1
Fifth stage
Pediatrics
Lec-8
Dr. Athal
10/11/2016
“ Metabolic Disturbances “
Neonatal Cold Injury
Neonatal cold injury usually occurs in neglected infants, infants in inadequately heated
homes during cold spells when the outside temperature is low, and in preterm infants.
Manifestation:
The initial features are apathy, refusal of food, oliguria, and coldness to touch.
The body temperature is usually between 29.5 and 35°C, and immobility, edema, and
redness of the extremities, especially the hands and feet, and of the face are observed.
The facial erythema frequently gives a false impression of health and delays recognition
that the infant is ill .
Local hardening over areas of edema (sclerema neonatorum).
Bradycardia and apnea may also occur .
Hypoglycemia and acidosis are common .
Hemorrhagic manifestations are frequent; massive pulmonary hemorrhage is a common
finding at autopsy.
Treatment:
Rapid rewarming.
Fluid resuscitation to treat hypovolemia.
Correction of metabolic imbalances, particularly hypoglycemia.
Hypocalcemia
All infants show a slight decline of serum calcium levels after birth, reaching a trough
level at 24 to 48 hours, the point at which hypocalcemia usually occurs.
Total serum calcium levels of less than 7 mg/dL and ionized calcium levels of less than 3
to 3.5 mg/dL are considered hypocalcemia.
The etiology
of hypocalcemia varies with the time of onset and the associated illnesses
of the child.
Early neonatal hypocalcemia occurs in the first 3 days of life and is often asymptomatic.
Transient hypoparathyroidism and a reduced parathyroid response to the usual
postnatal decline of serum calcium levels may be responsible for hypocalcemia in
premature infants and infants of diabetic mothers .
2
Congenital absences of the parathyroid gland with DiGeorge syndrome is a cause of
hypocalcemia .
Hypomagnesemia (<1.5 mg/dL) may be seen simultaneously with hypocalcemia,
especially in infants of diabetic mothers. Treatment with calcium alone does not relieve
symptoms or increase serum calcium levels until hypomagnesemia is also treated .
Sodium bicarbonate therapy, transient hypoparathyroidism, and hypercalcitoninemia
may be responsible for early neonatal hypocalcemia associated with asphyxia.
Late neonatal hypocalcemia, or neonatal tetany, often is the result of :
Ingestion of high phosphate–containing milk or the inability to excrete the usual
phosphorus in commercial infant formula. Hyperphosphatemia (>8 mg/dL) usually
occurs in infants with hypocalcemia after the first week of life.
Vitamin D deficiency states and malabsorption also have been associated with late-onset
hypocalcemia.
Clinical Manifestations
Include apnea, muscle twitching, seizures, laryngospasm
Chvostek sign (facial muscle spasm when the side of the face over the seventh nerve is
tapped).
Trousseau sign (carpopedal spasm induced by partial inflation of a blood pressure cuff).
The latter two signs are rare in the immediate newborn period.
Treatment
Early asymptomatic hypocalcemia of preterm infants and infants of diabetic mothers
often resolves spontaneously .
Symptomatic hypocalcemia should be treated with 2 to 4 mL/kg of 10% calcium
gluconate given intravenously and slowly over 10 to 15 minutes, followed by a
continuous infusion of 75 mg/kg/24 hr of elemental calcium.
If hypomagnesemia is associated with hypocalcemia, 50% magnesium sulfate, 0.1 mL/kg,
should be given by intramuscular injection and repeated every 8 to 12 hours.
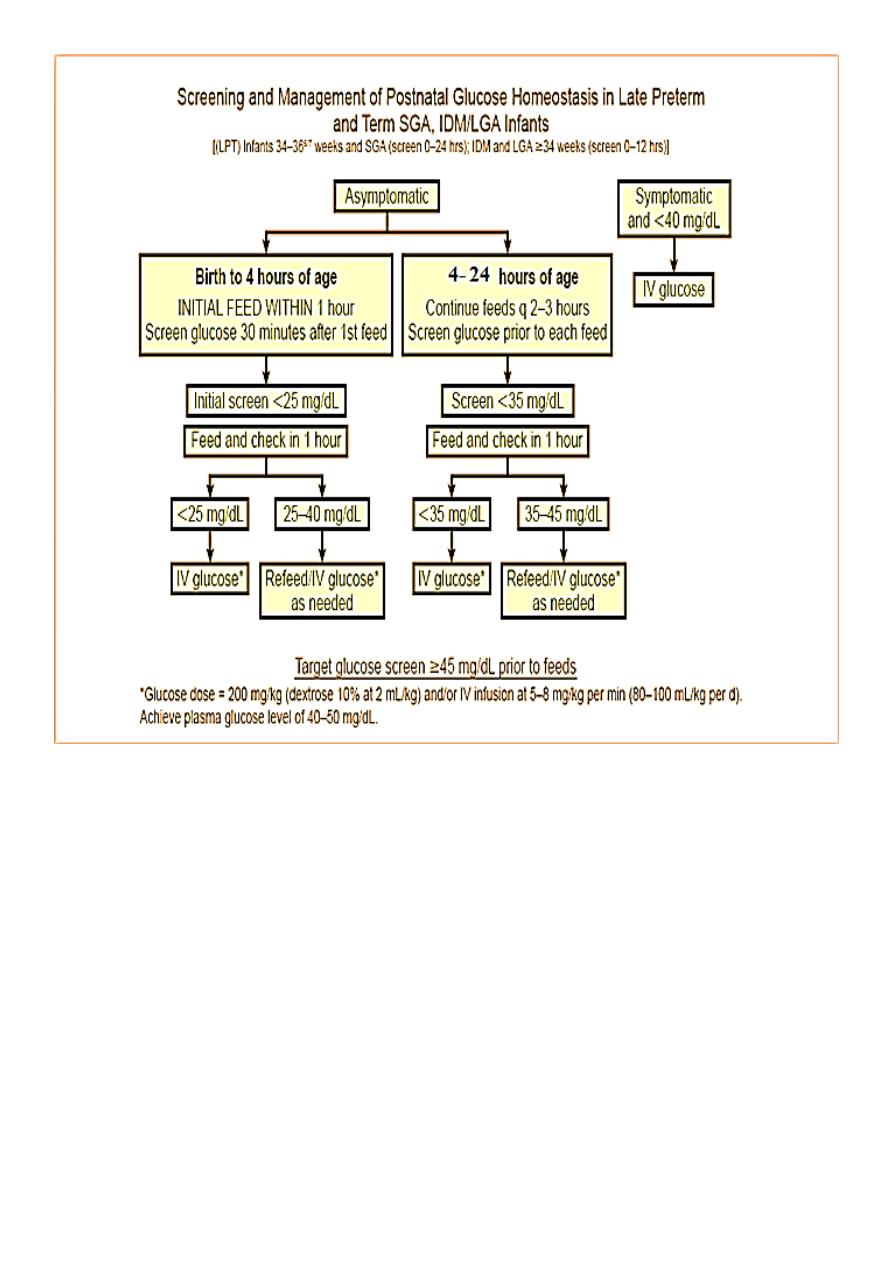
Hypoglycemia
In neonates, there is not always an obvious correlation between blood glucose
concentration and the classic clinical manifestations of hypoglycemia. The absence of
symptoms does not indicate that glucose concentration is normal and has not fallen to
less than some optimal level for maintaining brain metabolism. There is evidence that
hypoxemia and ischemia may potentiate the role of hypoglycemia in causing permanent
brain damage .
Consequently, the lower limit of accepted normality of the blood glucose level in
newborn infants with associated illness that already impairs cerebral metabolism has
not been determined.
3
Most authorities recommend that any value of blood glucose <55 mg/dL in neonates
represents hypoglycemia, and should be treated. This is particularly applicable after the
initial 2-3 hr of life, when glucose normally has reached its nadir.
Eitiology
1. NEONATAL TRANSITIONAL (ADAPTIVE) HYPOGLYCEMIA
A) Associated with Inadequate Substrate or Immature Enzyme Function in Otherwise
Normal Neonates:
Prematurity.
Small for gestational age.
Normal newborn.
B) Transient Neonatal Hyperinsulinism:
Infant of diabetic mother.
2.NEONATAL PERSISTENT HYPOGLYCEMIAS
A) Hyperinsulinism:
Genetics.
Acquired islet adenoma.
Beckwith-Wiedemann syndrome.
Insulin administration (Munchausen syndrome by proxy).
B) Counterregulatory Hormone Deficiency:
Panhypopituitarism.
Isolated growth hormone deficiency.
C) Glycogenolysis and Gluconeogenesis Disorders:
Galactosemia.
3.SYSTEMIC DISORDERS
Sepsis.
CLINICAL MANIFESTATIONS
1. Symptoms associated with the activation of the autonomic nervous system and
epinephrine release, such as perspiration, palpitation (tachycardia), pallor,
tremulousness, weakness.
2. Symptoms caused by decreased cerebral glucose utilization (cerebral glycopenia), such
as refusal to feed, somnolence, lethargy, seizures.
3. The symptoms of hypoglycemia in newborns and infants may be subtler and include
cyanosis, apnea, hypothermia, hypotonia, weak or high-pitched cry. Some of these
symptoms may be so mild that they are missed.
4. Occasionally, hypoglycemia may be asymptomatic in the immediate newborn period.
5. Newborns with hyperinsulinism are often large for gestational age.
4
Infants of Diabetic Mothers
IDM often surprisingly resemblance to each other. They tend to be large and plump,
with puffy, plethoric facies .
The probability that hypoglycemia will develop in IDM increases, and glucose levels are
likely to be lower with higher cord or maternal fasting blood glucose levels.
The infants tend to be jittery, tremulous, and hyperexcitable during the 1st 3 days after
birth, although hypotonia, lethargy, and poor sucking may also occur .
Tachypnea .
IDM have a higher incidence of RDS.
Birth trauma is also a common sequela of fetal macrosomia.
These infants have an increased incidence of hyperbilirubinemia, polycythemia, and
RVT.
The incidence of congenital anomalies is increased 3-fold IDM; cardiac and lumbosacral
agenesis are most common. Additional anomalies include neural tube defects,
hydronephrosis, renal agenesis and dysplasia, duodenal or anorectal atresia & situs
inversus. These infants may also demonstrate abdominal distention caused by a
transient delay in development of the left side of the colon, the small left colon
syndrome.
TREATMENT
Prophylactic treatment of infants of diabetic mothers should be initiated before birth by
means of preconception and frequent prenatal evaluations of all women with diabetes
and pregnant women with gestational diabetes.
Periconception glucose control reduces the risk of anomalies and other adverse
outcomes, and glucose control during labor reduces the incidence of neonatal
hypoglycemia.
5
SEQUELAE OF HYPOGLYCEMIA
The major long-term sequelae of severe, prolonged hypoglycemia are:
Cognitive impairment
Recurrent seizure activity
Cerebral palsy
Autonomic dysregulation .
Subtle effects on personality are also possible.
