Fetus and Placenta II
Development of PlacentaUniversity Of Babylon
College Of Medicine
Department Of Human Anatomy And Histology
Dr. Haythem Ali Alsayigh
Clinical Surgical Anatomy
MB.Ch.B.-F.I.M.B.S.
FETAL MEMBRANES AND PLACENTA
The placenta is the organ that facilitates nutrient and gas exchange between the maternal and fetal compartments.As the fetus begins the ninth week of development, its demands for nutritional and other factors increase, causing major changes in the placenta.
Foremost among these is an increase in surface area between maternal and fetal components to facilitate exchange.
The disposition of fetal membranes is also altered as production of amniotic fluid increases
CHANGES IN THE TROPHOBLAST
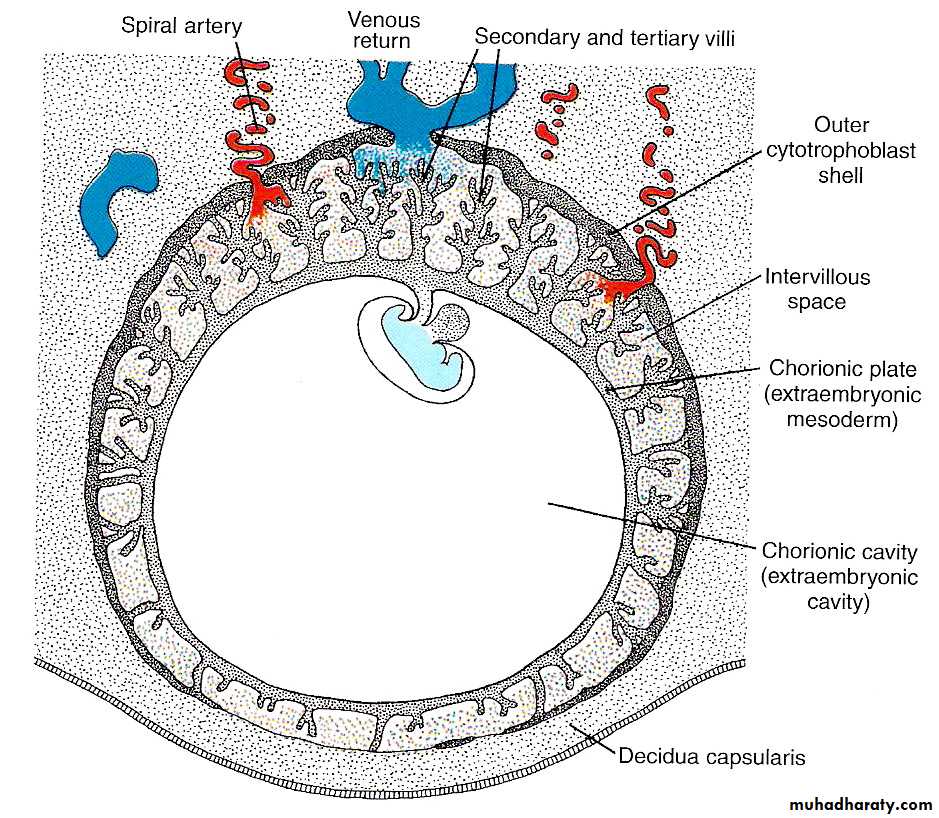
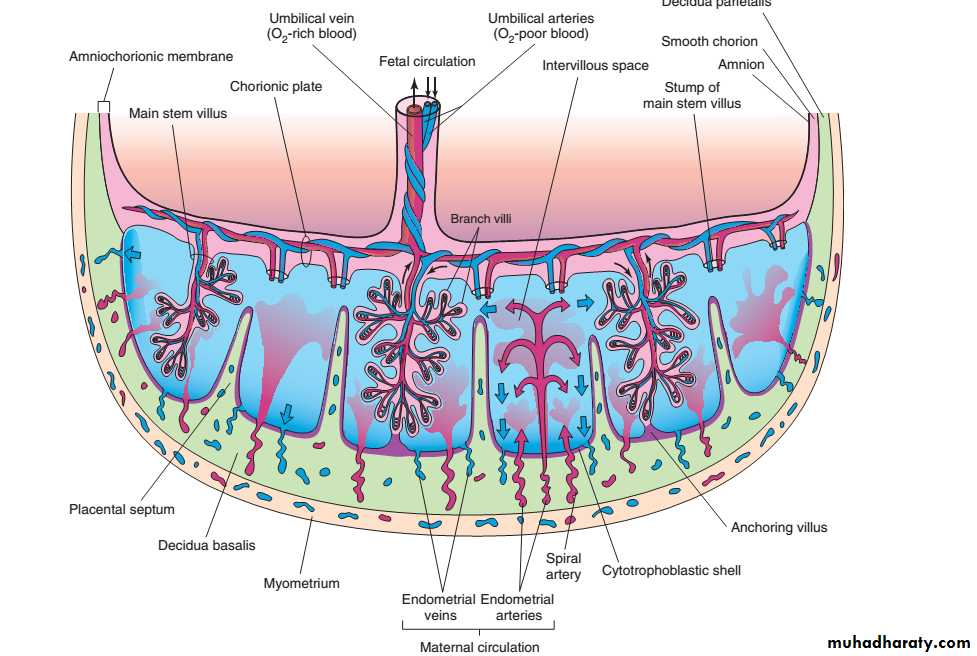
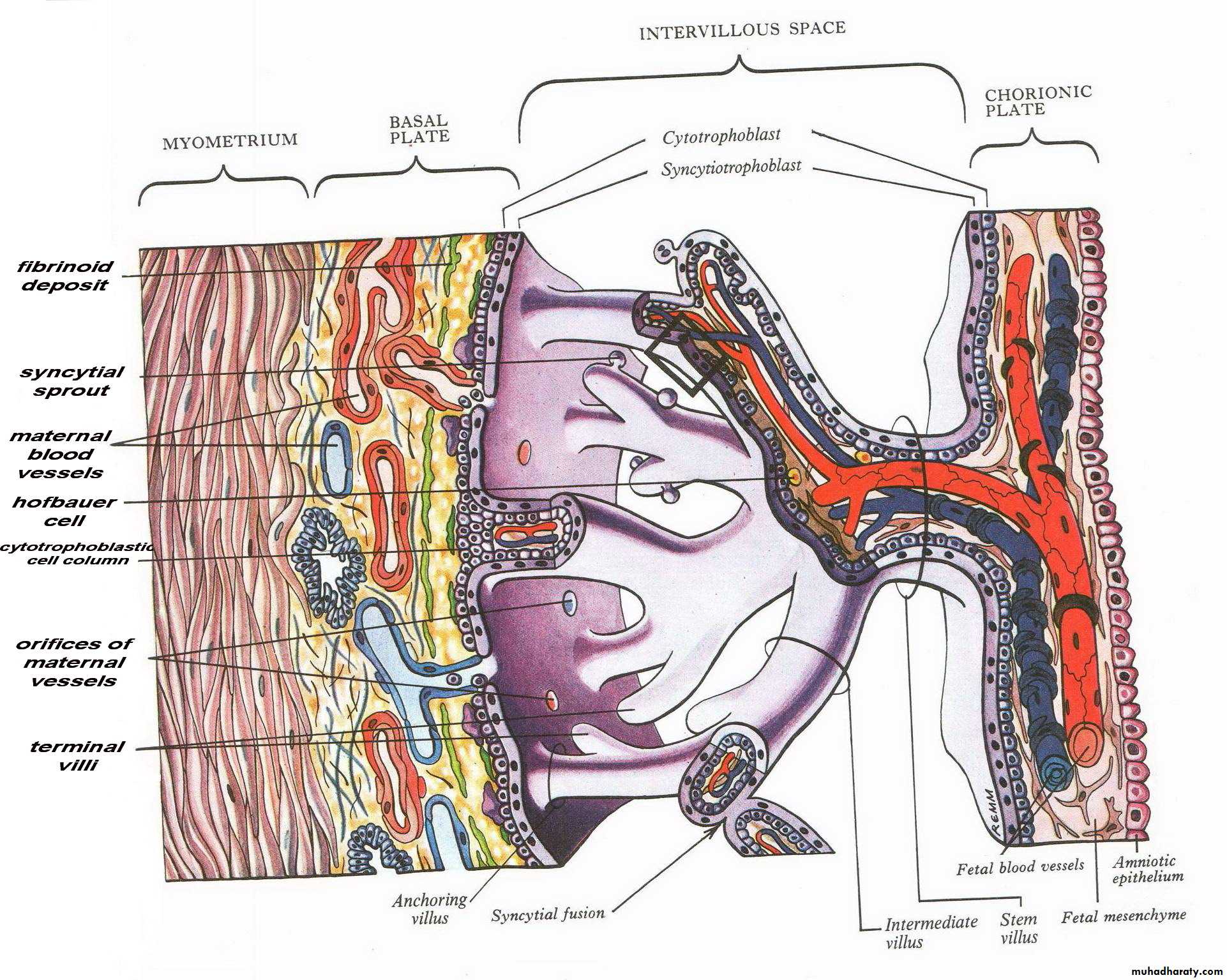
The fetal component of the placenta is derived from the trophoblast and extraembryonic mesoderm (the chorionic plate);the maternal component is derived from the uterine endometrium
By the beginning of the second month, the trophoblast is characterized by a great number of secondary and tertiary villi that give it a radial appearance
CHANGES IN THE TROPHOBLAST
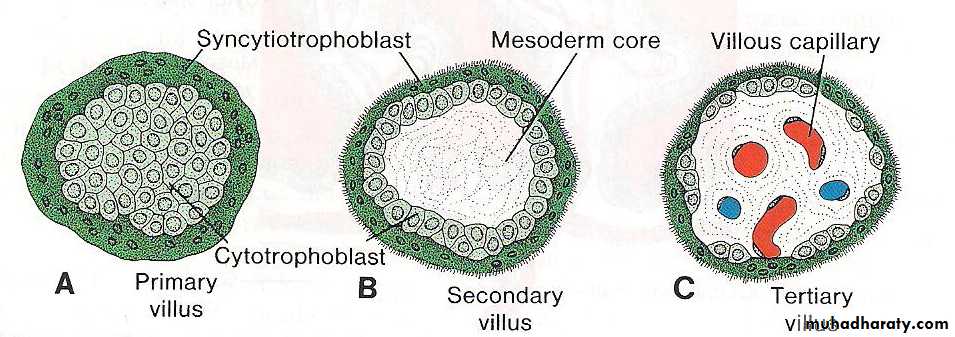
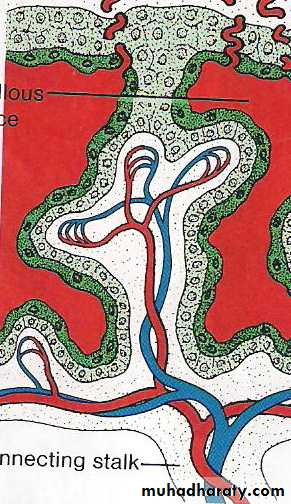
Stem (anchoring) villi extend from the mesoderm of the chorionic plate to the cytotrophoblast shell.The surface of the villi is formed by the syncytium, resting on a layer of cytotrophoblastic cells that in turn cover a core of vascular mesoderm
The capillary system developing in the core of the villous stems soon comes in contact with capillaries of the chorionic plate and connecting stalk, thus giving rise to the extraembryonic vascular system
Development of the placenta:
Definition :the development of the placenta: (villous structure) of the trophoblast as following:
• The primary villi (2nd W)
• The secondary villi (3rd W)
• The tertiary villi (3rd W)
Development of the placenta:
• The primary villi (2nd W)• The secondary villi (3rd W)
• The tertiary villi (3rd W)
EmbryoPlacental Circulation
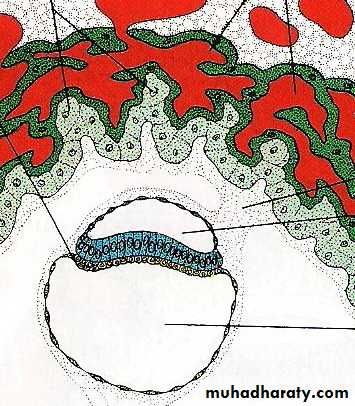
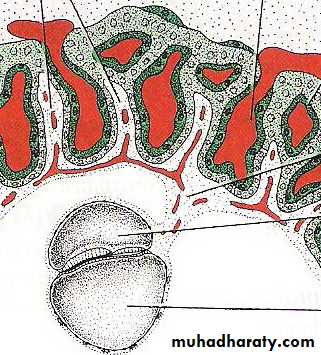
During the following months, numerous small extensions sprout(developed) from existing villous stems into the surrounding lacunar or intervillous spaces.
Initially these newly formed villi are primitive
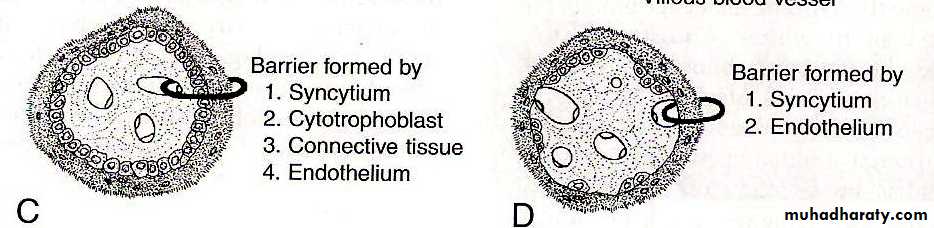
but by the beginning of the fourth month, cytotrophoblastic cells and some connective tissue cells disappear.
The syncytium and endothelial wall of the blood vessels are then the only layers that separate the maternal and fetal circulations Frequently the syncytium becomes very thin, and large pieces containing several nuclei may break off and drop into the intervillous blood lakes.
These pieces, known as syncytial knots, enter the maternal circulation and usually degenerate without causing any symptoms.
Disappearance of cytotrophoblastic cells progresses from the smaller to larger villi, and although some always persist in large villi, they do not participate in the exchange between the two circulations
CHORION FRONDOSUM AND DECIDUA BASALIS
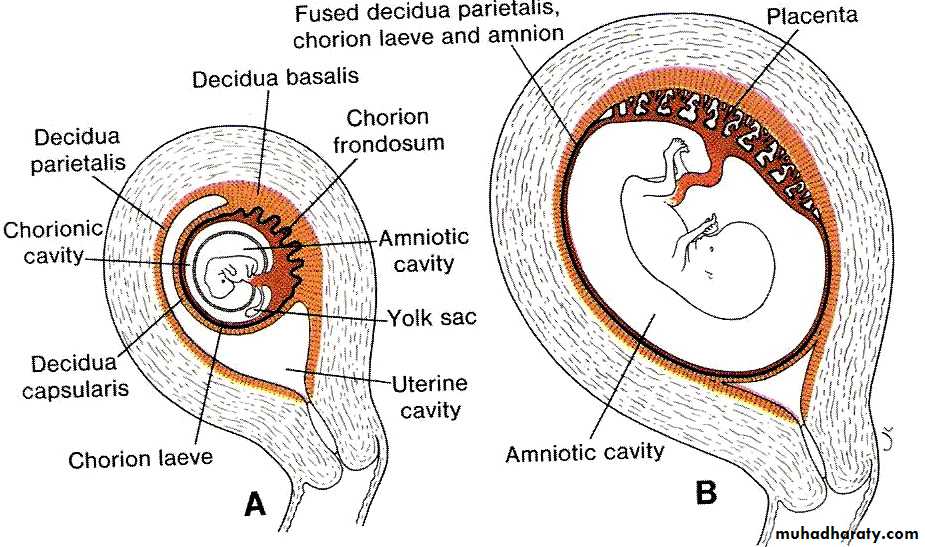
In the early weeks of development, villi cover the entire surface of the chorion.As pregnancy advances, villi on the embryonic pole continue to grow and expand, giving rise to the chorion frondosum (bushy chorion).
Villi on the abembryonic pole degenerate and b and by the third month, this side of the chorion, now known as the chorion laeve, is smooth
now known as the chorion laeve, is smooth The difference between the embryonic and abembryonic poles of the chorion is also reflected in the structure of the decidua,
the functional layer of the endometrium which is shed during parturition.
The decidua over the chorion frondosum, the decidua basalis consists of a compact layer of large cells, decidual cells, with abundant amounts of lipids and glycogen
CHORION FRONDOSUM AND DECIDUA BASALIS Development of the placenta:
• Formation of an outer cytotrophoblastic shell:• - End of 3rd w.
• - Stabilizes Implantation Firmly.
The endometrial mucosa functioning for implantation is called the Deciduas.
Stem villi or Anchoring villi
Free villi or Terminal villi, these villi grow into the lacunar spaces of the syncytium which are filled with maternal blood and are therefore called Intervillous spaces.
This layer, the decidual plate, is tightly connected to the chorion. The decidual layer over
the abembryonic pole is the decidua capsularis.
With growth of the chorionic vesicle, this layer becomes stretched and degenerates. Subsequently, the chorion laeve comes into contact with the uterine wall (decidua parietalis)
Development of the placenta:
2nd month
Development of the placenta:
5. At the 3rd monthChorion :
- Chorion Frondosum (the bushy chorion),
- Chorion Laeve.
Mucosal Decidua
- Deciduas Basalis (decidual plate) loaded with lipid and glycogen.
- Deciduas Capsularis.
- Deciduas Parietalis
Development of the placenta:
Enlargement of gestational sac obliteration of uterine cavity which result in fusion between Deciduas Capsularis with Deciduas Parietalis.After this fusion:
Deciduas Capsularis degenerate resulting in:
Fusion of the Chorion Laeve with the Deciduas Parietalis and Amnion
Fused D. per with chorionic leave and amnion
Development of the placenta:
6. Thining of the villous walls:- Beginning of 4th month
- Partial disappearance of cytotrophoblast cells and extraembryonic mesoderm of the tertiary villi (terminal villi )that are functioning in the fetomaternal exchange.
- (syncytial knots).
- Placental barrier only 2; endothelium of the villous vessels and the syncytium.
Structures of the placenta:
7. By the beginning of the 4th month, the placenta is formed by two components:- Chorion Frondosum (fetal part)
- Deciduas Basalis (maternal part).
Enlargment of amniotic cavity fill the extraembryonic chorionic cavity fusion of amniotic membrane with extraembryonic chorionic plate (amniochorionic membrane) that surround the developing fetus.
Structures of the placenta:
• The placental tissues are arranged as :• chorionic plate
• basal plate
• the intervillous space.
Structures of the placenta:
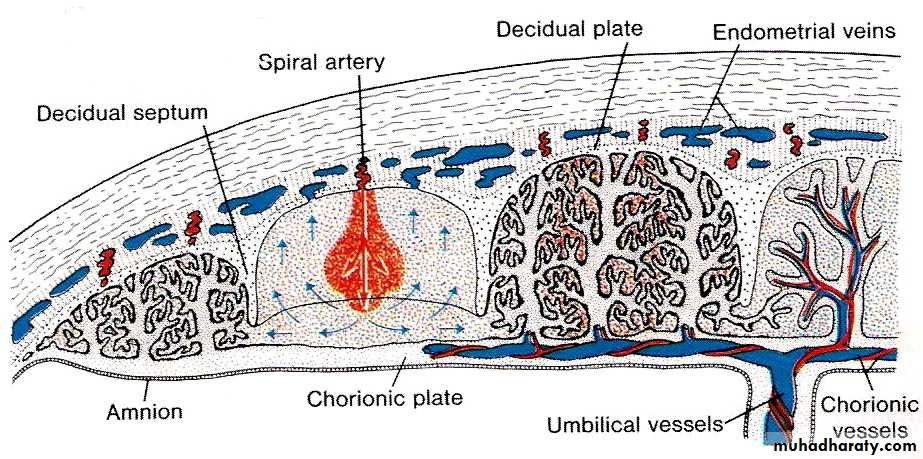
8. Formation of the Cotyledons:4th and 5th months:
many mucosal (or decidual) septae project into the intervillous spaces decidual septae
15 -20 lobes (cotyledons).
No complete septation.
septum = maternal deciduas covered by syncytium,
Structures of the placenta:
The cotyledons:are supplied by about 80 -100 maternal spiral arteries: accomplished by endovascular invasion by cytotrophoblast cells
The intervillous spaces are filled with about 150 ml of blood that replenished 3 times per minute.
As a result of continuous growth of fetus and enlargment of the uterus, placenta will enlarge (15%-30% of internal surface of uterus)
The increase thickness of placenta is due to increase arborization of the villi and not to more penetration of villi
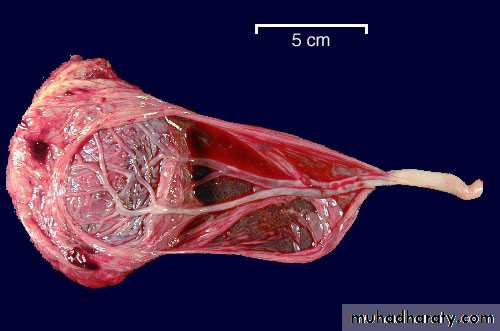
Features of full term placenta:
The placenta torn and expelled out 30 minutes after birth (NVD)Characteristic feature :
flattened discoid mass
circular or oval outline .
Average weight about 500-600 g
average diameter 15-25 cm .
Average thickness 3 cm.
Thickest at its center.
Diminishes in thickness towards its periphery.
Features of full term placenta:
Fetal side:shiny, grey and translucent
coverd by the amnionChorionic vessels that converge toward the umblical cord which is usually eccentric located.
Features of full term placenta:
Maternal side:maroon in color
See deciduas basalis.15-20 bulging cotyledons separated by the groove formed by the decidual septae.
Features of full term placenta:
attachment of the umbilical cord is usually eccentric or marginal.
Rarely the cord is attached to the chorionic plate not to the placenta and is called velamentous inserting cord.
Features of full term placenta:
At the end of pregnancy;the villi show an increase fibrous tissue
thickening of the capillary basement membrane.
Obliteration of some of the villous capillaries
deposition of fibrinoid on the villi and in the chorionic plate.
These changes may lead to the infarction of some of the cotyledons that appears white in color.
Function of the placenta:
1.exhang of gases:Oxygen, CO2 and CO …..by simple diffusion
At term the fetus extract 20-30 ml of O2/ min
The placental blood flow is critical to oxygen
2.exchange of nutrients and electrolytes:
Amino acids, free fatty acids,CHO and vitamines
Rapid and increases as pregnancy advances
Function of the placenta:
3.transmission of maternal IgG antibodies to the fetus; that begins to be transported to the fetus at approximately 14 weeks and thus providing passive immunity for the fetus against some infectious diseases (except chicken pox and whooping cough). This passive immunity support the new born for a short time after birth
Newborn begin to produce their own IgG, but adult levels not attained until the age of 3 yrs
Function of the placenta:
4.Hormone production;Syncytial trophoblast synthesized the following
Progesterone (end of 4th month)
Estrogen (estriol): stimulate growth of the uterus and the breast.
Placental Lactogen (somatomammotropin), the mother be diabetogenic and gives the fetus priority to maternal blood sugar. Also this hormone promotes the development of the breast.
During the 1st and 2nd months of pregnancy, (HCG)
Rh isoimmunization (Rh incompatibility):
THE ENDTHANK YOU