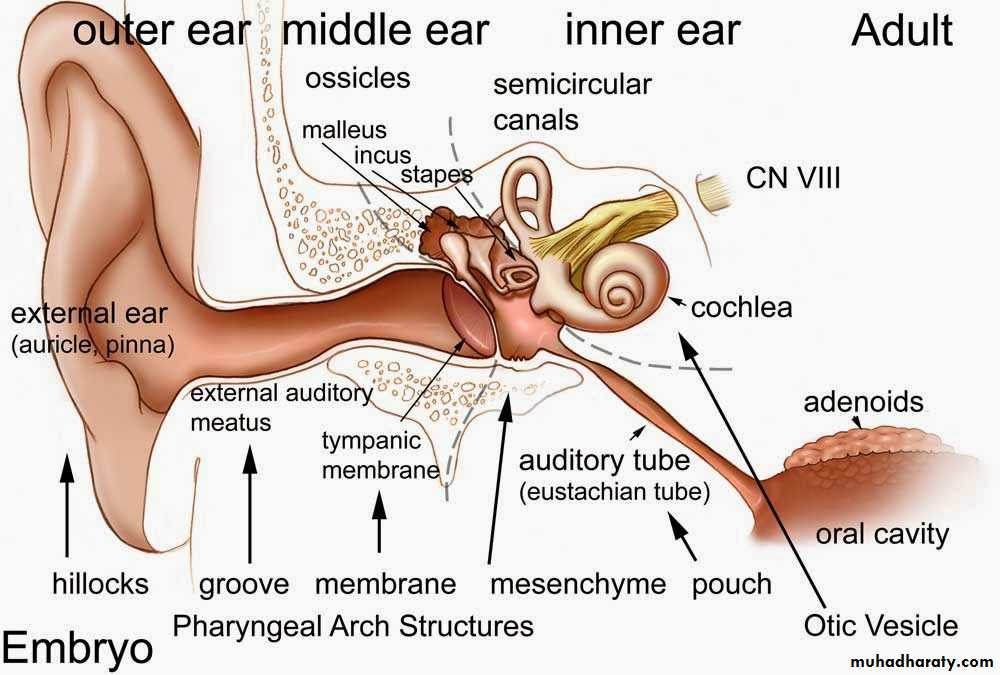
DEVELOPMENT OF EAR
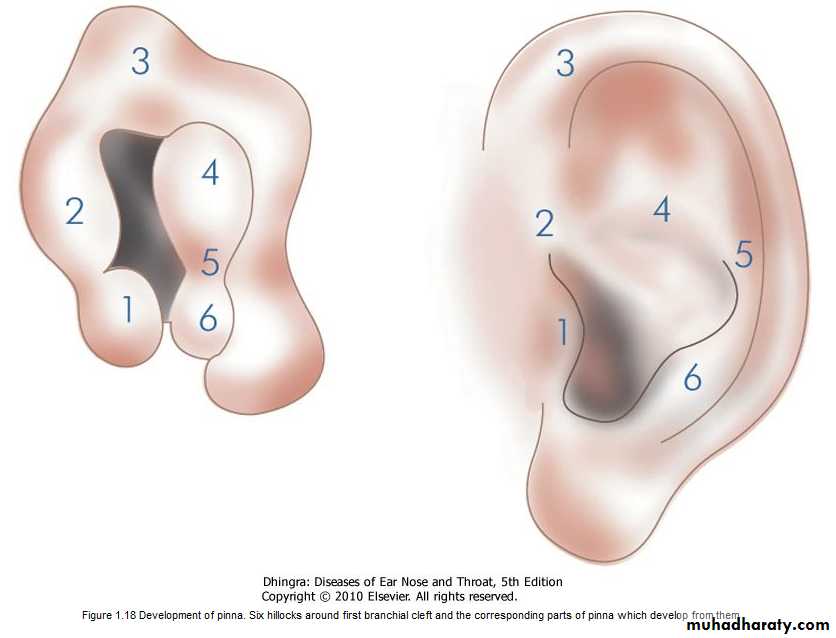
Auricle
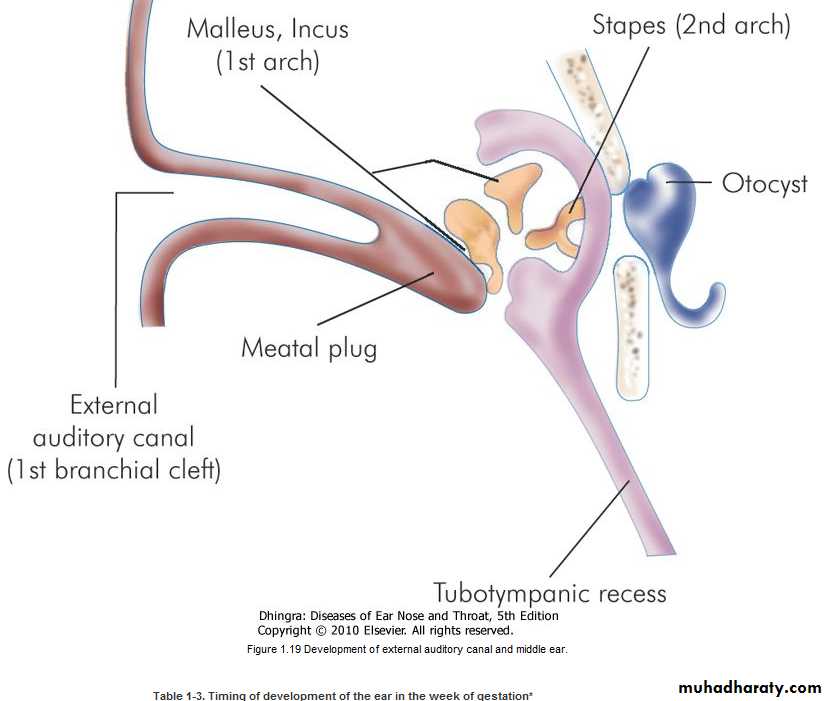
Around the sixth week of embryonic life, a series of six tubercles (hillocks of His) appear around the first branchial cleft. They progressively coalesce to form the auricle. By the 20th week, pinna achieves adult shape.External auditory meatus
develops from the first branchial cleft. By about the 16th embryonic week, ectodermal cleft forms a meatal plug. Recanalisation begins from the deeper part near the tympanic membrane and progresses outwards. External ear canal is fully formed by the 28th week of gestation.Tympanic membrane
develops from all the three germinal layers. Outer epithelial layer is formed by the ectoderm, inner mucosal layer by the endoderm and the middle fibrous layer by the mesoderm.
Middle ear cleft
The eustachian tube, tympanic cavity, attic, antrum and mastoid air cells develop from the endoderm of tubotympanic recess which arises from the first pharyngeal pouch .Malleus and incus are derived from mesoderm of the first arch while the stapes develop from the second arch .
Membranous inner ear
Development of the inner ear starts in the third week of foetal life and is complete by the 16th week(without end organs). Ectoderm in the region of hind brain thickens to form an auditory placode which is invaginated to form auditory vesicle or the otocyst. The latter then differentiates into the endolymphatic duct and sac; the utricle, the semicircular ducts; and saccule and the cochlea.
The cochlea is developed sufficiently by 20 weeks of gestation and the foetus can hear in the womb of the mother.
Peripheral Receptors and Physiology of Auditory and Vestibular Systems
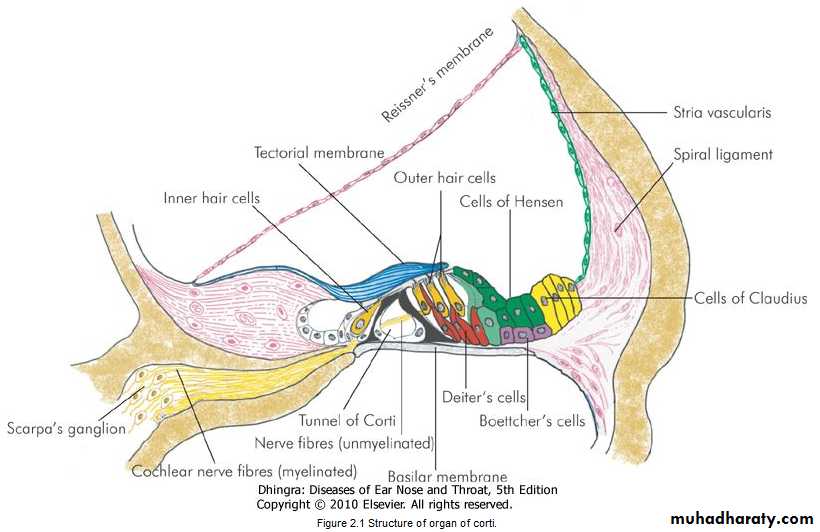
AUDITORY SYSTEMOrgan of Corti
Organ of corti is the sense organ of hearing and is situated on the basilar membrane. Important components of the organ of corti are:1. Tunnel of Corti
which is formed by the inner and outer rods.Figure 2.1 Structure of organ of corti.
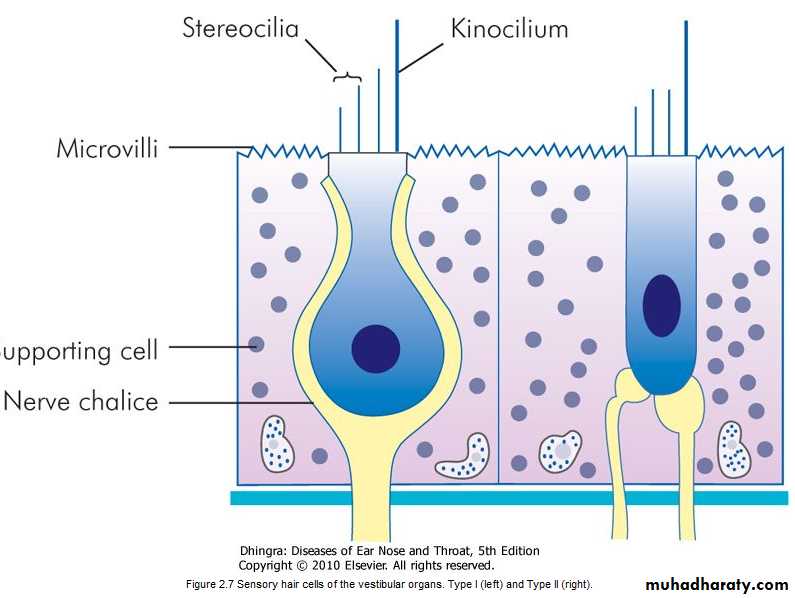
2. Hair cellsThey are important receptor cells of hearing and transduce sound energy into electrical energy.
3. Supporting cells
4. Tectorial membrane
It consists of gelatinous matrix with delicate fibres. It overlies the organ of Corti. The shearing force between the hair cells and tectorial membrane produces the stimulus to hair cellsDifferences between inner and outer hair cells
Inner hair cellsOuter hair cells
Total no.
3500
12,000
Rows
One row
Three or four rows
Shape
Flask-shaped
Cylindrical
Nerve supply
Primarily afferent fibres and very few efferent
Mainly efferent fibres and very few afferent
Development
Develop earlier
Develop late
Function
Transmit auditory stimuli
Modulate function of inner hair cells
Vulnerability
More resistant
Easily damaged by ototoxic drugs and high intensity noise
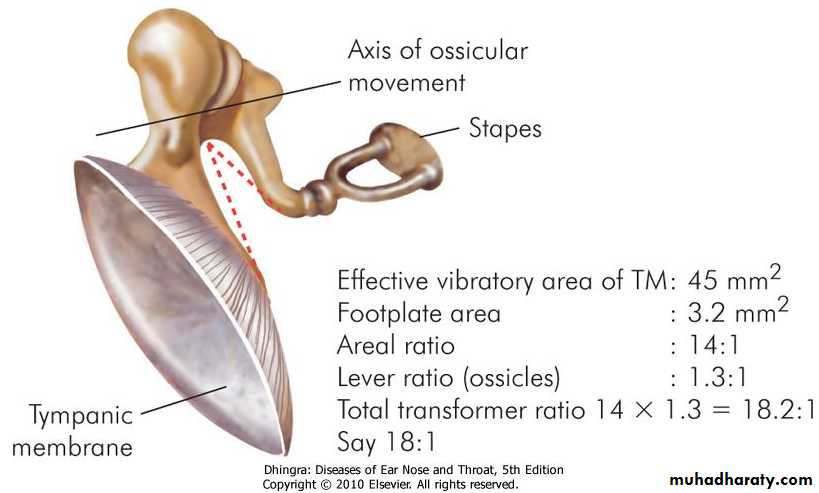
Mechanism of Hearing
A sound signal in the environment is collected by the pinna, passes through external auditory canal and strikes the tympanic membrane. Vibrations of the tympanic membrane are transmitted to stapes footplate through a chain of ossicles coupled to the tympanic membrane. Movements of stapes footplate cause pressure changes in the labyrinthine fluids which move the basilar membrane. This stimulates the hair cells of the organ of Corti. It is these hair cells which act as transducers and convert the mechanical energy into electrical impulses which travel along the auditory nerve. Thus, the mechanism of hearing can be broadly divided into:
1. Conduction of Sound
This function of the middle ear is called impedance matching mechanism or the transformer action.It is accomplished by:
(a) Lever action of the ossicles. Handle of malleus is 1.3 times longer than long process of the incus, providing a mechanical advantage of 1.3.(b) Hydraulic action of tympanic membrane. The area of tympanic membrane is much larger than the area of stapes footplate, the average ratio between the two being 21:1. As the effective vibratory area of tympanic membrane is only two-thirds, the effective areal ratio is reduced to 14:1.
2. Transduction of Mechanical Energy to Electrical Impulses
Figure 2.4 Frequency localisation in the cochlea. Higher frequencies are localised in the basal turn and then progressively decrease towards the apex.
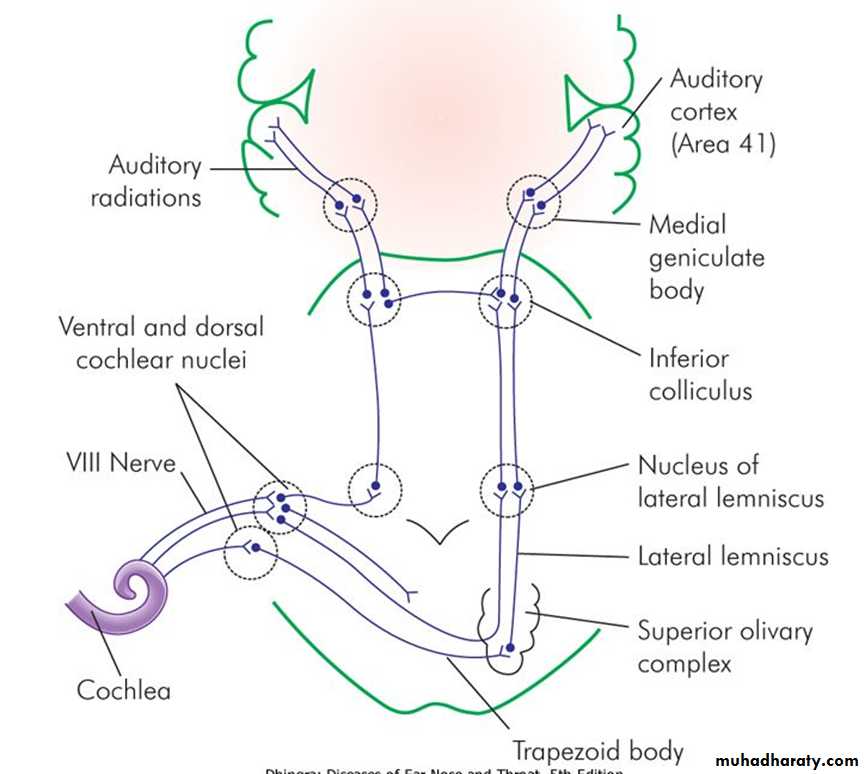
3. Neural Pathways
Hair cells get innervation from the bipolar cells of spiral ganglion. Central axons of these cells collect to form cochlear nerve which goes to cochlear nuclei. From there fibres travel to the superior olivary nucleus, lateral lemniscus, inferior colliculus, medial geniculate body and finally reach the auditory cortex of the temporal lobe.Auditory Neural Pathways and their Nuclei (Fig. 2.2)
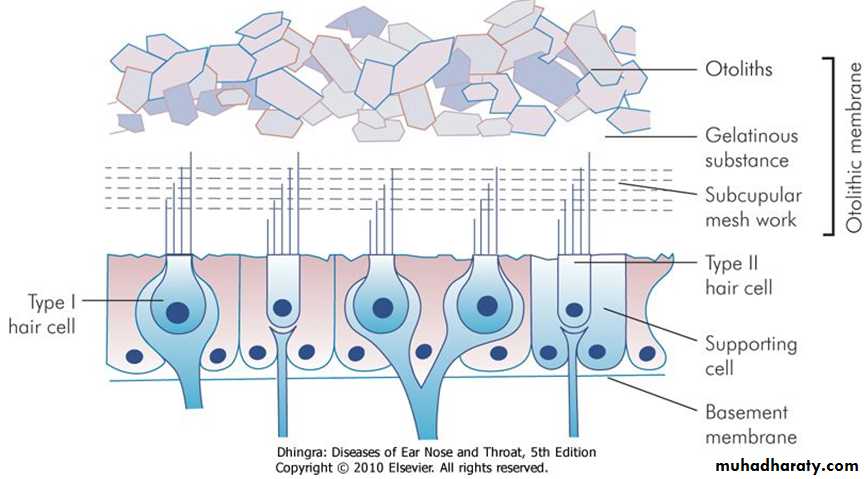
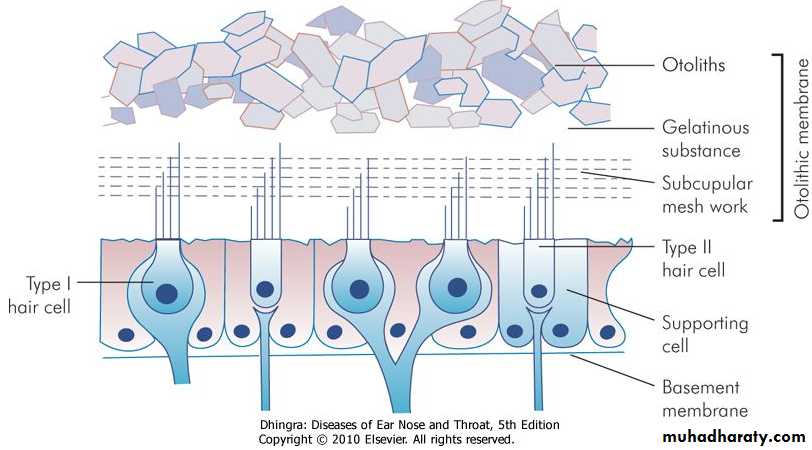
VESTIBULAR SYSTEMThe vestibular sense organ consists of the three semicircular canals, the saccule and the utricle. These are membranous tubes within the dense temporal bone, are fluid filled and have cells with cilia which bend as the fluid moves relative to them. This excites or depresses the nerve cells and alters the tonic input into the brain. The semicircular canals are at right angles to each other and detect changes in angular acceleration. The utricle and saccule have otoconia embedded in a gel overlying the cilia and are positioned to detect linear acceleration.
The nerve impulses from the labyrinth go to the vestibular nuclei in the brain stem. Here they are integrated with two other inputs that enable us to balance. The, two other inputs are vision and proprioception, from the joints, skin and muscle receptors. The neck and ankles are the most important
proprioceptive inputs. The brain stem computerizes these three inputs and with the help of the cerebellum maintains the balance and co-ordination of the head and body.
Peripheral Receptors
1. CristaeThey are located in the ampullated ends of the three semicircular ducts. These receptors respond to angular acceleration.
2. Maculae
They are located in otolith organs (i.e. utricle and saccule). They sense position of head in response to gravity and linear acceleration.