Fifth stage
Surgery
Lec-1
.د
علي
30/3/2017
Supracondylar Fractures of the Femur
Mechanism and classification:
Direct trauma is the usual cause.
The fracture line is just above the condyles, but may extend between them.
In the worst cases the fracture is severely comminuted.
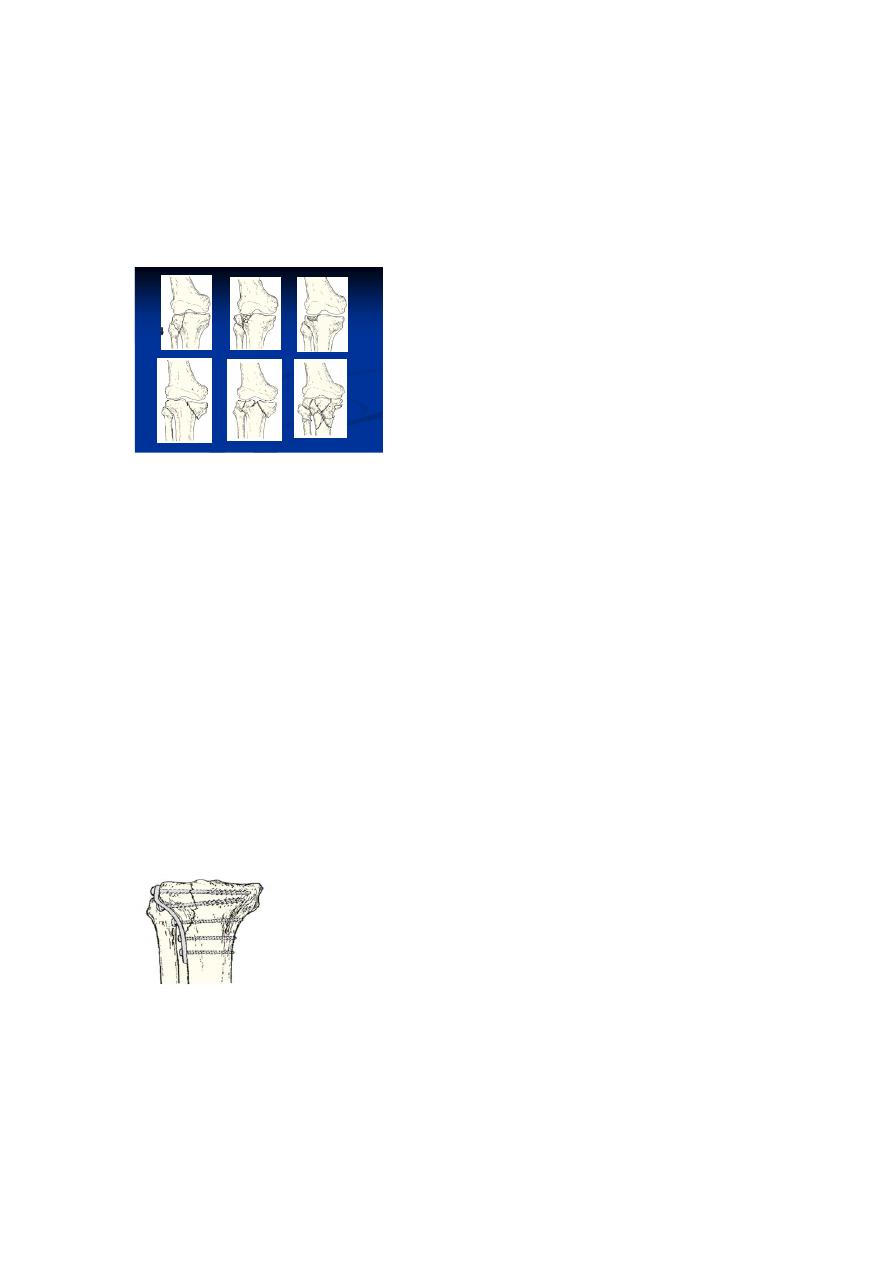
A useful classification is from the AO group:
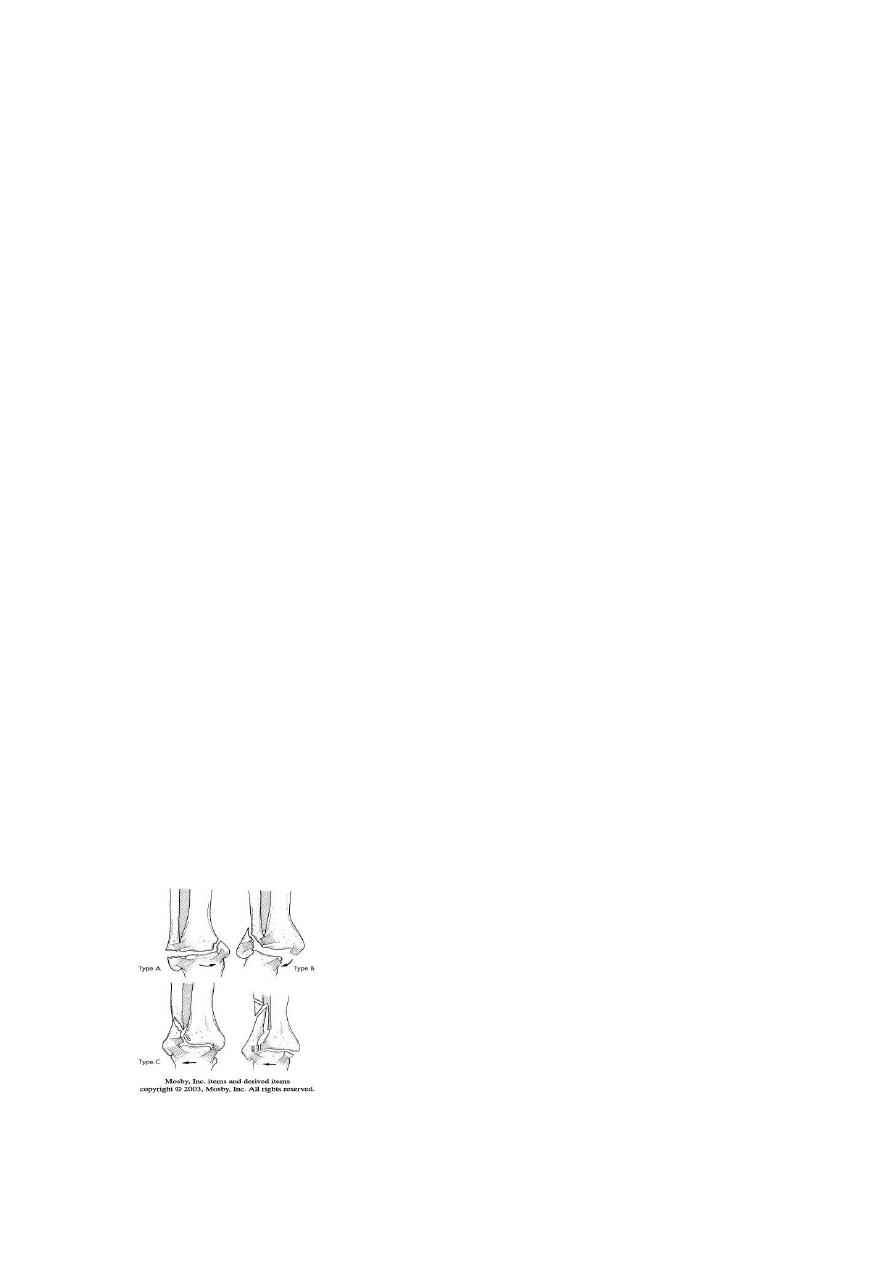
type A fractures have no articular splits and are truly ‘supracondylar’;
type B fractures are simply shear fractures of one of the condyles;
type C fractures have supracondylar and intercondylar fissures
a
a
b
c
Clinical features
The knee is swollen because of a haemarthrosis – this can be severe enough to cause
blistering later.
Movement is too painful to be attempted.
The tibial pulses should always be checked to ensure the popliteal artery was not injured in
the fracture.
X-RAY
The entire femur should be x-rayed so as not to miss a proximal fracture or dislocated hip.
In x- ray we see:
(a) whether there is a fracture into the joint and if it is comminuted.
(b) the size of the distal segment.
(c) whether the bone is osteoporotic.
These factors influence the type of internal fixation required.
مكتب الجامعة للطباعه واالستنساخ
عدد االوراق|
01
السعر|
011
Treatment
Non-operative
Traction:
If the fracture is only slightly displaced and extra-articular, it can be treated by traction
through the proximal tibia (skeletal traction) for 4 weeks then a functional-brace and the
patient allowed up and partially weight bearing with crutches.
Sometimes, the Distal fragment tilted backward by gastrocnemeous muscle.
Surgery
Operative treatment with internal fixation can enable accurate fracture reduction, especially
of the joint surface, and early movement.
If the necessary facilities and skill are available, this is the treatment of choice.
For the elderly, early mobilization is so important that internal fixation is almost obligatory.
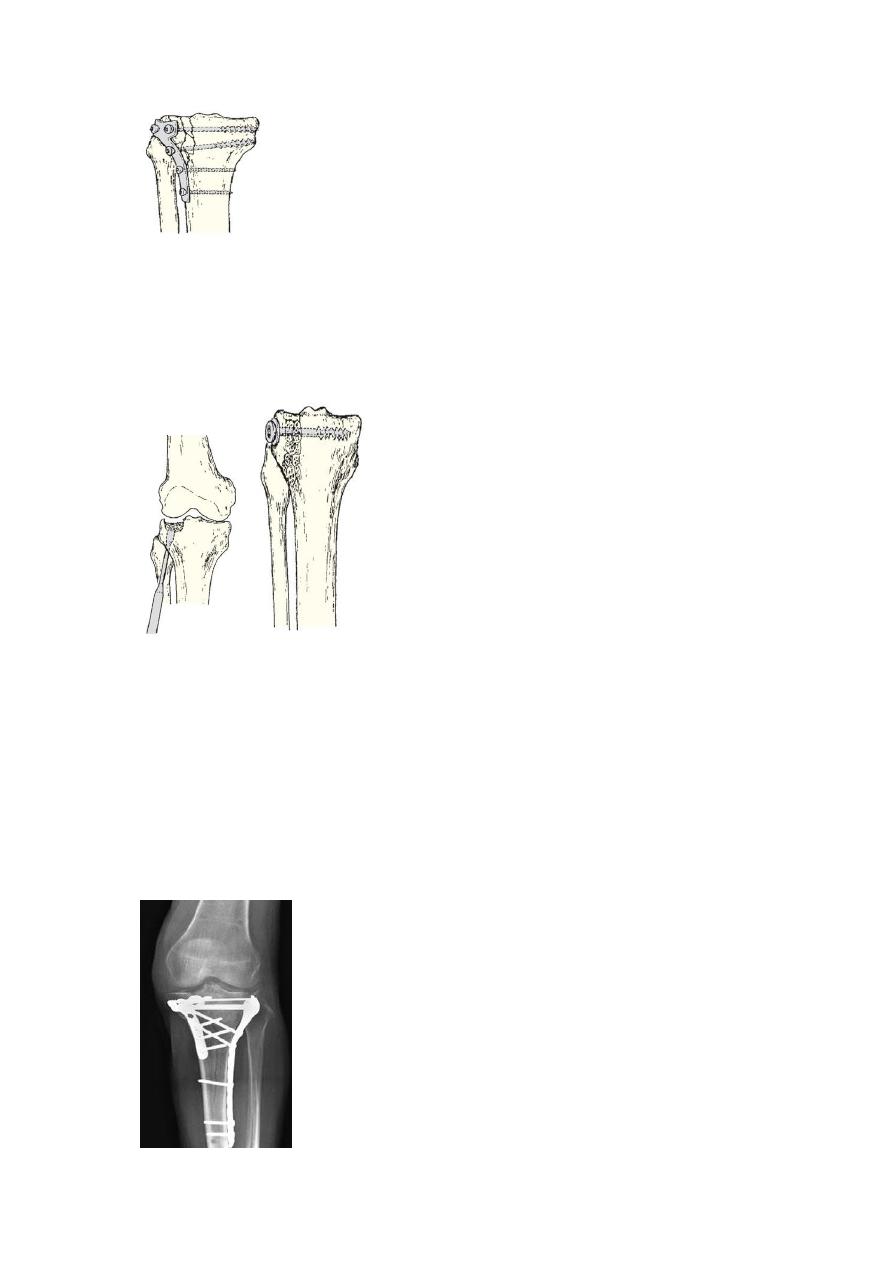
1. Fixed angle plate (90 degree) and screws (also called condylar plate)
2. Dynamic condylar screw.
3. Locked intramedullary nail ( in type 1)
4. Simple lag screws – these suffice for type B fractures
Complications:
1. Vascular injury
2. Joint stiffness
3. Malunion
DISLOCATION OF KNEE
The knee can be dislocated only by considerable violence, as in a road accident.
The cruciate ligaments and one or both lateral ligaments are torn.
Clinical features
Rupture of the joint capsule produces a leak of the haemarthrosis, leading to severe bruising
and swelling.
This may be the only clue on inspection, especially if the dislocated joint has reduced
spontaneously. Otherwise, the diagnosis is straight forward as there is gross deformity
The circulation in the foot must be examined because the popliteal artery may be torn or
obstructed.
Repeated examination is necessary as compartment syndrome is also a risk.
Common peroneal nerve injury occurs in nearly 20 per cent of cases; distal sensation and
movement should be tested.
Treatment:
Reduction under anaesthesia is urgent. If reduction is achieved, the limb is rested on a back-
splint and the circulation is checked repeatedly during the 48 hours.
In general, early reconstruction of the torn ligaments followed by protected movement of
the joint reduces the severity of joint stiffness.
The cruciate ligaments can be reconstructed after knee movement has recovered, usually
some 6–12 months later.

Complications:
Vascular injury, compartment syndrome, nerve injury, joint instability, stiffness.
FRACTURED PATELLA
The patella is a sesamoid bone in continuity with the quadriceps tendon and the patellar
ligament (also called the patellar tendon).
There are additional insertions from the vastus medialis and lateralis into the medial and
lateral edges of the patella.
The mechanical function of the patella is to hold the entire extensor ‘strap’ away from the
centre of rotation of the knee, thereby lengthening the anterior lever arm and increasing the
efficiency of the quadriceps.
The key to the management of patellar fractures is the state of the entire extensor
mechanism.
If the extensor retinacula are intact, active knee extension is still possible, even if the patella
itself is fractured.
Mechanism of injury
Direct injury – usually a fall onto the knee or a blow against the dashboard of a car – causes
either an undisplaced crack or else a comminuted (‘stellate’) fracture without severe
damage to the extensor expansions.
Indirect injury occurs, typically, when someone catches the foot against a solid obstacle and,
to avoid falling, contracts the quadriceps muscle forcefully.
This is a transverse fracture with a gap between the fragments.
Clinical features:
History of trauma; the knee becomes swollen and painful. There may be an abrasion or
bruising over the front of the joint. The patella is tender and sometimes a gap can be felt.
Active knee extension should be tested. If the patient can lift the straight leg, the quadriceps
mechanism is still intact.
Usually there is an haemarthrosis, aspiration may reveal the presence of blood and fat
droplets.
X-ray:
The x-ray may show
1. one or more fine fracture lines without displacement.
2. multiple fracture lines with irregular displacement. (Stellate fracture).
3. a transverse fracture with a gap between the fragments.
Treatment
1. Undisplaced or minimally displaced fractures:
If there is a haemarthrosis it should be aspirated. The extensor mechanism is intact and
treatment is mainly protective.
A plaster cylinder holding the knee straight should be worn for 3–4 weeks, and during this
time quadriceps exercises are to be practised every day.
2. Comminuted (stellate) fracture:
The extensor expansions are intact and the patient may be able to lift the leg. However, the
undersurface of the patella is irregular and there is a serious risk of damage to the
patellofemoral joint. For this reason some people advocate patellectomy, whatever the
degree of displacement.
3. Displaced transverse fracture:
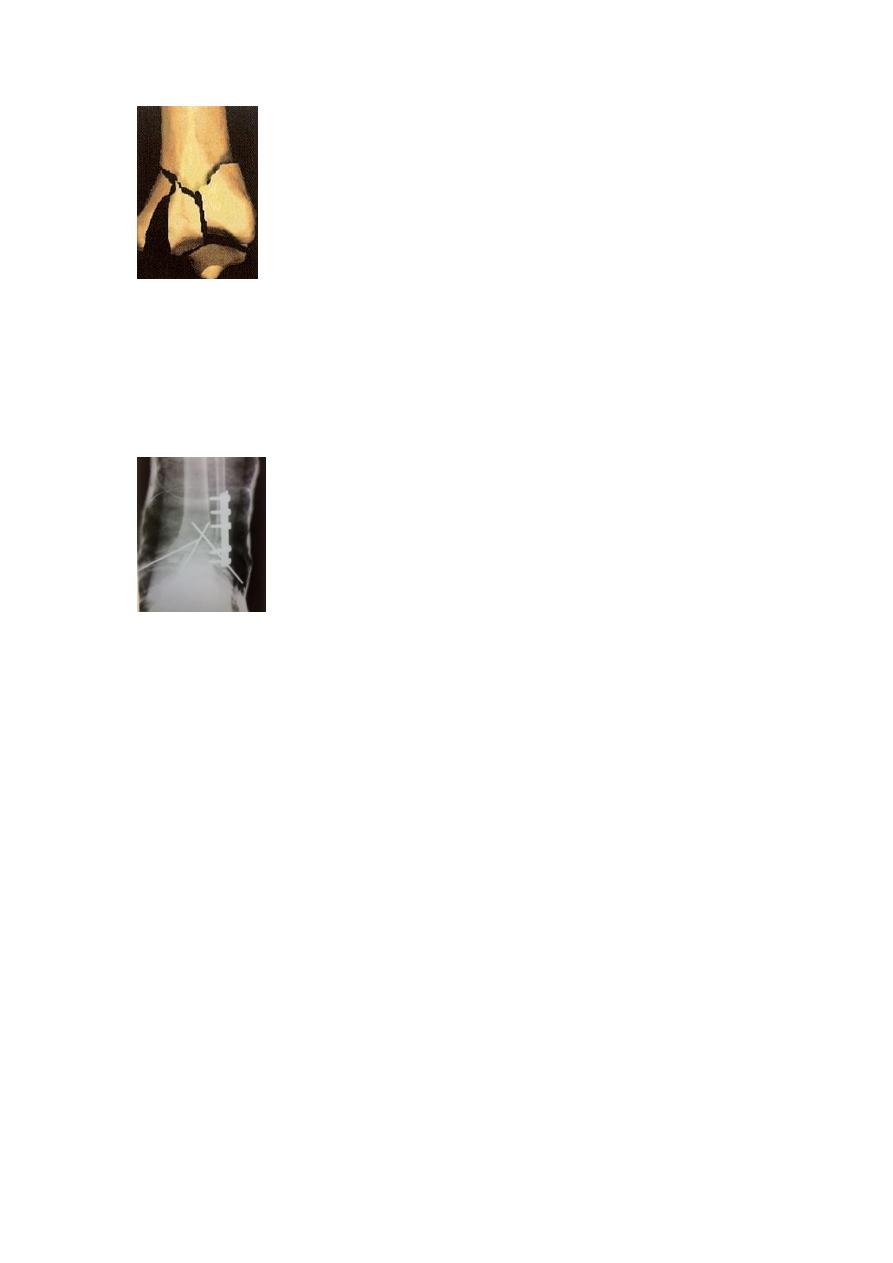
The lateral expansions are torn and the entire extensor mechanism is disrupted. Operation
is essential.
Open reduction and internal fixation by 2 parallel K -wires, with tension band wire.
The tears in the extensor expansions are then repaired. A plaster back slab applied

Outcome
Patients usually regain good function but, depending on the severity of the injury, there is a
significant incidence of late patellofemoral osteoarthritis.
DISLOCATION OF PATELLA
Because the knee is normally angled in slight valgus, there is a natural tendency for the
patella to pull towards the lateral side when the quadriceps muscle contracts.
Mechanism of injury
Mostly due to indirect force: sudden, severe contraction of the quadriceps muscle while the
knee is stretched in valgus and external rotation.
Predisposing factors:
1. anatomical variations such as genu valgum, tibial torsion, high-riding patella (patella
alta).
2. a shallow intercondylar groove.
3. patellar hypermobility due to generalized ligamentous laxity or localized muscle
weakness.
Clinical features
In a ‘first-time’ dislocation the patient may fell a tearing sensation and a feeling that the
knee has gone ‘out of joint’; when running, he or she may collapse and fall to the ground.
There is deformity: the displaced patella, seated on the lateral side of the knee, is not easily
noticed but the uncovered medial femoral condyle is unduly prominent and may be
mistaken for the patella.
The knee is swollen and there may be bruising and tenderness on the medial side.
Aspiration may show that the fluid is bloodstained;

The presence of fat droplets suggests osteochondral fracture.
Treatment
In most cases the patella can be pushed back into place without much difficulty and
anaesthesia is not always necessary; the exception is an intra-articular (intercondylar)
dislocation, which may need open reduction.
Back slab for 2-3 weeks and quadriceps strengthening exercise for 2-3 months.
Complication
1. Recurrent patella dislocation
2. Stiffness
3. Osteoarthritis of patelofemoral joint.
TIBIAL PLATEAU FRACTURES
Mechanism of injury
Fractures of the tibial plateau are caused by a varus or valgus force combined with axial
loading (a pure valgus force is more likely to rupture the ligaments).
This is sometimes the result of a car striking a pedestrian (hence the term ‘bumper
fracture’); more often it is due to a fall from a height in which the knee is forced into valgus
or varus. The tibial condyle is crushed or split by the opposing femoral condyle, which
remains intact.
A useful classification is that of Schatzker:
Type 1 – a vertical split of the lateral condyle.
Type 2 – a vertical split of the lateral condyle combined with depression of an adjacent load
bearing part of the condyle.
Type 3 – depression of the articular surface with an intact condylar rim.
Type 4 – fracture of the medial tibial condyle.
The momentary varus angulation may be severe enough to cause a rupture of the lateral
collateral ligament and a traction injury of the peroneal nerve. The severity of these injuries
should not be underestimated.
Type 5 – fracture of both condyles Both condyles are split
Type 6 – combined condylar and subcondylar fractures
Clinical features
The knee is swollen and may be deformed. Bruising is usually extensive and
the tissues feel ‘doughy’ because of haemarthrosis.
More importantly, the leg and foot should be carefully examined for signs of
vascular or neurological injury.
Traction injury of the peroneal or tibial nerves is not uncommon and it is
important to establish whether this is present at the time of admission and
before operation.
Imaging
Anteroposterior, lateral and oblique x-rays will usually show the fracture.
But the amount of comminution or plateau depression may not be appreciated
without computer tomography (CT).
Treatments
Type 1 fractures Undisplaced type 1 fractures can be treated conservatively (splint).
Displaced type need open reduction and internal fixation.
Type 2 fractures If depression is slight (less than 5 mm) and the knee is not unstable, or if the
patient is old and frail or osteoporotic, the fracture is treated closed with the aim of
regaining mobility and function rather than anatomical restitution.
In younger patients, and more so in those with a central depression of more than 5 mm,
open reduction with elevation of the plateau and internal fixation is often preferred.
Type 3:
The depressed fragments may need to be elevated through a window in the metaphysis;
The elevated fragments are supported with bone grafts and the whole segment is fixed in
position with ‘raft’ screws.
Type 4 fracture of the medial condyle:
Medial condylar split fractures usually occur in younger people and are caused by high-
energy trauma.
There is often an underlying ligament injury on the lateral side. Stable fixation of the medial
side then allow an assessment of the ligament injury. If the joint is unstable after fracture
fixation, the torn structures on the lateral side may need repair.
Types 5 and 6 fractures These are severe injuries that carry the added risk of a compartment
syndrome.

it is more usual to consider stable internal fixation and early joint movement for these
injuries, but surgery is not without significant risk.
The danger is that the wide exposure necessary to gain access to both condyles may strip
the supporting soft tissues, thus increasing the risk of wound breakdown and delayed union
or non-union.
complications
1. Compartment syndrome
2. Stiffness
3. Deformity
4. Osteoarthritis
Fifth stage
Surgery
Lec-2
.د
علي
30/3/2017
Fractures of the tibia and fibula
Indirect force: (low energy)
Twisting: spiral fractures of both bones
Angulation: oblique fractures with butterfly segment.
Direct force:
Transverse (low energy) or comminuted (high energy) fractures usually with
skin and soft tissue damage.
In fractures of the tibia and fibula we must look for:
Size of wound (if present) and soft tissue damage.
Distal pulses, sensation and movements.
Signs of compartment syndrome.
X-ray must include the knee and ankle.
Management
Objectives:
To limit soft tissue damage and preserve skin cover.
To obtain and hold fracture alignment.
To recognize compartment syndrome.
To start early weight bearing to promote healing.
To start joint movement as soon as possible.
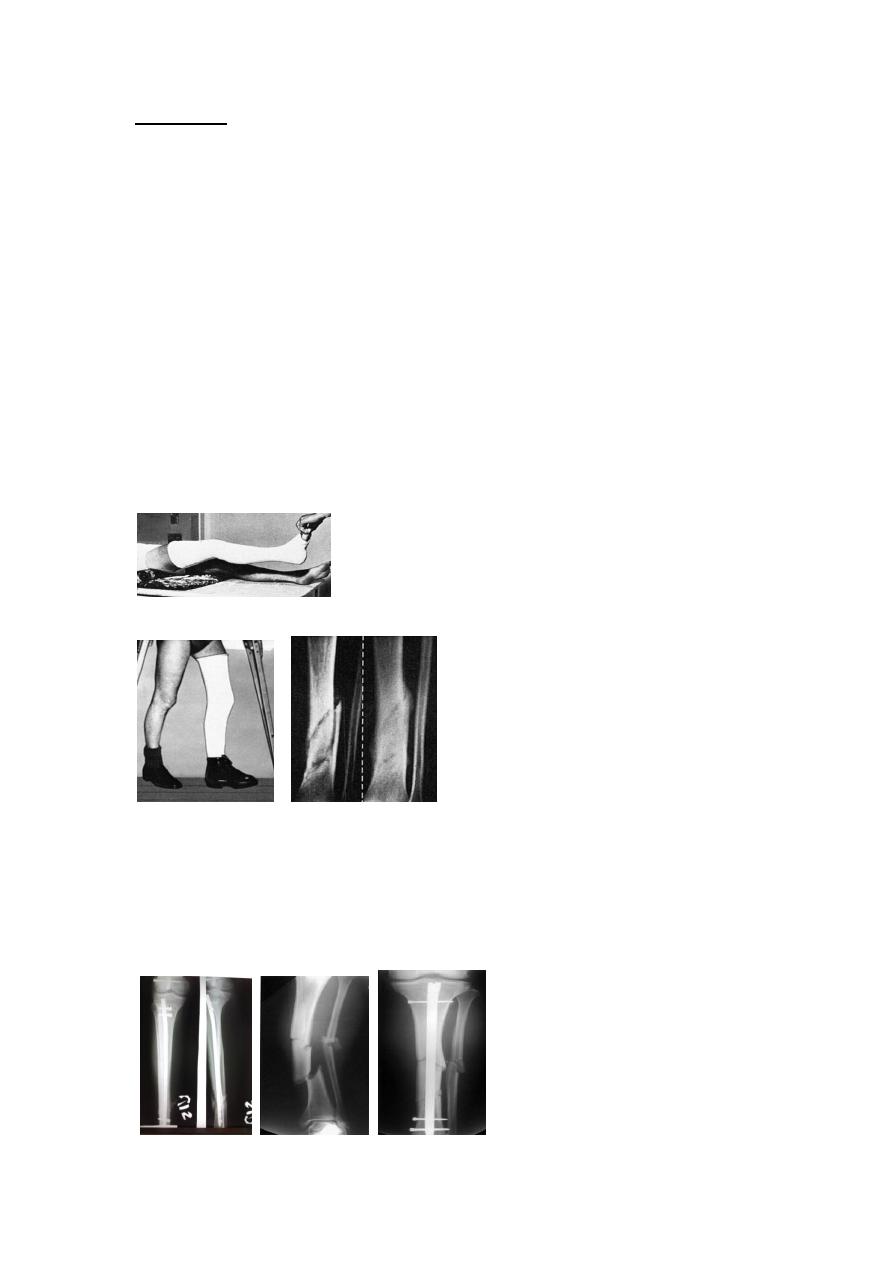
Treatment of low energy fractures
Closed undisplaced fractures treated by non-operative methods;
MUA for displaced fractures.
Then
Full-length cast from upper thigh to metatarsal necks with the knee in slight
flexion and the foot plantigrade (right angle), then slit cut done in the cast to
decrease the possibility for compartment. Or in sever swelling apply back slab
above knee.
Elevate the leg and observe for 2-3 days for compartment syndrome.
After 4-6 weeks change to below knee functional brace and allow weight
bearing and knee movement.
Healing may complete in 8 wks in children and in 16 wks in adults.
Skeletal fixation
Internal fixation is indicated in displaced and unstable fractures.
Locked intramedullary fixation is the method of choice for displaced
diaphyseal (shaft) fractures in adult.
Plate and screws for fractures near bone ends (metaphyseal) and for children with closed
unstable fractures.
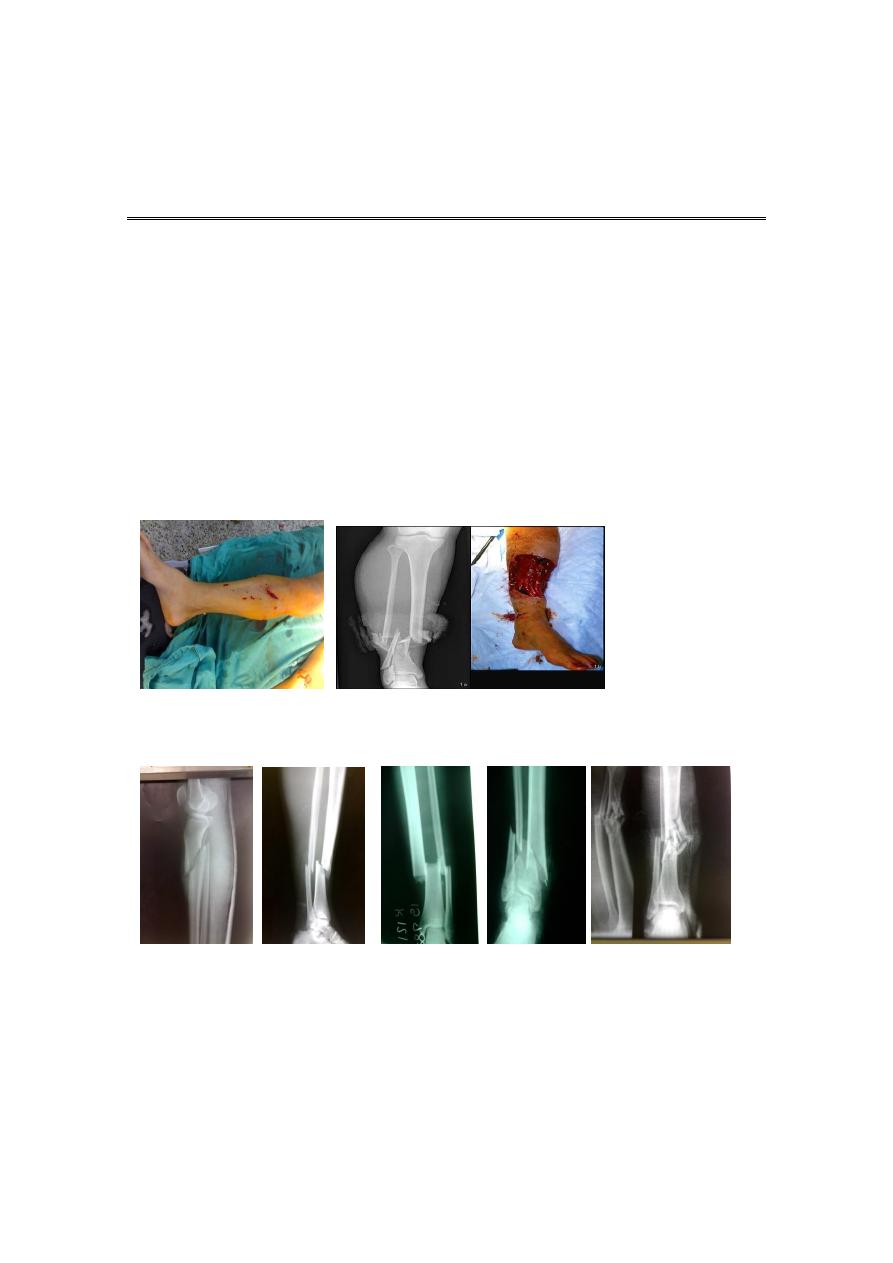
Open fractures: classification of the fracture according to Gustilo classification.
Antibiotics & anti-tetanus.
Debridement; thorough wash with normal saline, removal of dead tissues and debris.
Stabilization preferably using external fixation.
Soft tissue cover using flaps or grafts.
Rehabilitation.
Complications
1. Vascular injury.
2. Compartment syndrome.
3. Infection after open fractures and open surgery.
4. Malunion: shortening >1.5cm, angulation > 10 degrees or rotation should be corrected.
5. Delayed union and non-union; bone grafting and good fixation is required.
6. Joint stiffness.

Ankle ligament injuries
Types:
1. Stretching of the ligament.
2. Partial tear: healing restores full function.
3. Complete tear: joint instability.
Usually involves lateral ankle ligaments (ant. Talofibular lig., talocalcaneal lig., and post.
Talofibular lig.).
Medial calcaneal lig. (deltoid lig.) can result from abduction or eversion injury.
Clinical features:
Bruising, swelling, tenderness (usually distal and anterior to lat. Malleolus in anterior
talofebular lig. Injury).
Treatment
Partial tears:
elastic bandage and gentle active exercise.
Complete tears:
cast immobilization from below knee to toes for 6 wks then physiotherapy.
if this regime fails; operative repair is done.
Complications:
Recurrent sprains.
Recurrent giving way or instability.
FRACTURES AND FRACTURE- DISLOCATIONS OF THE ANKLE
Injury may involve one or more of the following structures:
1. Lateral maleolus.
2. Medial malleolus.
3. Tibiofibular syndesmosis.
4. Lateral ligament (ant. And posterior talofebular lig., and calcaneofibular
lig.).
5. Medial (deltoid) lig.
6. Tibial articular surface (tibial plafond).
7. Talus.
Clinical features
History of severe injury in young athletes or simple injury in elderly osteoporotic.
The patient complain from Intense pain, swelling, inability to stand.
In severe injury there is deformity around the ankle joint
Look for points of tenderness especially over medial or lateral malleolus.
Danis-Weber classification
(based on the level of fibular fracture)
Type A: a fibular fracture below syndesmosis and oblique fracture medial malleolus.
Type B: fibular fracture at syndesmosis + disruption of ant. fibers of tibiofibular lig. + fracture
of medial malleolus or rupture of deltoid lig.
Type C: fibular fracture above syndesmosis+ tibiofibular lig. (syndesmosis) is torn. Unstable
fracture-subluxation of ankle mortise+ fracture medial malleolus.

Principals of treatment
Treatment should start within hours; or after several days until swelling subside by elevation
and splintage.
Anatomical reduction is a must; to avoid later osteoarthritis.
Undisplaced fractures treated by cast splint for 4-6 weeks
Displaced fractures need open reduction and internal fixation.
Complications
1. Joint stiffness and prolonged swelling. Treat by compression stocking and elevation.
2. Complex regional pain syndrome.
3. Secondary Osteoarthritis
Comminuted fractures of the tibial plafond (Pilon fracture)
Severe axial compression of the ankle (FFH).
Shattering of ankle joint surface (articular surface of distal tibia).
Swelling and blistering;
Secondary Osteoarthritis is common.
Treatment
The priority is to control sever soft tissue swelling by elevation and cross ankle external
fixation for 2-3 weeks ( give time for soft tissue improvement and for actively manage the
fracture blisters).
Then open reduction and fixation.
Fractures of Talus
Rare and usually due to considerable violence- FFH, car accidents,…
May involve the body, neck, head or dislocation of the talus.
Clinical features
Pain, swelling, deformity.
X-ray: difficult to diagnose. May need to repeat several days later to see the fracture.
C-T in difficult cases.
Treatment
Undisplaced : Below knee plaster with knee plantigrade for 6-8 wks.
Displaced fractures or fracture dislocations: urgent reduction by closed manipulation; if fails,
ORIF

Complications
Non-union.
Avascular necrosis of body after fracture of neck.
Secondary osteoarthritis.
Calcaneal fractures
Usually seen after FFH.
Associated injuries: spine, pelvis, hip or base of skull.
Types:
1. Extra-articular fractures: need closed treatment. Have good prognosis.
2. Intra-articular fractures:
involve superior articular
surface.
May be comminuted.
Special features
The foot swollen, bruised and the heel look broad. Movement is painful.
Signs of compartment syndrome: intense pain and diminished sensation.
Necessary to X-ray the knees, spine, and pelvis.
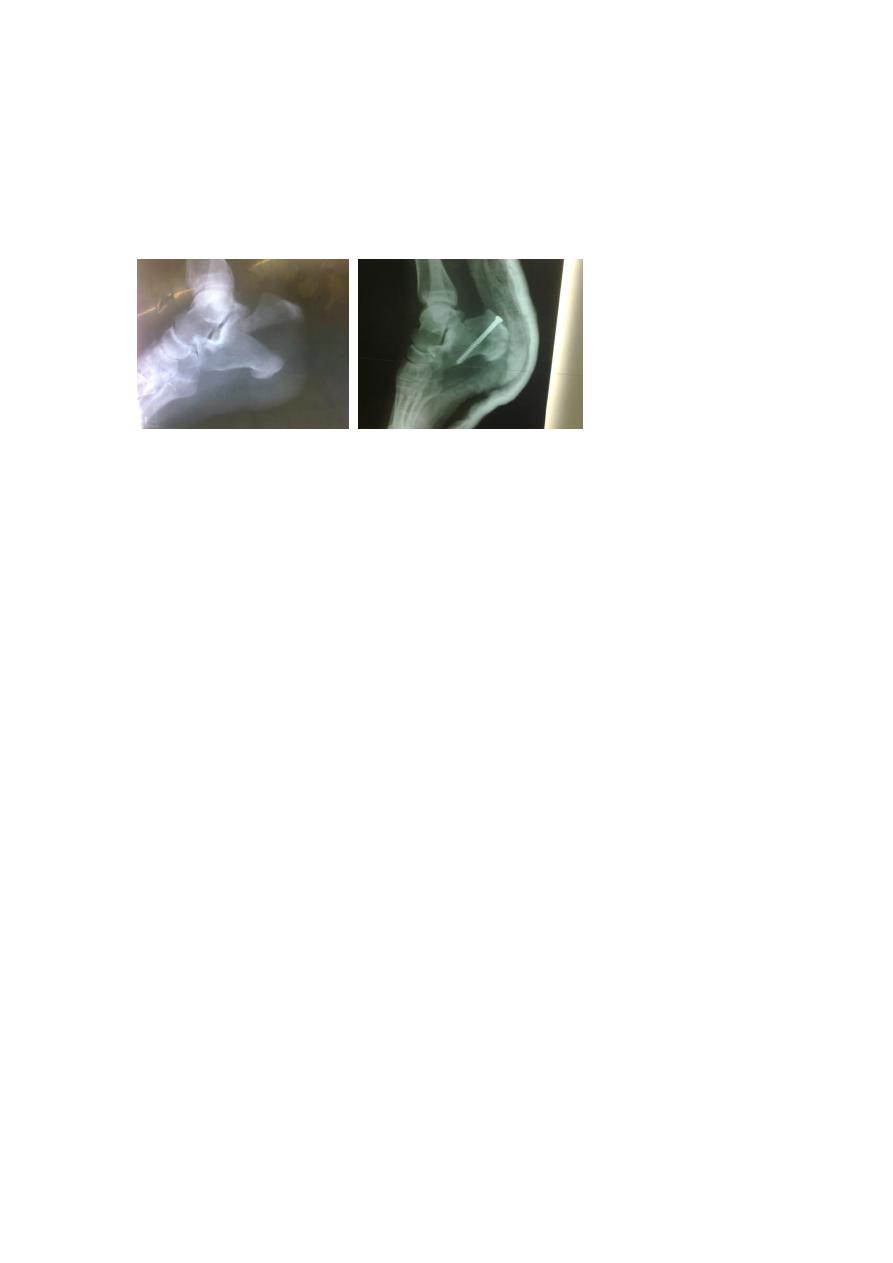
Treatment
Admit to hospital, elevate the leg and apply ice-packs until swelling subside.
Undisplaced fractures: closed treatment.
Displaced fractures: ORIF with screws or calcaneal plate and screws.
Complications
1. Broadening of the heel
2. Stiffness
3. OA
Metatarsal fractures
Mechanism of injury:
Direct trauma, Twisting, Repetitive stress.
Treatment:
Walking plaster for 3 wks.
Displaced fractures; Kirschner wire fixation.
Stress injury (march fracture)
Young adult (often recruit or a nurse)
Painful foot after overuse.
Tender lump in shaft of metatarsal (usually in the 2
nd week
).
X-ray: at first normal but later show hairline fracture and callus.
Radioisotope shows early increased activity.
Treatment: rest, bandage and NSAID.
Avulsion of base of fifth metatarsal
Result from forefoot inversion injury.
Base of 5
th
MT avulsed by peroneus brevis tendon.
Below knee walking cast for 3wks in undisplaced fractures.
In displaced type it may need ORIF
Treatment:
