NEUROGENIC BLADDER
Description of NB
Dysfunction of the urinary bladder due to disease of the central nervous system or peripheral nerves involved in the control of micturition.Epidemiology
Prevalence of voiding dysfunction (VD) is reported for specific conditions:Cerebrovascular accident: 20-50%
Parkinson disease: 35-70%
Multiple sclerosis: 50-90%
Diabetes mellitus: 5-60%
Risk factors
Neurologic disease, injury, or congenital malformation
DM
Radical pelvic surgery
Genetics
Genetic diseases that may be associated with NB include:Muscular dystophy
Hereditary spastic paraplegia
Neurofibromatosis
Familial dysautonomia
General prevention
Prevention aimed at preventing secondary complications:Infections
Incontinence
Skin breakdown
Urolithiasis
Classification of Neurogenic Bladder
• Hyperreflexic bladder.• Hyporeflexic (atonic) bladder.
• DSD
• Supraspinal lesion.
• Spinal (suprasacral or infrasacral) lesion.
• Peripheral nerves.
• 1-Motor lesion:
• A- upper MNL.
• B- lower MNL.
• C- mixed lesion.
• 2- Sensory lesion.
• Failure to Store:
• Because of the bladder.
• Because of the outlet.
• Failure to Empty:
• Because of the bladder.
• Because of the outlet.
Classification of Neurogenic Bladder
Most often done using urodynamic classification scheme:
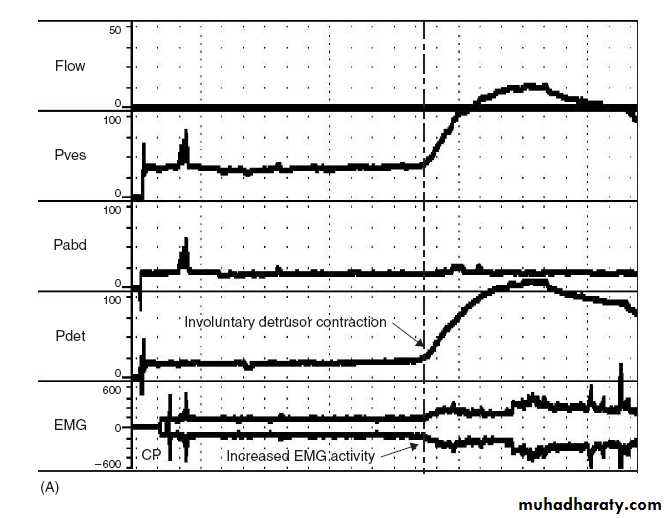
• Neurogenic DO (hyperreflexia): uncontrolled reflex bladder contraction
• Detrusor underactivity (areflexia):
• DSD: abnormal reflexive sphincter contraction during involuntary detrusor contraction
Functional BOO, elevated intravesical pressure
Secvondary damage: pressure, infection, urolithiasis
Pathophysiology
Voiding center include:Higher centers (suprapontine):
Function: inhibit sacral micturition center
Predicted type of VD with suprapontine lesion would be detrusor overactivity (DO) due to loss of inhibition on sacral micturition center
Pontine micturition center (PMC):
Function: coordinates sphincter relaxation during bladder contraction
Predicted type of VD with lesion between pontine and sacral micturition center is DO and detrusor-sphinecter dyssynergia (DSD)
Pathophysiology
Sacral micturition center (SMC):Function: mediates reflex and voluntary bladder contraction
Predicted type of VD with lesion of SMC is detrusor underactivity or areflexia
Peripheral lesions: VD is variable including:
Detrusor underactivity
Impaired bladder sensation
Impaired sphincteric function
Pathophysiology
Upper motor neuron lesion: spastic, uninhibited: injury above spinal cord micturition center
Lower motor neuron lesion: flaccid, atonic, areflexic: injury in the pelvic nerves or spinal micturition center
Spinal shock:
Immediately after injury, regardless of the level, there is a stage of flaccid paralysis with numbness below the level of the injury that lead to bladder overfilling to the point of overflow incontinence & rectal impaction.
It lasts few weeks up to 6 months
Pathophysiology
Autonomic dysreflexia (AD):A potentially life threatening condition that can cause rapid, extreme BP elevation, headache, diaphoresis, bradycardia, sweating, nausea and piloerection in patients with spinal cord lesions at and above the 6th thoracic vertebral level (T6).
Causes: noxious stimulus below the level of injury such as: bladder distention, bowel distention, or pain activate sympathetic neurons causing unopposed reflex sympathetic activity
Commonly associated conditions
Neural tube defects (NTD)CNS diseases:
CVA
SCI
TM
MS
PD
Normal-pressure hydrocephalus
Static disorders of development: as CP
PNS disease:
Radical pelvic surgery:
AP resection
radical hysterectomy
DM
IDP
Spinal stenosis
GB syndrome
Diagnosis
History:Voiding symptoms:
Irritative or obstructiveUI: urge, stress
Spastic Neuropathic Bladder:
• The severity of symptoms depends on the site and extent of the lesion as well as the length of time from injury.
• OAB syndrome: urinary urgency with or without UUI, usually associated with frequency and nocturia
Flaccid (Atonic) Bladder:
• principal urinary symptom is urine retention with overflow incontinence. Male patients lose their erections.
• Extremity reflexes are hypoactive or absent. Sensation is diminished or absent
History of any risk factor:
neurologic disease: onset, duration
DM
Congenital disorders:
NTD
CP
Method of urinary management:
Volitional or reflex voiding
Condom catheter urinary collection
CISC
Indwelling urethral or suprapubic catheter
Crede, Valsalva voiding
UTI:
Severity of infection: febrile, hospitalization, IV antibiotics required
Frequency of recurrence
Urolithiasis :
episodes
surgical intervention
calculus composition
AD: SCD above T6
Physical Examination
HTN: renal dysfunction, AD
Generalized edema: severe renal insufficiencyPalpable flank mass: HN
Flank tenderness: ureteral obstruction, pyelonephritis
Abdominal mass: distended bladder, urinary retention
UI: stress maneuvers, Marshall test
Testicular mass: epididymitis/epididymo-orchitis, secondary abscess
prostate: size: BPH may coexist with NB dysfunction
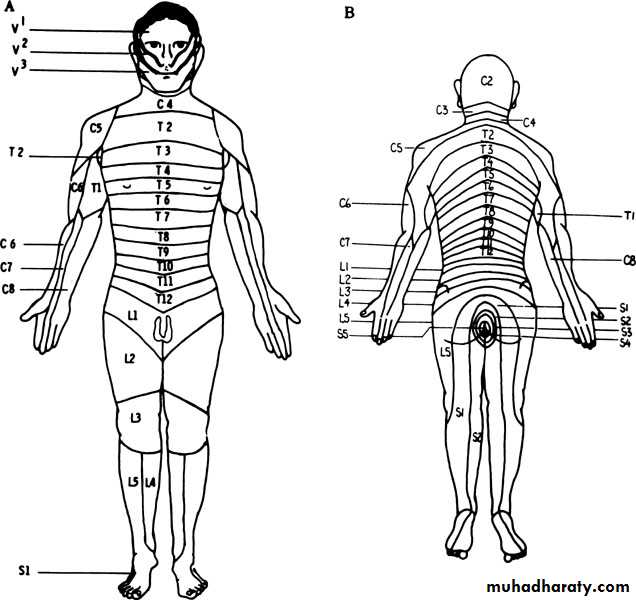
Sacral abnormalities: sacral dimple or tuft of hair, sacral agenesisNeurologic: sacral root, perianal sensation, sensory level, anal tone, sphincter control, bulbocavernosal, knee, ankle, and toe reflexes.
Diagnostic tests
Blood studies:Serum chemistry: RFT
CBC: elevated WBC, secondary anaemia due to ↓ renal function or chronic infection
Urinalysis:
Proteinuria: renal dysfunction
pyuria, nitrite, leukocyte esterase: acute or chronic infection
Hematuria: infection or lithiasis
Imaging
Imaging is most important in pts with risk factors for upper tract compromise:
DSD: particularly males who void reflexively
Impaired bladder compliance
Renal US: to screen for calculus, HN, or mass
KUB: radio-opaque calculi
Excretory urography:
Delayed excretion of contrast with high urinary-storage pressures
HUN: marked elevation of intravesical pressure (ie, NDO/DSD) or calculi
VCUG: for VUR, urethral abnormaity
Nuclear medicine renal scan:
Sequential studies detect deterioration of renal function
MRI: bladder neck and posterior urethra
Diagnostic procedures
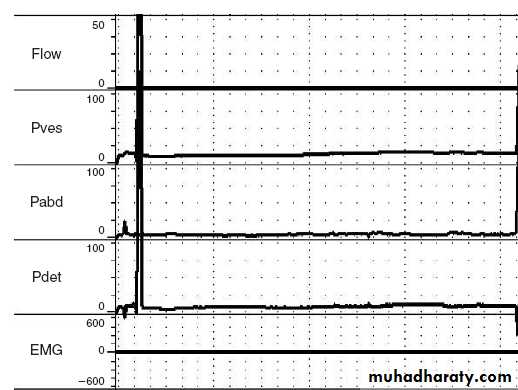
Cystourethroscopy: degree of trabeculation, diverticuli, bladder capacity, stone, ureteral orifice competency, integrety of BN and external sphincter, Cx of chronic catheterization and infectionUrodynamics: Technique used to obtain graphic recording of activity in UB, urethral sphincters ,
& pelvic musculature
Components include:
• Uroflowmetry.
• Cystometry.
• Urethral pressure profile.
• EMG.
Necessary to determine effective urologic management for all pts with neurogenic lower urinary tract dysfunction
Differential Diagnosis
• Cystitis.• Chronic urethritis.
• Vesical irritation secondary to stone.
• Interstitial cystitis.
• Cystocele.
• Infravesical obstruction (LUTS).
Treatment
UDS are essential to detrmine lower urinary tract function/dysfunction and to plan urologic MxControl intravesical pressure and empty the bladder effectively: in order to protects upper tracts, preserve renal function, continence, & control infection
Spontaneous voiding with continence is possible with NDO controlled medically
Voiding by trigger technique: tapping the abdomen suprapubically, tugging on the pubic hair, squeezing the penis, or scratching the skin of the lower abdomen, genitalia, or thighs.
Urinary darinage: SCIC or external collection appliance (condom)
SCIC: most effective Rx; requires low storage pressure
Indwelling cath: avoid due to Cx (UTI, erosion, calcui, etc)
Treatment of spinal shock
Bladder drainage: must be instituted immediately and maintained:by clean self intermittent catheterisation(CSIC), indwelling catheter or suprapubic cystostomy
Increase fluid intake to 2 – 3 L/day
Prophylaxis for calculus formation by reducing calcium & oxalate intake & decrease vit D from diet
Spastic neuropathic bladder
Medication:
First line:
Anticholinergics: to improve urinary storage pressure/↓ involuntary contraction:
Oxybutynin
Hypscyamine
Tolterodine
ᾳ1-adrenergic blockers:↓internal sphincter resistance, lower voiding pressure; ineffective for DSD, may control symptoms of AD:
Doxazosin
Terazosin
tamsulosin
Spastic neuropathic bladder
Medication:Second line:
Botulinum toxin:
Injection into external sphincter for DSD:
short-lived
requires repeated inj.
Inj. Into detrusor muscle for DO:
Duration of action is 3-9 mon
requires repeated inj.
Vanilloid agents instillation: capsaicin and resiniferatoxin:
Suppress uninhibited involuntary detrusor contraction
Spastic neuropathic bladder
Surgery
Endoscopic sphincter ablation or stenting
Only males with DSD
Requires condom catheter
Augmentation cystoplasty: using intestinal segment to enlarge the badder:
Intermittent cath for urine drainage
Cystectomy with continent urinary reservoir and catheterizable stoma:
For pts with limited dexterity specially in females
Ileal or colon pouch
Continent cathetrizable stoma (appendix or terminal ileum)
Ileovesicostomy (bladder chimney): for those unable to perform CSIC (quadriplegia)
Cystectomy with ileal conduit
Sacral rhizotomy at S3-4: Conversion of the spastic bladder to a flaccid bladder
Sacral neuromodulation (bladder pacemaker): of the sacral nerve roots to accomplish bladder evacuation in selected cases
Flaccid neuropathic bladder
Crede maneuver (manual suprapubic pressure) accompanied by strainingBladder training & care , voiding every 2hr
CSIC every 3-6 hr
Parasympathomimetic drugs like bethanecol chloride ( Urecholine), 5 – 50 mg every 6-8hr
Surgery:
TURP in hypertrophied bladder neck or BPH
Implanting an artificial sphincter.
Complications
Recurrent UTI:
cystitis, periurethritis, prostatitis, epididymoorchitis, pyelonephritis
Calculus formation
Urinary retention
HUN
Renal impairment and amyloidosis
Neoplastic transformation: associated with chronic catheter
Urethral erosion
Sexual dysfunction
AD
Mx of AD
Acute management: removal of triggering stimulus by bladder drainage or rectal decompressionChronic treatment:
ᾳ-blockers
calcium channel blocker
Botulinum toxin injection
Prophylaxis before cystoscopy:
Oral nifedipine (20mg), 30 min before cystoscopy as prophylaxis
Prognosis
Proper urologic Mx greatly improves QoL in pts with NB dysfunction
Follow up
Annual evaluation in high risk pts may include:• UDS
• imaging: typically renal US
• Serum creatinine