Pigmented lesions of oral cavity
طب فم \ خامس اسناند. وائل م(8)
26\ 4\ 2017
Pigmented lesions are commonly found in the mouth. Such lesions represent a variety of clinical entities, ranging from physiologic changes to manifestations of systemic illnesses and malignant neoplasm
Oral pigmentation may be exogenous or endogenous in origin.
Exogenous pigmentation is commonly due to foreign-body implantation in the oral mucosa.Endogenous pigments include melanin, hemoglobin, hemosiderin and carotene.
The color of oral pigmentation can vary depending on the quantity and depth or location of the pigment. Generally, the surface shows brown pigmentation and those located deeper are black or blue.Pigmented lesions caused by increased melanin deposition may be brown, blue, grey or black, depending on the amount and location of melanin in the tissues
Differential diagnosis of pigmented lesions of oral cavity
The history should include the onset and duration of the lesion
The presence of associated skin hyperpigmentation
The presence of systemic signs and symptoms
Use of prescription and nonprescription medications,
Smoking habits
The number, distribution, size, shape and colour of intraoral pigmented lesions should be assessed.
Clinical tests -diascopy and radiography and laboratory investigations
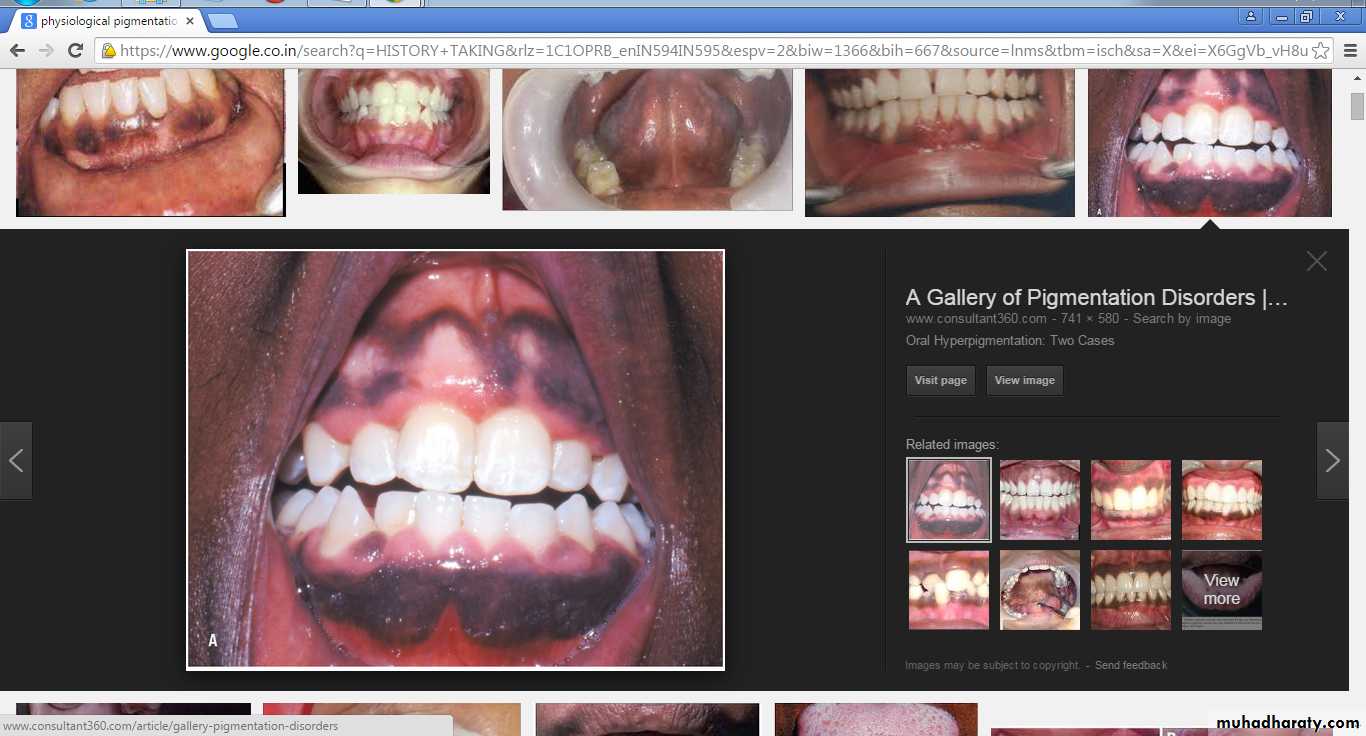
Diffuse And Bilateral Pigmentation
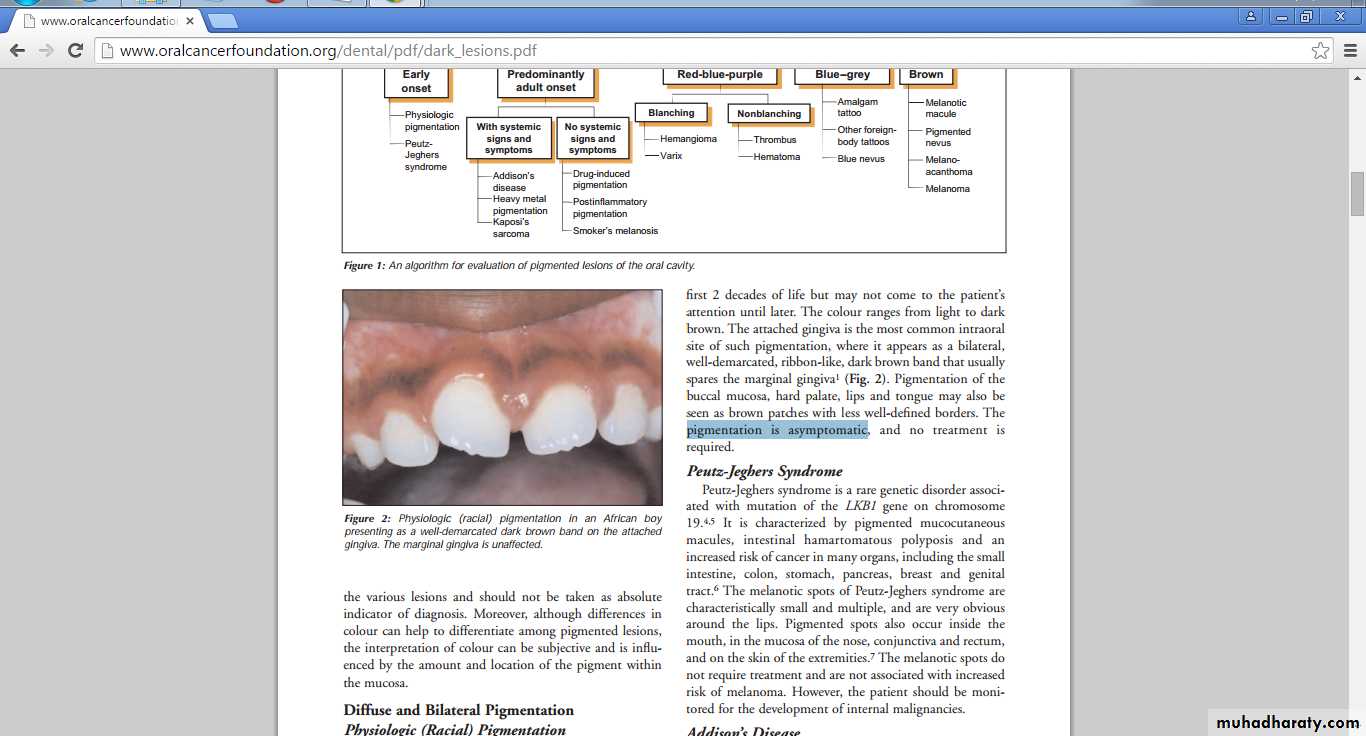
Physiologic (Racial) Pigmentation
Greater melanocytic activity
The colour ranges from light to dark brown.
The attached gingiva is the most common intraoral site of such pigmentation
Pigmentation of the buccal mucosa, hard palate, lips and tongue may
pigmentation is asymptomatic
Physiologic (Racial) Pigmentation
Phy-siological pigmentation increases with age, and color intensity can be influenced by smoking, hormones and systemic medications
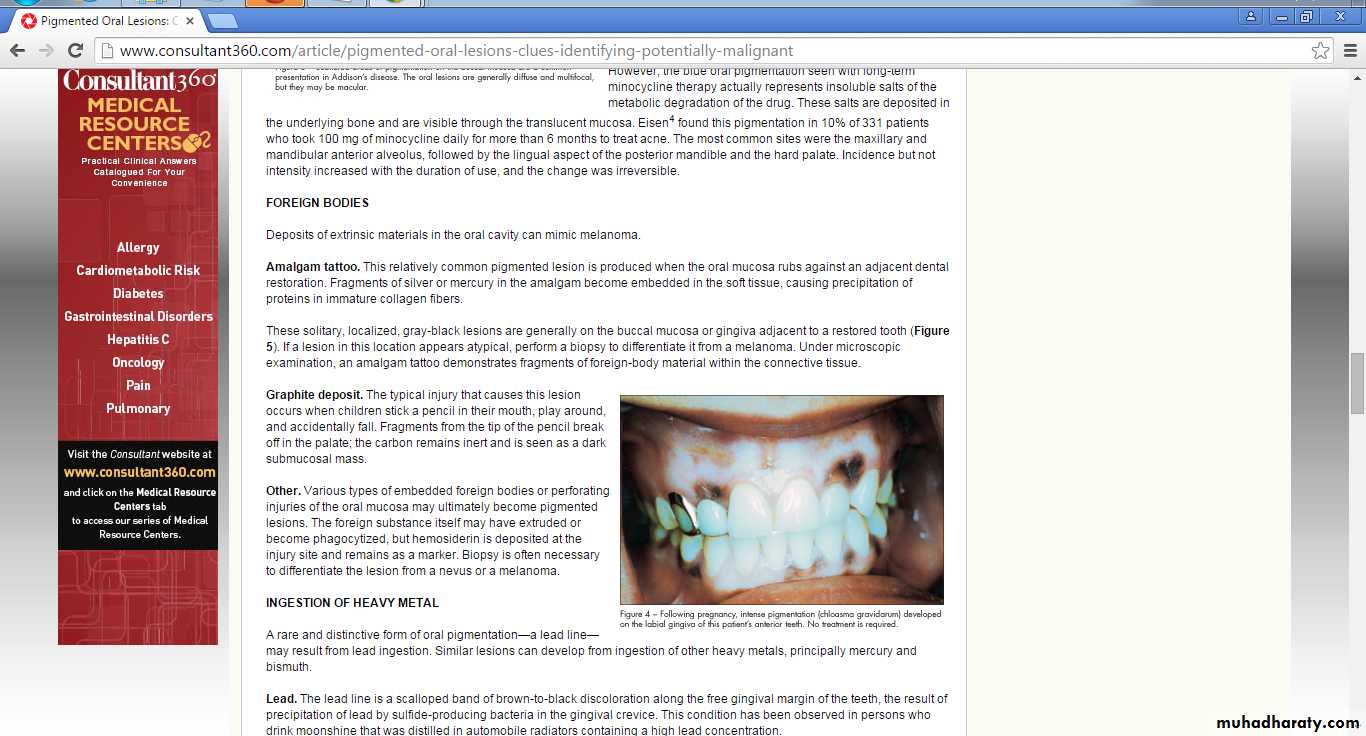
Chloasma
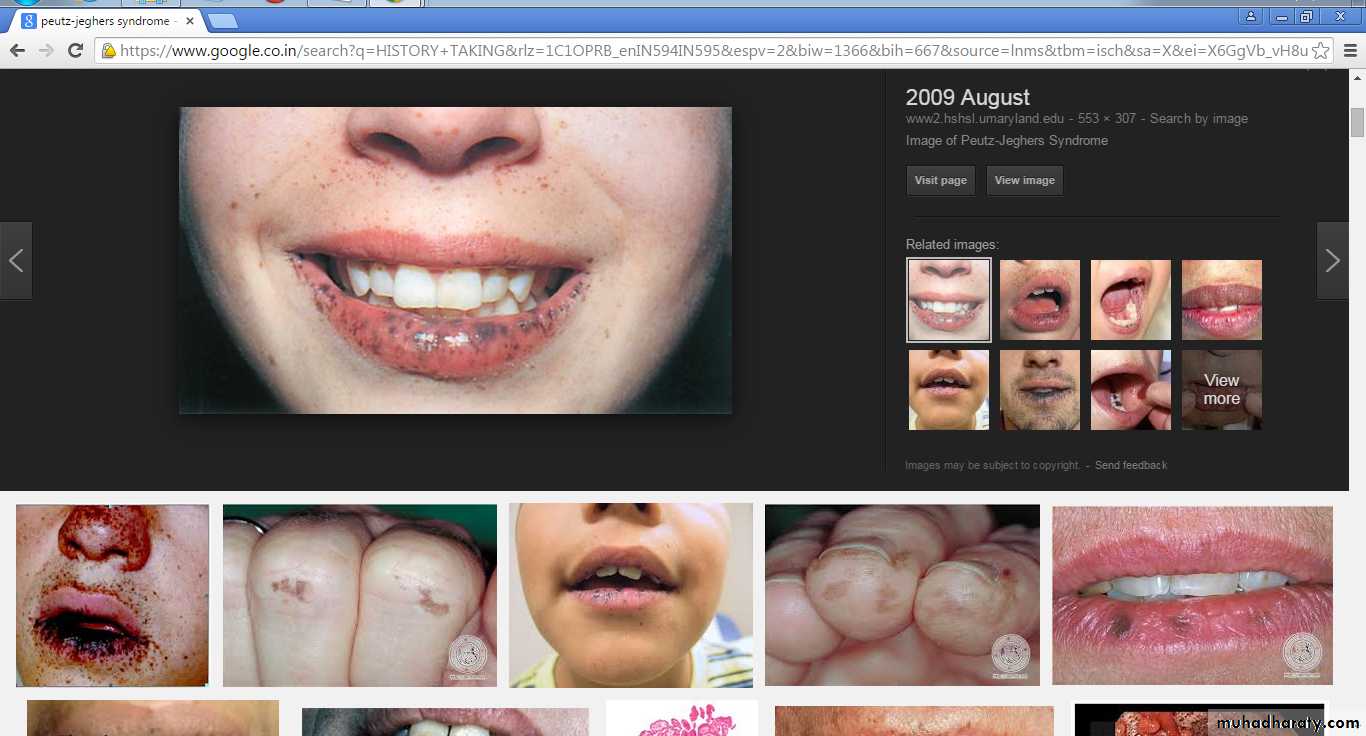
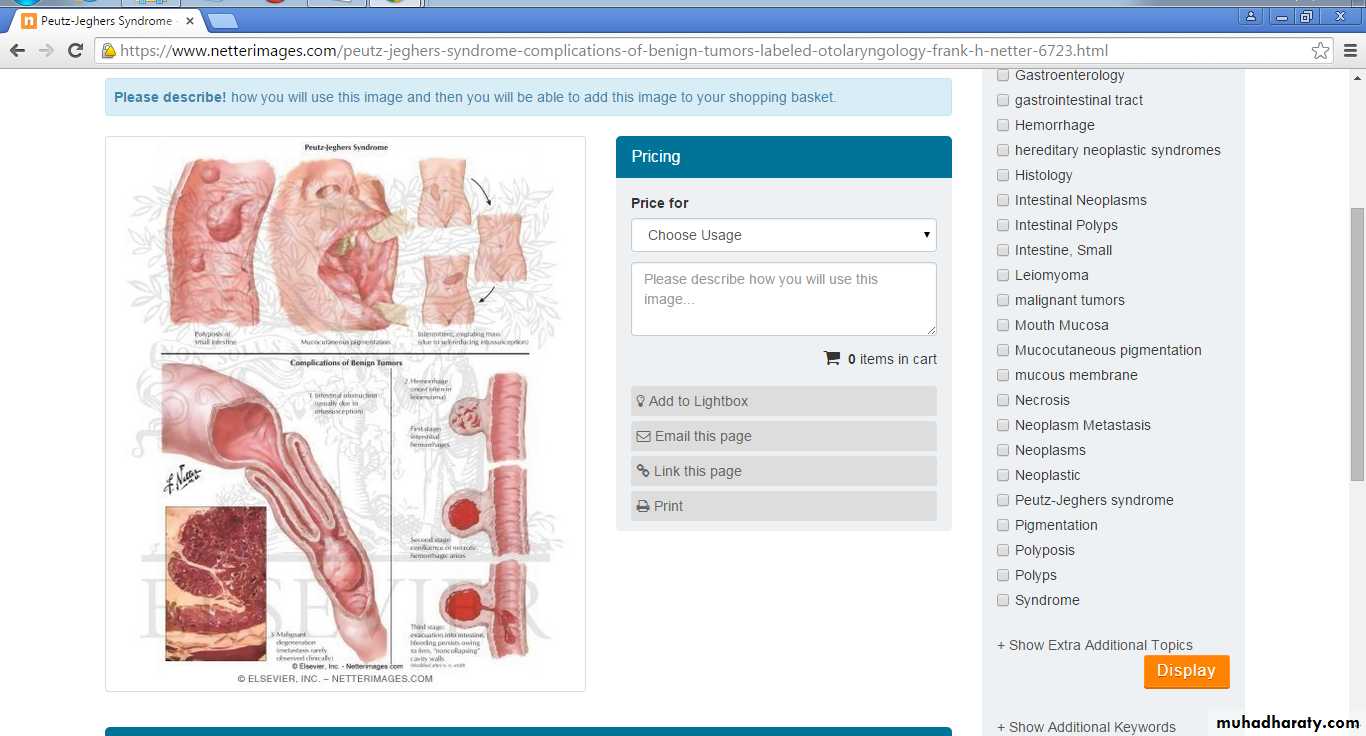
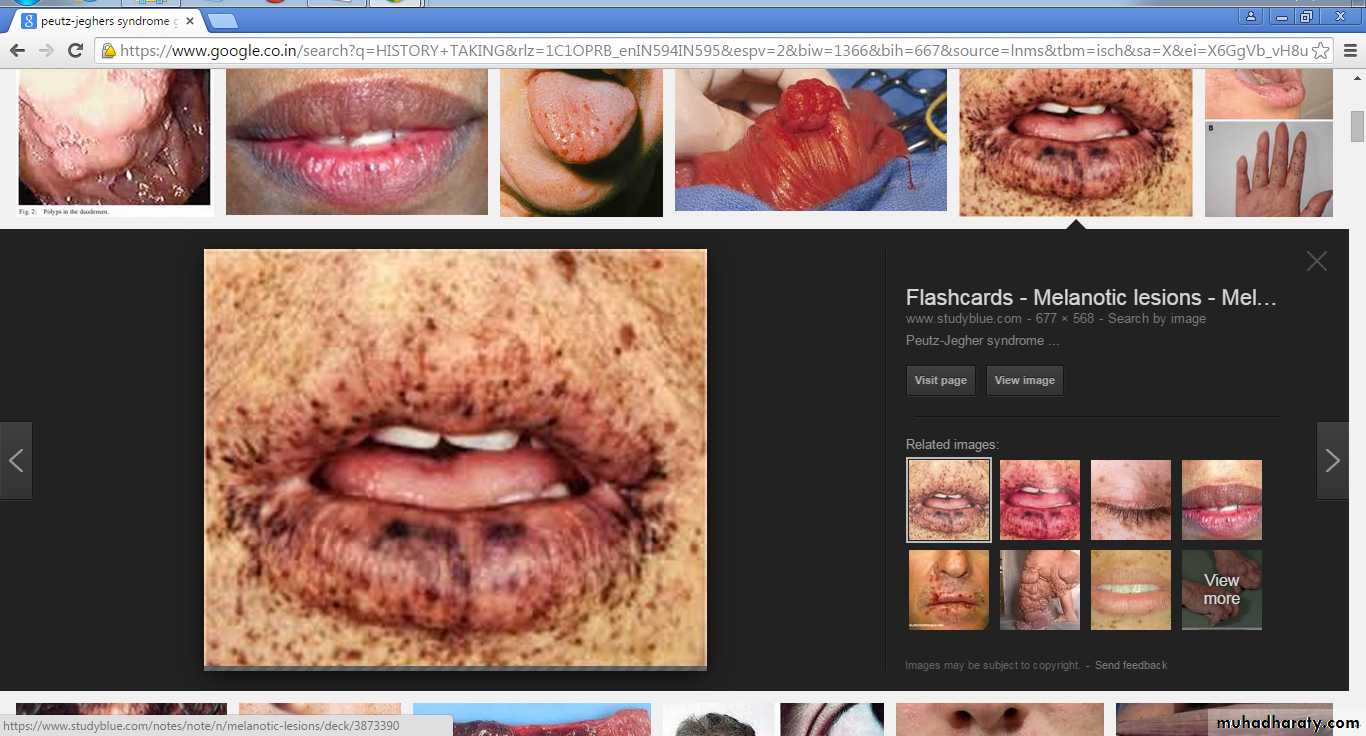
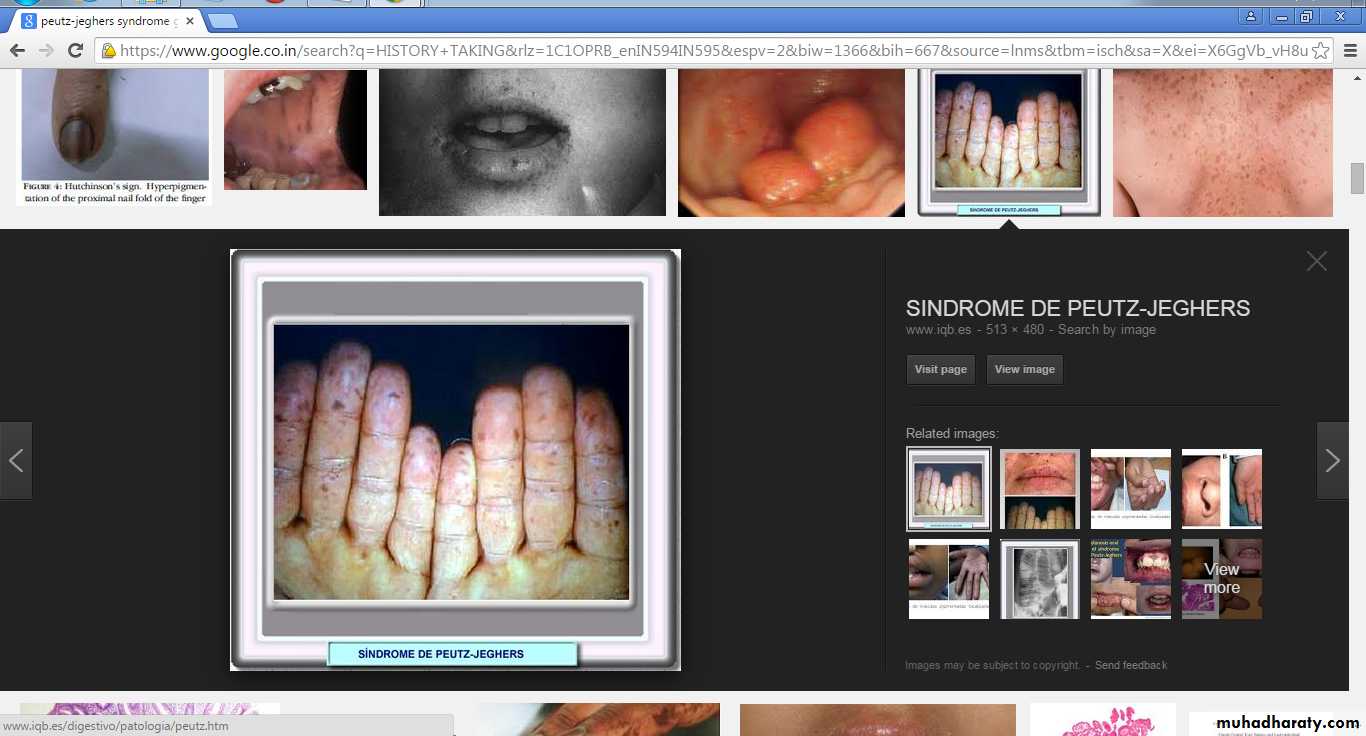
Peutz-Jeghers Syndrome
Peutz-Jeghers SyndromeRare genetic disorder associated with mutation of the LKB1 gene
The melanotic spots of Peutz-Jeghers syndrome are characteristically small and multiple
Obvious around the lips.
The melanotic spots do not require treatment and are not associated with increased risk of melanoma.
Black-to-brown spots of less than 1 mm in size are typically localized on the lower lip and in the perioral are
Peutz-Jeghers Syndrome
Characterized by pigmented mucocutaneous macules,
intestinal hamartomatous polyposis and an increased risk of cancer in many organs, including the small intestine, colon, stomach, pancreas, breast and genital tractGastric polyps
Mucocutaneous symptoms
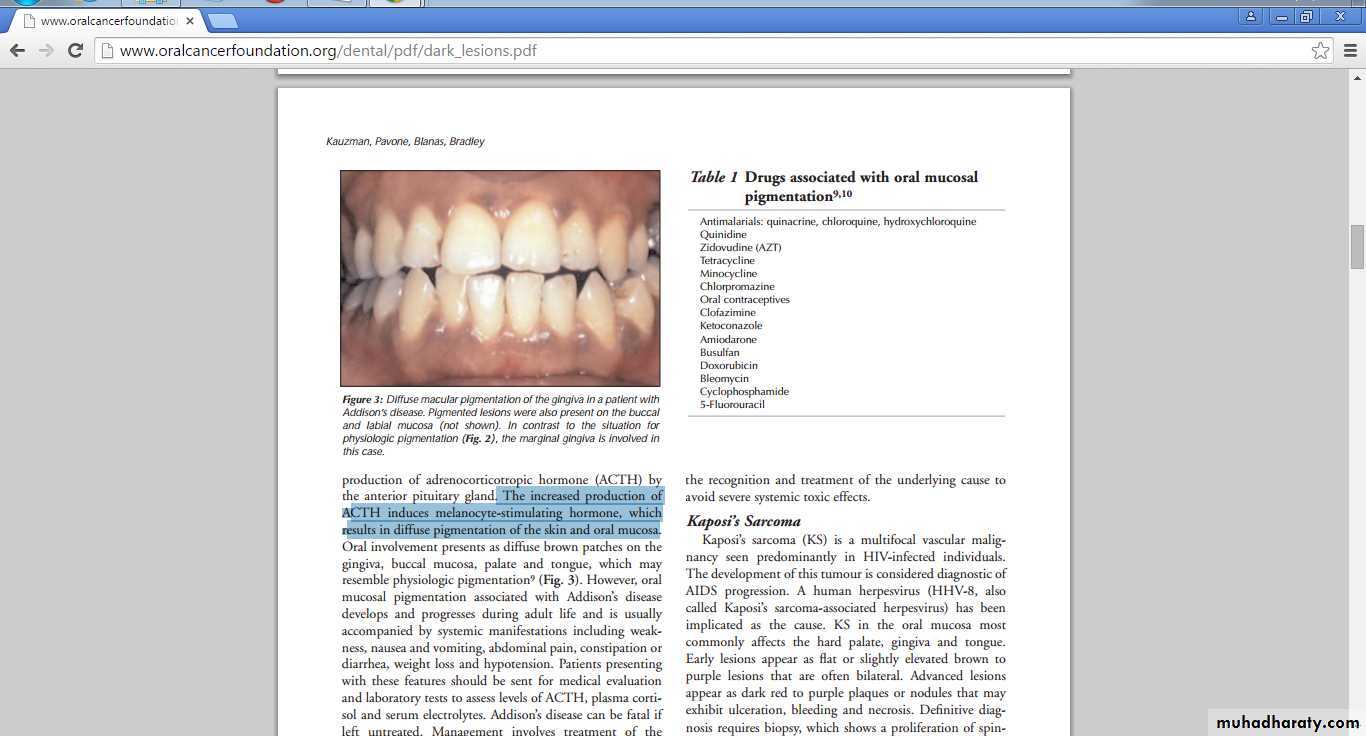
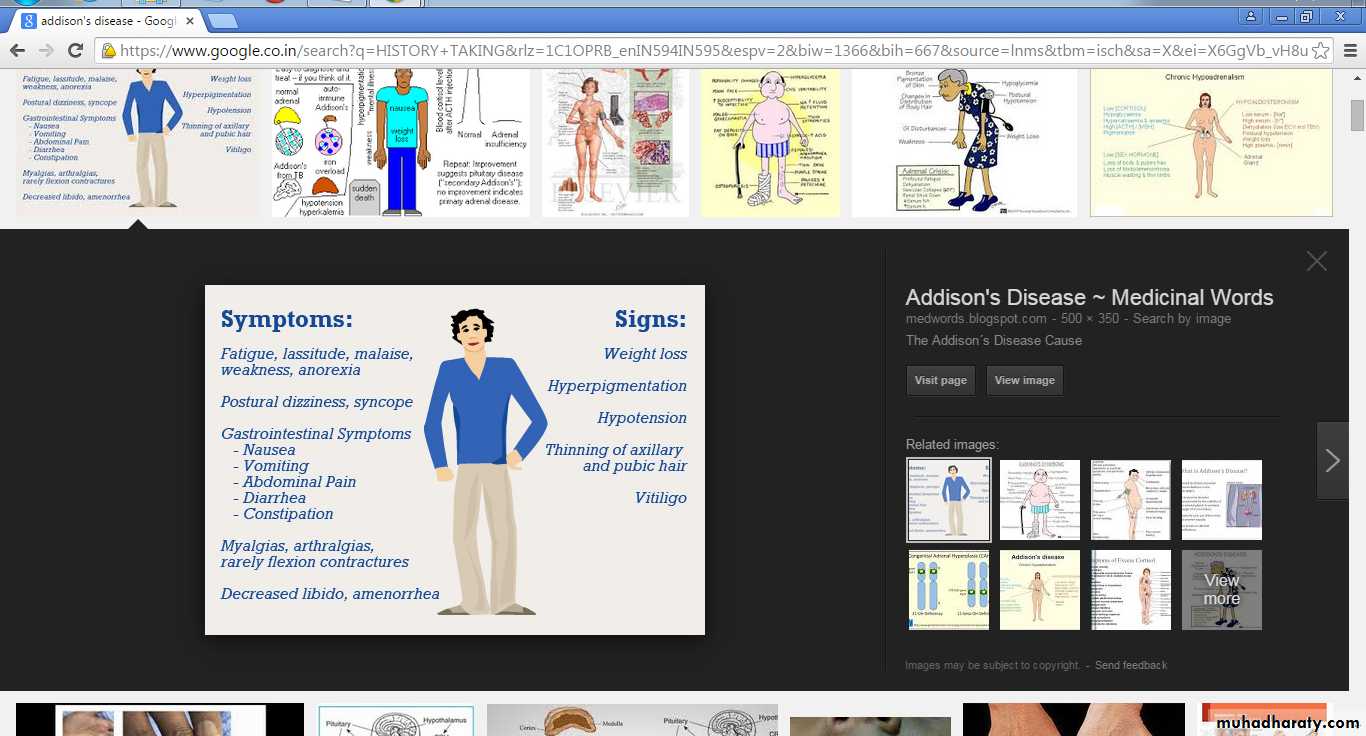
Addisons disease
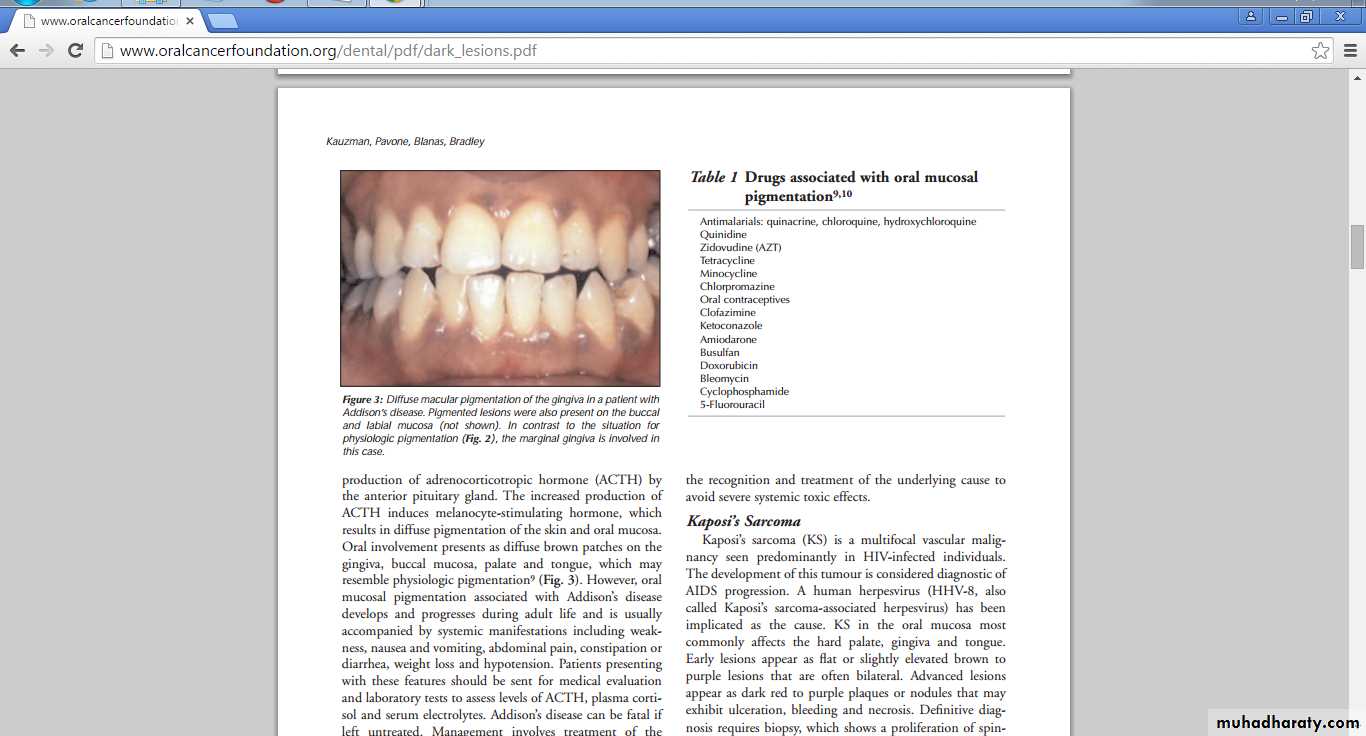
Addison’s disease or primary hypoadrenalismProgressive bilateral destruction of the adrenal cortex by autoimmune disease, infection or malignancy
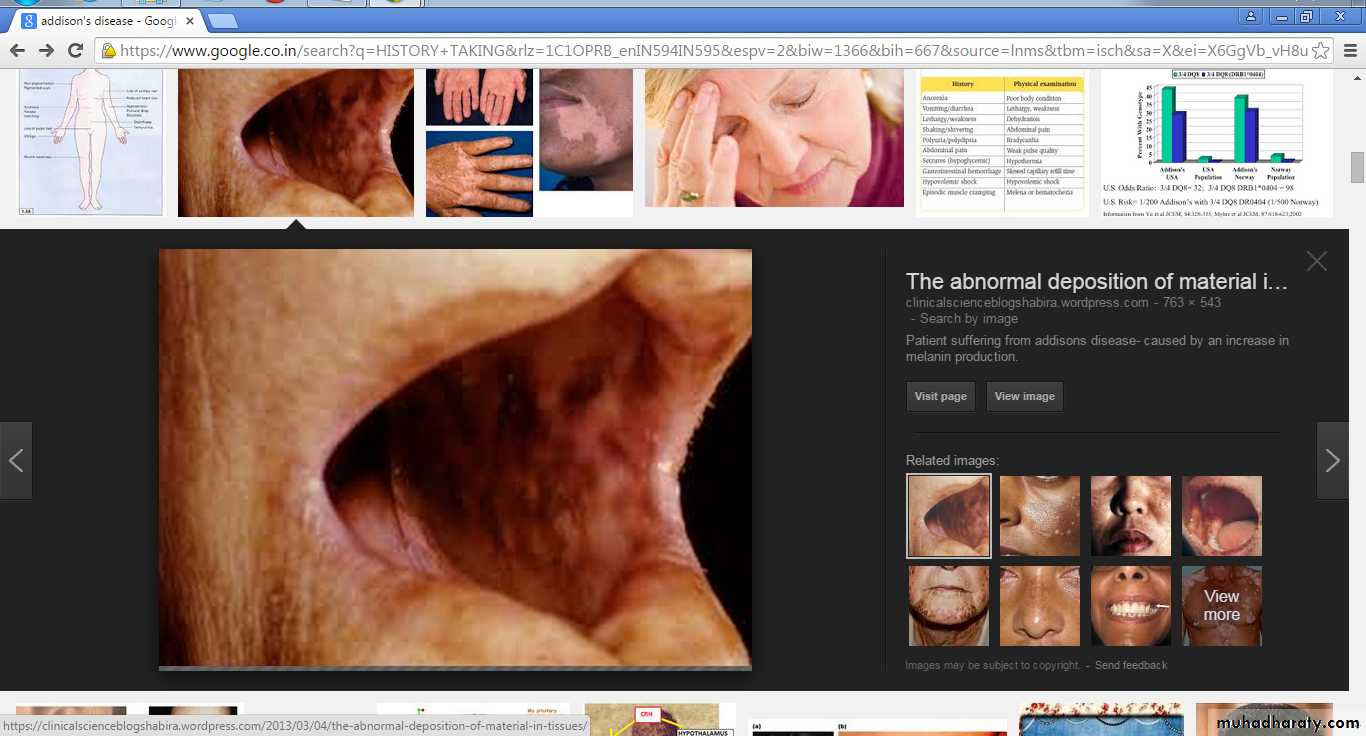
Oral involvement presents as diffuse brown patches on the gingiva, buccal mucosa, palate and tongue
Addison’s disease can be fatal if left untreated
Oral mucosal pigmentation associated with Addison’s disease develops and progresses during adult life
Usually accompanied by systemic manifestations including weakness, nausea and vomiting, abdominal pain, constipation or diarrhea, weight loss and hypotension
ADDISONS DISEASE
The increased production of ACTH induces melanocyte-stimulating hormone, which results in diffuse pigmentation of the skin and oral mucosa
The disappearance of oral lesions may follow the treatment of the underlying condition
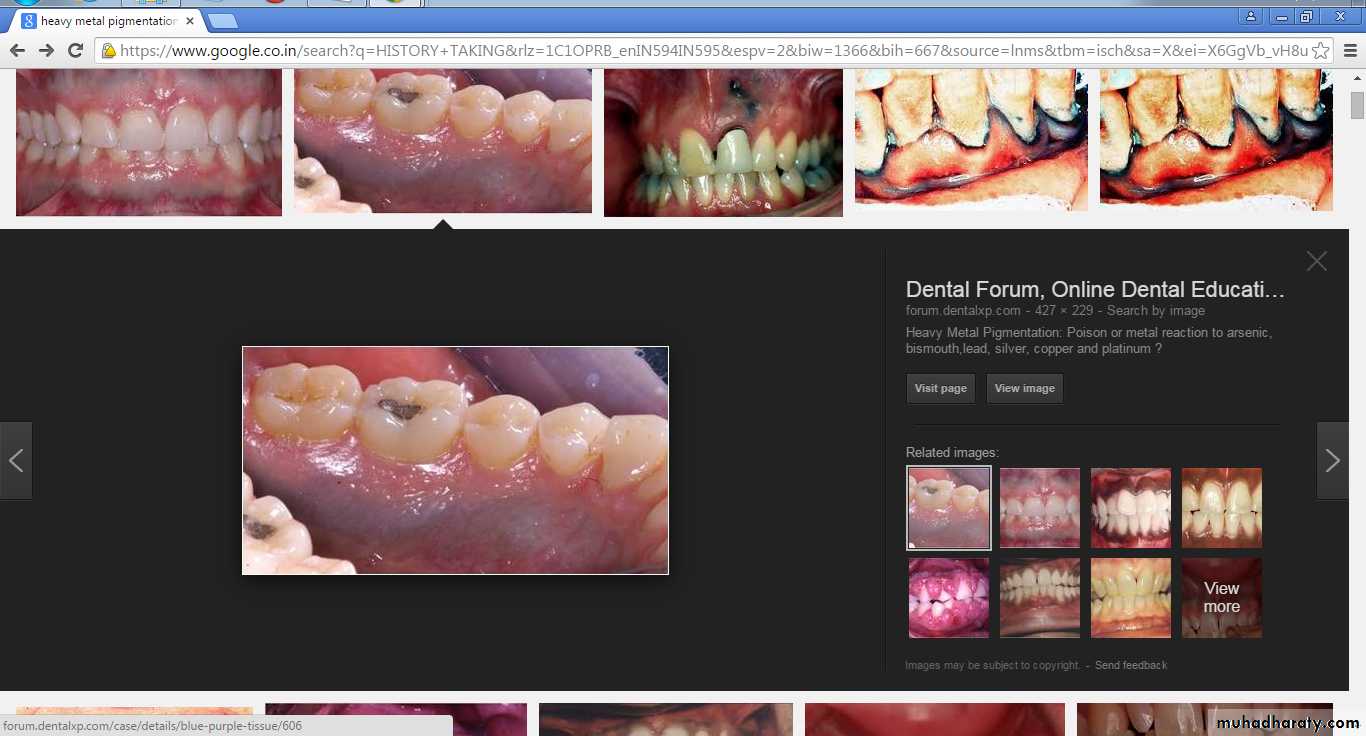
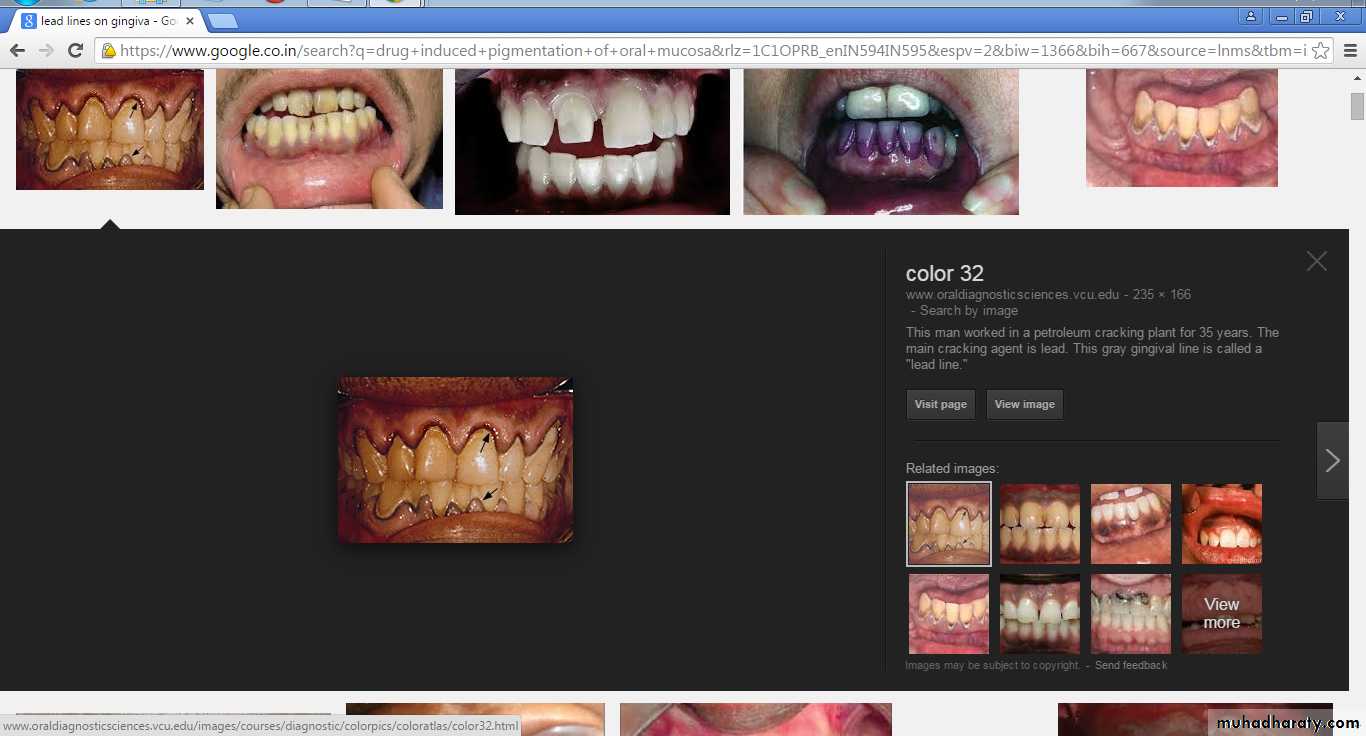
Heavy Metal Pigmentation
Increased levels of heavy metals in the blood represent a known cause of oral mucosal discolourationcommon cause for such increased levels is occupational exposure
In children, possible sources of exposure include lead-contaminated water or paint and mercury- or silver-containing drugs
Lead, bismuth, mercury, silver, arsenic and gold ingestion and occupational exposure leads to pigmentation
Diffuse mucosal ulceration and a metallic taste may also be noted.
Lead line of gingiva
Bismuth line of gingiva
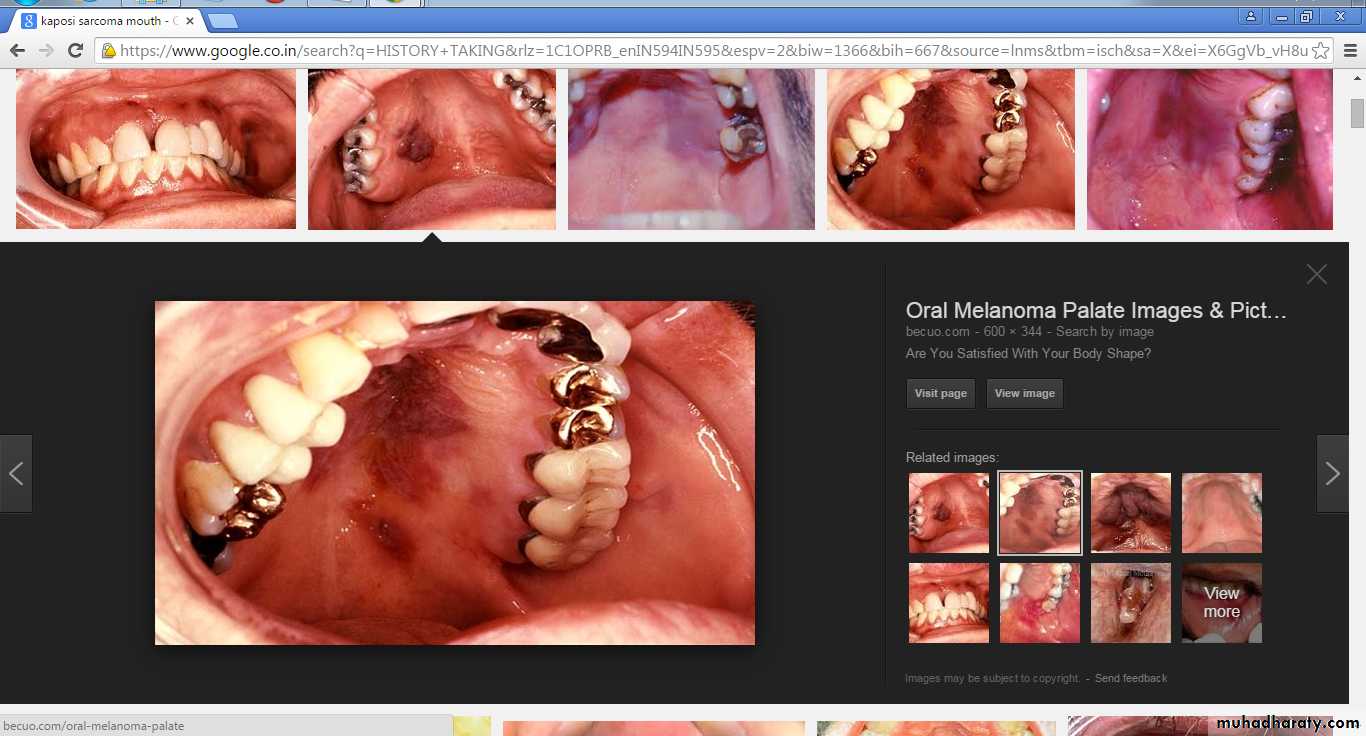
Kaposi’s SarcomaMultifocal vascular malignancy
Diagnostic of AIDS progression
KS in the oral mucosa most commonly affects the hard palate, gingiva and tongue
Early lesions appear as flat or slightly elevated brown to purple lesions that are often bilateral.
Definitive diagnosis requires biopsy
Advanced lesions appear as dark red to purple plaques or nodules that may exhibit ulceration, bleeding and necrosis
Kaposi sarcoma
Kaposi sarcoma (KS) is a cancer that develops from the cells that line lymph or blood vessels.
Appears as tumors on the skin or on mucosal surfaces
Kaposi sarcoma tumors usually manifest as bluish-red or purple bumps
Options for treatment include antiviral combination chemotherapy,
cryotherapy, or radiation therapy.
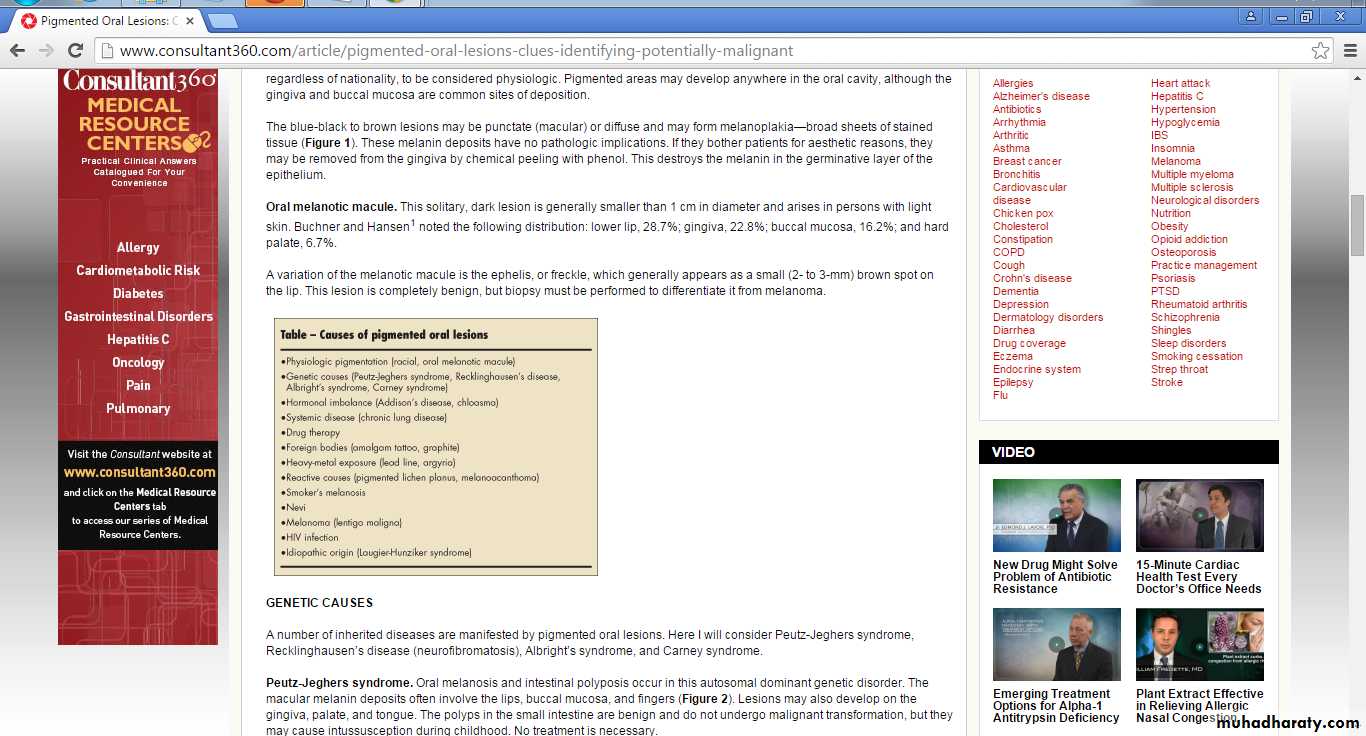
Drug-Induced Pigmentation
The pathogenesis of drug-induced pigmentation varies, depending on the causative drugIt can involve accumulation of melanin, deposits of the drug or one of its metabolites
Mucosal discolouration associated can be described as blue–grey or blue–black
In most cases only the hard palate is involved
Laboratory studies have shown that these drugs may produce a direct stimulatory effect on the melanocytes.
Cotrimazole was the most common drug associated to oral pigmentation followed by tetracycline
Drugs Associated With Oral Pigmentation
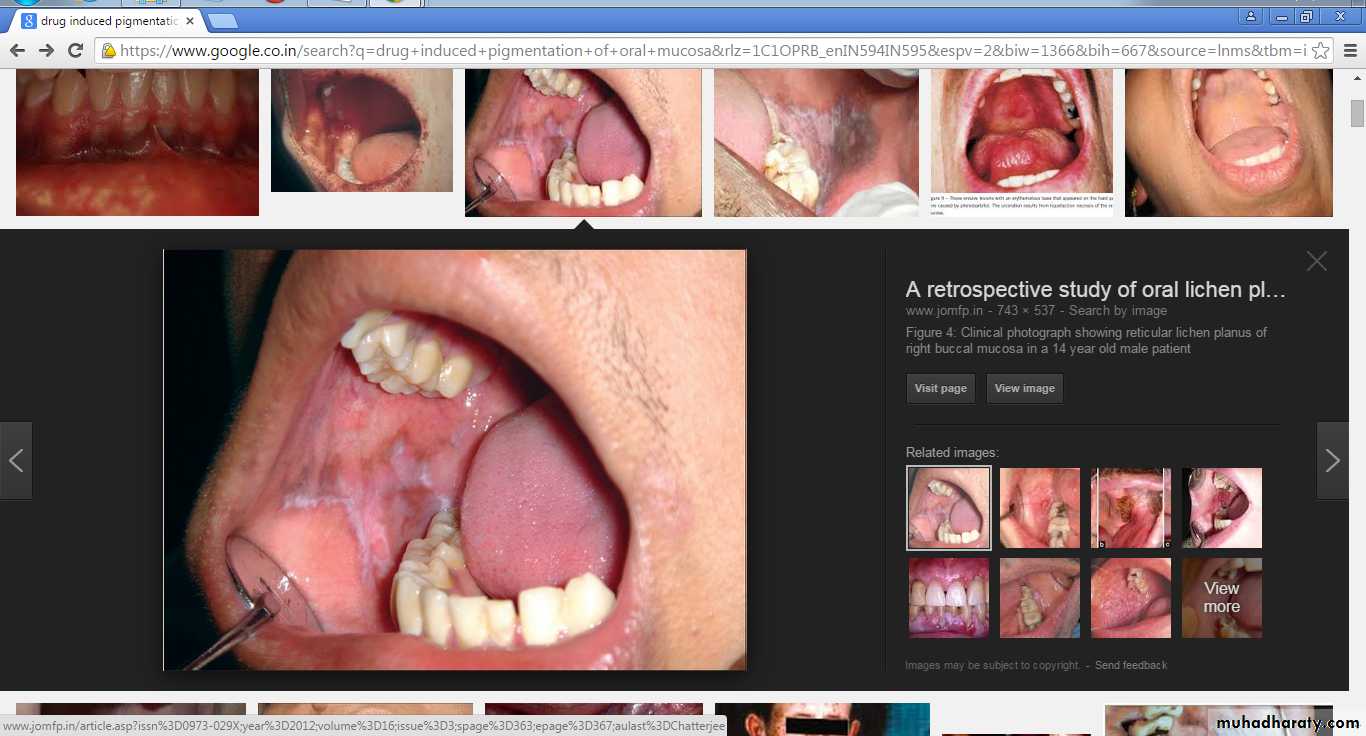
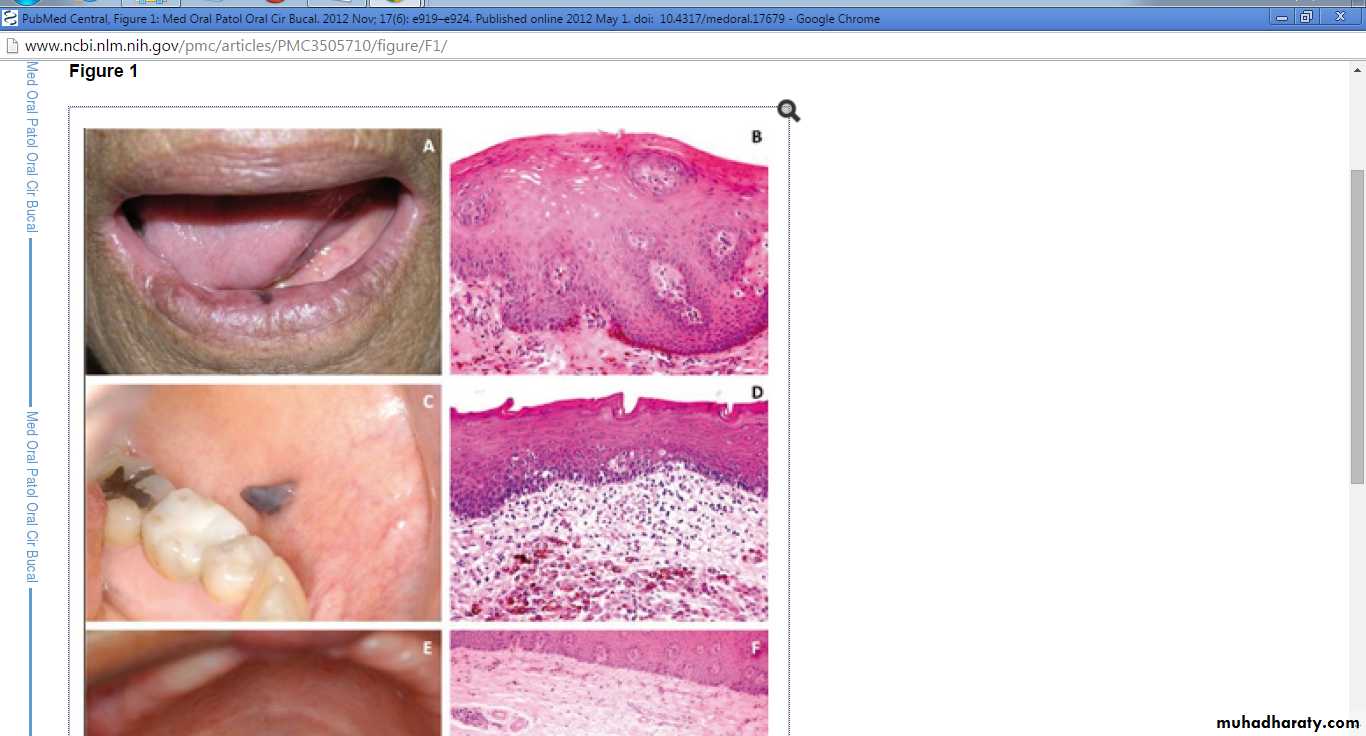
Post-inflammatory Pigmentation
Long-standing inflammatory mucosal diseases, such as oral lichen planus , pemphigus or pemphigoid can cause mucosal pigmentation
The pathogenesis of post inflammatory pigmentation remains unclear
Clinically, multiple brown–black pigmented areas are noted adjacent to reticular, erosive or vesicular lesions.
Generally, the resolution of the inflammatory process allows the cessation of oral pigmentation.
Reticular lichen planus with pigmentation
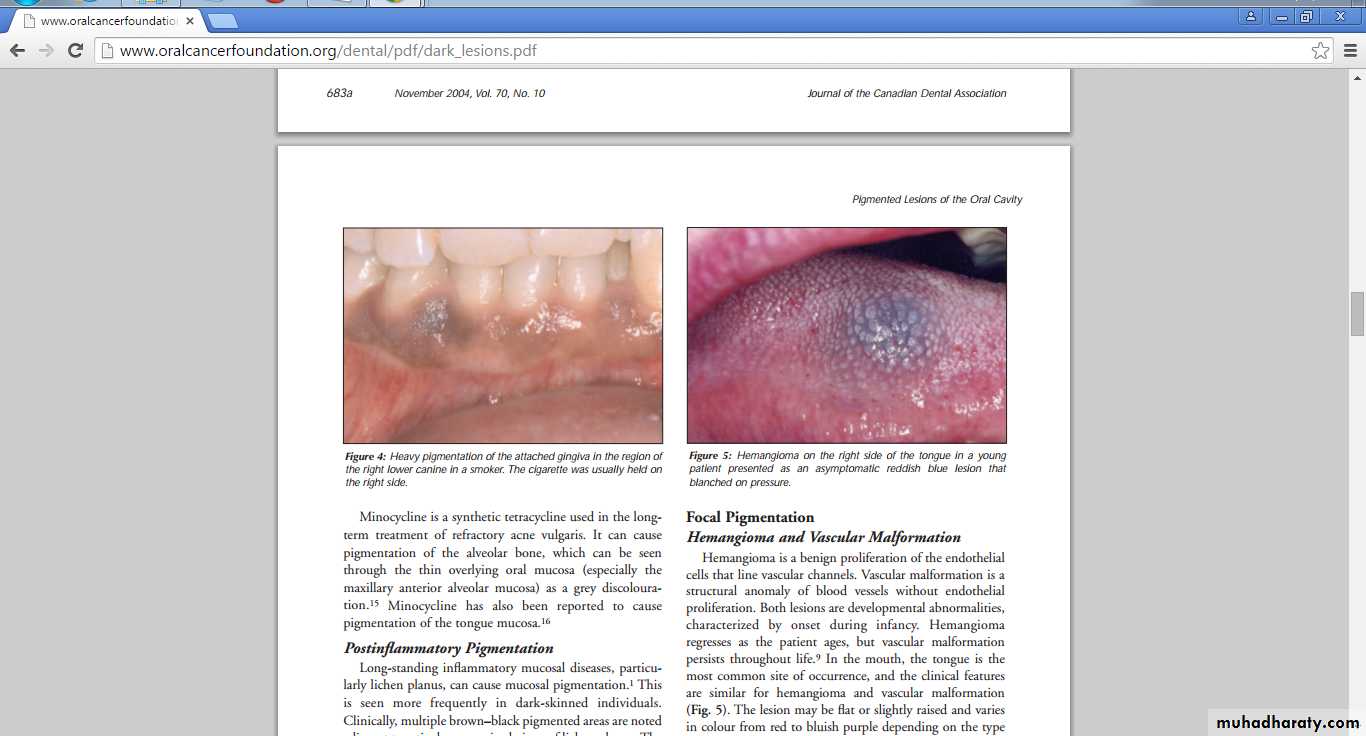
Smoker’s MelanosisIncreased production of melanin, provide a biologic defence against the noxious agents present in tobacco smoke
Smoker’s melanosis occurs in up to 21.5% of smokers.
The intensity of the pigmentation is related to the duration and amount of smoking
The brown–black lesions most often involve the anterior labial gingiva followed by buccal mucosa
Characterized by discrete or coalescing multiple brown macules that usually involve the attached mandibular gingiva on the labial side
Unlike heavy-metal pigmentation, which affects the free gingival margin, smoker’s melanosis develops on the attached gingiva
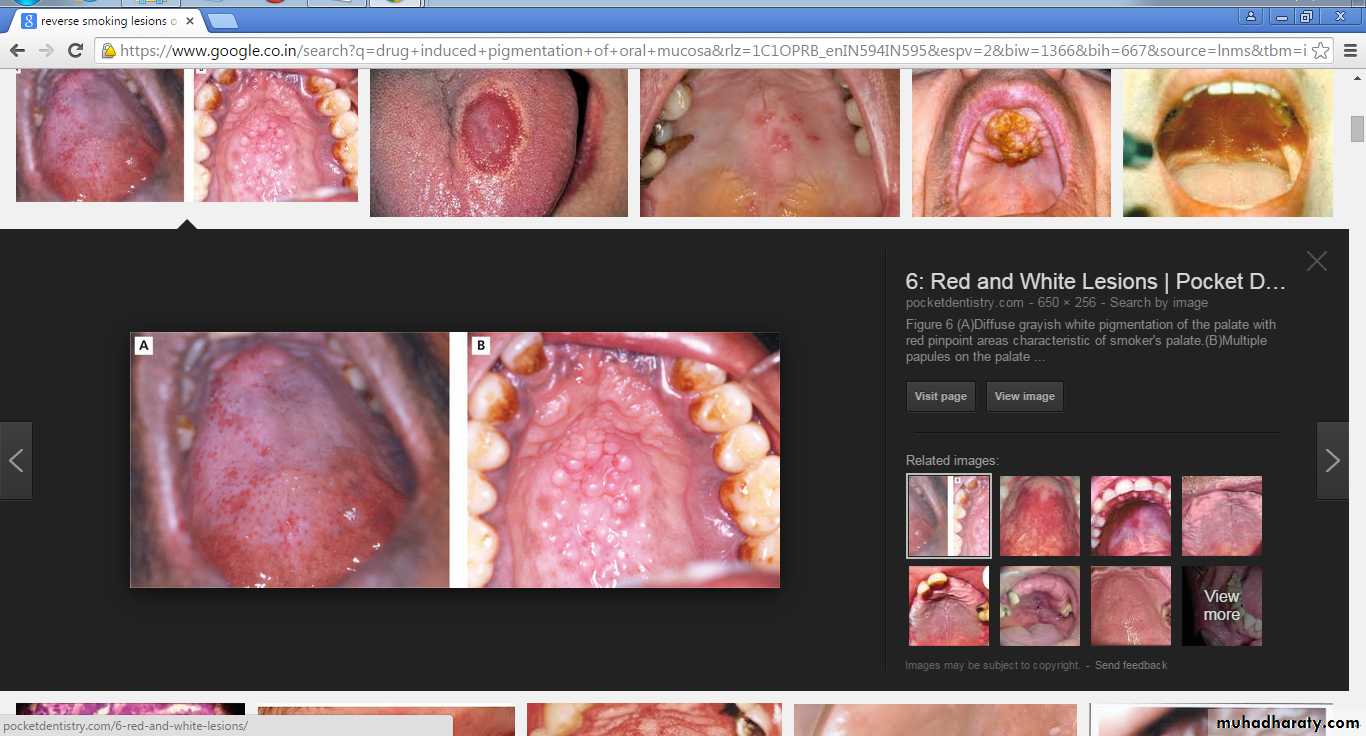
Diffuse grayish white pigmentation of palate with red pin point areas- smokers palate
Focal Pigmentation
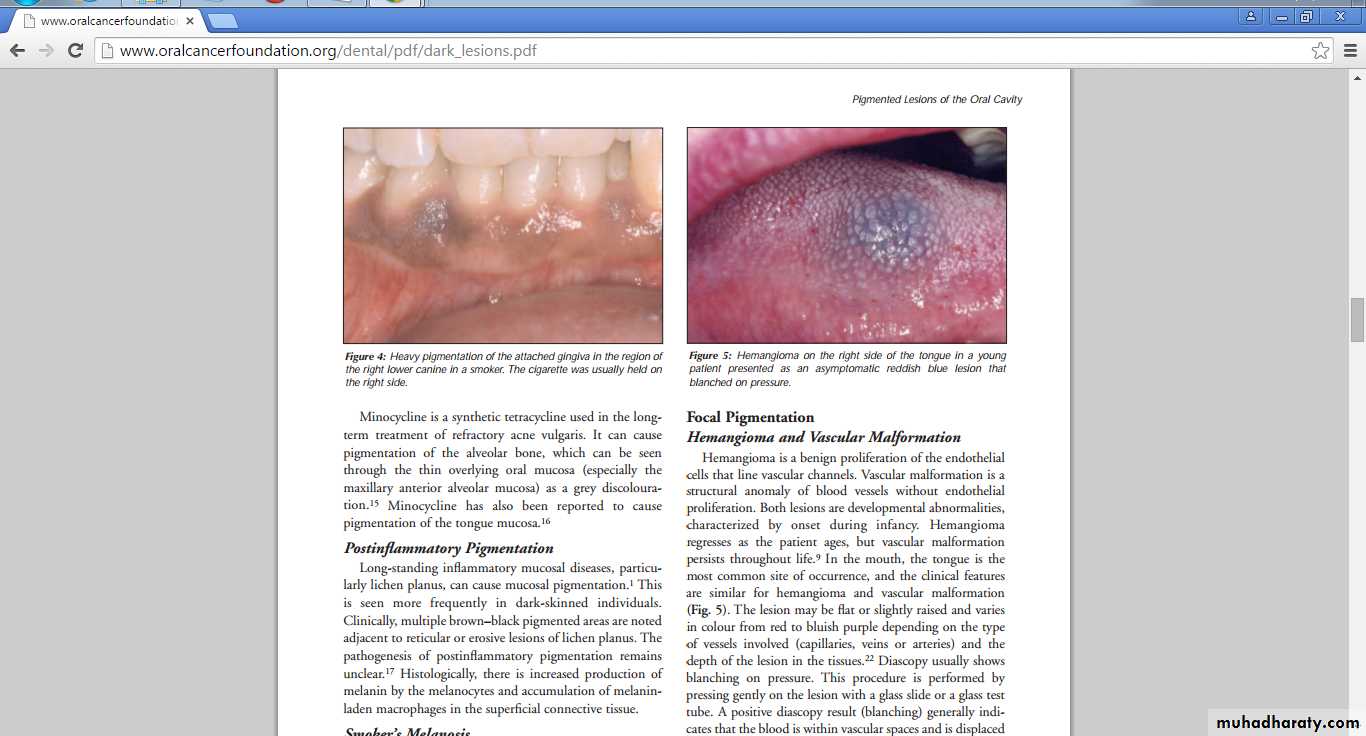
HemangiomaHemangioma is a benign proliferation of the endothelial cells that line vascular channels.
Hemangioma regresses as the patient ages
The lesion may be flat or slightly raised
Varies in color from red to bluish purple depending on the type of vessels involved
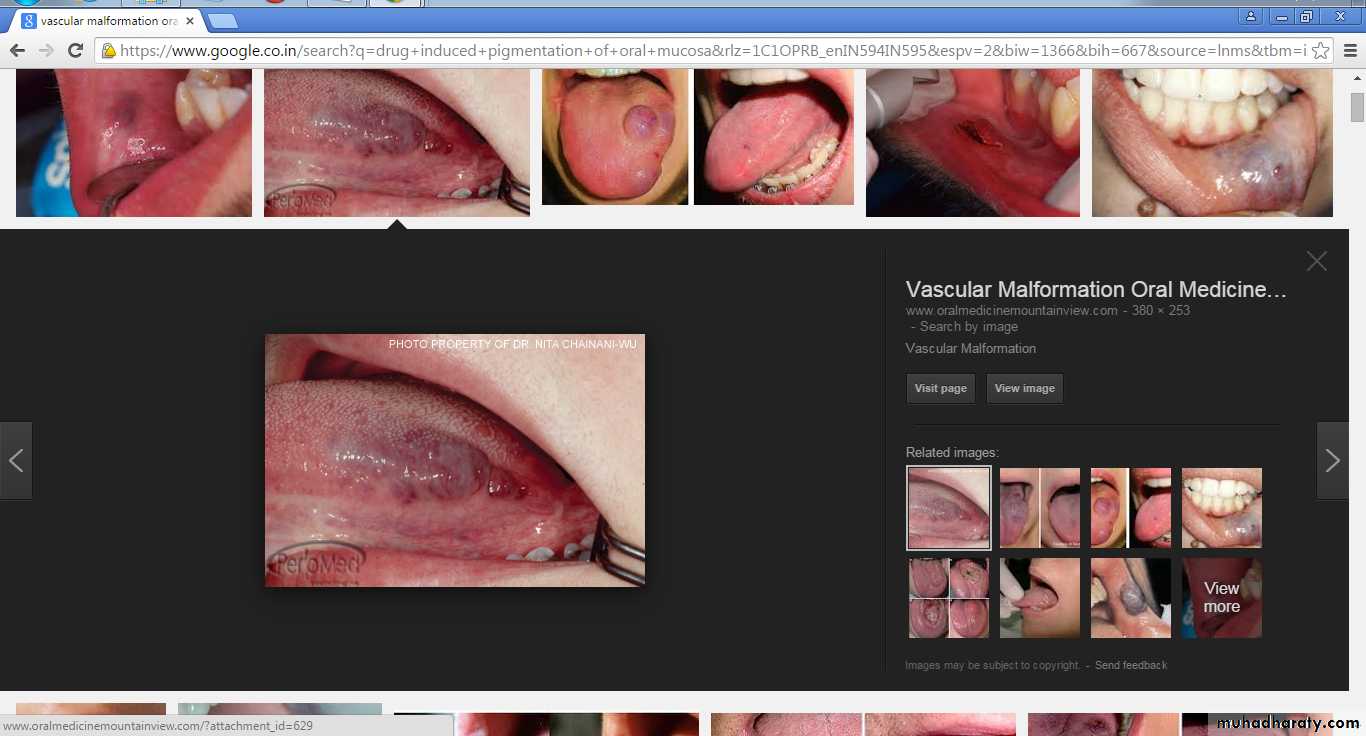
Vascular malformation
Vascular malformation is a structural anomaly of blood vessels without endothelial proliferationVascular malformation persists throughout life
Haemangioma
VMIn the mouth, the tongue is the most common site of occurrence, and the clinical features are similar for hemangioma and vascular malformation
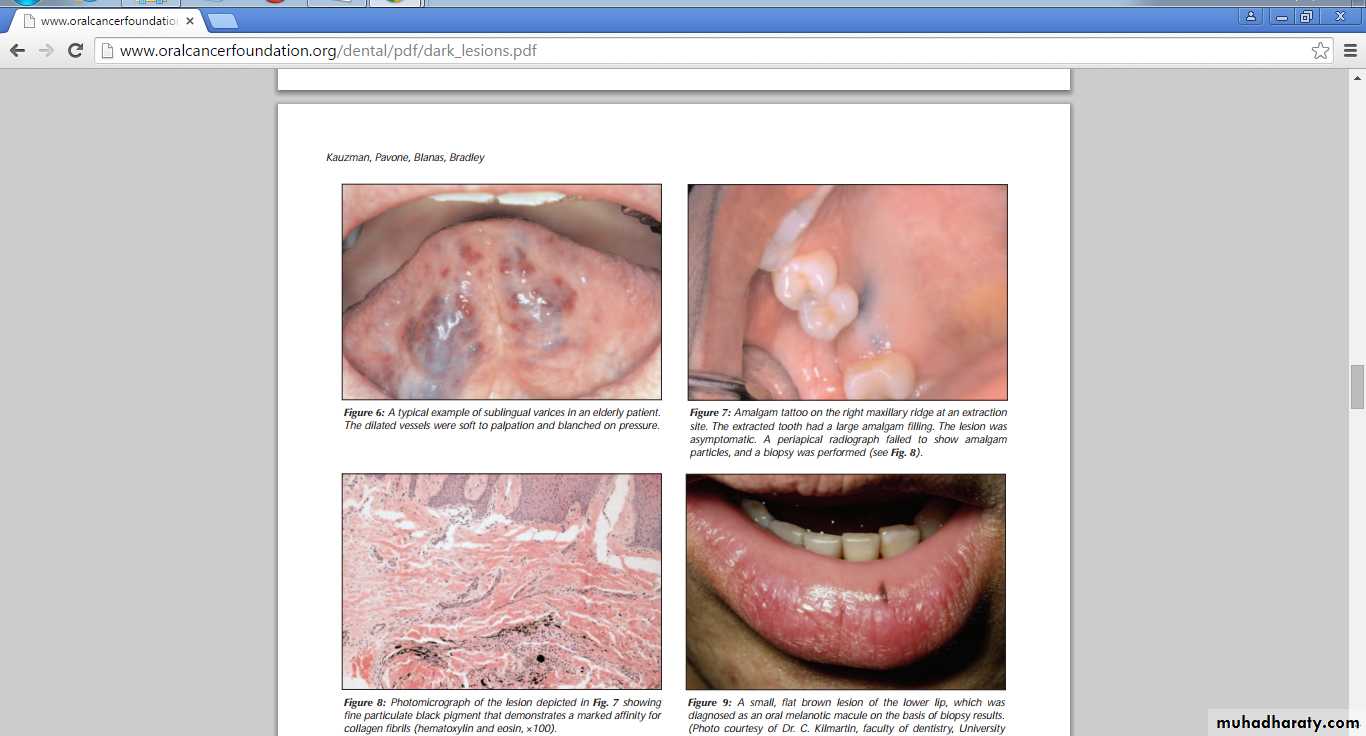
Varix and Thrombus
Varices are abnormally dilated veinsThe most common intraoral location is the ventral surface of the tongue
If the varix contains a thrombus, it presents as a firm bluish purple nodule that does not blanch on pressure
multiple bluish purple, irregular, soft elevations that blanch on pressure
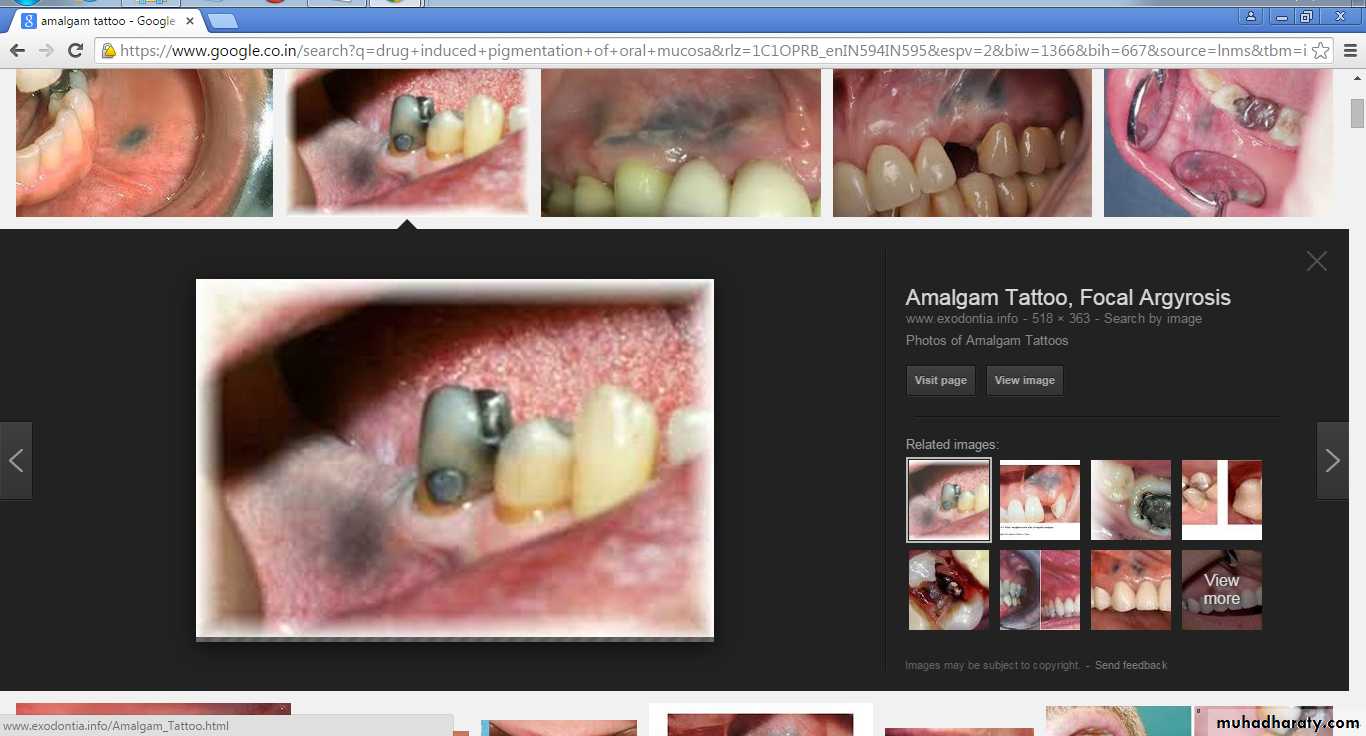
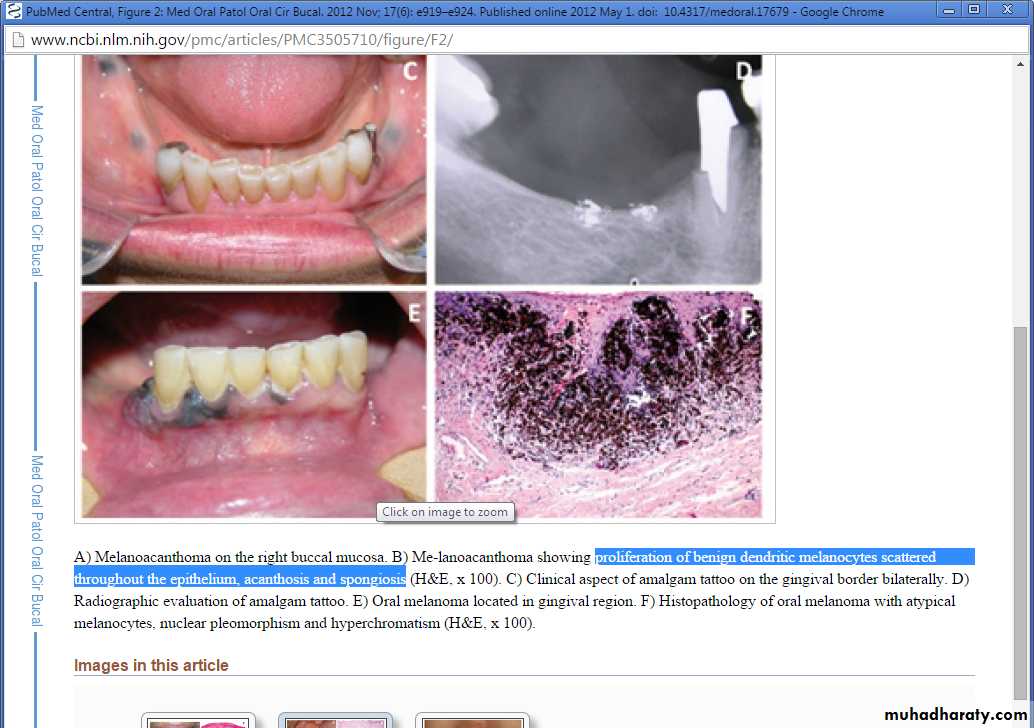
Amalgam Tattoo and Other Foreign-Body PigmentationAmalgam tattoo is caused by the presence of metallic material in the oral tissues.
Amalgam tattoos are painless, gray-blue macules that range in size from a few millimeters to greater than 1 cm.The gingiva and alveolar mucosa are the most common sites of involvement
No signs of inflammation are present at the periphery of the lesionAccidental implantation of dental filling material into the gingival or buccal mucosa
Graphite accumulation
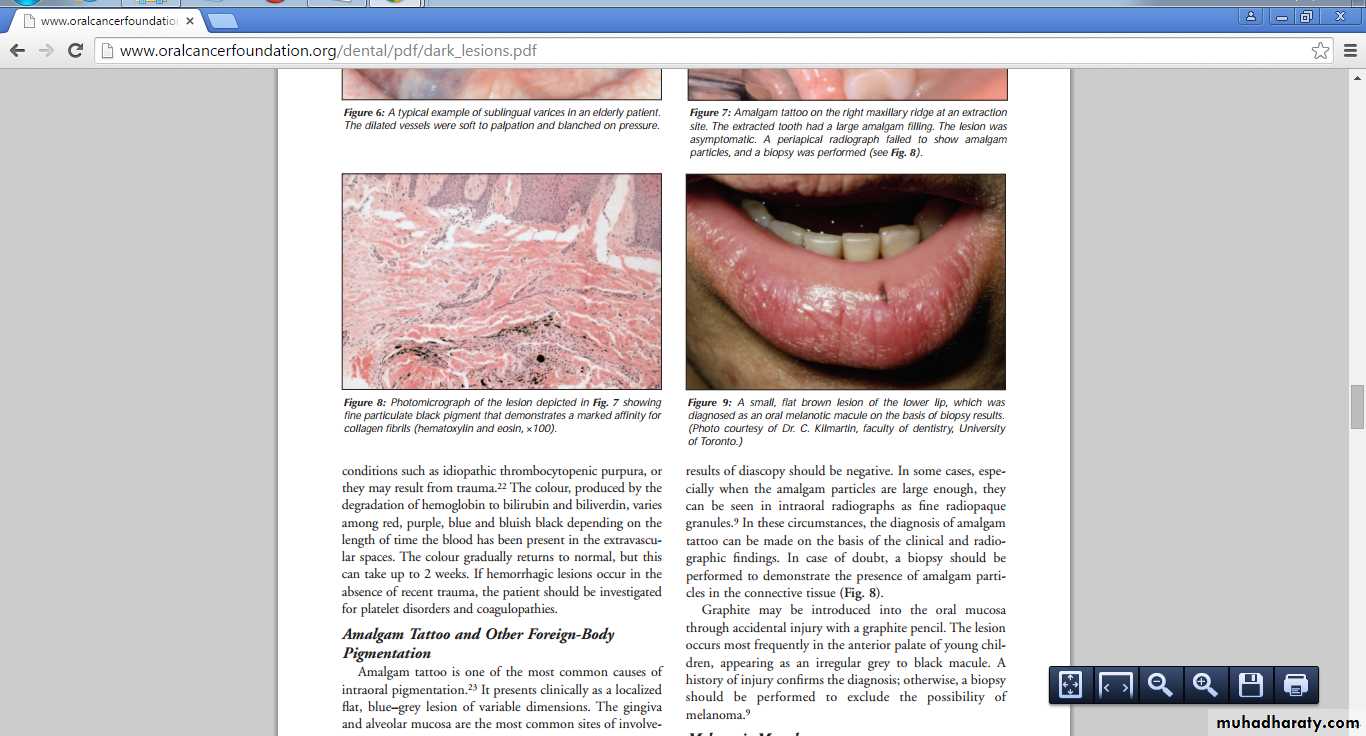
Melanotic MaculesThe labial melanotic macule is a benign pigmented lesion
oral melanotic macule is the same lesion seen inside the oral cavity, most commonly on the gingiva, buccal mucosa and palate
Melanotic macules are usually smaller than 1 cm in diameter and show a well-demarcated smooth border
The colour may be light or dark brown and is homogeneous within each lesion.
They usually occur as single lesions
Labial melanotic macule.
Increased numbers of melanocytes along the junctional zoneIntraoral melanocytic nevus
Nevus cells located within the connective tissue
Pigmented Nevi
Junctional nevi are flat and dark brown in color because the nevus cells proliferate at the tips of the rete pegs close to the surface.
Intramucosal and compound nevi are typically light brown, dome-shaped lesions
Melanocytic nevi constitute benign neoplasms of cutaneous melanocytes
Proliferation of benign neoplastic melanocytes along the sub mucosal junction -=junctional nevus
Migration of these cells to the underlying mesenchyme tissue =compound nevus
Loss of the junctional component of the nevi, so that all remaining melanocytes are located within the sub epithelial connective tissue stroma = sub epithelial nevus
Pigmented Nevi
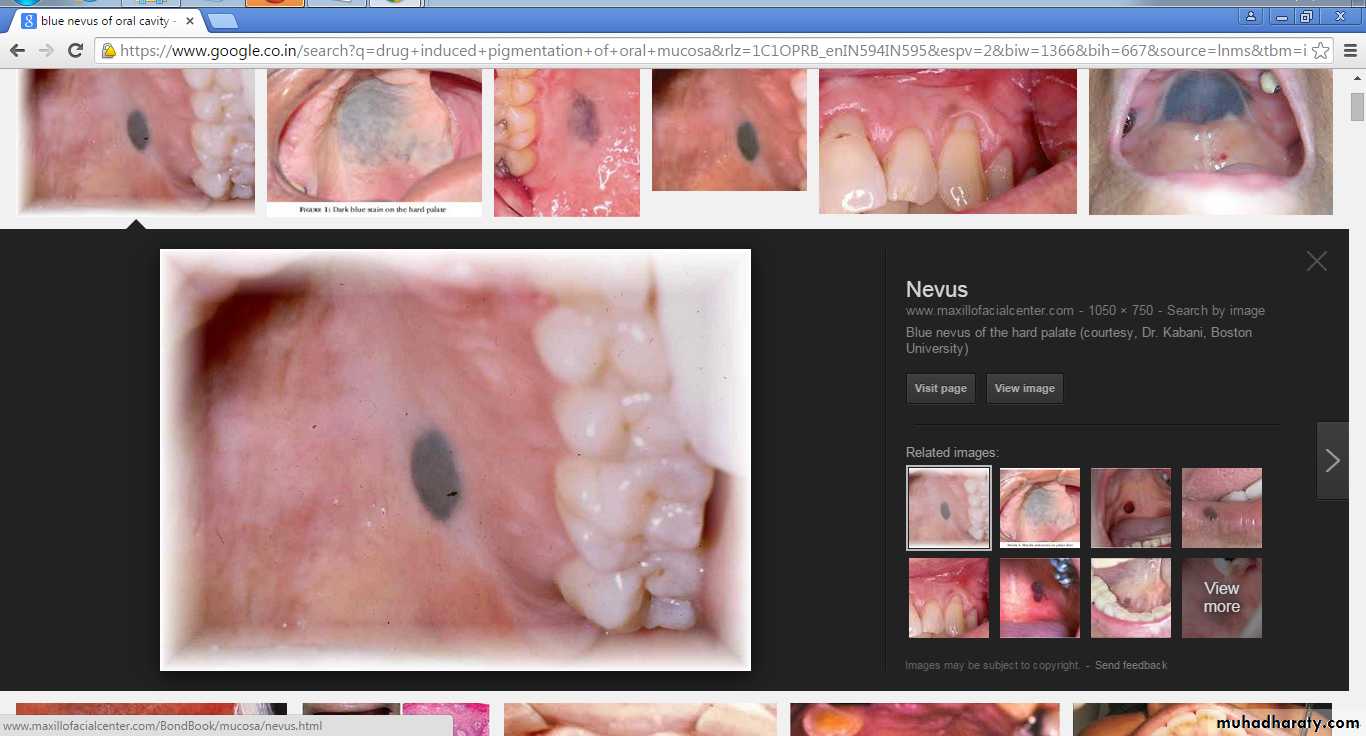
Blue nevus
A blue nevus is a benign, acquired melanocytic lesion that typically presents as an asymptomatic, blue-black smooth-surfaced macule or papule and usually measures less than 6 mm in diameter.
Two thirds of all intraoral blue nevi are found on the hard palate, and the buccal mucosa is the second most common site of presentation.
The common blue nevus, which is the most frequent subtype seen in the oral cavity is characterized by an Intramucosal proliferation of elongated, bipolar, spindle-shaped melanocytes.
Blue nevus on hard palate
Blue nevi are characterized by proliferation of dermal melanocytes within the deep connective tissue at some distance from the surface epithelium, which accounts for the blue colorOral Melanoacanthoma
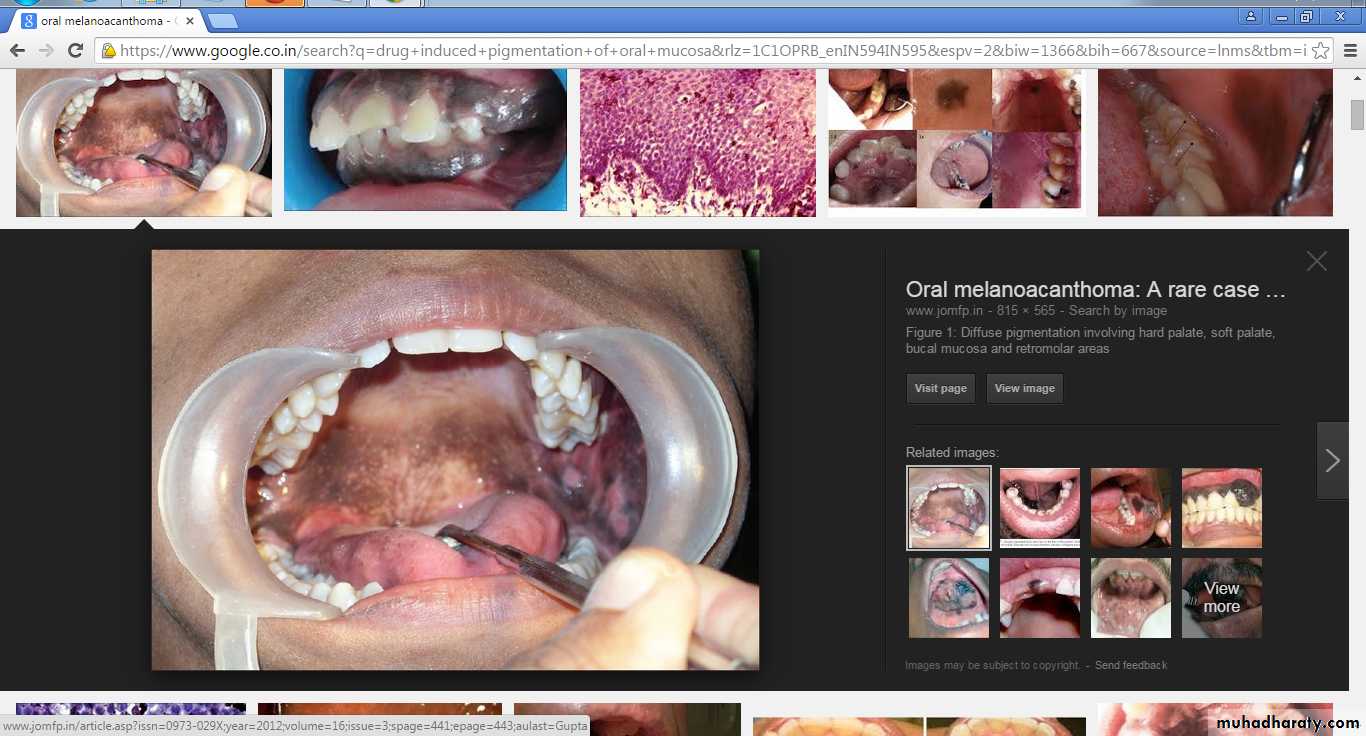
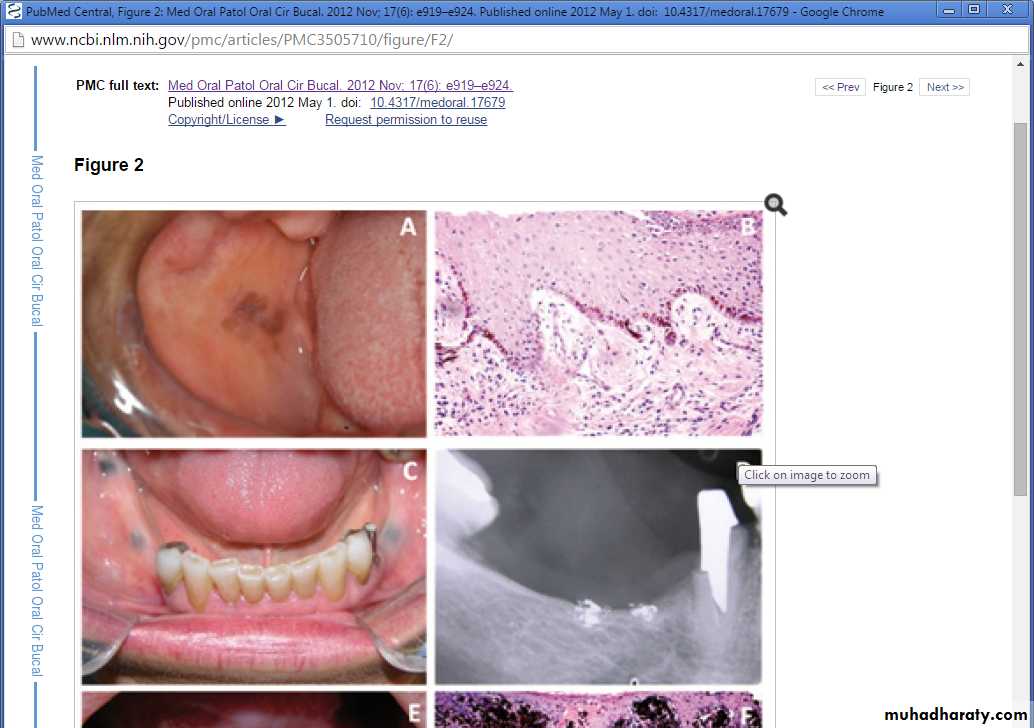
Oral melanoacanthoma is an uncommon benign pigmented lesion of the oral mucosacharacterized by proliferation of dendritic melanocytes scattered throughout the thickness of an acanthotic and hyperkeratotic surface epithelium
Clinically, the lesion appears flat or slightly raised and is hyper pigmented, the color ranging from dark brown to black.
The buccal mucosa and soft palate are the most common sites of occurrence.
Melanoacanthoma on the right buccal mucosa
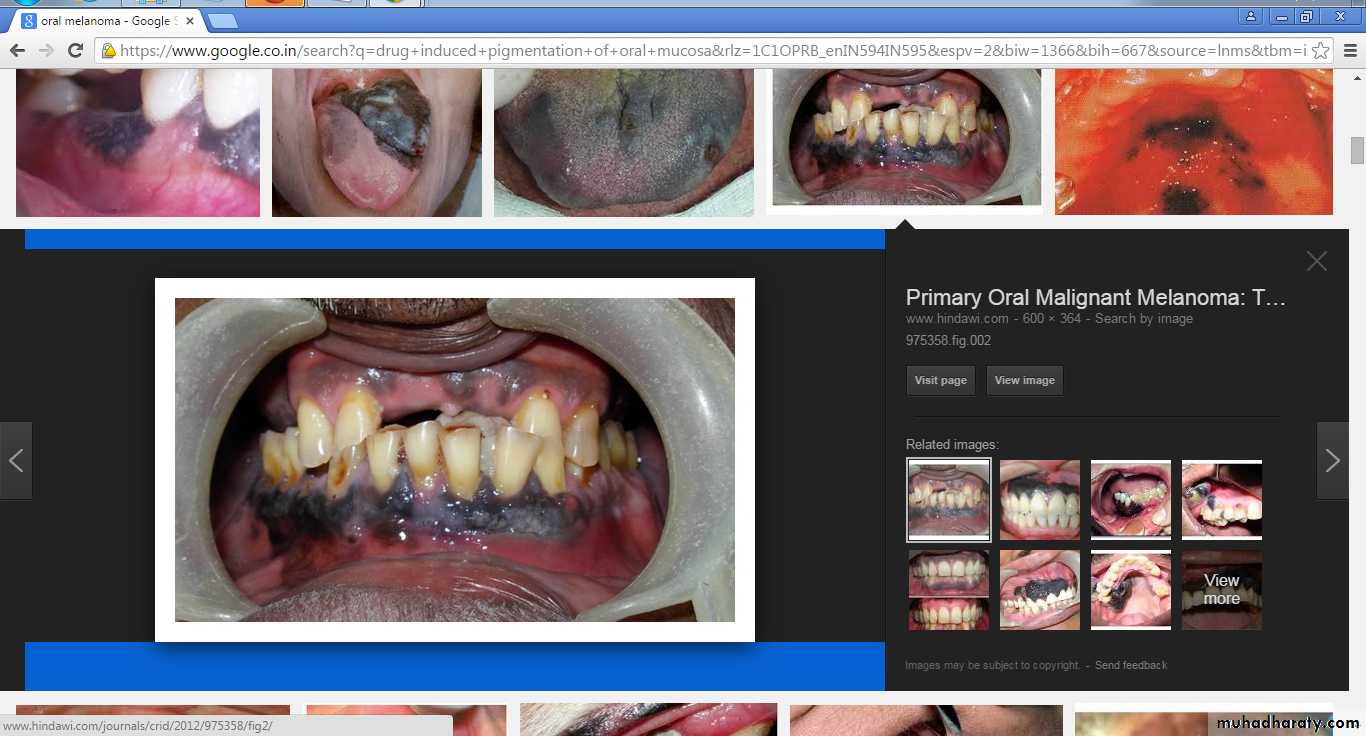
Proliferation of benign dendritic melanocytes scattered throughout the epithelium.Oral Melanoma
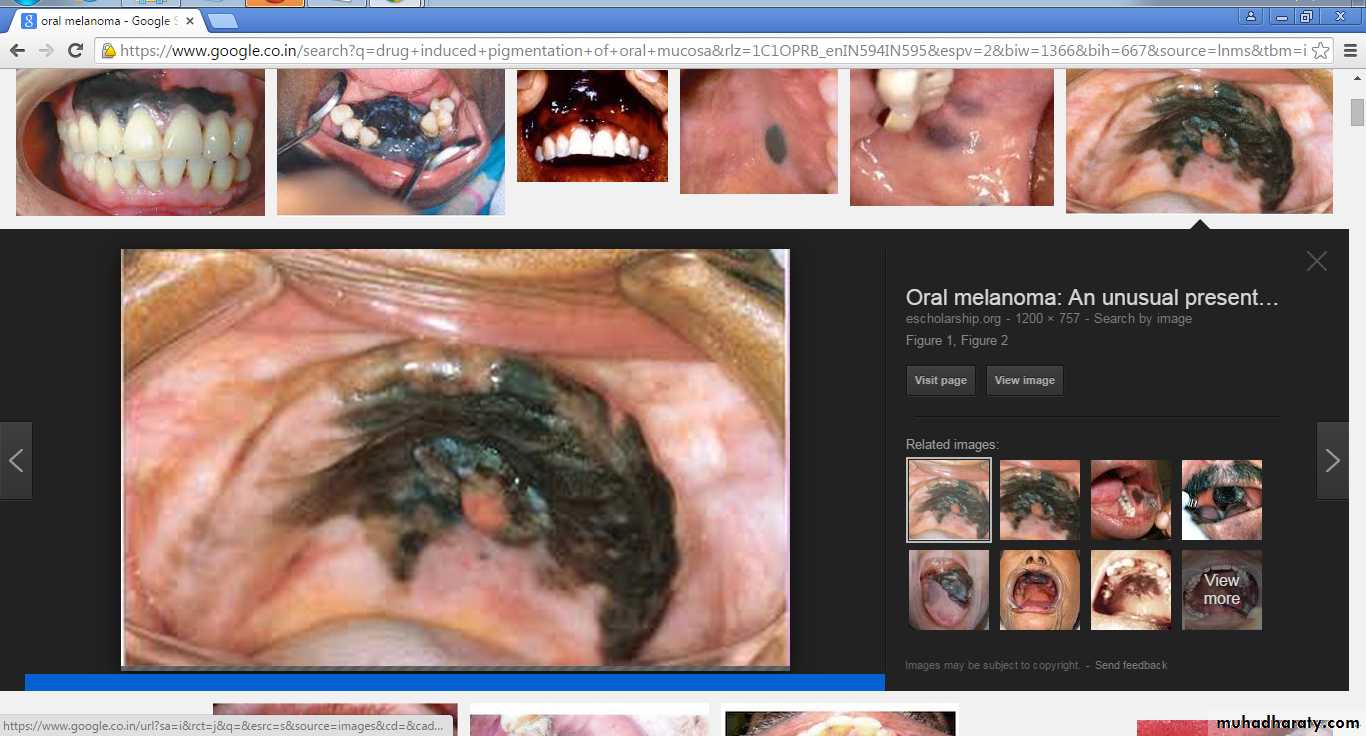
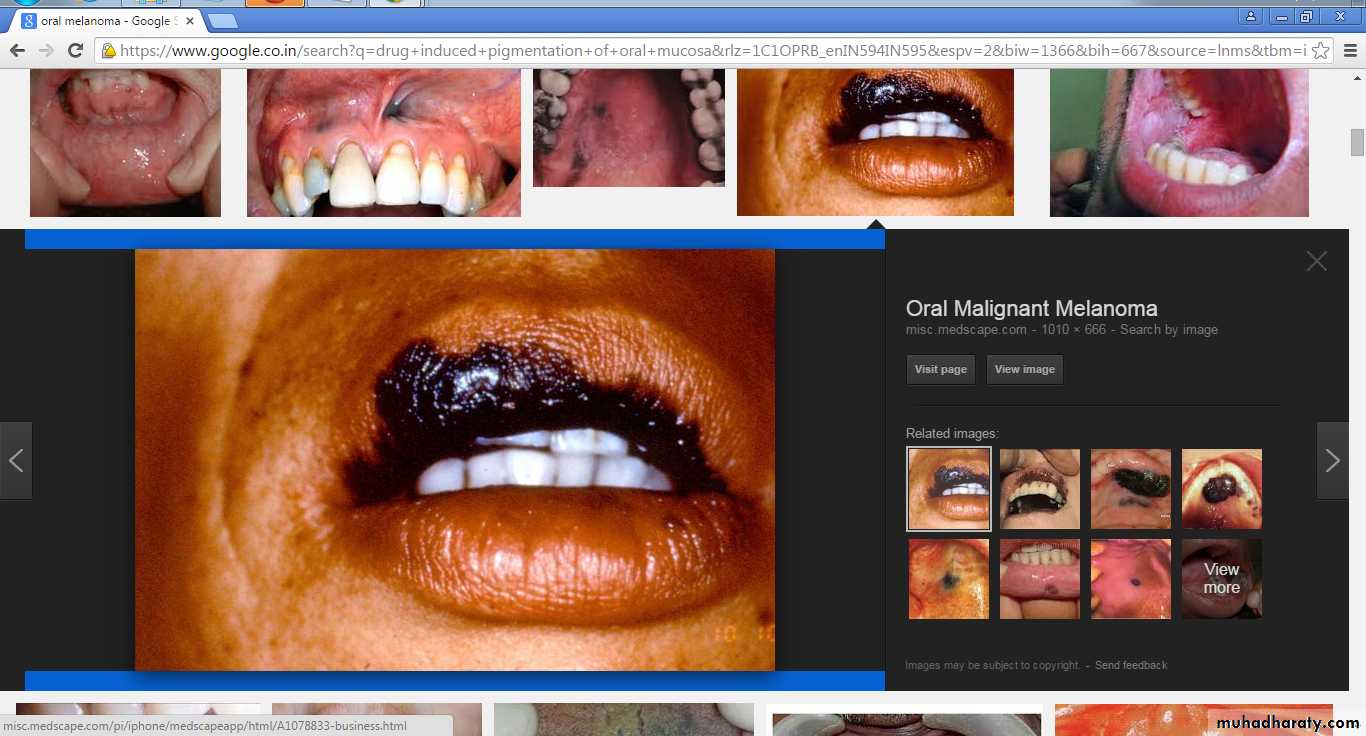
It is characterized by proliferation of malignant melanocytes along the junction between the epithelial and connective tissues, as well as within the connective tissueThe most common site is the palate, followed by the gingiva
oral melanoma may present as an asymptomatic, slow-growing brown or black patch with asymmetric and irregular borders or as a rapidly enlarging mass associated with ulceration, bleeding, pain and bone destruction
Histopathology of oral melanoma with atypical melanocytes, nuclear pleomorphism and hyperchromatism
They tend to be more aggressive than their cutaneous counterparts
Treatment involves radical surgical excision with clear marginsRadiation and chemotherapy are ineffective