
1
Fifth stage
Medicine
Lec-1
د.عبد هللا
26/3/2017
Stroke
The main arterial supply of the brain comes from the internal carotid
arteries, which supply the anterior brain, and the vertebral and basilar
arteries (vertebrobasilarsystem), which provide the posterior circulation.
The anterior and middle cerebral arteries supply the frontal and parietal
lobes, while the posterior cerebral artery supplies the occipital lobe.
The vertebral and basilar arteries perfuse the brain stem, mid-brain and
cerebellum.
Communicating arteries provide connections between the anterior and
posterior circulations and between left and right hemispheres, creating
protective anastomotic connections that form the circle of Willis.

2
In health, regulatory mechanisms maintain a constant cerebral blood flow
across a wide range of arterial blood pressures to meet the high resting
metabolic activity of brain tissue; cerebral blood vessels dilate when
systemic blood pressure is lowered and constrict when it is raised , This
autoregulatory mechanism can be disrupted after stroke
Definition:
Cerebrovascular disease is the third most common cause of death in the
developed world after cancer and ischaemic heart disease, and is the most
common cause of severe physical disability.
Cerebrovascular diseases include: ischemic stroke, hemorrhagic stroke,
and cerebrovascular anomalies such as (intracranial aneurysms and
arteriovenous malformations (AVMs)).
The incidence of cerebrovascular diseases increases with age.
It is define by its abrupt onset of a neurologic deficit that is attributable
to a focal vascular cause ,most commonly( a hemiplegia with or without
signs of focal higher cerebral dysfunction (such as aphasia), hemisensory
loss, visual field defect or brain-stem deficit)
Cerebral ischemia is caused by a reduction in blood flow that lasts longer
than several seconds.
Neurologic symptoms are manifest within seconds because neurons lack
glycogen, so energy failure is rapid.
If the cessation of flow lasts for more than a few minutes, infarction or
death of brain tissue results; When blood flow is quickly restored, brain
tissue can recover fully and the patient’s symptoms are only transient:
This is called a transient ischemic attack (TIA).

3
TIA requires that all neurologic signs and symptoms resolve within 24 ;
stroke has occurred if the neurologic signs and symptoms last for >24 h.
generalized reduction in cerebral blood flow due to systemic hypotension
(e.g., cardiac arrhythmia, myocardial infarction, or hemorrhagic shock)
usually produces syncope ;If low cerebral blood flow persists for a longer
duration, then infarction in the border zones between the major cerebral
artery distributions may develop ;In more severe instances, global
hypoxia-ischemia causes widespread brain injury is called hypoxic-
ischemic encephalopathy .
Focal ischemia or infarction, is usually caused by thrombosis of the
cerebral vessels themselves or by emboli from a proximal arterial source
or the heart.
Intracranial hemorrhage is caused by bleeding directly into or around the
brain; it produces neurologic symptoms by producing a mass effect on
neural structures, from the toxic effects of blood itself, or by increasing
intracranial pressure.
Progressing stroke (or stroke in evolution): This describes a stroke in which
the focal neurological deficit worsens after the patient first presents. may be
due to increasing volume of infarction, haemorrhagic transformation or
increasing oedema.
Completed stroke: This describes a stroke in which the focal deficit persists
and is not progressing.

4
Pathophysiology:
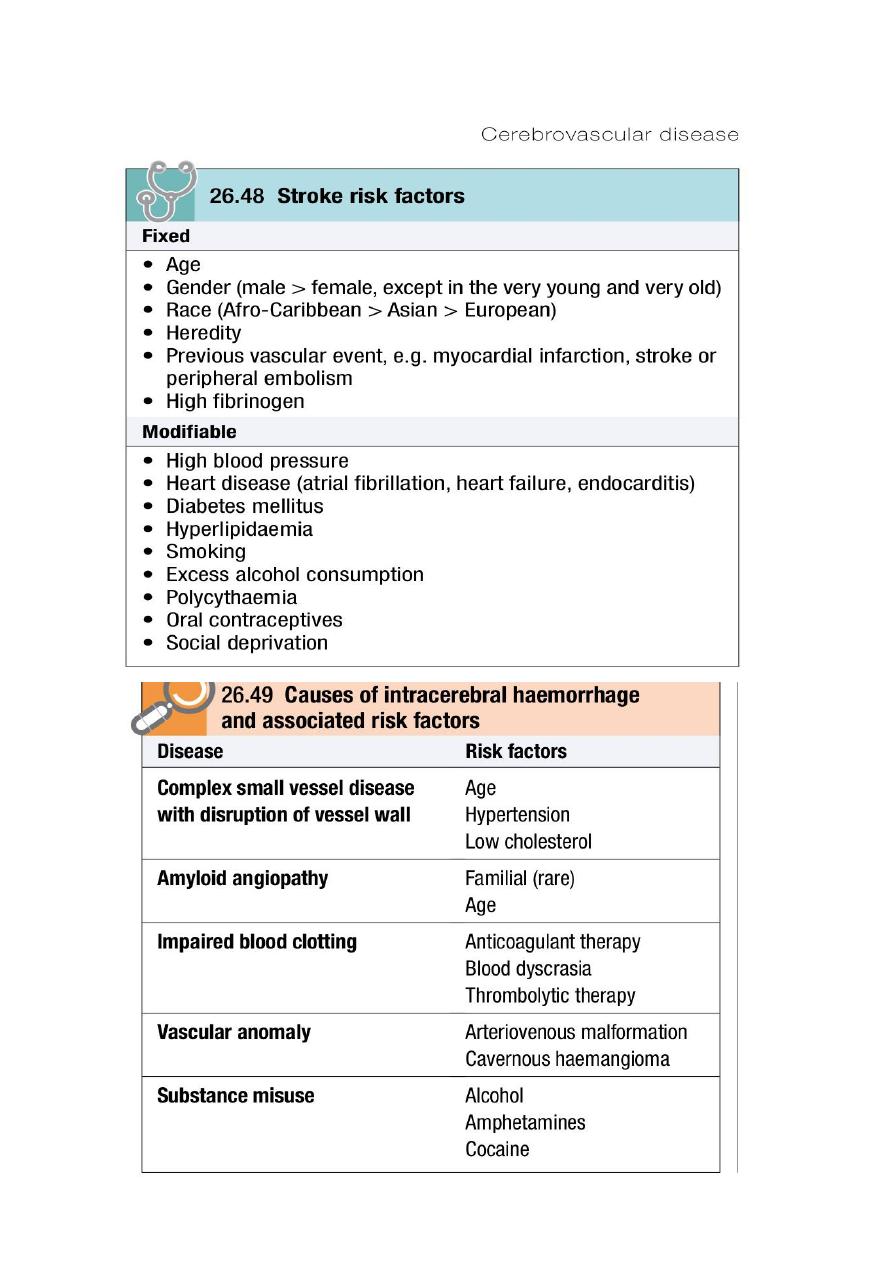
Of patients with a stroke, 85% will have a cerebral infarction and the
remainder will have had an intracerebral haemorrhage.
Brain imaging is required to distinguish these pathologies and to guide
management.
The combination of severe headache and vomiting at the onset of the
focal neurological deficits increases the likelihood of a haemorrhagic
stroke.
Cerebral infarction
is mostly due to thromboembolic disease secondary to atherosclerosis in
the major extracranial arteries (carotid artery and aortic arch).
About 20% of infarctions are due to embolism from the heart, and a
further 20% are due to intrinsic disease of small perforating vessels
(lenticulostriate arteries), producing so-called ‘lacunar’ infarctions.
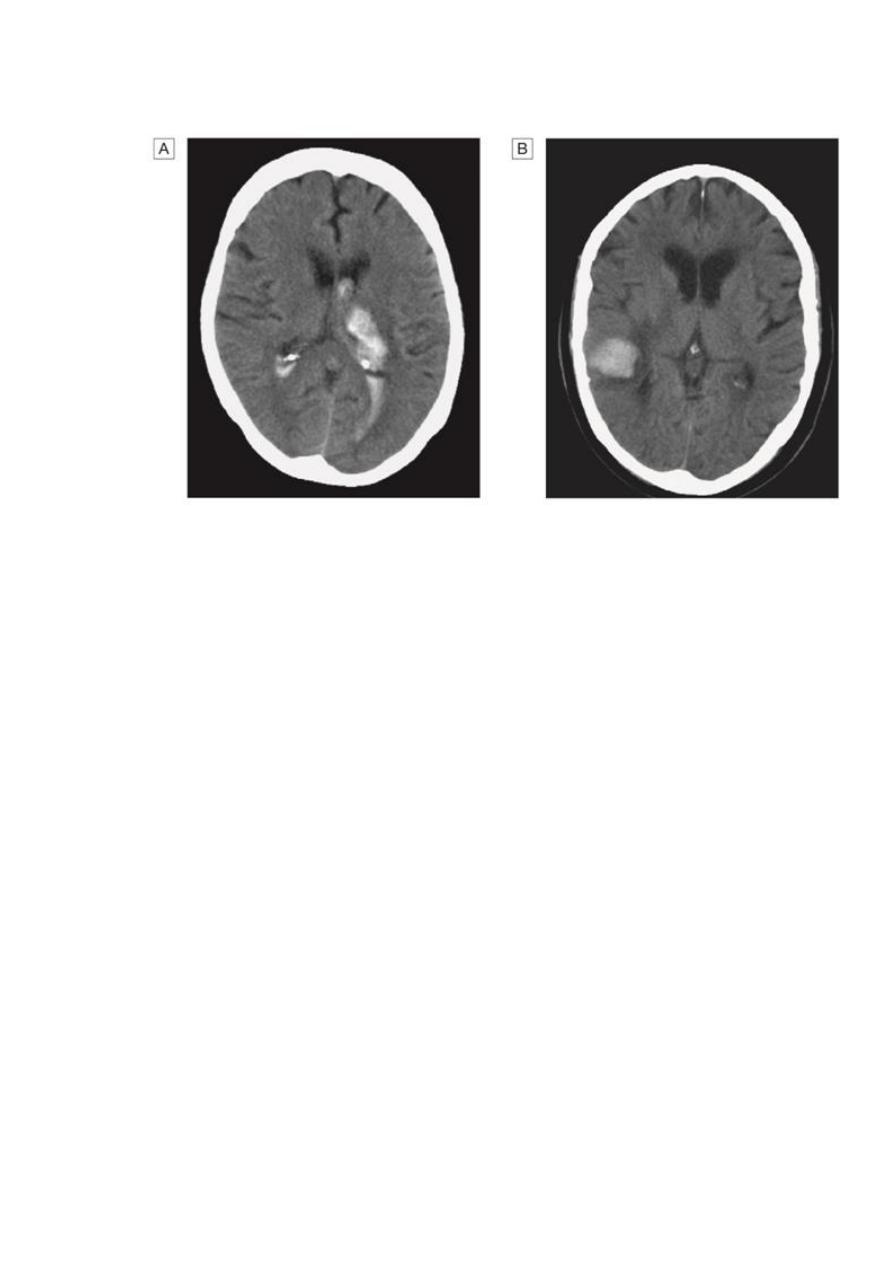
Intracerebral hemorrhage
This usually results from rupture of a blood vessel within the brain
parenchyma but may also occur in a patient with a subarachnoid
hemorrhage if the artery ruptures into the subarachnoid space.
Hemorrhage frequently occurs into an area of brain infarction.
The haemorrhage itself may expand over the first minutes or hours, or it
may be associated with a rim of cerebral oedema, which, along with the
haematoma, acts like a mass lesion to cause progression of the
neurological deficit. If big enough, this can cause shift of the intracranial
contents, producing transtentorial coning and sometimes rapid death.
If the patient survives, the haematoma is gradually absorbed, leaving a
haemosiderinlined slit in the brain parenchyma.
5

6
Clinical features
:
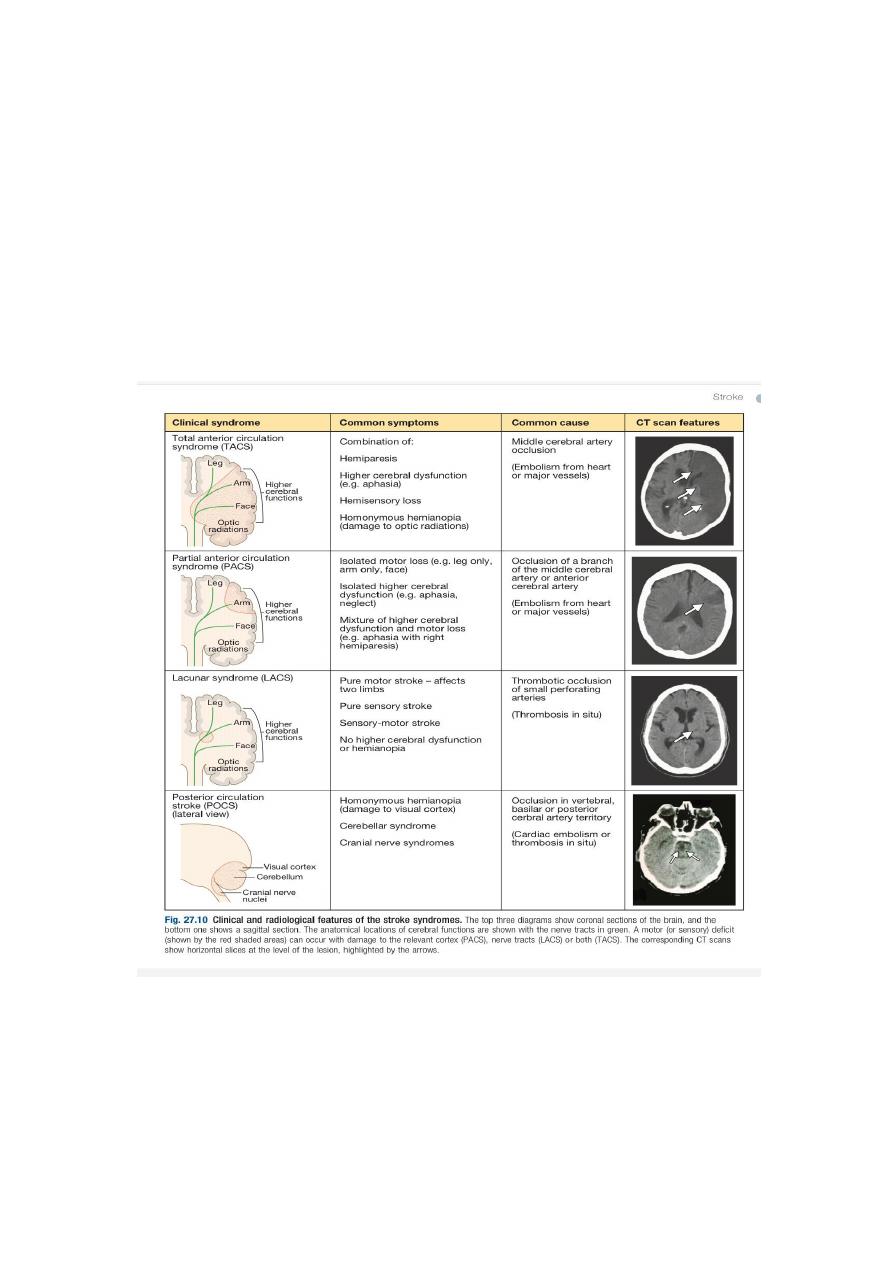
The clinical presentation of stroke depends upon which arterial territory is
involved and the size of the lesion.
The presence of a unilateral motor deficit, a higher cerebral function
deficit such as aphasia or neglect, or a visual field defect usually places the
lesion in the cerebral hemisphere.
Ataxia, diplopia, vertigo and/or bilateral weakness usually indicate a
lesion in the brain stem or cerebellum.
Reduced conscious level usually indicates a large volume lesion in the
cerebral hemisphere but may result from a lesion in the brain stem or
complications such as obstructive hydrocephalus, hypoxia or severe
systemic infection.
Clinical assessment of the patient with a stroke should also include a
general examination since this may provide clues to the cause of the
stroke, and identify important comorbidities and complications of the
stroke.

7
Investigations:
aims to confirm the vascular nature of the lesion, distinguish cerebral
infarction from haemorrhage and identify the underlying vascular disease
and risk factors
Initial investigation of all patients with stroke includes a range of simple
blood tests to detect common vascular risk factors and markers of rarer
causes, an electrocardiogram (ECG) and brain imaging. Where there is
uncertainty about the nature of the stroke, further investigations are
usually indicated
Neuroimaging :
Brain imaging with either CT or MRI should be performed in all patients
with acute stroke.
CT is the most practical and widely available method of imaging the brain.
It will usually exclude non- stroke lesions, including subdural haematomas
and brain tumours, and will demonstrate intracerebral haemorrhage
within minutes of stroke onset However, especially within the first few
hours after symptom onset, CT changes in cerebral infarction may be
completely absent or only very subtle.
MRI diffusion weighted imaging (DWI) can detect ischaemia earlier than
CT.
MRI is more sensitive than CT in detecting strokes affecting the brain stem
and cerebellum.
CT and MRI may reveal clues as to the nature of the arterial lesion. For
example, there may be a small, deep lacunar infarct indicating small-
vessel disease, or a more peripheral infarct suggesting an extracranial
source of embolism.
In a haemorrhagic lesion, the location might indicate the presence of an
underlying vascular malformation, saccular aneurysm or amyloid
angiopathy

8
Cardiac investigations:
Approximately 20% of ischaemic strokes are due to embolism from the
heart. The most common causes are atrial fibrillation, prosthetic heart
valves, other valvular abnormalities and recent myocardial infarction.
These can often be identified by clinical examination and ECG.
A transthoracic or transoesophageal echocardiogram can be useful, either
to confirm the presence of cardiac source or to identify an unsuspected
source such as endocarditis, atrial myxoma, intracardiac thrombus or
patent foramen ovale. Such findings may lead on to specific treatment .
Vascular imaging:
Many ischaemic strokes are caused by atherosclerotic thromboembolic
disease of the major extracranial vessels(arterial to arterial emboli).
Detection of extracranial vascular disease can help establish why the
patient has had an ischaemic stroke and may lead to specific treatments
including carotid endarterectomy to reduce the risk of further stroke.
Extracranial arterial disease can be non-invasively identified with duplex
ultra sound, MR angiography (MRA) or CT angiography.
Management:
is aimed at minimizing the volume of brain that is irreversibly damaged,
preventing complications
reducing the patient’s disability and handicap through rehabilitation,
and reducing the risk of recurrent episodes
9
The patient’s neurological deficits may worsen during the first few hours
or days after their onset. This is may be due to extension of the area of
infarction, hemorrhage into it, or the development of oedema with
consequent mass effect.
It is important to distinguish such patients from those who are
deterioratin as a result of complications such as hypoxia, sepsis, epileptic
seizures or metabolic abnormalities which can be easily reversed .
11
Management of acute stroke
:
Airway
Perform bedside swallow screen and keep patient nil by mouth if
swallowing unsafe or aspiration occurs.
Breathing
Check respiratory rate and oxygen saturation and give oxygen if
saturation < 95%.
Circulation
Check peripheral perfusion, pulse and blood pressure and treat
abnormalities with fluid replacement, antiarrhythmics and inotropic drugs
as appropriate.
Hydration
If signs of dehydration, give fluids parenterally or by nasogastric tube

11
Nutrition.
Assess nutritional status and provide nutritional supplements if necessary
If dysphagia persists for > 48 hrs, start feeding via a nasogastric tube.
Blood pressure
• Unless there is heart or renal failure, evidence of hypertensive
encephalopathy or aortic dissection, do not lower blood pressure in first
week as it may reduce cerebral perfusion. Blood pressure often returns
towards patient’s normal level within first few days.
Blood glucose
• Check blood glucose and treat when levels are ≥ 11.1 mmol/L (200
mg/dL)
• Monitor closely to avoid hypoglycemia.
Temperature
• If pyrexic, investigate and treat underlying cause
• Control with antipyretics, as raised brain temperature may increase
infarct volume
Incontinence
Check for constipation and urinary retention; treat appropriately
Avoid urinary catheterisation unless patient is in acute urinary retention or
incontinence is threatening pressure areas

12
treatments in acute stroke:
Thrombolysis:
Intravenous thrombolysis with recombinant tissue plasminogen
activator (rt-PA) increases the risk of haemorrhagic transformation
of the cerebral infarct with potentially fatal results. However, if it is
given within 4.5 hours of symptom onset to carefully selected
patients, the haemorrhagic risk is offset by an improvement in
overall outcome
The earlier treatment is given, the greater the benefit.
Aspirin:
In the absence of contraindications, aspirin (300 mg daily) should be
started immediately after an ischaemic stroke unless rt-PA has been
given, in which case it should be withheld for at least 24 hours.
Aspirin reduces the risk of early recurrence and has a small but
clinically worthwhile effect on long-term outcome
it may be given by rectal suppository or by nasogastric tube in
dysphagic patients.
Heparin:
routine use of heparin does not result in better long-term out-
comes, and therefore it should not be used in the routine
management of acute stroke.
heparin might provide benefit in selected patients, such as those
with recent myocardial infarction, arterial dissection or progressing
strokes. Intracranial haemorrhage must be excluded on brain
imaging before considering anticoagulation.

13
Coagulation abnormalities:
In those with intracerebral haemorrhage, coagulation abnormalities
should be reversed as quickly as possible to reduce the likelihood of
the haematoma enlarging. This most commonly arises in those on
warfarin therapy.
Management of risk factors:
Patients with ischaemic events should be put on long- term
antiplatelet drugs and statins to lower cholesterol.
For patients in atrial fibrillation, the risk can be reduced by about
60% by using oral anticoagulation to achieve an INR of 2–3.
The risk of recurrence after both ischaemic and haemorrhagic
strokes can be reduced by blood pressure reduction, even for those
with relatively normal blood pressures
Carotid endarterectomy and angioplasty:
Surgery is most effective in patients with more severe stenoses (70–
99%) and in those in whom it is performed within the first couple of
weeks after the TIA or ischaemic stroke.
Patients with cerebellar haematomas or infarcts with mass effect
may develop obstructive hydrocephalus and some will benefit from
insertion of a ventricu- lar drain and/or decompressive surgery.
Some patients with large haematomas or infarction with massive
oedema in the cerebral hemispheres may benefit from anti-oedema
agents, such as mannitol or artificial ventilation, and surgical
decompression to reduce intracranial pressure should be
considered in appropriate patients.

14
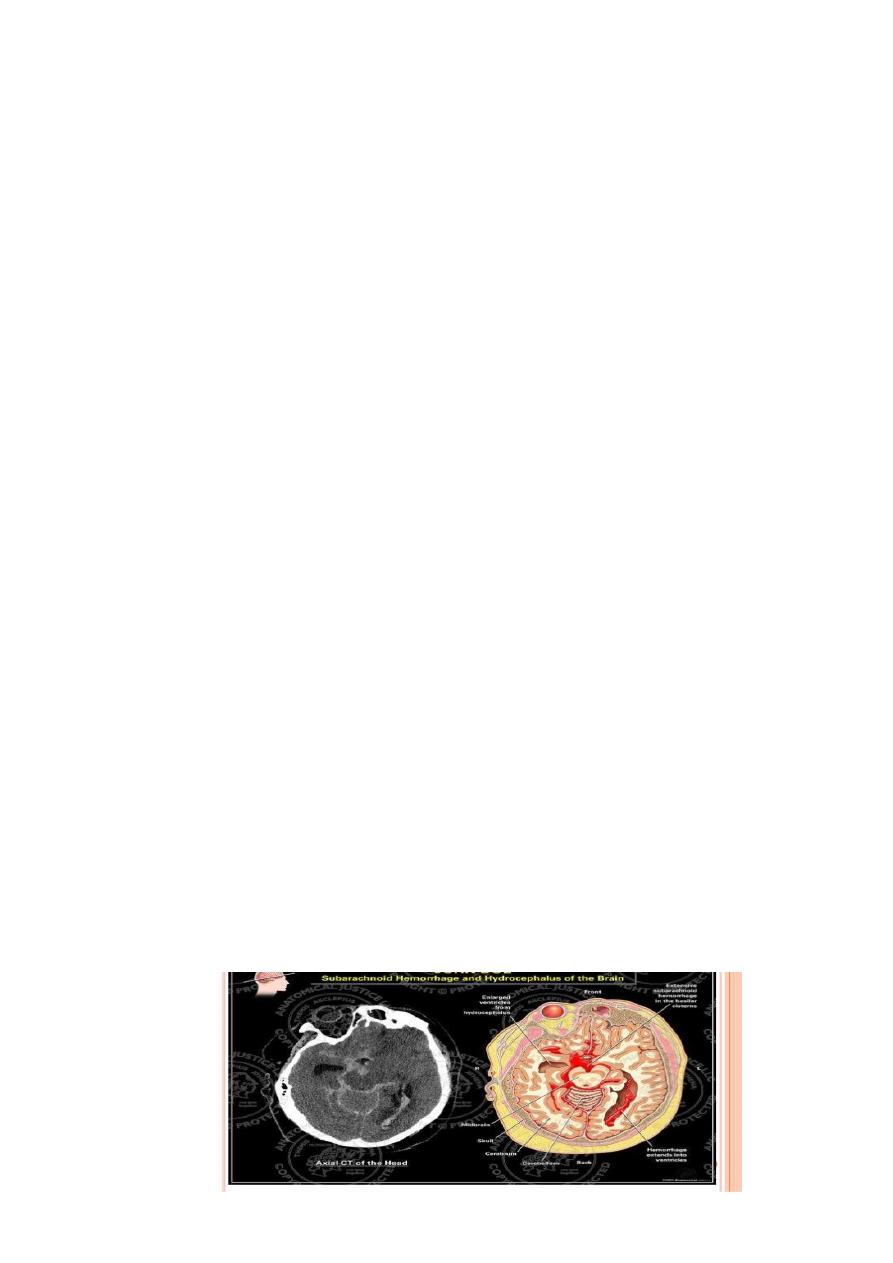
SUBARACHNOID HAEMORRHAGE :
Subarachnoid haemorrhage (SAH) is less common than ischaemic
stroke or intracerebral haemorrhage.
Women are affected more commonly than men and the condition
usually presents before the age of 65.
The immediate mortality of aneurysmal SAH is about 30%; survivors
have a recurrence (or rebleed) rate of about 40% in the first 4
weeks and 3% annually thereafter.
85% of SAH are caused by saccular or ‘berry’ aneurysms arising from
the bifurcation of cerebral arteries , particularly in the region of the
circle of Willis.
There is an increased risk in first-degree relatives of those with
saccular aneurysms, and in patients with polycystic kidney disease
and congenital connective tissue defects such as Ehlers– Danlos
syndrome.
In about 10% of cases, SAH are non-aneurysmal haemorrhages (so-
called peri- mesencephalic haemorrhages).
Five percent of SAH are due to arteriovenous malformations and
vertebral artery dissection.
15
Clinical features:
SAH typically presents with a sudden, severe, ‘thunderclap’
headache (often occipital), which lasts for hours or even days, often
accompanied by vomiting, raised blood pressure and neck stiffness
or pain. It commonly occurs on physical exertion, straining and
sexual excitement
There may be loss of consciousness at the onset, so SAH should be
considered if a patient is found comatose.
On examination, the patient is usually distressed and irritable, with
photophobia. There may be neck stiffness due to subarachnoid
blood but this may take some hours to develop. Focal hemisphere
signs, such as hemiparesis or aphasia, may be present at onset if
there is an associated intracerebral haematoma.
A third nerve palsy may be present due to local pressure from an
aneurysm of the posterior communicating artery, but this is rare.
Investigations;
CT brain scanning and lumbar puncture are required.
The diagnosis of SAH can be made by CT, but a negative result does
not exclude it, since small amounts of blood in the subarachnoid
space cannot be detected by CT.
Lumbar puncture should be performed 12 hours after symptom
onset if possible, to allow detection of xanthochromia , If either of
these tests is posi- tive, cerebral angiography is required to
determine the optimal approach to prevent recurrent bleeding.

16
Management:
Good control of blood pressure < 160 systolic
Good hydration
Strong analgesia
Avoid constipation
Nimodipine (30–60 mg tab for 21 days to prevent delayed
ischaemia in the acute phase.
Insertion of coils into an aneurysm (via an endovascular procedure)
or surgical clipping of the aneurysm neck reduces the risk of both
early and late recurrence.
Arteriovenous malformations can be managed either by surgical
removal, by ligation of the blood vessels that feed or drain the
lesion, or by injection of material to occlude the fistula or draining
veins.
Treatment may also be required for complications of SAH, which
include non obstructive hydrocephalus (that may require drainage
via a shunt),
delayed cerebral ischaemia due to vasospasm (which may be
treated with vasodilators),
hyponatraemia (best managed by fluid restriction) and systemic
complications associated with immobility, such as chest infection
and venous thrombosis.
17
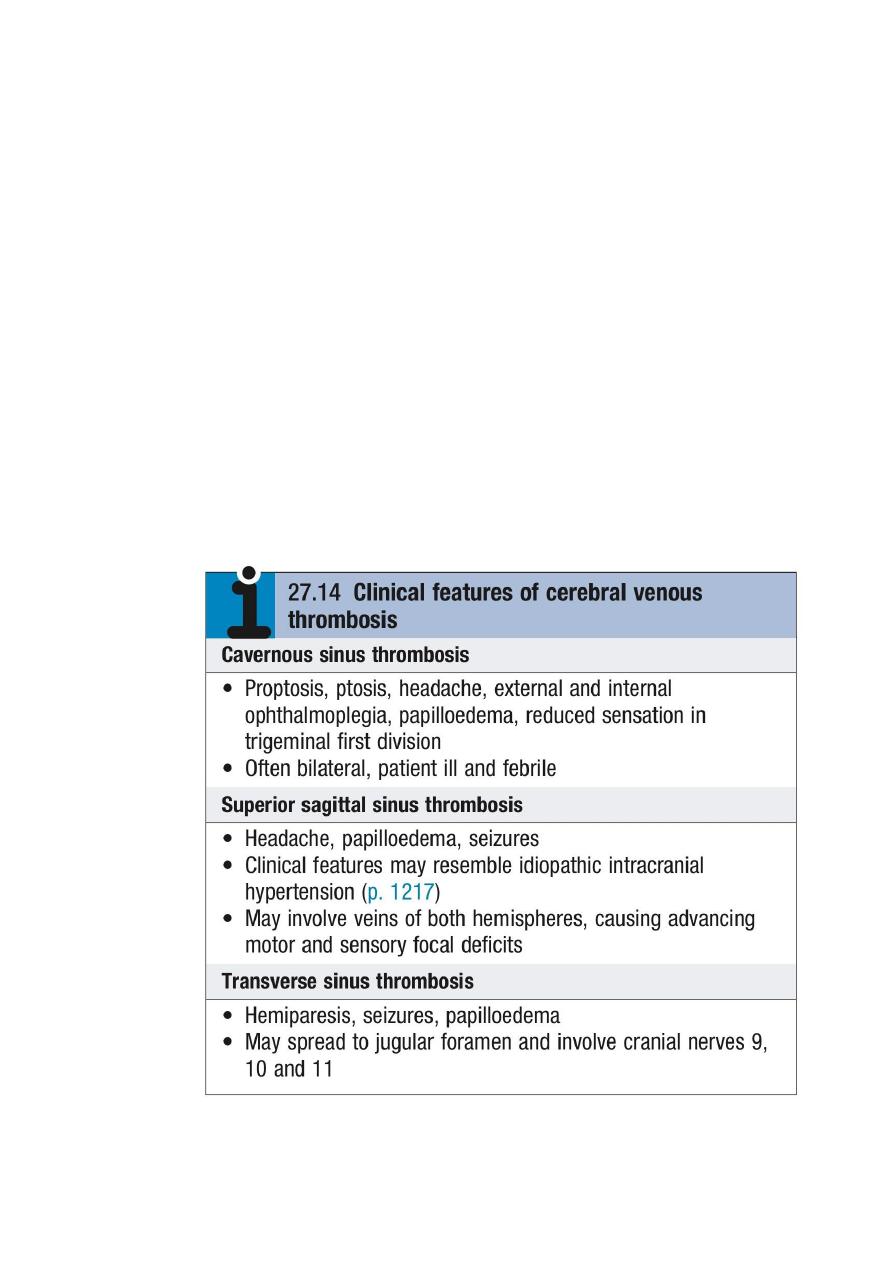
CEREBRAL VENOUS DISEASE:
Thrombosis of the cerebral veins and venous sinuses (cerebral
venous thrombosis) is much less common than arterial thrombosis.
Clinical features
Cerebral venous sinus thrombosis usually presents with symptoms
of raised intracranial pressure, seizures and focal neurological
symptoms.
The clinical features vary according to the sinus involved , Cortical
vein thrombosis presents with focal cortical deficits such as aphasia
and hemiparesis (depending on the area affected), and epilepsy
(focal or generalised).
The deficit can increase if spreading thrombophlebitis occurs.

18
Causes of cerebral venous thrombosis:
Predisposing systemic causes:
• Dehydration
• Thrombophilia
• Pregnancy
• Hypotension
• eh et’s disease
• Oral contraceptive use
Local causes:
• Paranasal sinusitis
• Facial skin infection
• Meningitis, subdural empyema
• Otitis media, mastoiditis
• Skull fracture
• Penetrating head and eye wounds

19
Investigations and management:
MR venography demonstrates a filling defect in the affected vessel.
Anticoagulation, initially with heparin followed by warfarin, is
usually beneficial, even in the presence of venous haemorrhage.
In selected patients, the use of endovascular thrombolysis has been
advocated. Management of underlying causes and complications,
such as persistently raised intracranial pressure, is also important.
About 10% of cerebral venous sinus thrombosis, particularly
cavernous sinus thrombosis, is associated with infection (most
commonly Staphylococcus aureus), which necessitates antibiotic
treatment.
