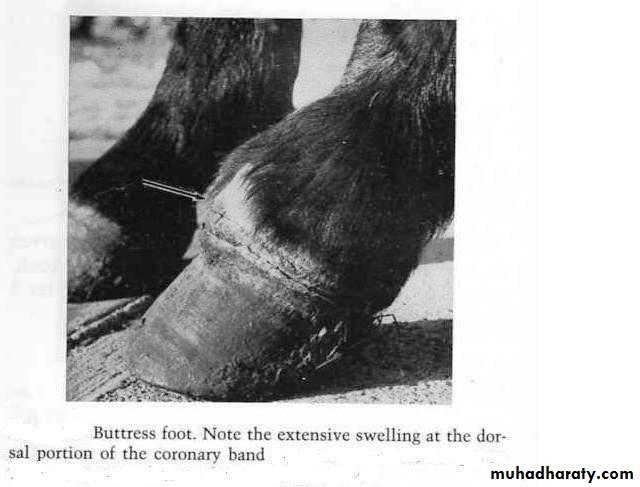
Pyramidal Disease (Buttress Foot)
It is due to new bone growth in the region of the extensor process of the distal phalanx, this new bone growth may be due to fracture or periostitis of the extensor process of the distal phalanx. Healing of the pathologic changes produces new bone growth, causing an enlargement at the coronary band at the center of the hoof.Etiology:-
Excessive strain on the long or common digital extensor and the extensor branch of the suspensory ligament as they insert on the extensor process of the distal phalanx. This results in a periostitis that causes new bone growth or in fracture of the extensor process.
Horses with high heels and short toes and horses that move with limbs lifted high in a short and rapid manner are predisposed to this disease.
Clinical Sings:-
Sings of lameness are not specific, but the horse show a shortened stride movement.
The horse tend to land heavily on the heels.
In early stages, heat, pain and some swelling are evident at the coronary band in the center of the wall, and lameness is present in all gaits.
The hair shows a tendency to stand up right at the center of the coronary band, and the horse flinches when figure pressure is put on the affected tissues.
Arthritis of the coffin joint results and usually becomes chronic.
Treatment:-
No treatment is of particular value for this disease but the following treatment can be done.Firing and blistering have been used but are of doubtful values.
In early cases injection of corticoids and immobilization of the part with a cast may be of some help.
Palmer digital neurectomy may relieve some sings of lameness and allow limited use of the horse.
Radiation therapy has been suggested to reduce the development of the periostitis.
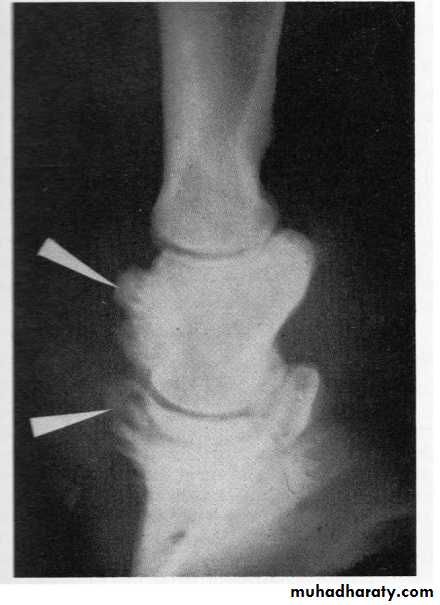
Buttress foot changes on radiograph. The new bone growth is shown by the upper arrow on the middle phalanx. The lower arrow shows new bone growth on the extensor process of the distal phalanx..
Navicular Disease(Pododotrochleosis)
It is a chronic progressive degenerative disease that affects the navicular bone, navicular bursa, and flexor tendons. It is one of the most common causes of intermittent, often- shifting, forelimb lameness in horses between 4 and 15 years of age. North America male Quarter horses are more susceptible, while the disease is rarely diagnosed in ponies or Arabian horses.Although the hind limbs can be affected , but it is considered a disease of the forelimbs.
Factors responsible for navicular disease syndrome:-
Hereditary predisposition which is perhaps related to conformation .Factors such as faulty conformation, improper trimming and shoeing.
Exercise on hard surfaces are thought to aggravate the condition.
Pathogenesis:-
Many hypotheses regarding the pathogenesis of navicular disease have been proposed.Bursitis Theory. This common theory suggests that concussion between the flexor tendon and navicular bone can cause bursitis, which in turn, leads to hyperemia an d rarification of the bone and alteration of the flexor surface of the bone.
Thrombosis and Ischemia. Thrombosis of the digital arteries results in ischemic necrosis of the bone. In response to this there is an increased number of arteriolar anastomoses and the number of arterioles in the distal nutrient foramina of the navicular bone.
Bone Remodeling. It is represented as a high rate of bone turnover, as a consequence of increased activation of bone remodeling caused by altered pressure from the deep digital flexor tendon on the bone and increased load on its palmar aspect. Histologically, there is increased osteoblasts, osteoclasts, and osteoid formation.
Clinical Sings:_
The affected horse often has a history of intermittent lameness that decreased when it is rested.The lameness of the horse may be noticeably worse the morning after heavy work.
In the early stages of the disease, rest will reduce produce remission of the clinical sings, suggesting that the horse is cured, but as soon as hard work is begun, sings of the disease reappear.
Both forefeet are usually involved in navicular disease, however, one foot often shows more lameness than the other.
If both feet are painful, the horse often points alternately with one foot and then the other, or stands with both feet too far in front.
During movement, the horse tends to land on the toe of the foot to avoid concussion to the heel region
Arthritis of the distal interphalangeal (coffin) joint may be caused by changes in the navicular bone that extend to the articular surface of the joint.
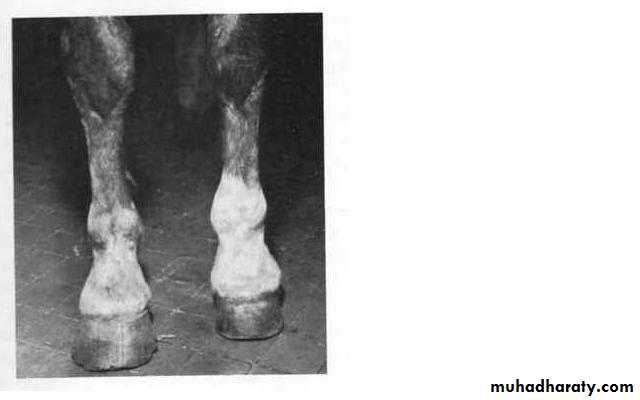
Over a period of time, the foot gradually changes shape. The sole becomes more concave and the foot narrows across the quarters. If the navicular disease is unilateral, the foot will become smaller due to contraction.
Contracted left foot resulting from chronic navicular disease.
Contracted left foot resulting from chronic navicular disease.
Treatment:-
Rest and the administration of nonsteroidal anti-inflammatory drugs is logical in the early acute phase of the disease.
Stall confinement from 5-10 days. Prolonged stall confinement may make horses appear comfortable.
Corrective trimming and shoeing is particularly important for horses that must continue to work and for those that have imbalanced feet.
The periodic administration of nonsteroidal anti-inflammatory drugs such as phenylbutazone, meclofenamic acid, naproxen, or flunixin meglumine also provides some relief to the lameness.
An alternative treatment is anticoagulant therapy. Dicumerol(warfarin sodium) can be administered per os daily at 0.018mg/kg body weight.
Recently a peripheral vasodilating agent, isoxsuprine hydrochloride has shown a benefit as a medical treatment for navicular disease.
Surgical treatment:-
Cryogesia:-Cryogesia of the palmer digital nerves by using cryio surgery blunt probe applied with pressure against the skin at the base of the base of the sesamoid bone where the palmar digital nerve is located, the application period is from 2 seconds to 2 minutes is required.
Palmar Digital Neurectomy:-
Inject the palmer digital nerve at the level of the proximal sesamoid bone for the neurectomy. This will block both the dorsal and palmer digital nerves. Incise the skin and subcutaneous tissues, then the nerve slightly stretched and incise it by clean cut. Post operative administration of NSAD is helpful in preventing inflammation at the surgical site, and wait at least 6 weeks before returning the horse to active use.Penetrating Wounds of the Foot:-
Puncture wounds of the foot are quite common in horses. A variety of objects may produce the wounds. Some puncture wounds are extremely difficult to find, especially if they occur in the frog and the foreign body is missing. Puncture wounds in the middle third of the frog are most serious because of the possibility of puncture of the navicular bursa. Puncture wounds of the sole may cause osteitis, fracture, and necrosis of the distal phalanx or of the digital cushion. Puncture wounds in the white line often cause infection that migrates proximad to break out the coronet band.Clinical Sings:-
In some cases the foreign body will still be in the foot, making the diagnosis relatively simple.
The attitude of the gait of the horse often is very helpful in determining the location of the puncture wound. If the wound is in the toe region, the horse tends to land too heavily on the heel. If the puncture is in the heel, the horse attempts to land on the toe. If the wound is in the medial side of the sole, the horse attempts to put most of his weight on the lateral side of the foot. If the wound is on the lateral side of the sole, the horse attempts to carry most of his weight on the medial side of the foot.
Cracks in the white line, nail punctures, and shoenail punctures can be identified as black spots in the sole. These black spots should be propped until their depth is determined.
Lameness may not be evident until after infection has caused a pododermatitis.
It is not uncommon to find that puncture wounds of the foot cause distention of the flexor tendon sheath just above the fetlock joint.
Some cases of puncture wound in the foot will cause septicemia and phlegmon of the limb with elevation of temperature and sever systemic manifestations.
Puncture wounds of the hind foot may cause a stringhalt attitude to the gait. The horse will move the limb in a hyperflexed manner.
Diagnosis:-
A hoof tester is essential for diagnosis of puncture wounds.Radiographs should be taken to determine damage of any bony structures.
Puncture wounds of the frog are the most difficult to locate, because once the foreign body has been pulled out, the spongy frog closes over the wound making it difficult to fined.
Oftentimes it is helpful to introduce a sterile probe into the tract to assess its depths and to determine whether vital structures have been penetrated.
Contrast radiographic studies of the draining tract may also be helpful. Contrast material can be injected through a needle, teat cannula, or a small diameter Foley catheter.
Also infection of the coffin joint can result from extension of infection in the navicular bursa. Arthrocentesis of the coffin joint will confirm the diagnosis.
Treatment:-
Generally to treat a puncture wound, you should establish drainage of the lesion, keep the region clean and protected until healing occurs, and prevent tetanus.
Steps of the treatment can be summarized in the following points:-
The entire sole, frog, and sulcus should be cleaned and washed.
The area of the puncture wound should be drained.
If the wound is in the frog, the tract should be trimmed away until adequate drainage is established.
Following drainage, the wound should be cleaned with an antiseptic solution.
The opening of the wound should be packed with povidine iodine, and the foot bandaged thoroughly.
The foot should be bandaged to protect it from moisture and filth, and the horse should be kept stalled, if possible, or at least in as dry area as possible.
A especial boot can be used in place of the bandaging.
Tetanus antitoxin should administered.
When the infection causes drainage from a sinus at the coronary band, it is advisable to soak the foot daily in a magnesium sulfate antiseptic solution.
It is beneficial to flush the tract from the coronary band with a 1% povidone iodine solution.
If the puncture wound penetrates the navicular bursa, the bursa may require drainage through the center third of the frog.
Occasionally the distal interphalangeal(coffin) joint will become involved that requires immediate treatment. Arthrocentesis of the coffin joint will be performed. The aspirate should be submitted for cytological examination and Gram stain, also culture and sensitivity tests should be conducted.