1
Fifth stage
Medicine
Lec-6
.د
فاخر
22/12/2016
Vasculitis
These are a heterogeneous group of diseases characterized by inflammation and
necrosis of blood-vessel walls, with associated damage to skin, kidney, lung, heart, brain
and gastrointestinal tract. There is a wide spectrum of involvement and disease severity,
ranging from mild and transient disease affecting only the skin, to life-threatening
fulminant disease with multiple organ failure
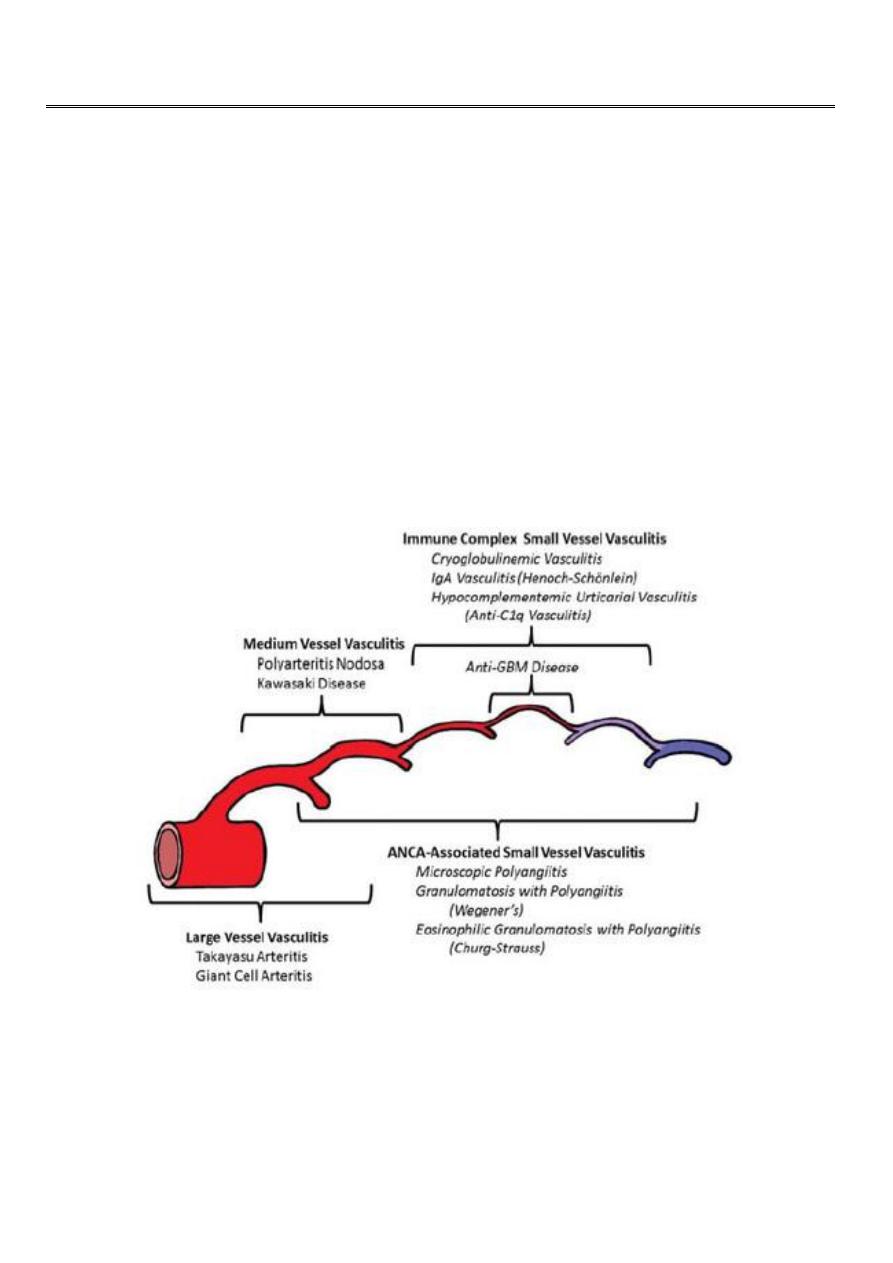
Primary Vasculitis
Classified according to the size of vessel involved into:
1. Large vessel –giant cell arteritis, Takayasu’s arteritis
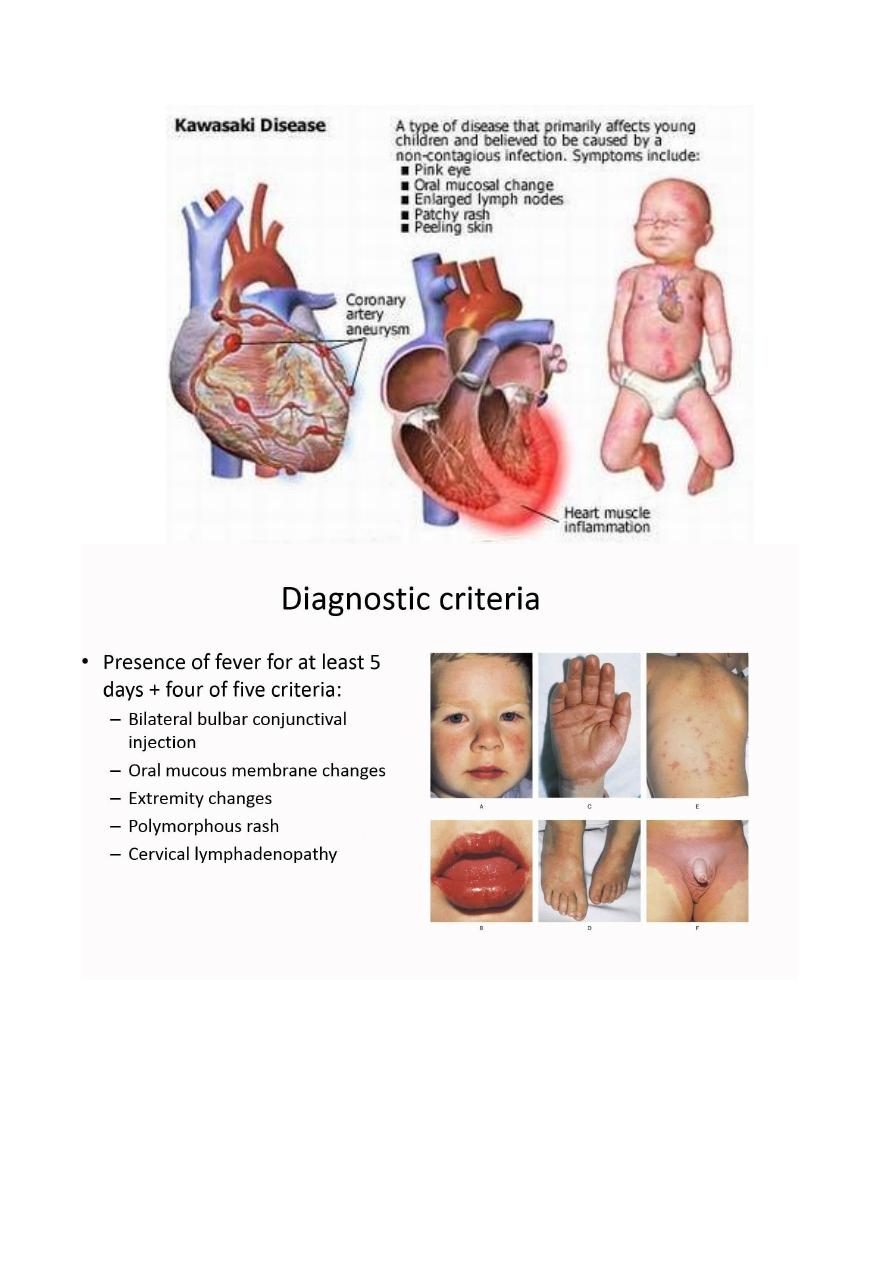
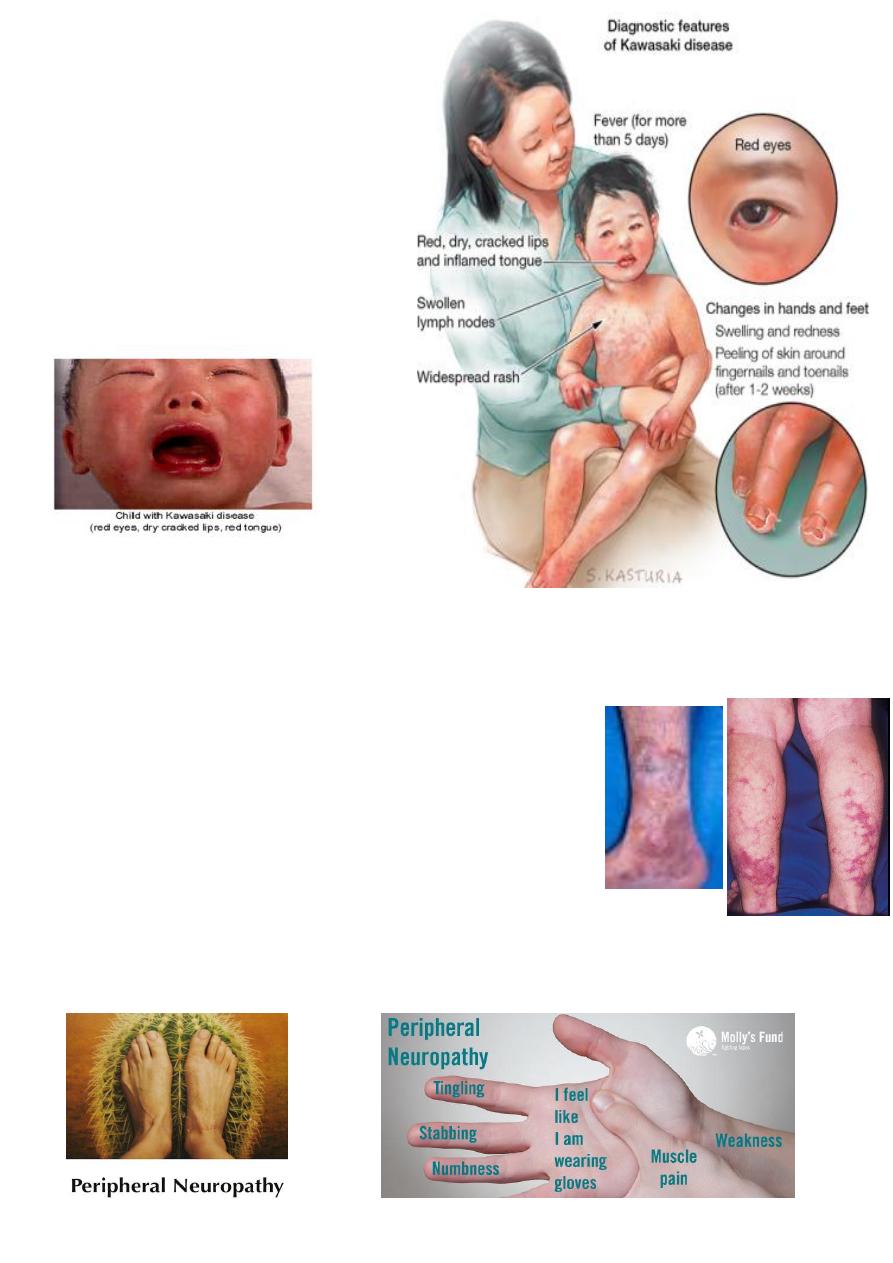
2. Medium vessel –classical polyarteritis nodosa, Kawasaki disease
3. Small vessel –microscopic polyangiitis, wegner’s granulomatosis, Churg-Strauss
syndrome, Henoch –Schonlein purpura, mixed essential cryoglobulinaemia
Secondary Vasculitis
Drug induced Vasculitis
Serum sickness
Vasculitis associated with other primary disorders:
1. Infection –HBV ,HCV
2. Malignancy
3. Rheumatic diseases –SLE ,RA
4. Endocarditis

2
Clinical Features
Constitutional symptoms –fever ,weight loss ,fatigue
Skin –purpura , liviido reticularis ,digital infarction
Musculoskeletal –arthralgias ,arthritis
Pulmonary –alveolar hemorrhage , pulmonary nodules
GIT –bowl ischemia /infarction
Renal –GN ,nephrotic syndrome ,renovascular involvement ,hypertension
Neurological –mononeuritis multiplex ,visual disturbances ,stroke ,lightheadedness
CVS –pulselessness /bruits ,claudication ,aneurysms
Investigations
Lab abnormalities –anemia ,eosinophilia , elevated acute phase reactant ,renal
insufficiency ,active urinary sediments
Tissue biopsy (skin ,nasal septum ,muscle)
Renal biopsy (RFT/GUE abnormality)
Visceral angiography
ANCA : c-ANCA - p-ANCA (Anti-neutrophil cytoplasmic antibody )
Which are a group of autoantibodies, mainly of the IgG type, against antigens in
the cytoplasm of neutrophil granulocytes (the most common type of white blood cell)
and monocytes. They are detected as a blood test in a number of autoimmune
disorders, but are particularly associated with systemic vasculitis.
Polymyalgia Rheumatica (PMR)
Clinical syndrome of muscle pain and stiffness and
classically, increased ESR
Close association with GCA
Prevalence is 20 per 100 000 (over 50)
Mean age of onset is 70
♀:♂ ratio is 3:1
3
Investigations
ESR is elevated above 40 mm/hour
Normochromic ,normocytic anemia
Elevated CRP (prior to ESR)
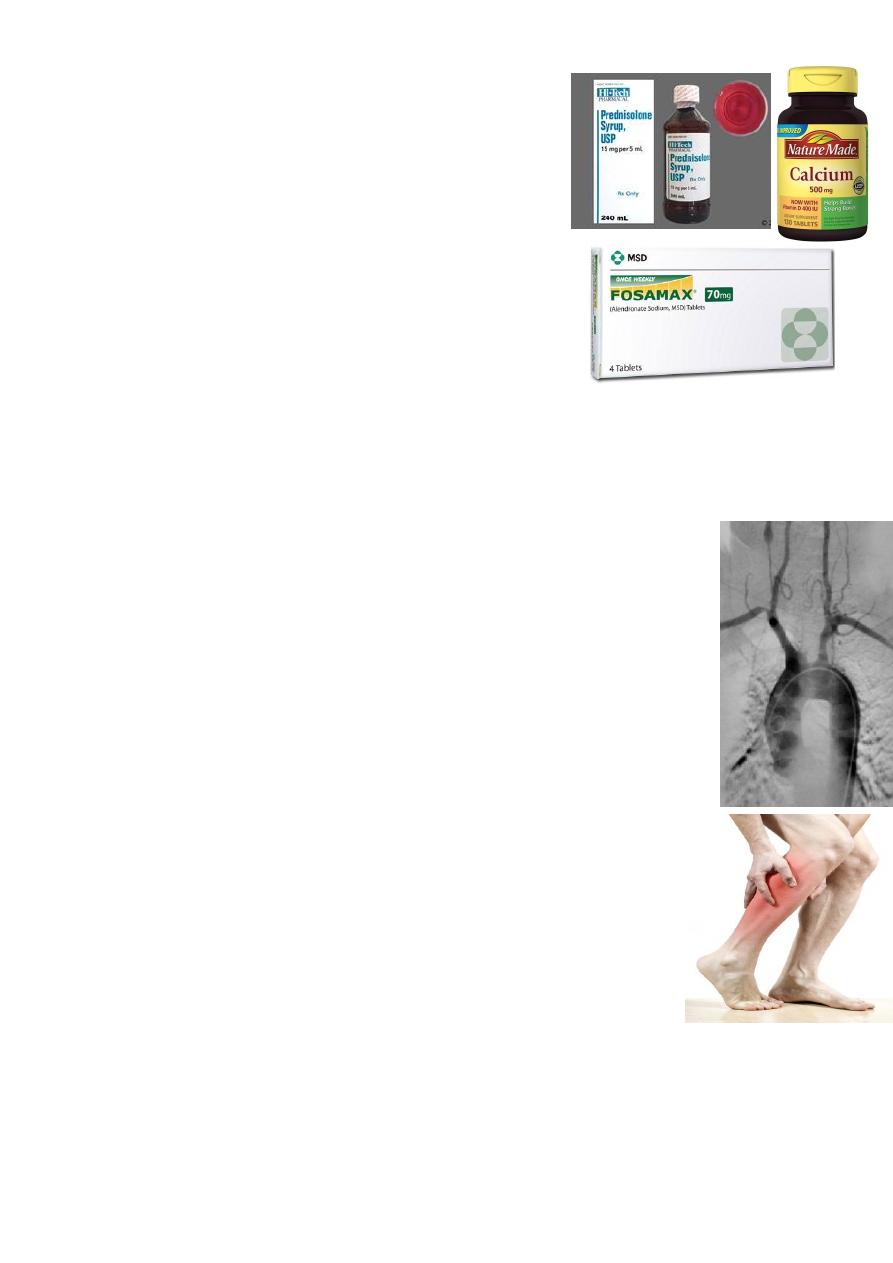
Management
Oral corticosteroids
Prednisolone 15 mg per day
Dramatic response within 72 hours
12 -18 months treatment
Osteoporosis prophylaxis with bisphosphonate
Steroid sparing agents (methotrexate, azathioprine)
Steroid cannot be withdrawn at 2 years
Dose greater than 7.5 mg per day
GCA should be treated promptly
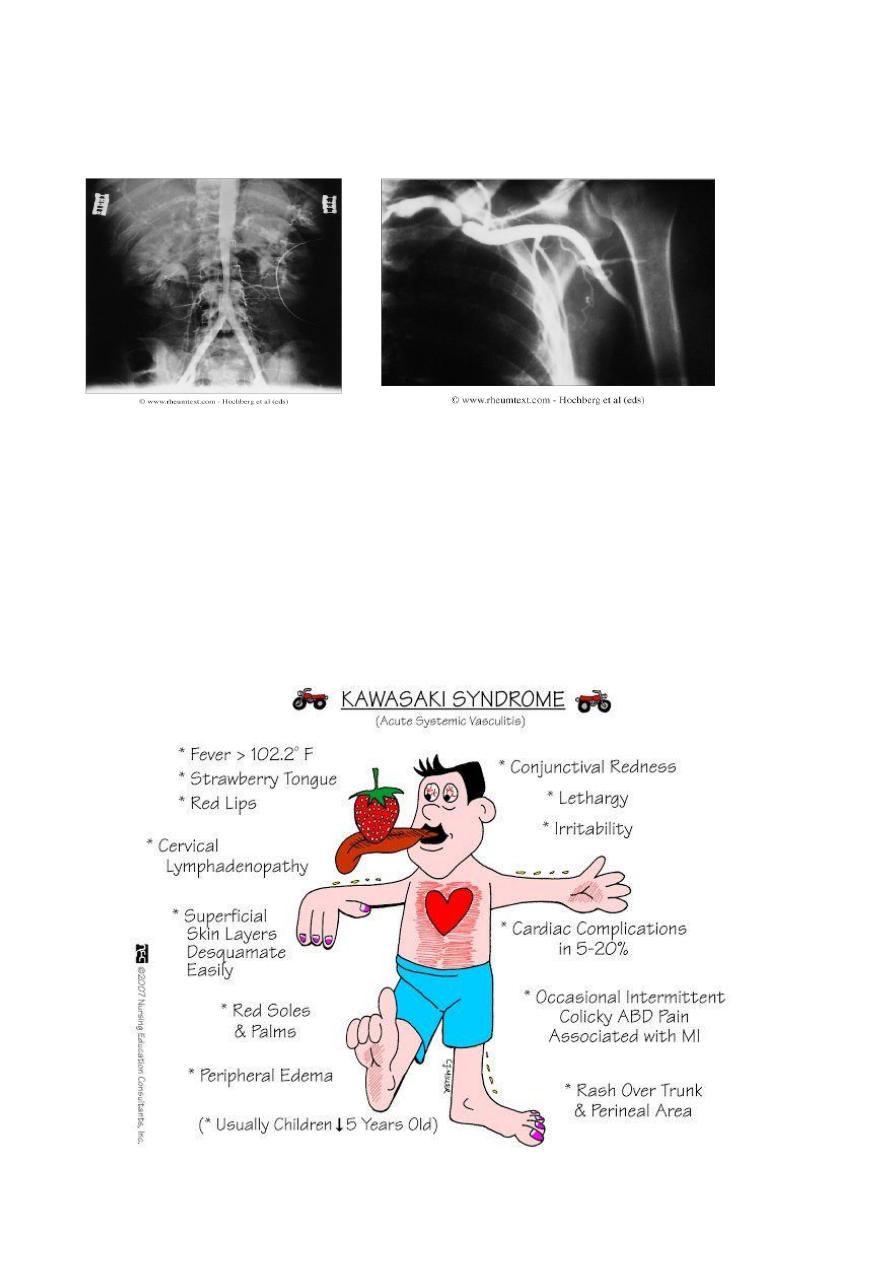
Takayasu’s Arteritis
Chronic inflammatory granulomatous panarteritis of elastic arteries
Aorta and its branches , carotid ,ulnar ,brachial ,radial and axillary
arteries are most commonly involved
♀:♂ ratio is 8 :1
Typical age of onset is 25 -30 years
Aetiology is unknown
Thickened and inflammed intima without fibrinoid degeneration
Clinical Features
Claudication
Systemic symptoms
On examination
Loss of pulses
Hypertension
Bruits
Aortic incompetance
Classified into four types:
Type 1: localized to the aorta and its branches
Type 2: localized to the descending thoracic and abdominal aorta
Type 3: combines features of 1 and 2
Type 4: involves the pulmonary artery.
4
Investigations
High ESR
Normochromic normocytic anemia
Angiography – coarctation, occlusion, anuerysmal dilatation
Management and Prognosis
High dose oral prednesolone
Additional methotrexate or cyclophosphamide is usually required
Reconstructive vascular surgery (avoided during active inflammation) benefit
hypertension secondary to aortic or renal lesion
5 –year survival rate is 80%
5
6
Polyarteritis Nodosa
PAN is a necrotizing vasculitis characterized by transmural inflammation of medium
sized to small arteries
Annual incidence is 2 per million
Peak incidence is 4
th
and 5
th
decade
♂:♀ ratio is 2:1
HBV is a risk factor
Clinical Features
Myalgia, arthralgia, fever and weight loss
Skin lesions –palpable purpura, ulceration, infarction and livedo reticularis
Peripheral neuropathy (70%) –symmetrical, sensory and motor
Severe hypertension and/ or renal impairment
Treatment
Aspirin
(5mg/kg for 14 days)
IV Gamaglobulin
400 mg/kg daily for 4 days
7
Investigation
Normochromic normocytic anemia
Mild to moderate leukocytosis
Moderate to profound thrombocytosis
Elevated ESR ,CRP
RF ,ANF are negative
GUE –hematuria , RBC cast
Hepatitis B and C serology
Diagnosis
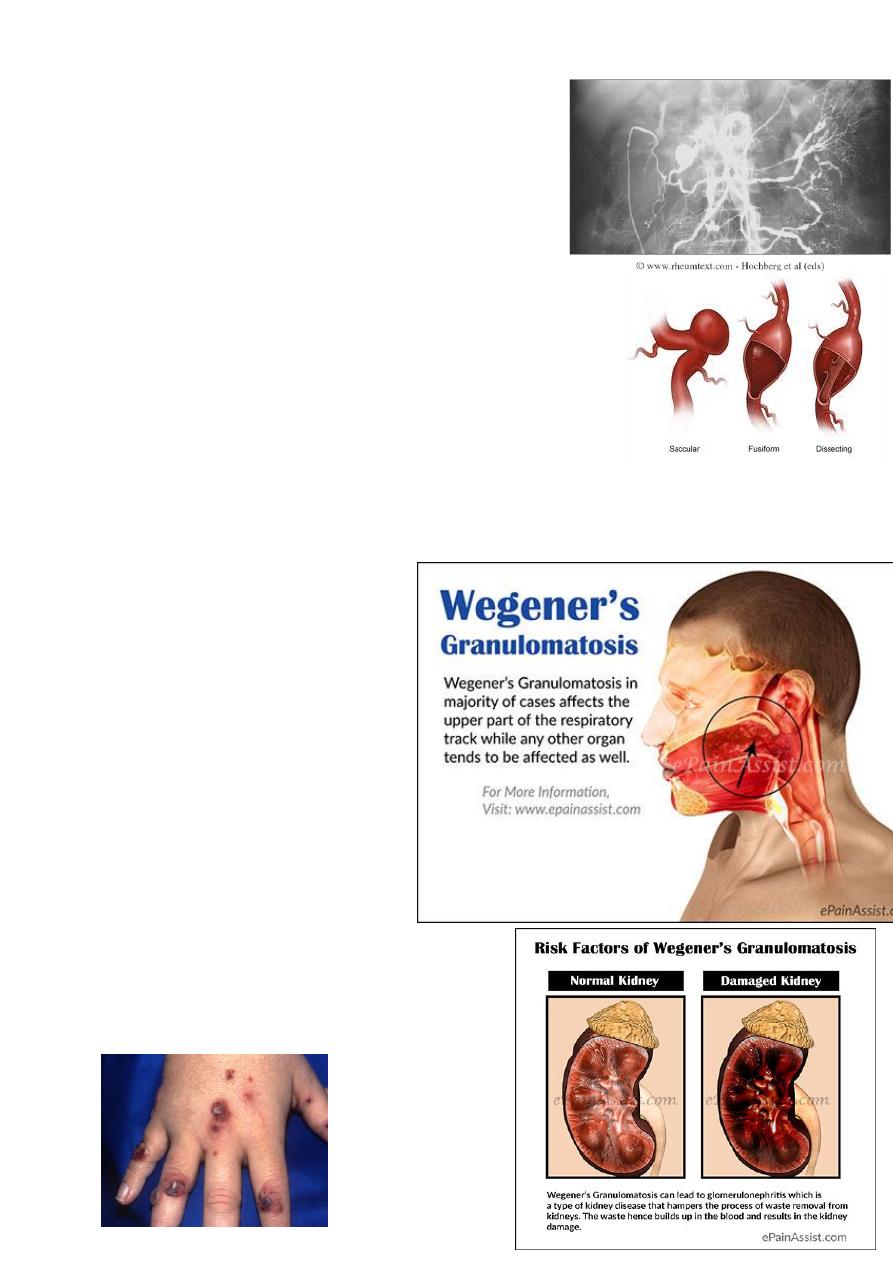
Angiography –multiple anuerysims and smooth narrowing
of mesenteric , hepatic or renal systems
Tissue biopsy (muscle or sural nerve)
Management and Prognosis
HBV related disease –antiviral therapy
Idiopathic disease –corticosteroids and cyclophosphamide
Mortality < 20%
Relapse –up to 50%
Wegner’s Granulomatosis(WG)
The annual incidence is 5 -10 per
million
♂:♀ ratio is 1:1
Can be seen at any age (rare
before adolescence)
Mean age of onset is 40 years
Definition
It is a syndrome characterized by:
Granulomatous inflammation
involving the respiratory tract
Necrotizing vasculitis affecting small to
medium sized vessel
Necrotizing GN is common
8
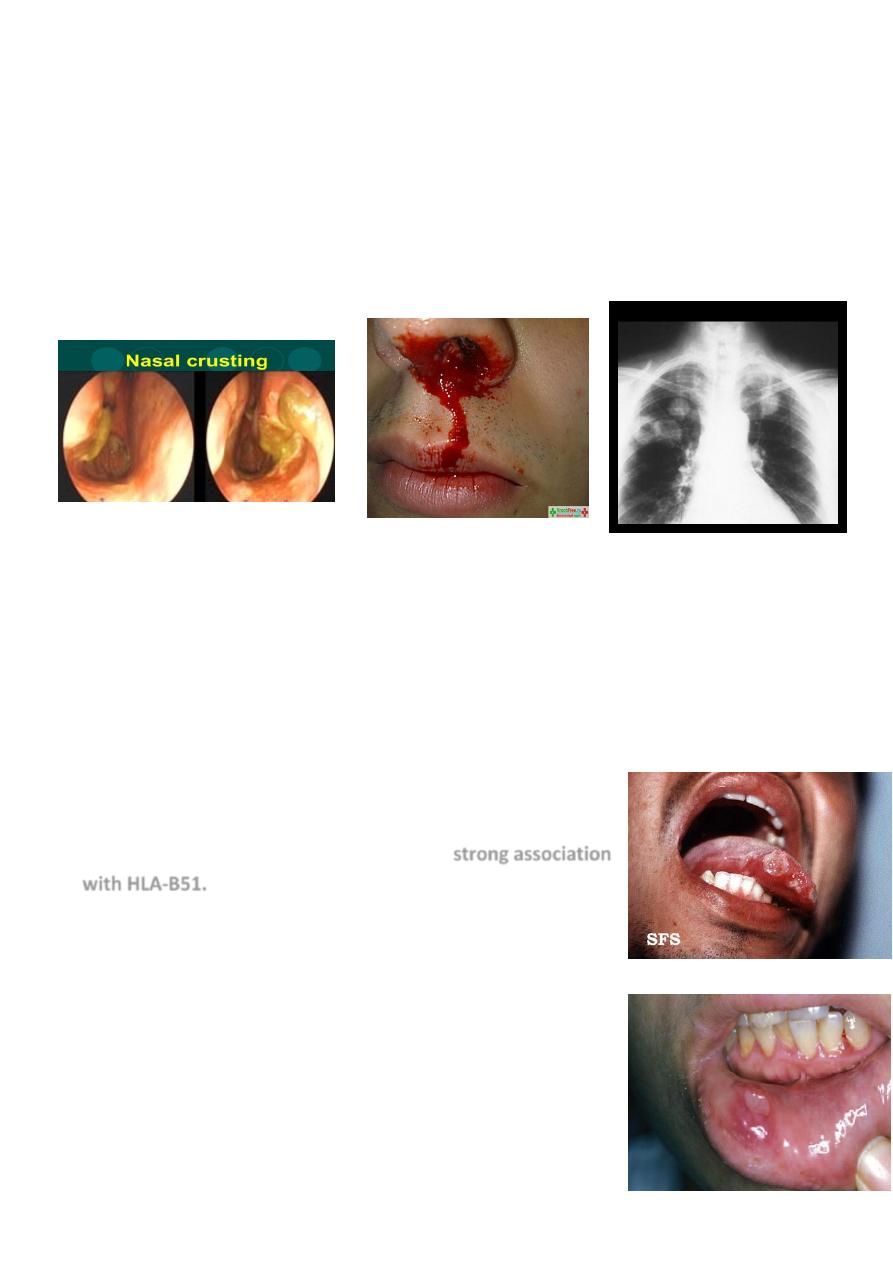
Clinical features
Upper airway involvement (95%) –epistaxis ,nasal crusting ,sinusitis ,nasal mucosal
ulceration, nasal septal perforation and deafness (serous otitis media )
Pulmonary involvement (85% -90%) –asymptomatic infiltrate ,cough, hemoptysis,
dyspnea and chest discomfort
Eye involvement(52%) –mild conjunctivitis, episcleritis, scleritis, granulomatous
sclerouveitis, cilliary vessel vasculitis, retroorbital mass lesion (proptosis, diplopia,
loss of vision)
Skin lesion –papule ,vesicle , palpable purpura ,ulcerations or subcutaneous nodules
Renal disease (77%) -GN
Diagnosis
Demonstration of necrotizing granulomatous vasculitis on tissue biopsy in the
presence of compatible clinical features (pulmonary tissue offer the highest
diagnostic yield )
When biopsy specimens are non-diagnostic, ANCA assays provide important adjunct
to diagnosis
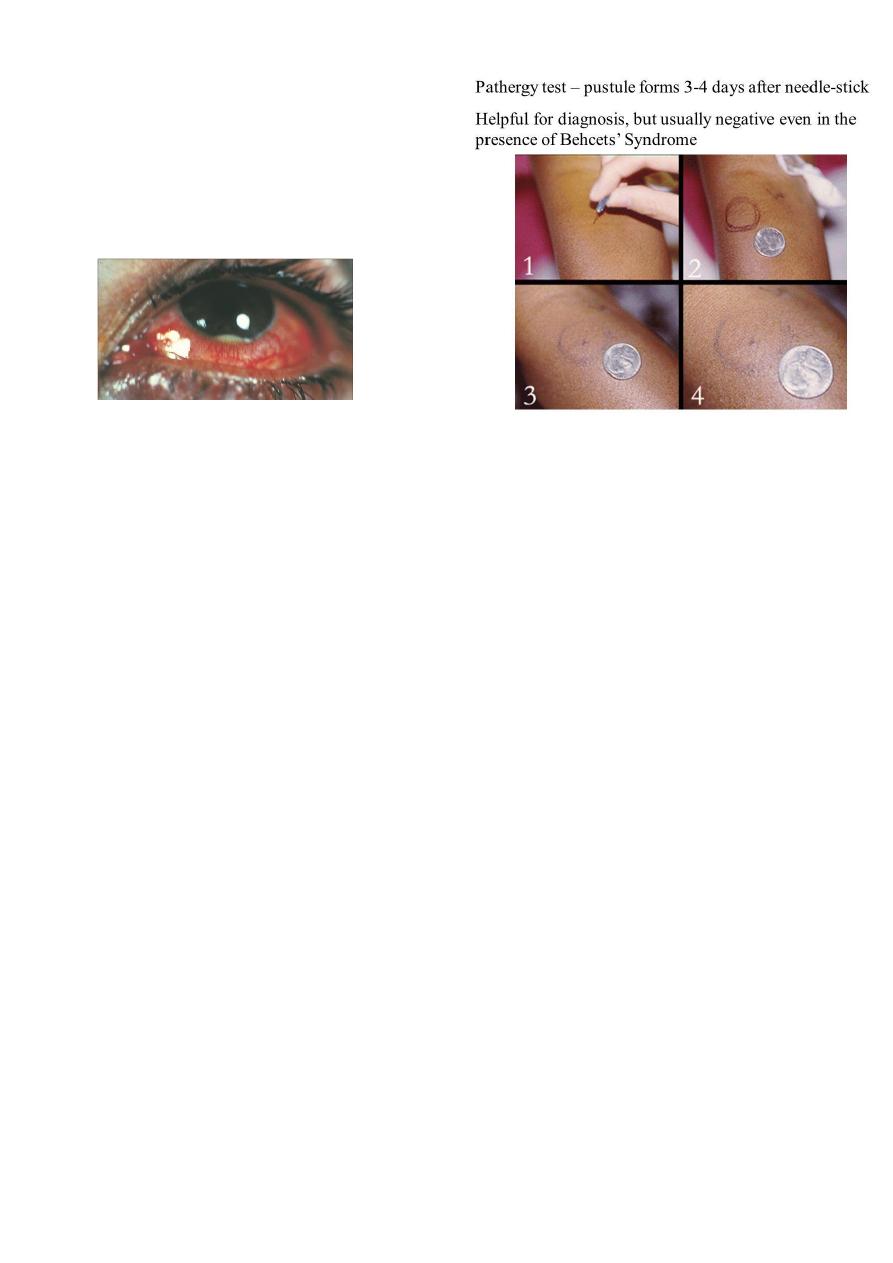
Behcet’s Syndrome
This is a vasculitis of unknown etiology that characteristically
targets small arteries and venules. It is rare in Western Europe
but more common in ‘Silk Route’ countries around the
Mediterranean and Japan, where there is a strong association
with HLA-B51.
Oral ulcers are universal, unlike aphthous ulcers, they are
usually deep and multiple, and last for 10–30 days. Genital
ulcers are also a common problem, occurring in 60–80% of
cases.
The usual skin lesions are erythema nodosum or acneiform
lesions, but migratory thrombophlebitis and vasculitis also
occur. Ocular involvement is common and may include
anterior or posterior uveitis or retinal vasculitis. Neurological
involvement occurs in 5% and mainly involves the brainstem,
although the meninges, hemispheres and cord can also be
affected, causing pyramidal signs
9
Diagnosis
Recurrent oral ulcerations plus 2 of the
followings:
Recurrent genital ulceration
Eye lesions
Skin lesions
Pathergy test
Clinical Features
Recurrent oral ulceration –universal ,usually painful, shallow or deep with central
yellowish necrotic base ,singly or in croups ,anywhere in the oral cavity ,persist for 1-2
weeks ,no scar formation.
Genital ulceration –less common, more specific, don’t affect the glance penis or urethra,
and produce scrotal scars.
Skin involvement –folliculitis, erythema nodosum, acne-like exanthem, and infrequently
vasculitis.
Lab Finding
Leukocytosis
Elevated ESR
Elevated CRP
Autoantibodies may be found
Treatment
Mucous membrane involvement –topical glucocorticoid (mouth wash or paste)
Thalidomide –resistant oral and genital ulceration
Colchicine –erythema nodosum and arthralgia
Thrombophlebitis –aspirin 325 mg /day
Uveitis and CNS-Behcet’s –systemic glucocorticoids and azathioprin
Interferon –very effective for CNS-Behcet’s and refractory uveitis
