The rectum diseases
Dr. Mohammed Abdzaid AgoolFIBMS, MRCS, FACS
INJURIES:
The rectum or anal canal may be injured in a number of ways, all uncommon:• by falling in a sitting posture onto pointed object !
• by penetrating injury (including gunshots) to the buttocks;• by sexual assault or sexual activity involving anal penetration;
• by the fetal head during childbirth, especially forceps-assisted.
Diagnosis
The anus should be inspected and the abdomen palpated.If rigidity or tenderness is present, early laparotomy is imperative.
A water-soluble contrast enema or computerised tomography (CT) scan with rectal contrast is useful to identify perforation.
Prior to the operation, a urethral catheter is passed, but if there is any possibility of urethral injury (suggested by difficulty passing urine or haematuria), a urethrogram should be performed
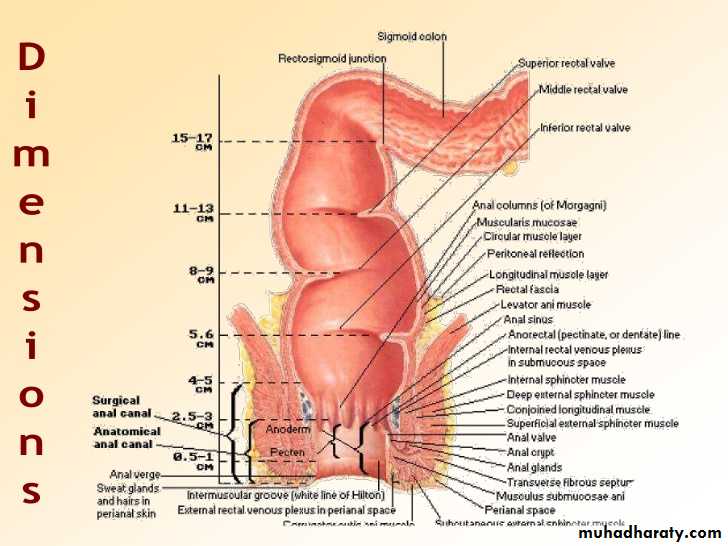
Rectum injury scale
Grade* Type of injury Description of injuryI Hematoma Contusion or hematoma without devascularization Laceration Partial-thickness laceration
II Laceration Laceration < 50% of circumference
III Laceration Laceration > 50% of circumference
IV Laceration Full-thickness laceration with extension into the perineum
V Vascular Devascularized segmentTreatment
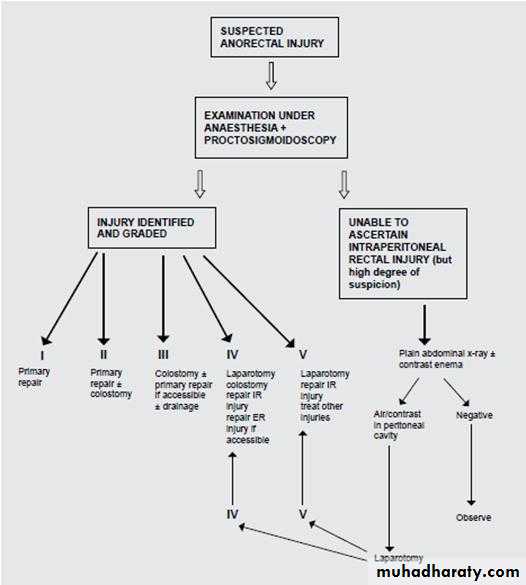
If perforation is suspected, the rectum is examined under general anaesthetic with a finger and a speculum, particular attention being directed to the anterior wall.If penetrating injury is confirmed, lower laparotomy is then performed. If an intraperitoneal rupture of the rectum is found, the perforation is closed with sutures. After closing the laparotomy wound, a defunctioning colostomy is usually required, constructed in the left iliac fossa.
If the rectal injury is below the peritoneal reflection, wide drainage from below is indicated, with rectal washout and a defunctioning colostomy.
If the defect in the rectum is very large, resection may have to be contemplated, usually in the form of a Hartmann’s procedure.
Care must be taken to preserve sphincter function during debridement of the perineal wounds. Antibiotic cover must be provided against both aerobic and anaerobic organisms
PROLAPSE:
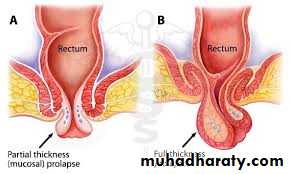
Rectal prolapse■ It may be mucosal or full thickness
■ If full thickness, the whole wall of the rectum is included
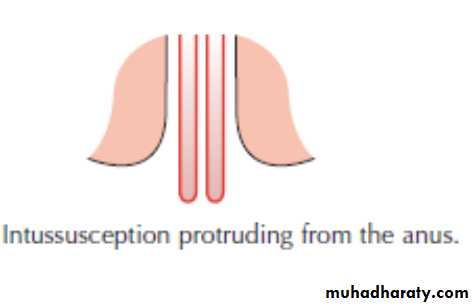
■ It commences as a rectal intussusception
■ In children, the prolapse is usually mucosal and should be treated conservatively
■ In the adult, the prolapse is often full thickness and is frequently associated with incontinence
■ Surgery is necessary for full-thickness rectal prolapse
■ The operation is performed either via the perineum or via the abdomen
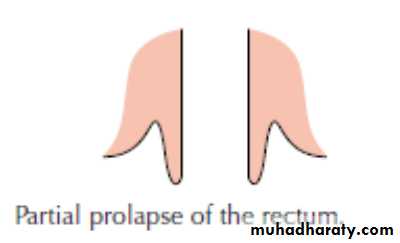
Mucosal prolapse
• The mucous membrane and submucosa of the rectum protrude outside the anus for approximately 1–4 cm. When the prolapsed mucosa is palpated between the finger and thumb, it is evident that it is composed of no more than a double layer of mucous membrane (cf. full-thickness prolapse).
In infants
The direct downward course of the rectum, due to the as yet undeveloped sacral curve , predisposes to this condition,as does the reduced resting anal tone, which offers diminished support to the mucosal lining of the anal canal.In children
Mucosal prolapse often commences after an attack of diarrhoea, or from loss of weight and consequent loss of fat in the ischiorectal fossae. It may also be associated with fibrocystic disease, neurological causes and maldevelopment of the pelvis.
In adults
The condition in adults is often associated with third-degree haemorrhoids. In the female a torn perineum, and in the male straining from urethral obstruction, predisposes to mucosal prolapse.In old age, both mucosal and full-thickness prolapse are associated with atony of the sphincter mechanism, but whether this is the cause of the problem or secondary to it is unknown.
Partial prolapse may follow an operation for fistula in ano where a large portion of muscle has been divided. Here, the prolapse is usually localised to the damaged quadrant and is seldom progressive.
Prolapsed mucous membrane is pink; prolapsed internal haemorrhoids are plum coloured and more pedunculated.
Treatment
In infants and young childrenA- Digital repositioning
B- Submucosal injections
If digital repositioning fails after 6 weeks’ trial, injections of 5% phenol in almond oil are carried out under general anaesthestic. As a result of the aseptic inflammation following these injections, the mucous membrane becomes tethered to the muscle coat.
C- Surgery
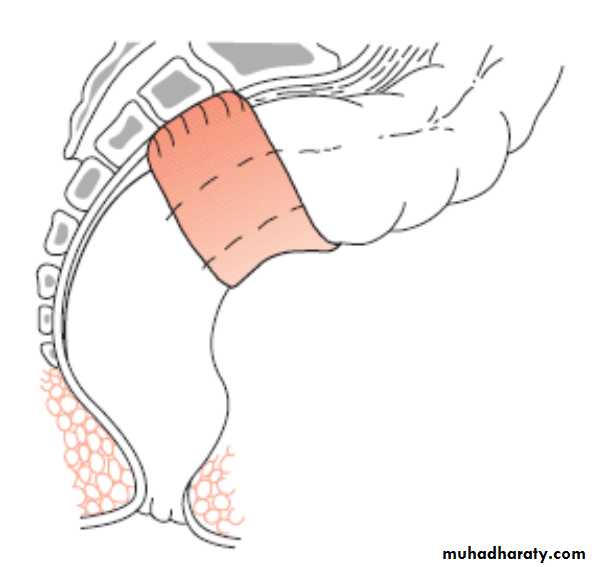
Occasionally, surgery is required and, in such cases, the child is placed in the prone jack-knife position, the retrorectal space is entered, and the rectum is sutured to the sacrum.
In adults
Local treatmentsSubmucosal injections of phenol in almond oil or the application of rubber bands are sometimes successful in cases of mucosal prolapse.
Excision of the prolapsed mucosa
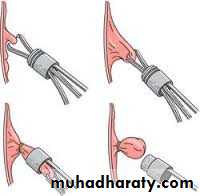
When the prolapse is unilateral, the redundant mucosa can be excised or, if circumferential, an endoluminal stapling technique can be used.
Full-thickness prolapse
Full-thickness prolapse (synonym: procidentia) is less common than the mucosal variety. The protrusion consists of all layers of the rectal wall and is usually associated with a weak pelvic floor.The prolapse is thought to commence as an intussusception of the rectum, which descends to protrude outside the anus. The process starts with the anterior wall of the rectum, where the supporting tissues are weakest, especially in women. It is more than 4 cm and commonly as much as 10–15 cm in length
On palpation between the finger and thumb, the prolapse feels much thicker than a mucosal prolapse, and obviously consists of a double thickness of the entire wall of the rectum. Any prolapse over 5 cm in length contains anteriorly between its layers a pouch of peritoneum.
The anal sphincter is characteristically patulous and gapes
widely on straining to allow the rectum to prolapse.
Complete prolapse is uncommon in children.
In adults, it can occur at any age, but it is more common in the elderly. Women are affected six times more often than men, and it is commonly associated with prolapse of the uterus.
Differential diagnosis
In the case of a child with abdominal pain, prolapse of the rectum must be distinguished from ileocaecal intussusception protruding from the anus.In rectosigmoid intussusception in the adult, there is a deep groove (5 cm or more) between the emerging protruding mass and the margin of the anus, into which the finger can be placed.
Treatment
Surgery is required, and the operation can be performed via the perineal or the abdominal approaches.An abdominal rectopexy has a lower rate of recurrence but, when the patient is elderly and very frail, a perineal operation is indicated.
As an abdominal procedure risks damage to the pelvic autonomic nerves, resulting in possible sexual dysfunction, a perineal approach is also usually preferred in young men.
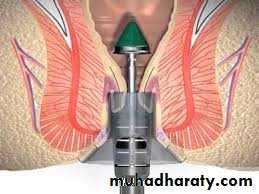
Perineal approach
Thiersch operation
Delorme’s operation
Altemeier’s procedure
Abdominal approach
The principle of all abdominal operations for rectal prolapse is to replace and hold the rectum in its proper position.They are recommended in patients with complete prolapse who are otherwise in good health. Many variations have been described:
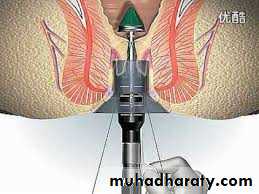
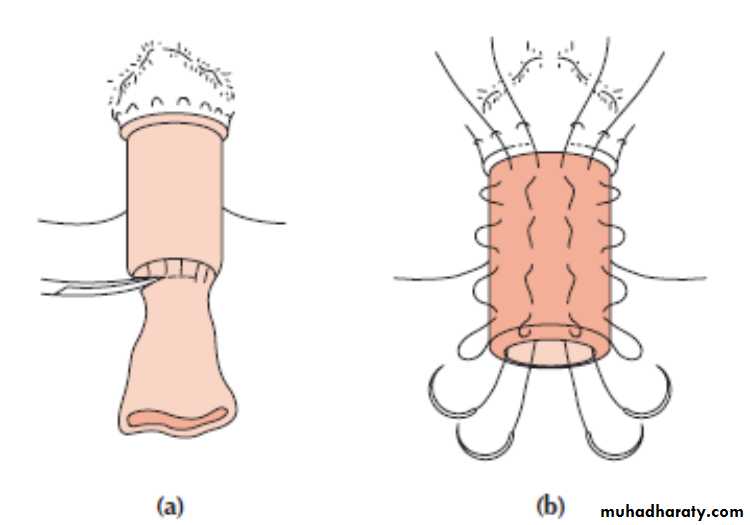
in Wells’ operation, the rectum is fixed firmly to the sacrum by inserting a sheet of polypropylene mesh between them.
Ripstein’s operation involves hitching up the rectosigmoid junction by a Teflon sling to the front of the sacrum.
sutured rectopexy many surgeons simply suture the mobilised rectum to the sacrum using four to six interrupted non-absorbable sutures .
Recently, the technique has been performed laparoscopically, thus reducing the operative trauma and limiting the time in hospital.
As an abdominal rectopexy may lead to severe constipation, some surgeons recommend combining this procedure with resection of the sigmoid colon (Goldberg), so called resection rectopexy.
Approximately 50% of adult patients with a complete rectal prolapse are incontinent, and rectopexy cures only about one third.
PROCTITIS
Inflammation is limited to the rectal mucosa; in other cases, it is associated with a similar condition in the colon (proctocolitis).The inflammation can be acute or chronic. The symptoms are tenesmus and the passage of blood and mucus and, in severe cases, of pus also.
Acute proctitis is usually accompanied by malaise and pyrexia. On rectal examination, the mucosa feels swollen and is often tender.
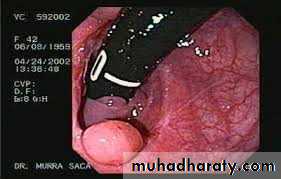
Proctoscopy is seldom sufficient, and sigmoidoscopy is the more valuable method of examination.
If the diagnosis is confirmed, colonoscopy with multiple biopsies is mandatory, to determine the extent of the inflammatory process.
Non-specific proctitis
is an inflammatory condition affecting the mucosa and, to a lesser extent, the submucosa, confined to the distal rectum. In 10% of cases, the condition extends to involve the whole colon (total ulcerative colitis).Aetiology
This is unknown. The concept that the condition is a mild and limited form of ulcerative colitis (although actual ulceration is often not present) is the most acceptable hypothesis.
The patient is usually middle-aged and complains of slight loss of blood in the motions. Often, the complaint is one of diarrhoea.
On rectal examination,
the mucosa feels warm and smooth. Often, there is some blood on the examining finger. Proctoscopic and sigmoidoscopic examination shows inflamed mucosa of the rectum, but usually no ulceration. The inflammation usually extends for only5–15 cm from the anus, with the mucosa above this level being normal.Treatment
The condition is usually self-limiting, but treatment with topical 5-aminosalicylic acid compounds (5-ASA) (Asacol, Penasa) in the form of suppositories or foam enemas is effective. Topical steroids are a less effective alternative. In very severe resistant cases, oral steroids may have to be used to obtain remission. Rarely, surgical treatment is required as a last resort when the patient is desperate for relief of symptoms.A- Ulcerative proctocolitis.
B- Proctitis due to Crohn’s disease.Specific proctitis:
Proctitis due to specific infections:
A- Clostridium difficile(pseudomembranous’ colitis)
B- Bacillary dysentery
C- Amoebic dysentery(Amoebic granuloma)
D- Tuberculous proctitis.
E- Gonococcal proctitis.
F- Lymphogranuloma venereum.
G- Acquired immunodeficiency syndrome.
H-‘Strawberry’ lesion of the rectosigmoid(Spirochaeta vincenti and Bacillus fusiformis.)
I- Rectal bilharziasis.
J- Proctitis due to herbal enemas.