DIRECT AND INDIRECT PULP CAPPING
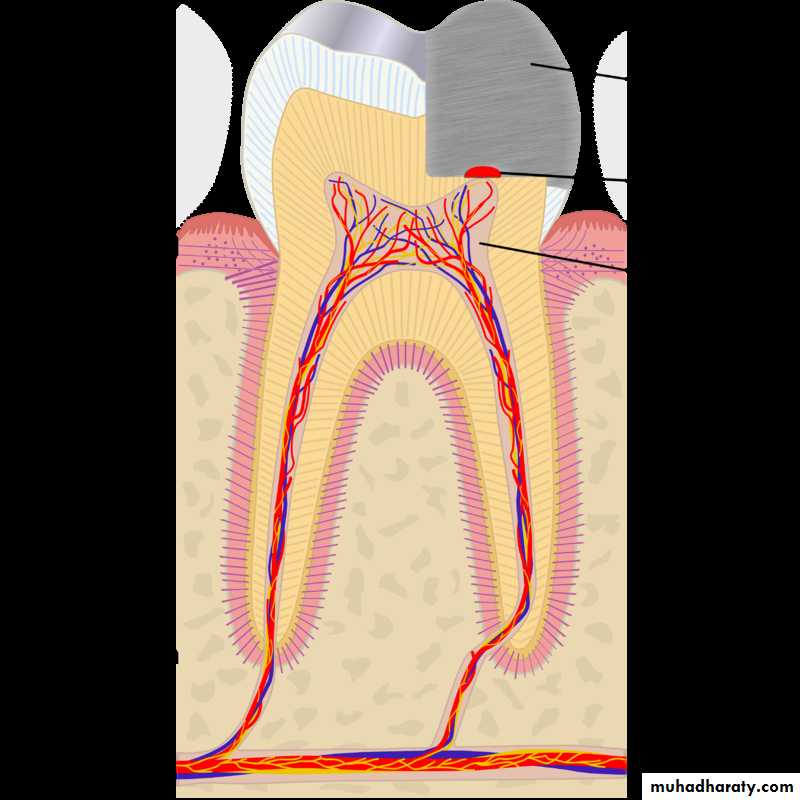
Pulp capping is a technique used in
dental restorations to prevent the dental pulp from necrosis , after being exposed, or nearly exposed during a cavity preparation.
To prevent the pulp from deteriorating when a dental restoration gets near the pulp, the dentist will place a small amount of a sedative dressing, such as calcium hydroxide or MTA (Mineral trioxide aggregate ).
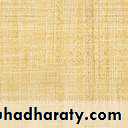
Direct pulp cap
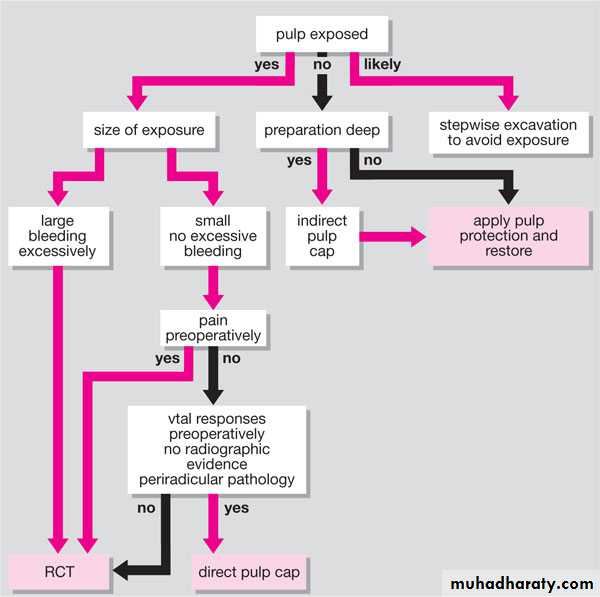
This technique is used when a pulpal exposure occurs, either due to caries extending to the pulp chamber, or accidentally, during caries removal.
Indirect pulp cap (stepwise caries removal)
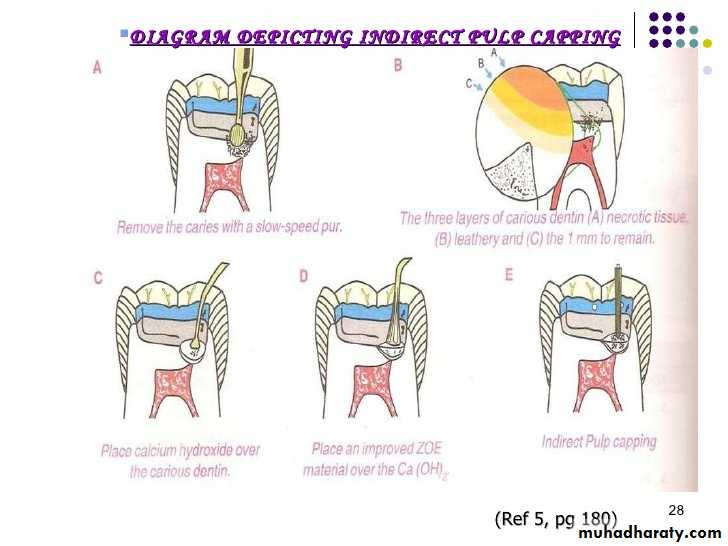
This technique is used when most of the decay has been removed from a deep cavity, but some softened dentin and decay remains over the pulp chamber that if removed would expose the pulp and form irreversible pulpitis.
INDIRECT PULP CAPPING
DIRECT PULP CAPPINGINDIRECT PULP CAPPING
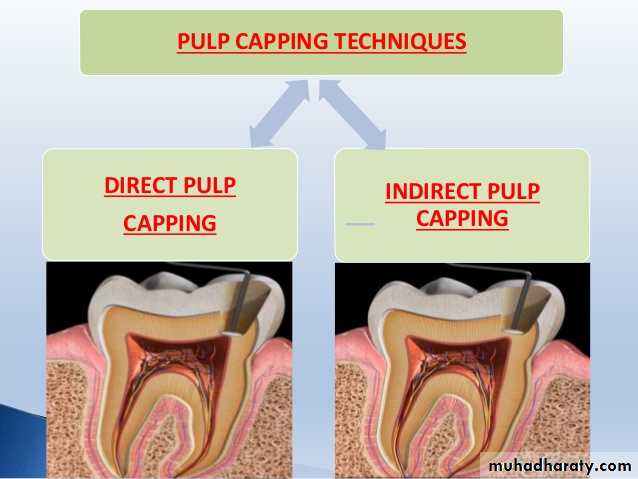
• Defined as a procedure wherein the deepest layer of the remaining affected carious dentin is covered with a layer of biocompatible material in order to prevent pulp exposure and further trauma to the pulp.• OBJECTIVE: a) Preserve the vitality of the pulp by completely removing the carious infected dentin followed by placement of a material that would enable the affected dentin to remineralize by stimulating the underlying ododntoblasts to form tertiary dentin.
• INDICATIONS: permanent teeth diagnosed with normal pulp with no signs or symptoms of pulpitis.
• CONTRAINDICATIONS: Large pulp exposure, non-restorable tooth or tooth with low prognosis.
• MATERIALS USED AS PULP CAPPING AGENT
PULP CAPPING AGENTADVANTAGES
DISADVANTAGES
1) Calcium hydroxide.
• Excellent antibacterial properties.
• Induction of mineralization.
• Low cytotoxicity.
• Highly soluble in oral fluids.
• Subject to dissolution over time.
• Presence of tunnels in reparative dentin.(tunnel defect.)
• Lack of adhesion.
2) Zinc oxide eugenol cement.
1)Reduces inflammation.
• Lack of calcific bridge formation.
• Releases eugenol in high concentration which is cytotoxic.
• Demonstrates interfacial leakage.
3) Corticosteroids and antibiotics.
• Reduces pulp inflammation.• Vanomycin and calcium hydroxide stimulated a more regular reparative dentin.
1) Should not be used in patients with risk from bacteremia.
4) Polycarboxylate cement.
1)Chemically bond to tooth structure.
• Lack of antibacterial effect.
• Fail to stimulate calcific bridge formation.
5) Inert materials( Isobutyl cyanoacrylate and tri calcium phosphate ceramic)
• Reduces pulp inflammation.
• Stimulate dentin bridge formation.
1) NONE of these materials have been promoted in dentist profession as a viable technique
6) Collagen
1) Less irritating than calcium hydroxide and promotes mineralization.
1) Does not help in thick dentin bridge formation.
• MATERIALS USED AS PULP CAPPING AGENT
PULP CAPPING AGENT
ADVANTAGES
DISADVANTAGES
• 7) Bonding Agents
• Superior adhesion to hard tissues.
• Effective seal against micro leakage.1) Has cytotoxic effect.
2) Absence of calcific bridge formation.8) Calcium phosphate.
• Helps in bridge formation with no superficial tissue necrosis.• Significant absence of pulp inflammation.
• Good physical properties.
1) Clinical trials are necessary to evaluate this material.
9) Hydroxyapatite.
• Biocompatible.
• Act as a scaffold for the newly formed mineralized tissue.
• Mild inflammation with superficial necrosis of pulp.
10) Carbon dioxide lasers
• Formation of secondary dentin.
• Bactericidal effects.
• Technique sensitive.
• Causes thermal damage to pulp at high doses.
11) Glass ionomer/ Resin modified glass ionomer.
• Excellent bacterial seal.
• Fluoride release, coeffient of thermal expansion and modulus of elasticity similar to dentin.
• Good biocompatibility.
• Cause chronic inflammation.
• Lack of dentin bridge formation.
• Cytotoxic when in direct cell contact.
• High solubility and slow setting rate.
PULP CAPPING AGENT
ADVANTAGES
DISADVANTAGES.
12) Mineral trioxide aggregate.
• Good biocompatibility.• Less pulpal inflammation.
• More predictable hard tissue barrier formation in comparison to calcium hydroxide.
• Radiopacity.
• More expensive.
• Poor handling characteristics.
• Two step procedure .
• High solubility.
13) MTA 1-Calcium
• Helps in dentin bridge formation without formation of necrotic layer.• Shear bond strength is higher than conventional GIC and similar to RMGIC.
1) Presence of 10% calcium hydroxide interferes with complete curing of the material, residual monomers causes cytotoxicity.
14) Growth factors.
• Formation of osteodentin and tubular dentin.
• Formation of more homogenous reparative dentin
• Superior to calcium hydroxide in the mineralization inducing properties.
• High concentration is required.
• Half life is less.
• Appropriate dose response is required to avoid uncontrolled obliteration of pulp chamber.
15) Odontogenic ameloblast associated protein.
• Biocompatible.
• Accelerates reactionary dentin formation.
• Normal pulp tissue appearance without excessive tertiary dentin formation and obliteration of the pulp cavity compared to MTA
• Till now only invitro studies were conducted.
• Further studies regarding this material is required.
• MATERIALS USED AS PULP CAPPING AGENT
PULP CAPPING AGENT
ADVANTAGES.
DISADVANTAGES.
16) Endo sequence root repair material
• Antibacterial property.• Less cytotoxic than MTA, Dycal and light cure calcium hydroxide.
• Bioactivity of the cells were decreased gradually when exposed to this material.
17) Castor oil bean cement.
• Good antibacterial property.• Less cytotoxic.
• Good mechanical properties.
• Facilitates tissue healing.
• Better sealing ability than MTA and GIC.
• Less cost.
• Bio inert rather than bioactive.
• More clinical trials are required.
18) Thera Cal.
• Act as protectant of the dental pulp complex.
• Has strong physical properties, no solubility, high radiopacity.
• TheraCal exhibited higher calcium releasing ability than MTA or Dycal.
1) It is opaque and whitish in color and it should be kept thin so as not to show through composite material that are very translucent affecting final restoration shading.
DIRECT AND INDIRECT PULP CAPPING
DEEP
CARIOUSLESION
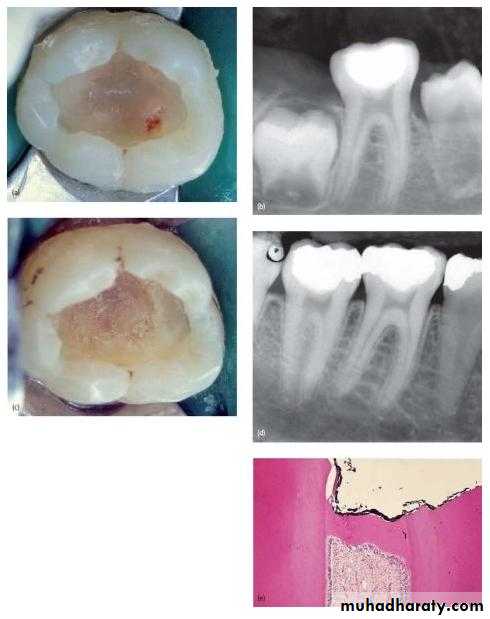
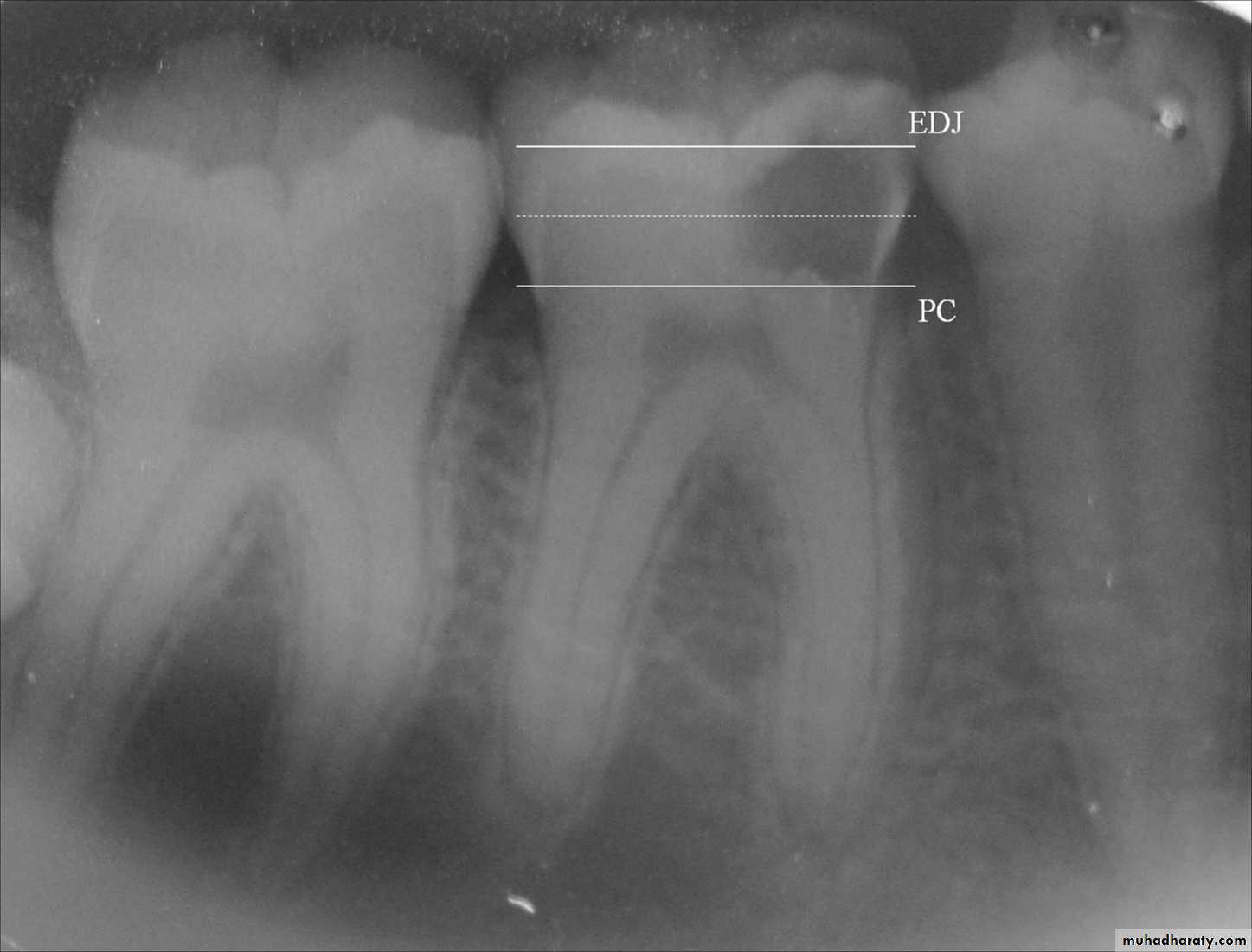
• Deep carious lesion in mandibular molars without pulp involvement.
RATIONALE
• Disinfection of residual affected dentin is more readily accomplished.• It eliminates the need for more difficult pulp therapy by arresting the carious process and allowing the pulp reparative process to occur.
• Patient comfort is immediate.
• Rampant dental caries is stopped when all the carious teeth are treated.
• CLINICAL PROCEDURE
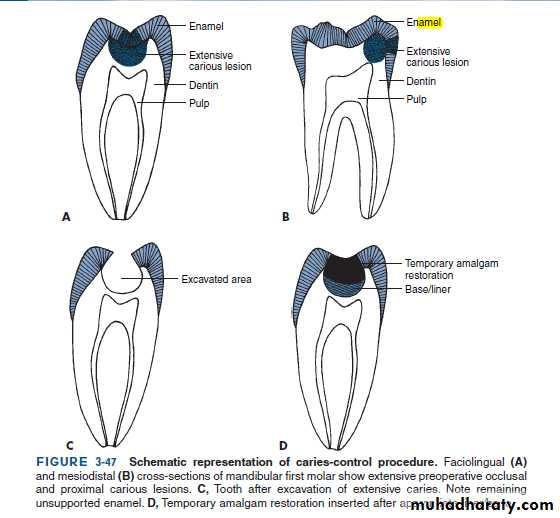
• It could be performed as a single or two step approach.
• Objective of this technique is to arrest carious lesion progression and allow formation of reparative dentin.
• The two-step stepwise excavation approach is recommended for the following reasons;
• It avoids unintentional pulp exposure which may deteriorate the pulp prognosis.
• The dentist gets a chance to assess the reaction of the tooth as well as gain information of the changes in caries activity.
• It gives an opportunity to remove the slow progressing lesion in slightly infected, discoloured, demineralized dentin before the placement of final restoration.
• The final excavation of caries is safer in the second sitting as it is easier to remove the dry carious dentin.
PROCEDURE
• FIRST APPOINTMENT
• Use of local Anesthesia and isolate with rubber dam.• A slow speed hand piece with round burs is used to remove the superficial debris and majority of soft infected dentin without exposing the pulp.
• Deepest layer of infected dentin is covered with a hard setting calcium hydroxide preparation and sealed with an overlying base of reinforced zinc-oxide eugenol preparation.
• This sealed cavity is not disturbed for 6-8 weeks.
• SECOND APPOINTMENT.
• A bitewing radiograph of the treated tooth is obtained.
• Use local Anesthesia and isolate with rubber dam.
• The previous remaining soft, deep, brownish red affected dentin will have changed to lighter brownish gray colour and most importantly harder in nature.
• The entire floor is covered with calcium hydroxide preparation.
• When clinical and radiographic findings are negative the final restoration is placed.
• RESULTS-BEFORE
• AND AFTER• FACTORS DETERMINING SUCCESS OF IPC.
• Remaining dentin thickness(0.5-2mm)• Choice of indirect pulp capping agent.
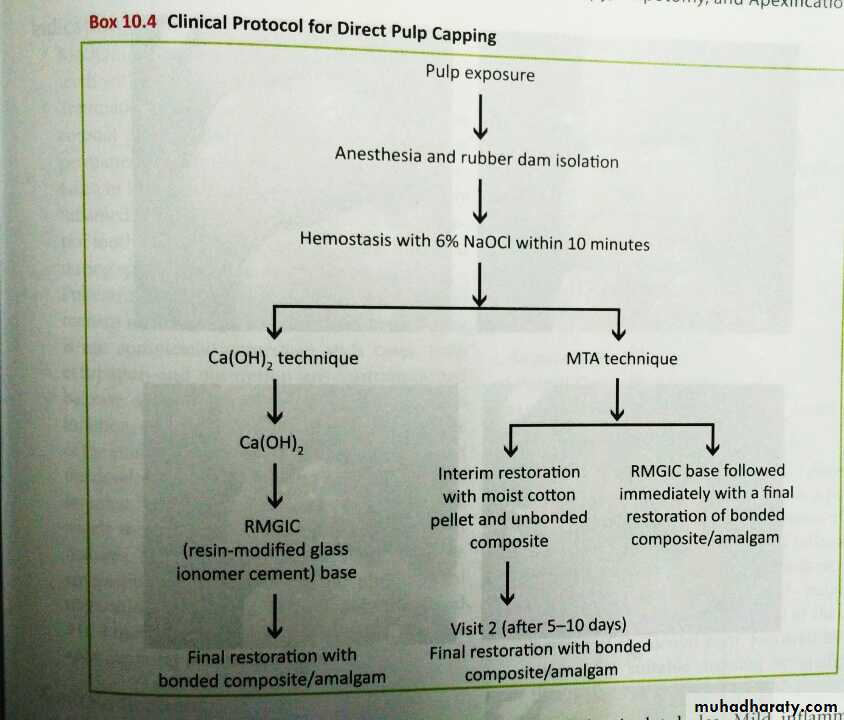
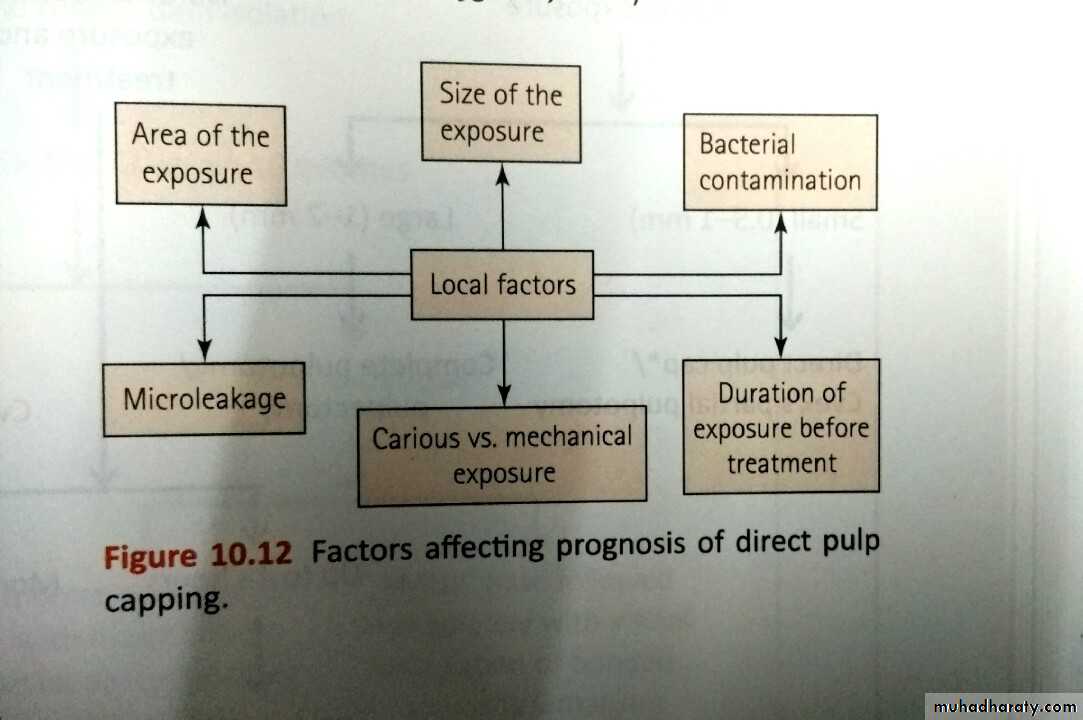
• DIRECT PULP CAPPING.
• Defined as a procedure in which the exposed vital pulp is covered with a protective dressing or base placed directly over the site of exposure in an attempt to preserve the pulp vitality.• OBJECTIVES: a) preservation of vitality of the radicular pulp.
• b) relief of pain in patients with acute pulpagia.
• c) ensuring the continuity of normal apexogenesis in immature permanent teeth.
• INDICATIONS: a) asymptomatic conditions.
• b) small exposure less than 0.5mm in diameter
• c)haemorrhage from the exposure site is easily controlled.(within 10min)
• d)the exposure occurred is clean and uncontaminated(rubber dam isolation)
• e)atraumatic exposure and little desiccation of the tooth with no evidence of
• aspiration of blood into the dentin.
• CONTRAINDICATION: Large carious exposure in symptomatic permanent tooth.
• CARIOUS LESIONS
• INVOLVING THE PULP
• DEEP CARIOUS LESION WITH PULPAL INVOLVEMENT
P
R
O
C
E
D
U
R
E