Oral mucous membrane (O.M.M)
• Functions of oral mucosa:-• Protection: ex. mechanical forces during chewing, acts as major barrier to microorganisms.
• Sensation:- receptors that respond to temperature (heat and cold), touch, pain, taste buds, thirst , reflexes such as swallowing.
• Secretion Salivary secretion, produced by minor salivary gland, to maintain the moist surface.
• Thermal regulation: In some animals (dog), considerable body heat is dissipated through oral mucosa by panting. For these animals, oral mucosa plays a major role in regulating of body temperature. This function is not active in humans.
Classification of Oral Mucosa
• 3main types of mucosa identified according to their primary function• (1)-Lining mucosa (60%) lips, cheeks, floor of the mouth, interior surface of the tongue.
• (2)-Masticatory mucosa (25%) gingiva and palate.
• (3)-Specialized mucosa (15%) on the dorsal surface (dorsum) of the tongue.
1
2
3
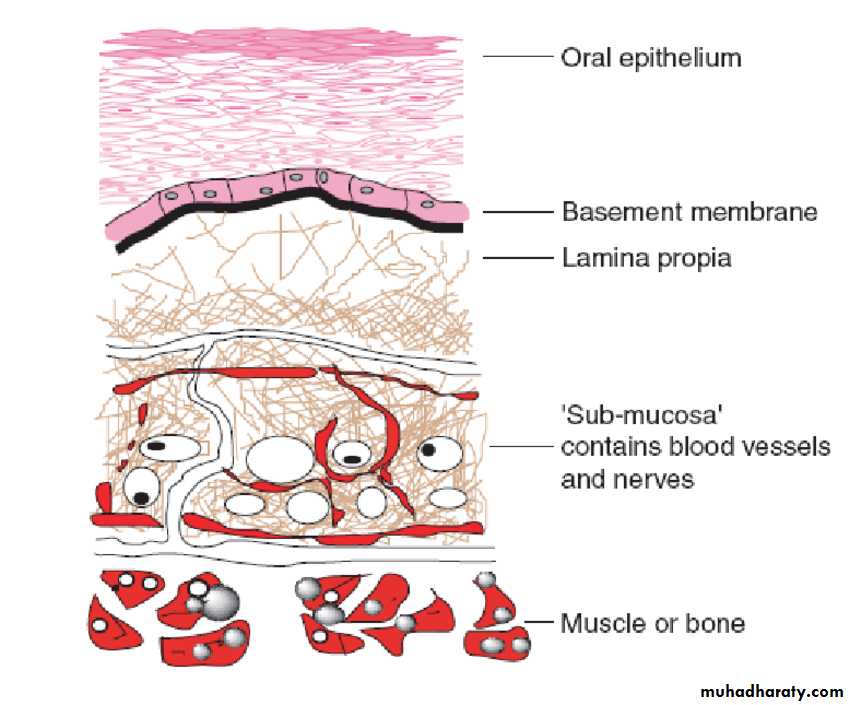
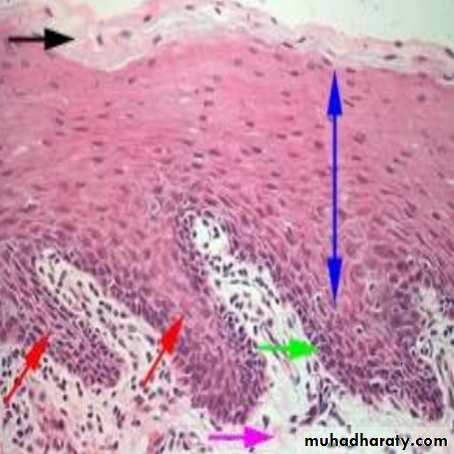
Histological appearance of O.M.M.
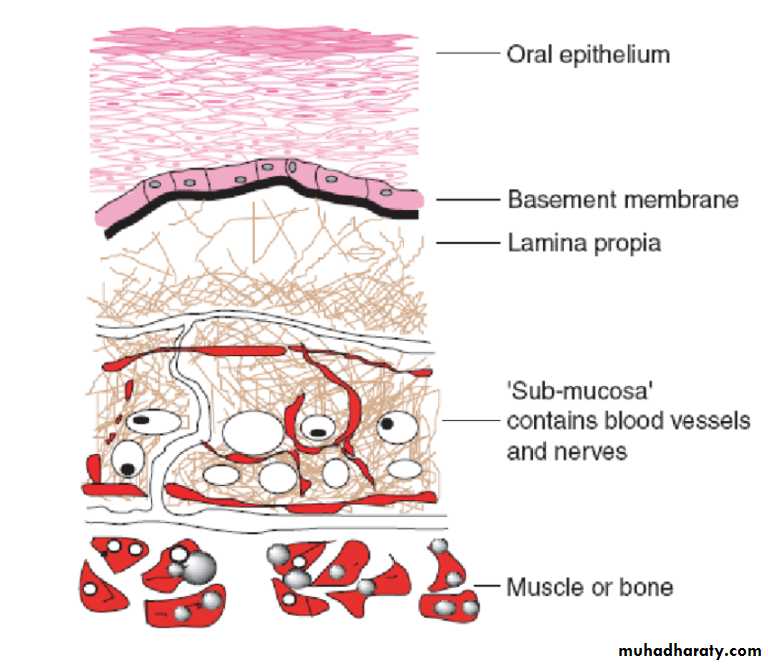
• There are mainly 2 components• oral epithelium made up of stratified squamous epithelium
• underlying connective tissue called lamina propria.
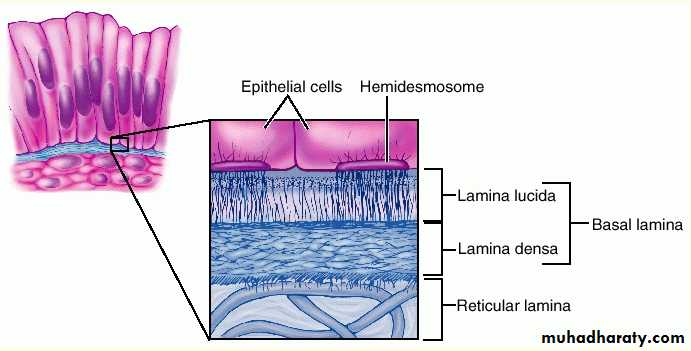
• the structural interface between epithelium and connective tissue called the basement membrane
• Submucosa it attaches the mucosa to the underlying structures, it could be absent.
Oral epithelium
• It is derived from the embryonic ectoderm.• Its stratified squamous variety, it may be:-
• Keratinized .
• Parakeratinized.
• Non-keratinized.
• The epithelial cell of the O.M. called keratinocyts.
• A common feature of all epithelial cells is that contain keratin intermediate filaments.
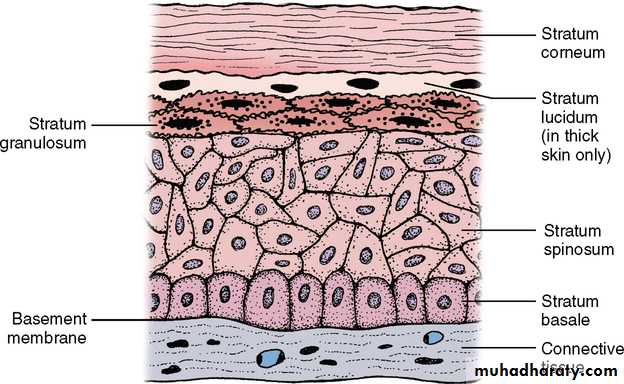
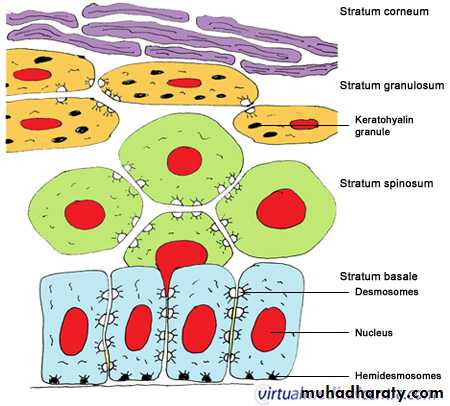
Keratinized oral epithelium
• Stratum basali
• Stratum spinosum
• Stratum granulosum
• Stratum cornium
• 1.Stratum basali
• Layer of cubodial or columnar cells.• Adjacent to the basement membrane.
• There cells have a capacity to divides and proliferates to replace the desquamating surface cells.
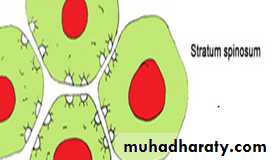
• Stratum Spinosum
• Composed of several rows of larger elliptical or spherical cells ( termed as prickle cell )• They remain in contact through intercellular bridges or desmosomes.
• They are active in protein synthesis.
• The basal cells layer & parabasal spinous cells are known as agerminative layer.
• Stratum granulosum
Cells of stratum granulosum are flat and are found in layers of three to five cells thickThis layer is prominent in keratinized epithelium (and absent in nonkeratinized epithelium)
These cells have keratohyaline granules in their cytoplasm
Keratohyaline granules help to form the matrix of the keratin fibres.
• Stratum cornium
The cells are larger and flatter than granular layer.The nuclei and other cytoplasmic organelles such as ribosomes & mitochondria have disappeared.
The layer is acidophilic ( red staining with H & E).
Histologically amorphous layer that the cell composed of densely packed filaments.
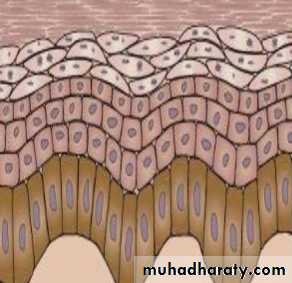
Parakeratinized epithelium:-
• The keratinocytes maintain their nuclei.• Prickle cell layer.
• Basal layer.
• Rete pegs.
• Lamina propria (underlying connective tissue).
•
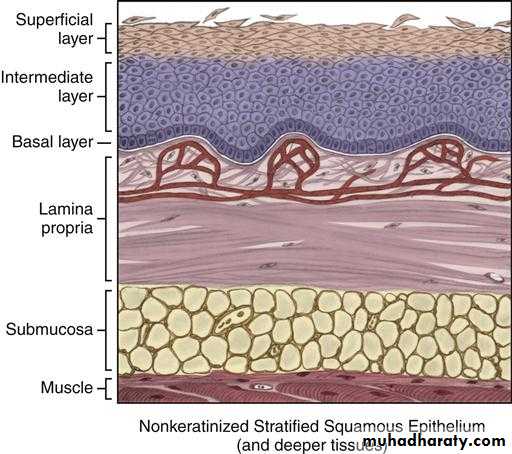
Non-Keratinized epithelium
• Sratum basali• Sratum intermedium
• Superficial layer
•
Constitute the major part of epithelial cells
The cells are arranged in different layersAlways present in sheets & attached to each other by one or more type of cellular junctions.
The attachment of epithelial cells to one another is by desmosome, while The attachment of epithelial cell to connective tissue is by Hemi Desmosome.
Cytoplasm of these cells is stained with H & E.
Cytoplasm contains the tonofilaments
During maturation play important role; they either change to keratin or share in keratin formation.
KERATINOCYTES
NON-KERATINOCYTES
Present in both keratinized & non-keratinized epithelium & have the following criteria:-• Present as scattered cells & not in sheets
• No cellular junctions
• Does not appear as clear cells by ordinary H&E stain, they need special stains
• A clear hallows around their nuclei
• Their cytoplasm is free from tonofilaments
• Do not play any role in synthesis of keratohyaline granules or keratin .
Melanocytes:- dendritic cell, present in basal layer, originates from neural crest cells, produce melanin.
Langerhans cell:- dendritic, present in supra basal layer, act as macrophage.
Merkells cell:- non-dendritic, present in basal layer, act as sensory cell.
Lymphocytes:- present in any layer associated with inflammatory response.
Connective tissue
Connective tissue can be differentiated as Lamina Propria and Submucosa
Lamina propria is the connective tissue layer immediately below the epithelium, Lamina propia can be divided into:
1)papillary layer - prominent in masticatory mucosa.
2)reticular layer-prominent in lining mucosa.
Lamina propria consists of blood vessels, cells like fibroblasts, lymphatics and nerves.
Lamina propria variable thickness
Epithelium is avascular, hence its metabolic needs come via the vessels of the lamina propria.
Submucosa (S.M.)
• It consist of c.t. of varying thickness and density.
• It attach the m.m. to the underlying structures.• It composed of glands, b.v. , nerve & adepose tissue.
• The larger arteries divided into smaller branches, which enter the lamina properia to give an subepithelial branches.
Basal Lamina ( B.L. )
• Lamina lucida – present on epithelial side.• Lamina densa – present on c.t. side.