
Superficial Fungal Infections of
the Skin
By
Dr. Salam Al-Temimi

Dermatophyte infections
The dermatophytes include a group of fungi
(ringworm) that have the ability to infect and
survive only on dead keratin (stratum corneum
of the skin, the hair, and the nails).
Dermatophytes are classified into 3 genera:
Microsporum, Trichophyton, and
Epidermophyton.

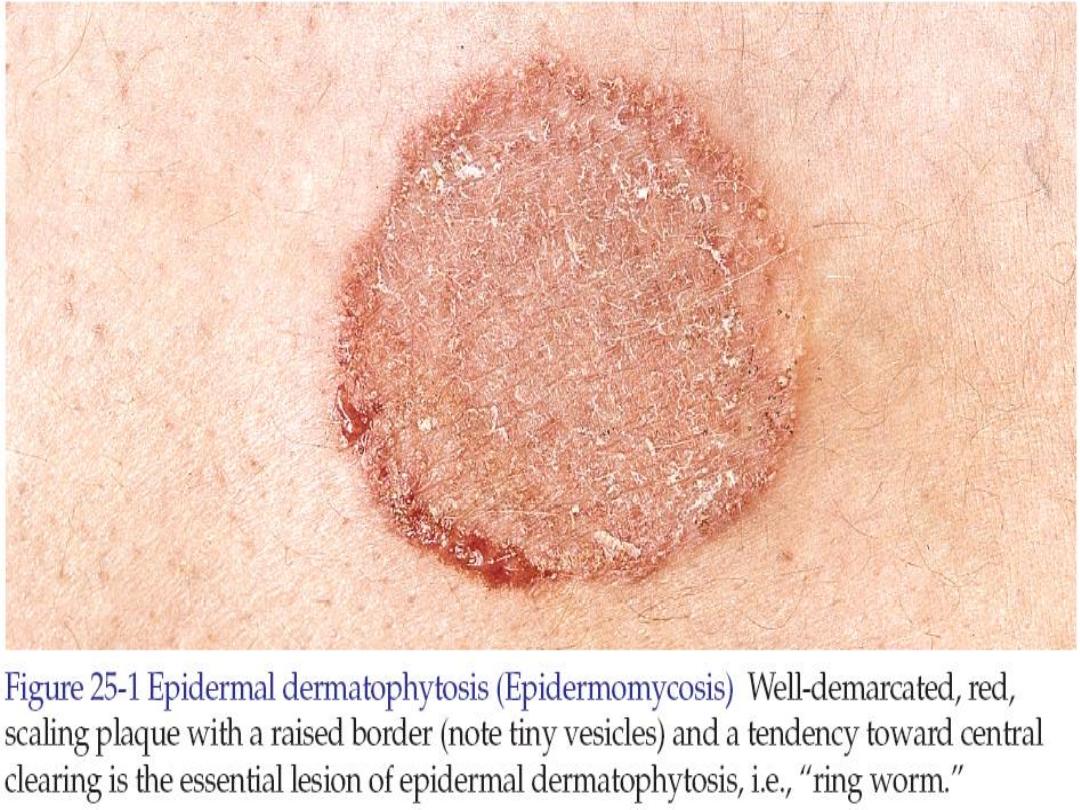
• Clinically skin infections characterized by
active border which is scaly, red and
slightly elevated. Vesicles occur in intense
inflammation. As the lesion expands the
center become relatively clear.
• This classical pattern of presentation
present in all locations except the palms
and soles.

Investigations
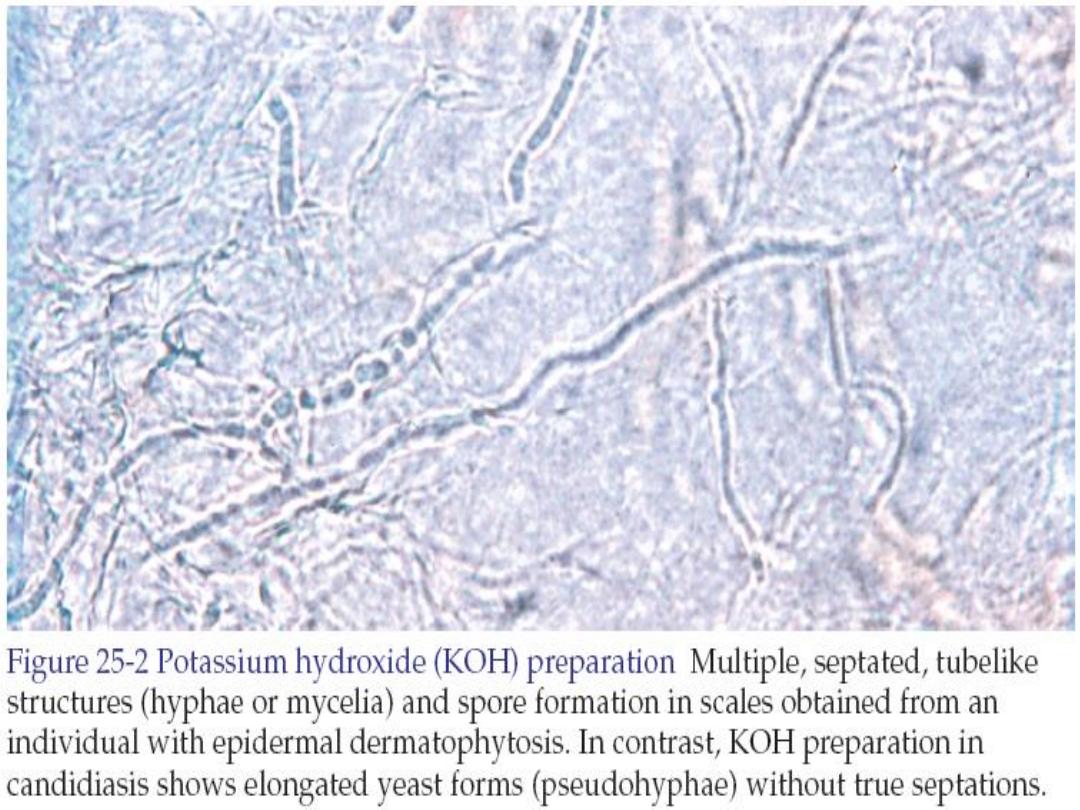
• KOH wet mount preparation:
dermatophytes appear as translucent
branching, rod-shaped filaments (hyphae)
of uniform width with lines of separation
(septa) spanning the width and appearing
at irregular intervals.

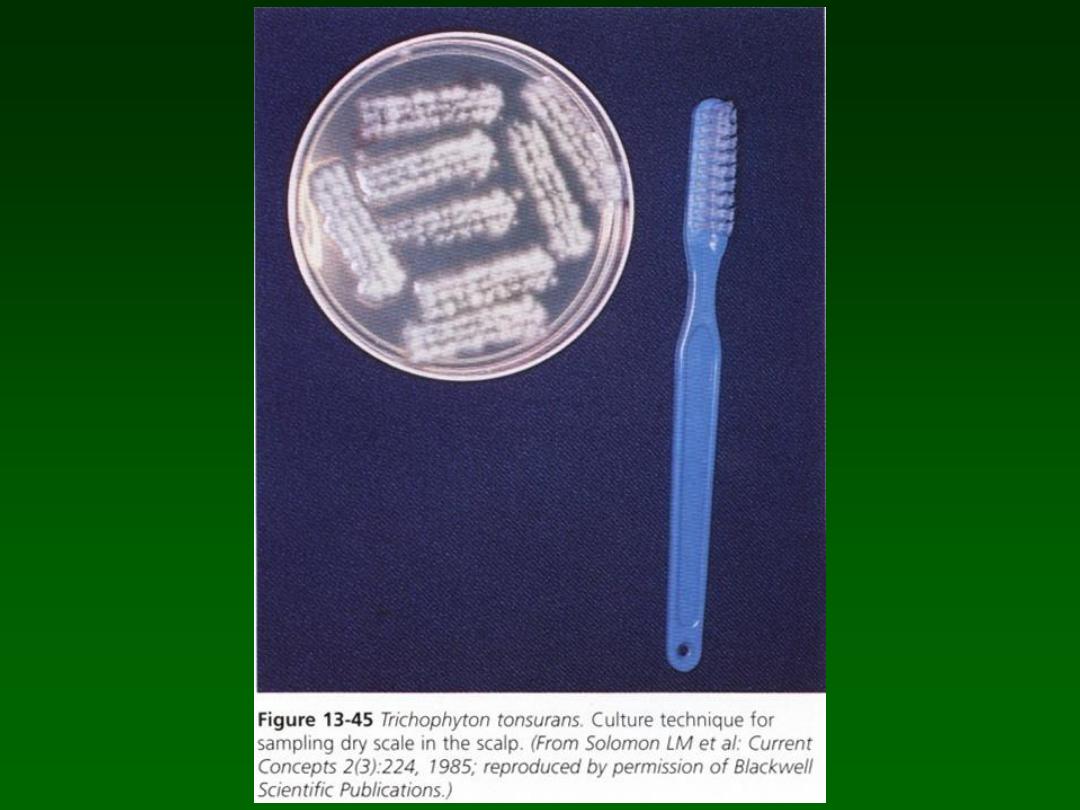
• Culture: is used to identify the species of
dermatophytes. There are Mycosel agar
and Sabouraud agar.
• Wood’s light examination: it is a device
gives light rays with wave length above
365 nm. Hairs fluoresce with a
blue-green
fluorescence if infected with microsporum
species. Hairs fluoresce
pale green
fluorescence if infected with trichophyton
schoenleinii. Pityriasis versicolor fluoresce
pale white yellow
fluorescence.

Tinea
• Tinea means fungus infection.
• Dermatophytes infections are classified by
body regions.

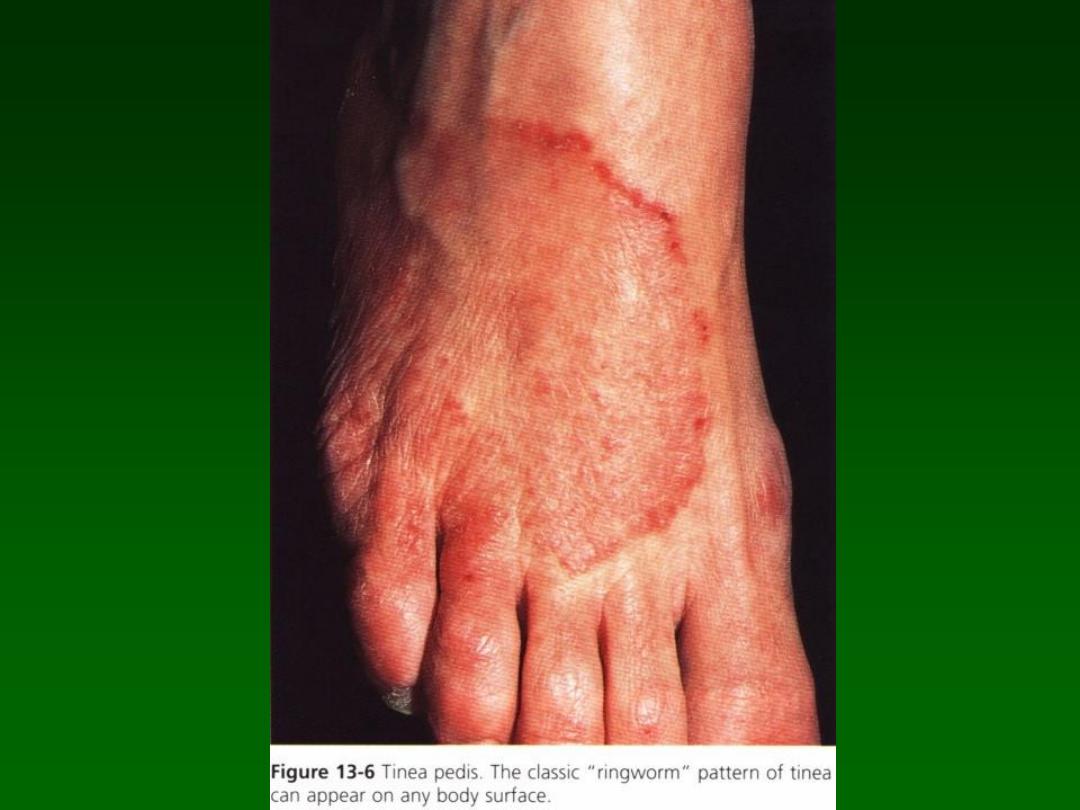
Tinea pedis (Athlete’s foot)
It is tinea of the foot. Shoes promote warmth
and sweating which encourage fungal growth.
It is common in men.

Clinical presentations of
tinea pedis
1. Classical ringworm infection
as described
above occurs on the dorsum of the foot.

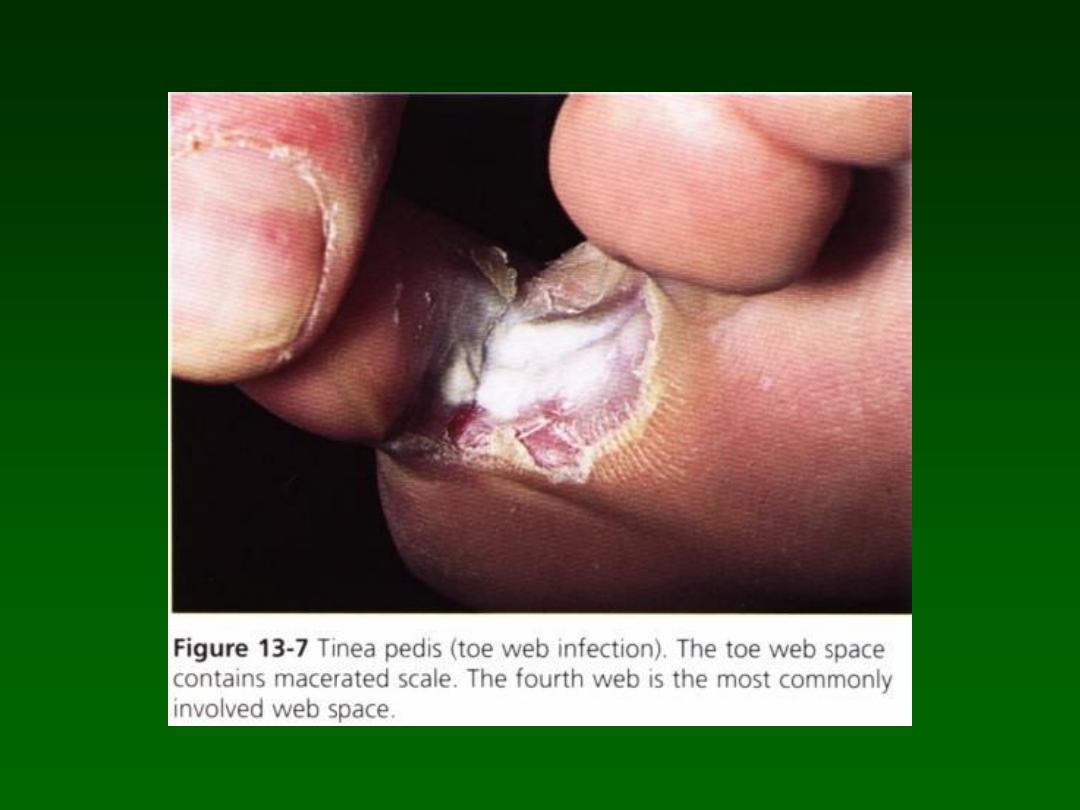
2. Interdigital tinea pedis (toe web infection):
the fourth toe web is common site. The
web becomes dry, scaly, fissured or
white, macerated and soggy. Itching is
common. Superadded bacterial infection
may complicate the infection.

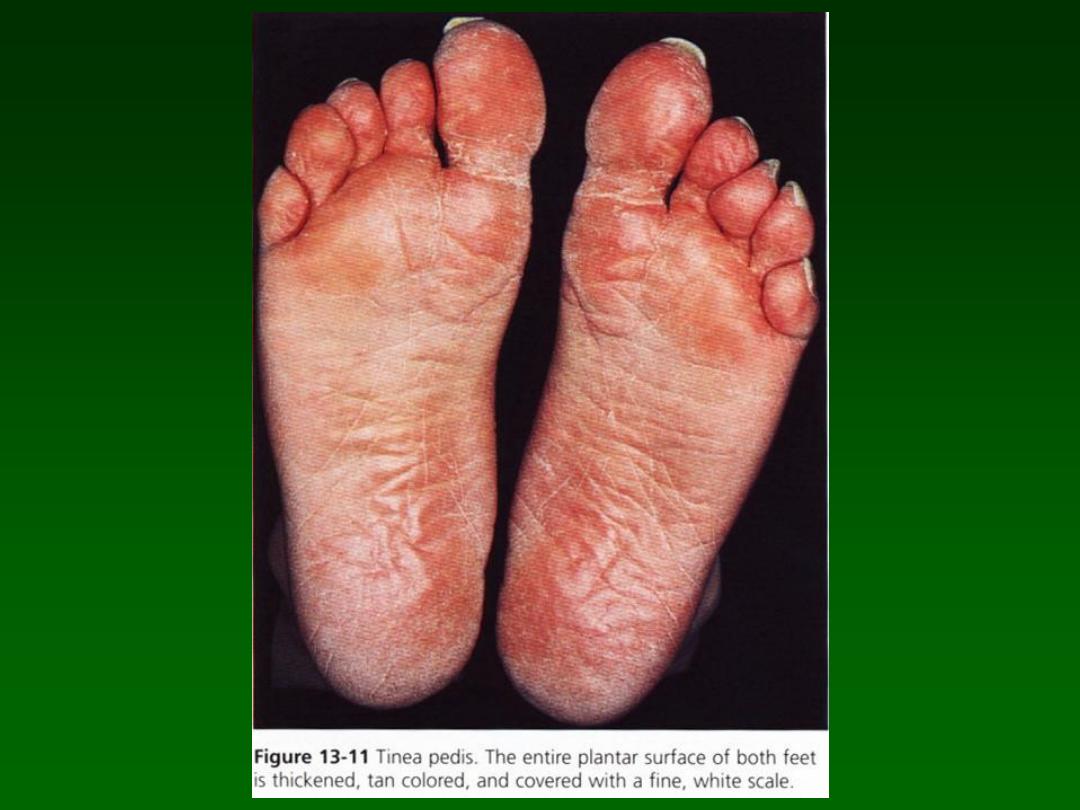
3. Chronic scaly infection of the planter
surface (hyperkeratotic or moccasin type
of tinea pedis):
the entire sole is usually
infected and covered with fine silvery
white scales. The skin is pink, tender and
pruritic. The hands may also be infected.
It is rare to see both palms and soles
infected simultaneously; rather, the
pattern is infection of two feet and one
hand or of two hands and one foot.
Trichophyton rubrum is the usual
pathogen.

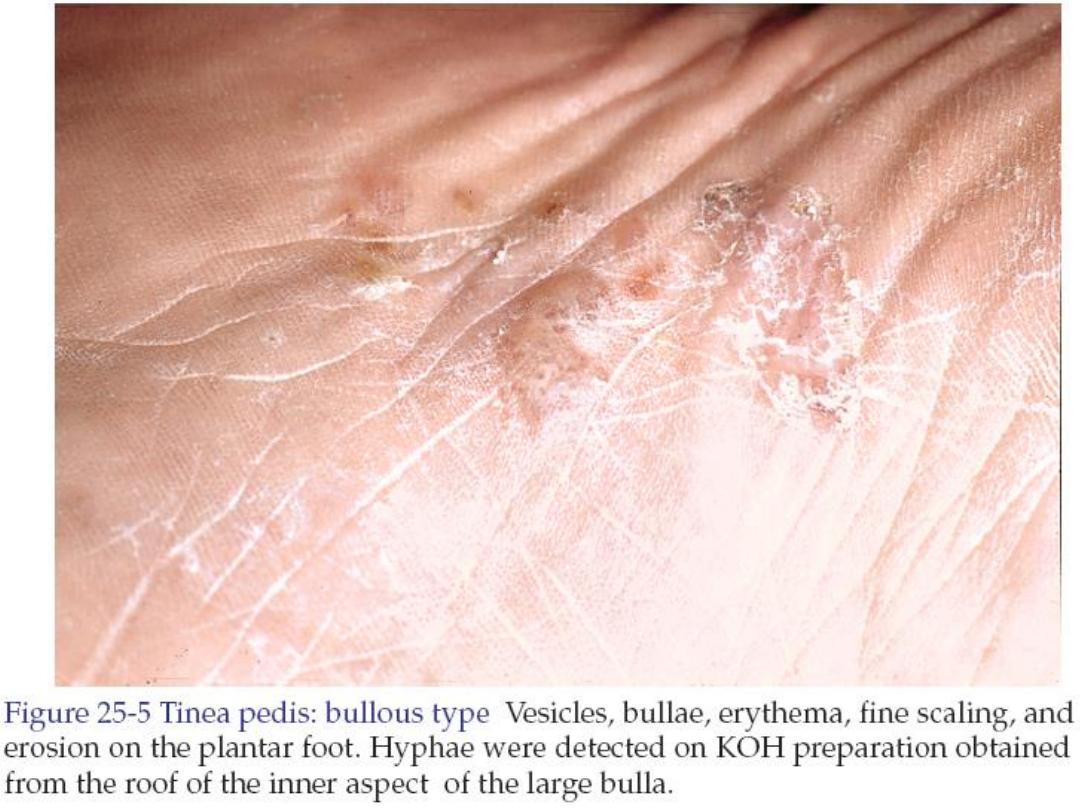
4. Acute vesicular tinea pedis:
is highly
inflammatory infection characterized by
vesicular eruption which may fuse into
bullae. A second wave of vesicles may
follow shortly in the same area or at
distant site such as arm, chest, and along
the sides of the fingers. These itchy
sterile vesicles represent an allergic
response to the fungus and are termed
dermatophytid or id reaction
. They
subside when the infection is controlled.

• Treatment:
– Terbinafine 1% cream (Fungicidal, Lamisil)
applied twice daily for 1 week.
– For moccasin tinea pedis use oral choices:
Fluconazole 50 mg once weekly for 4 weeks,
Itraconazole 200 twice daily for 1 week.
Terbinafine 250mg once daily for 2 weeks.
– Acute vesicular tinea pedis treated by oral
antifungal agents as above. Secondary bacterial
infections treated by antibiotics. Id reaction
treated by topical steroids or prednisone 20 mg
twice daily for 10 days.

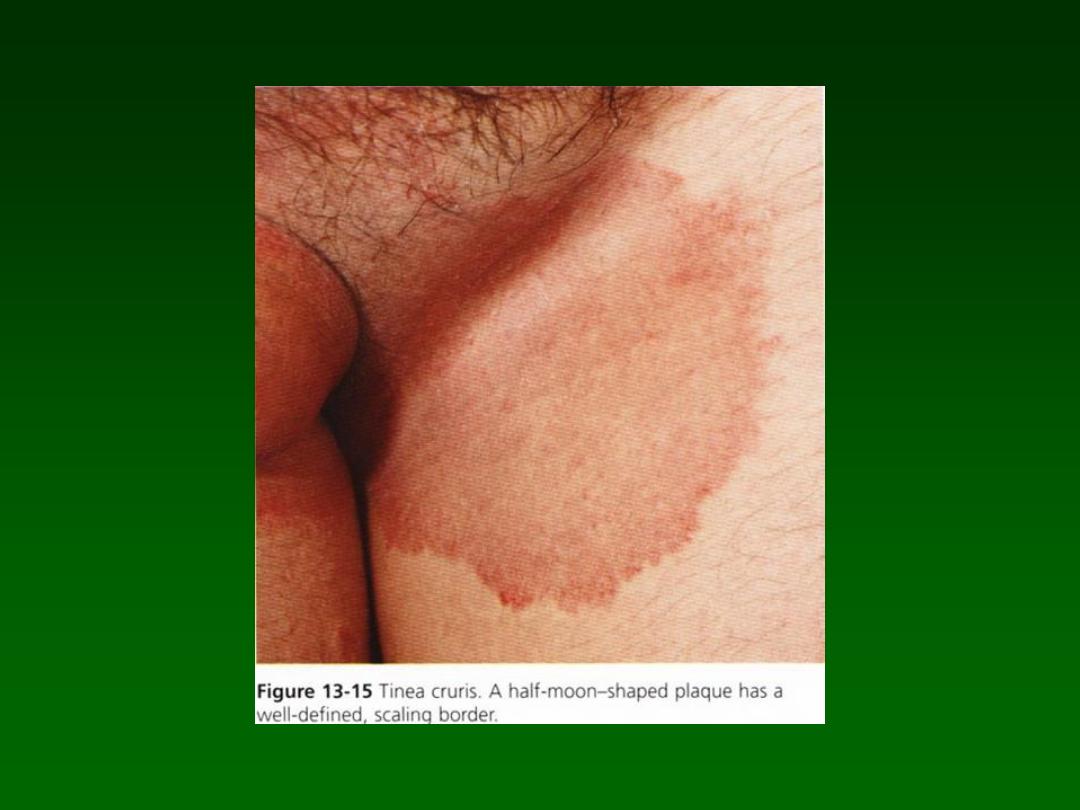
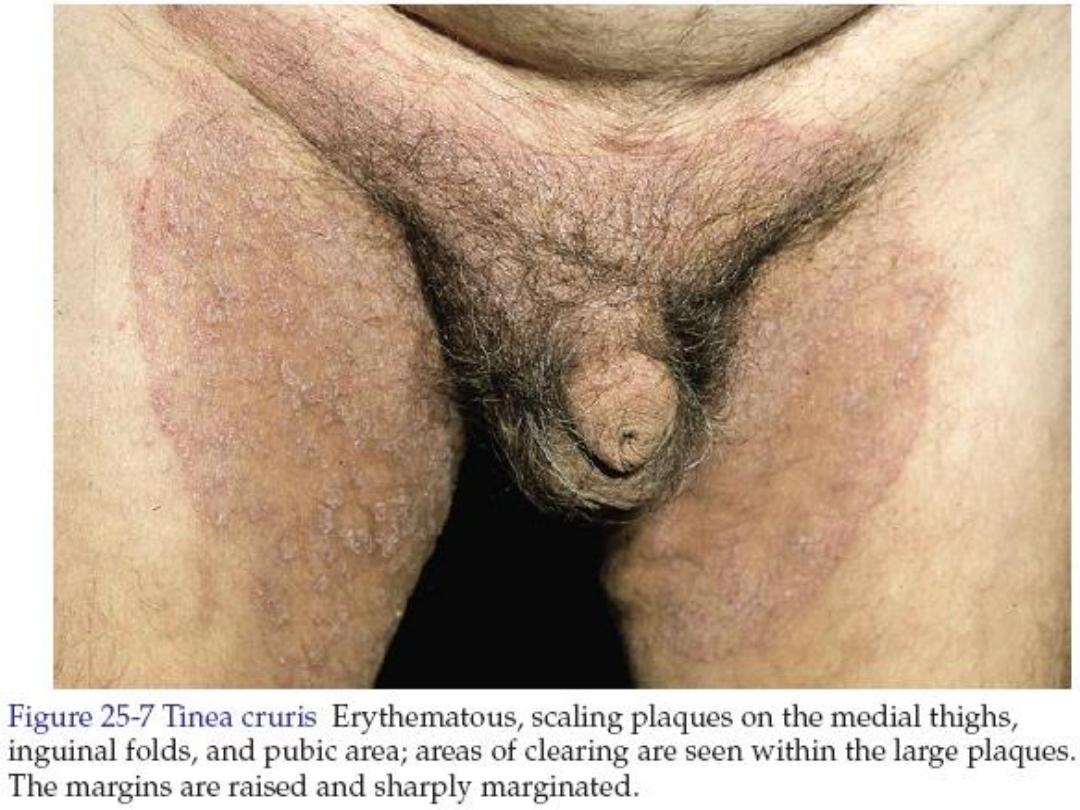
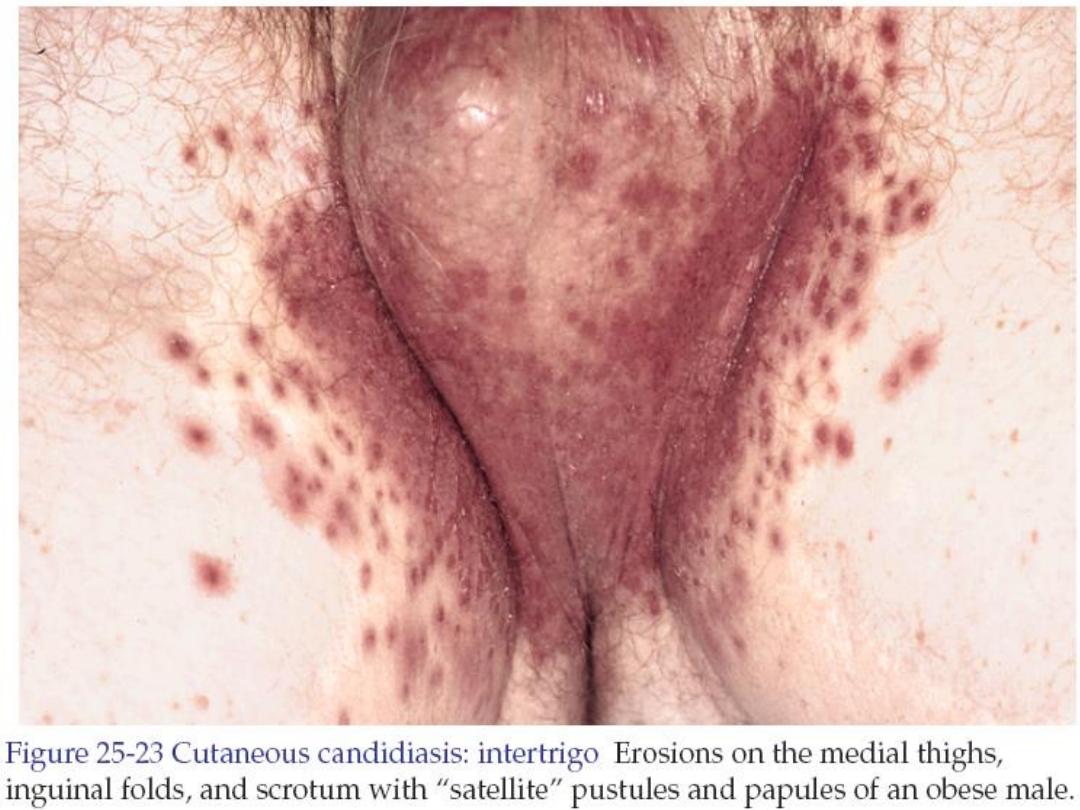
Tinea cruris
• It is tinea of the groin. Common in men.
Rare in children.
• A half moon shaped red brown plaque forms
as a well-defined scaling, and sometimes a
vesicular border, advances out of the crural
fold onto the thigh.
• Itching is common.

• Involvement of the scrotum is unusual. Unlike
candida in which scrotal involvement is
common and bilateral involvements is common
and there is typical fringe of scales at the
border and satellite papules and pustules.
• Differential diagnosis: intertrigo, erythrasma.

• Treatment:
– Terbinafine 1% cream (Fungicidal, Lamisil)
applied twice daily for 1 week.
– Oral choices:
• Fluconazole 150 mg once weekly for 2-4
weeks.
• Itraconazole 100 mg twice daily for 1 week.
• Terbinafine 250mg once daily for 1-2 weeks.

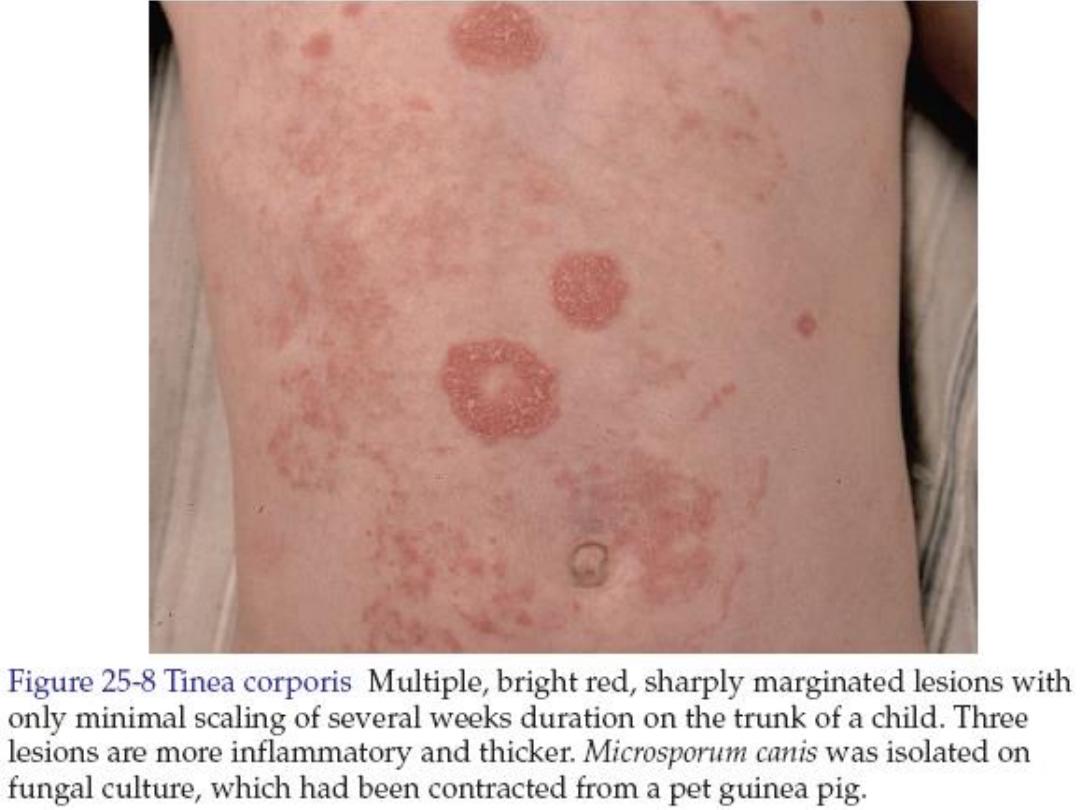
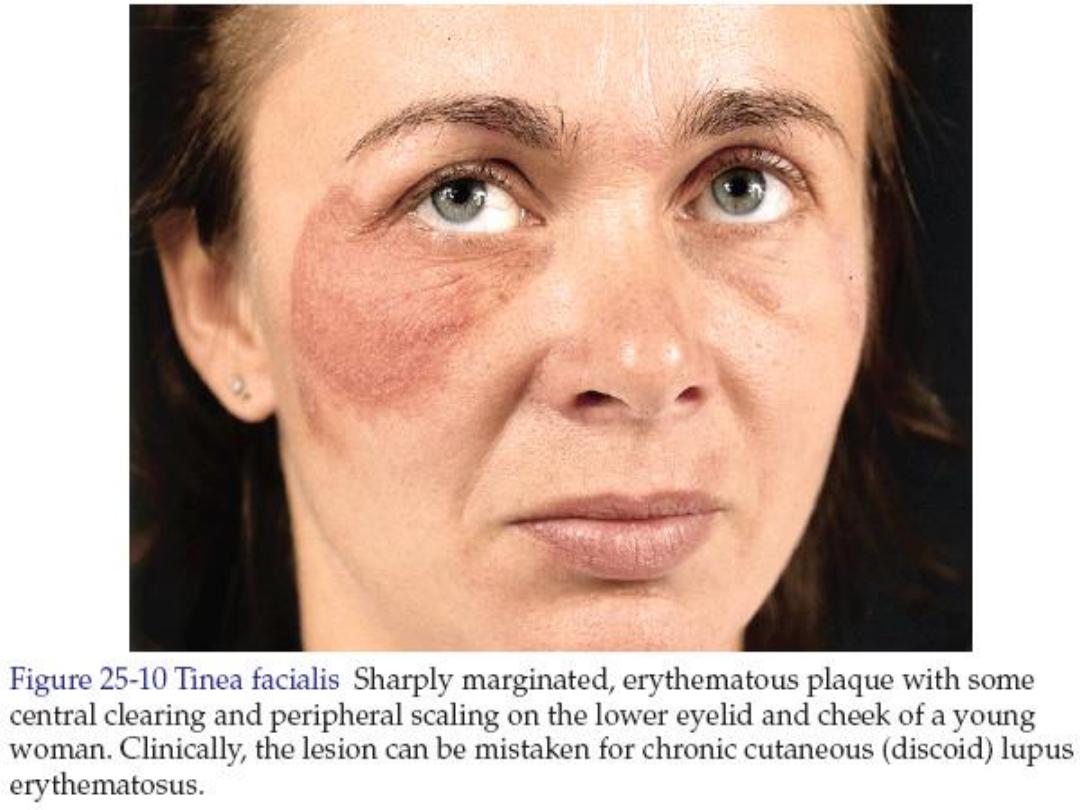
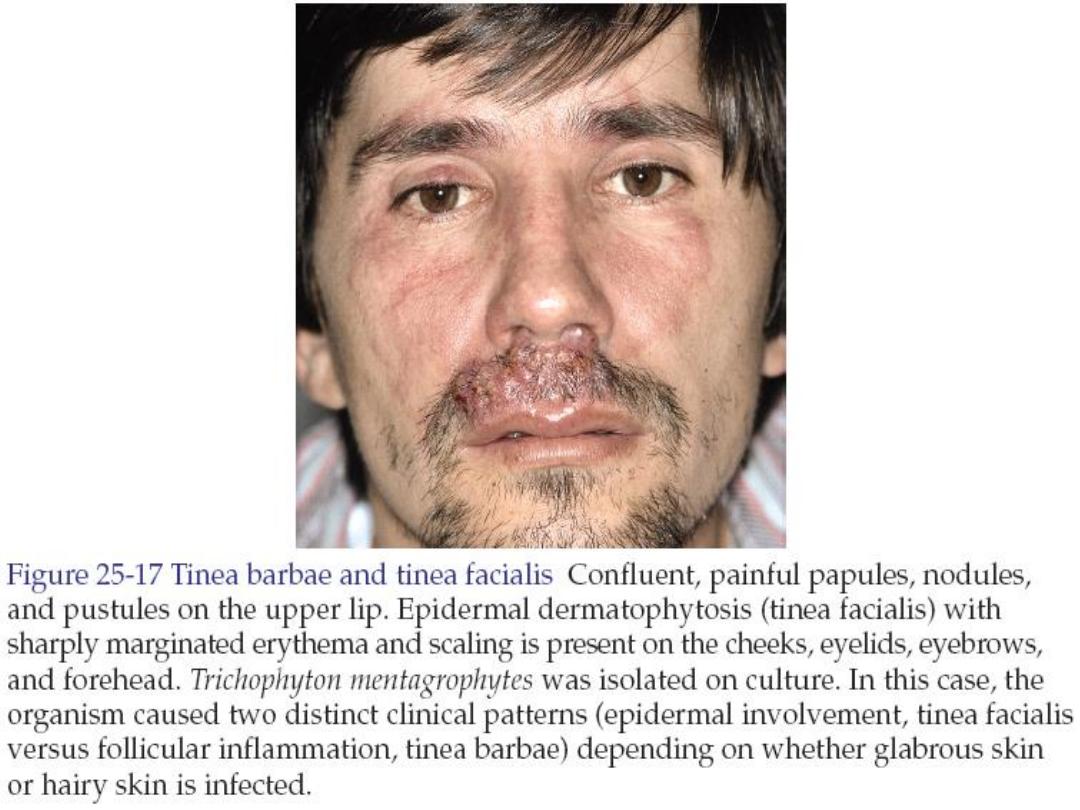
Tinea corporis
• It is tinea of the trunk, limbs and the face
excluding the beard and mustache areas in
men. It is present as round annular lesion as
described previously in classical presentation.
• Treatment: as tinea cruris.


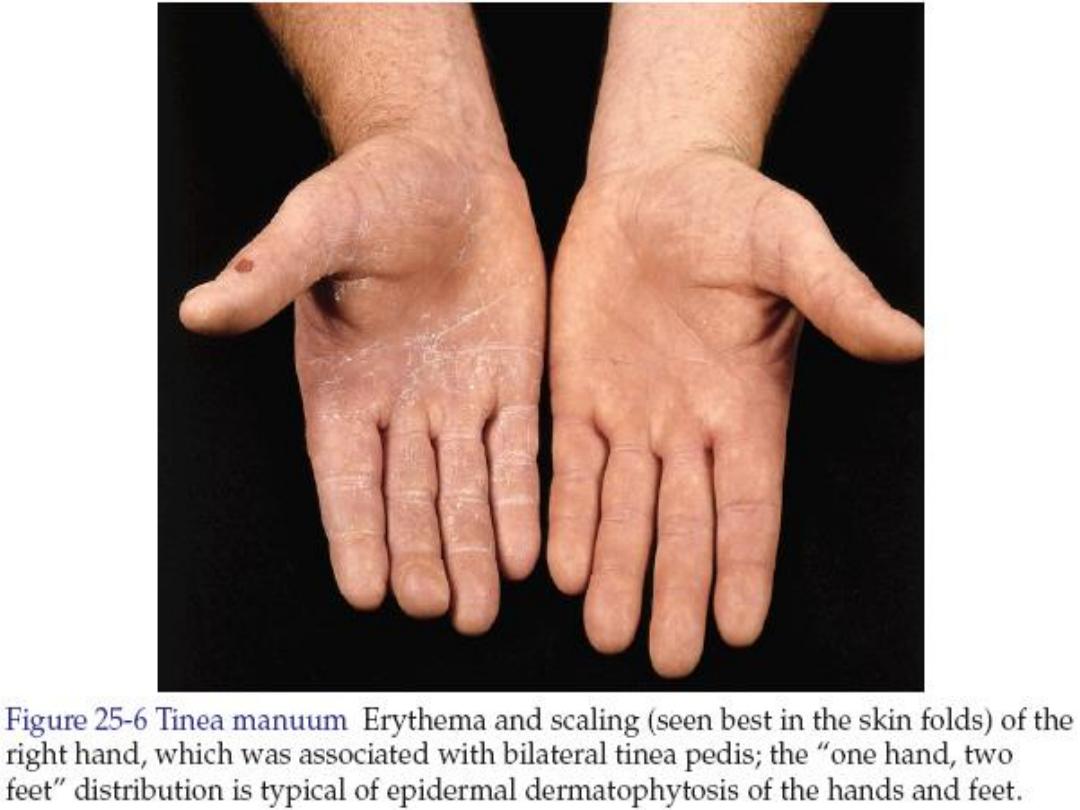
Tinea manum
• It is tinea of the hand. Tinea of the dorsal
aspect of the hand is similar to tinea
corporis. Tinea of palmar surface has the
same appearance as the dry diffuse
hyperkeratotic form of tinea of the sole.
Tinea of the palm is frequently associated
with tinea pedis. Finger nails infection also
a frequent accompaniment.
• Treatment: as tinea cruris.

Tinea capitis
• It is tinea of the scalp. It occurs frequently in
children between 3-7 years of age. Clinically
there is cervical or occipital lymphoadenopathy.
• Fungal infection is rarely the cause when
neither adenopathy nor alopecia is present.

Clinical types of tinea capitis
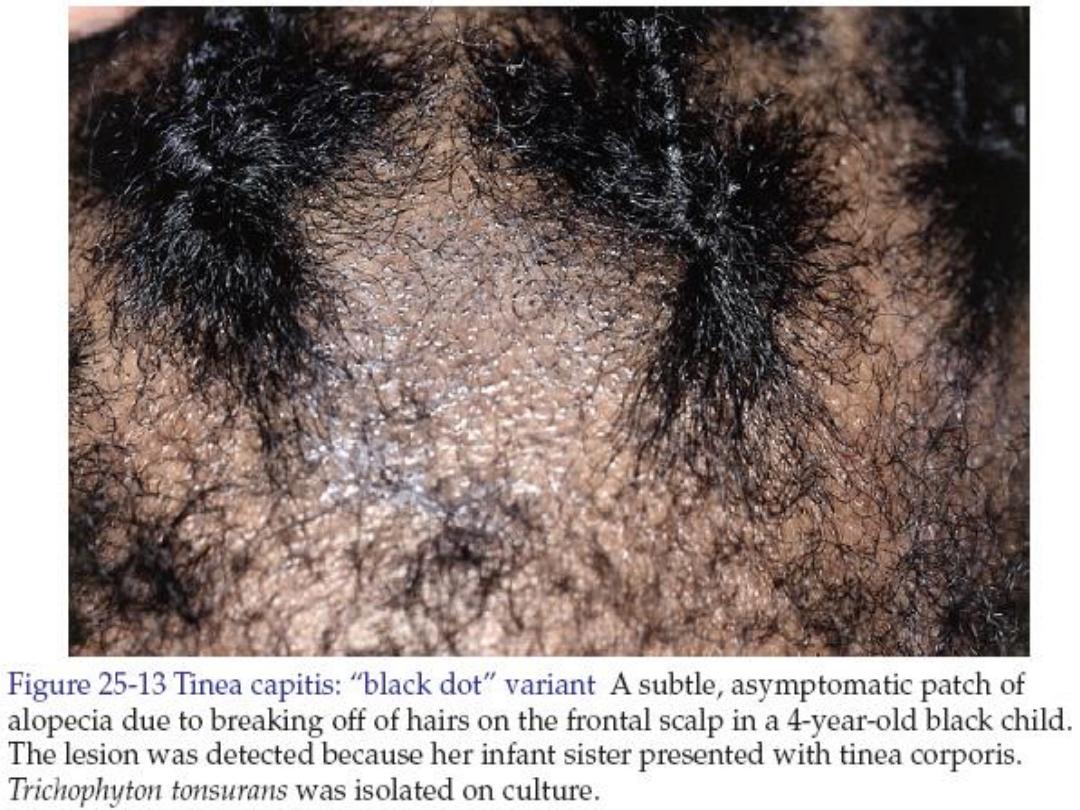
1. Non-inflammatory black dot pattern:
there
is area of hair loss with hairs broken off at
the follicular orifice give the appearance
of black dots.
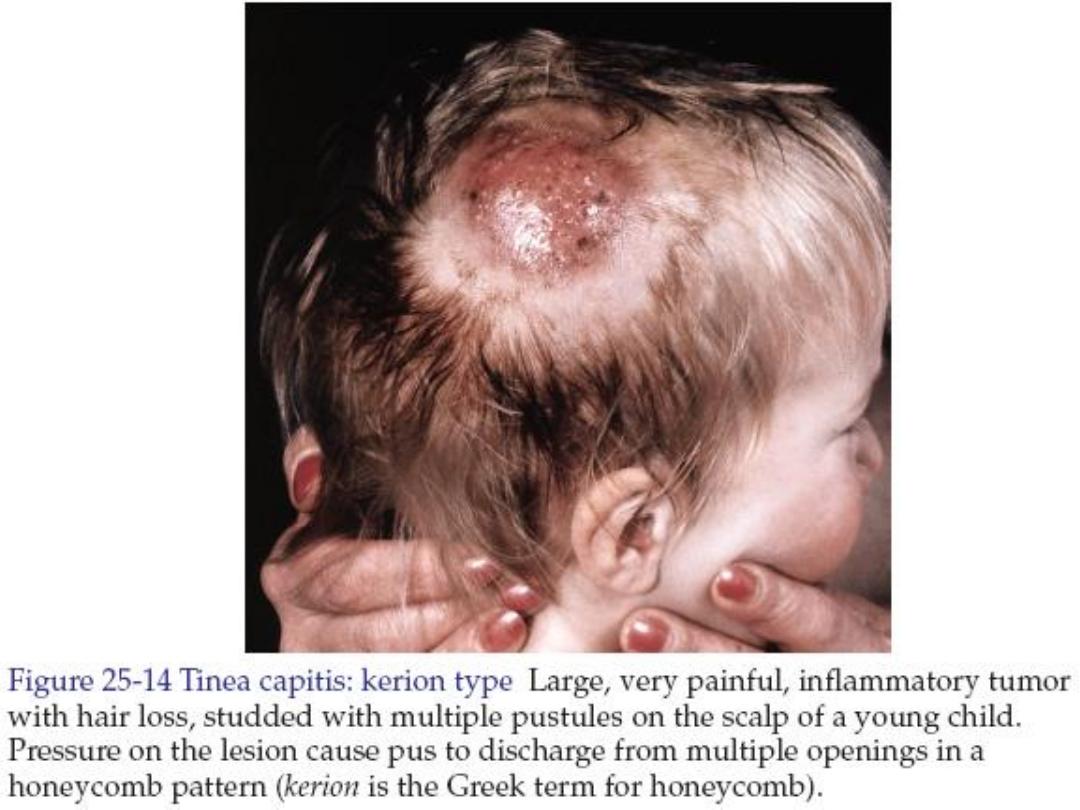
2. Inflammatory tinea capitis (kerion):
there
are one or multiple inflamed boggy tender
areas of alopecia with pustules on and/or
in surrounding skin. The condition leads
to scarring alopecia if not treated
promptly.

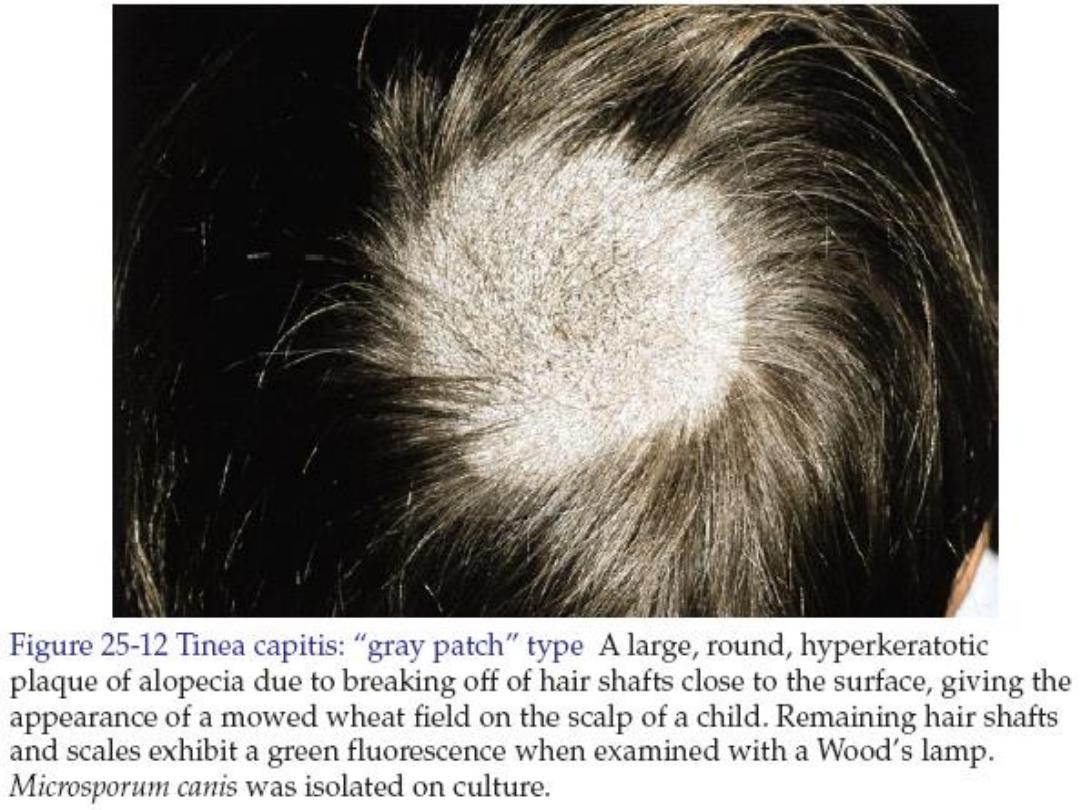
3. Seborrheic dermatitis like (grey patchy) type:
there is
diffuse or patchy fine white adherent scales on the
scalp. There are tiny perifollicular pustules and/or
hair stubs of broken hair.
4. Pustular type:
there are discrete pustules or scabbed
area without scaling or significant hair loss.
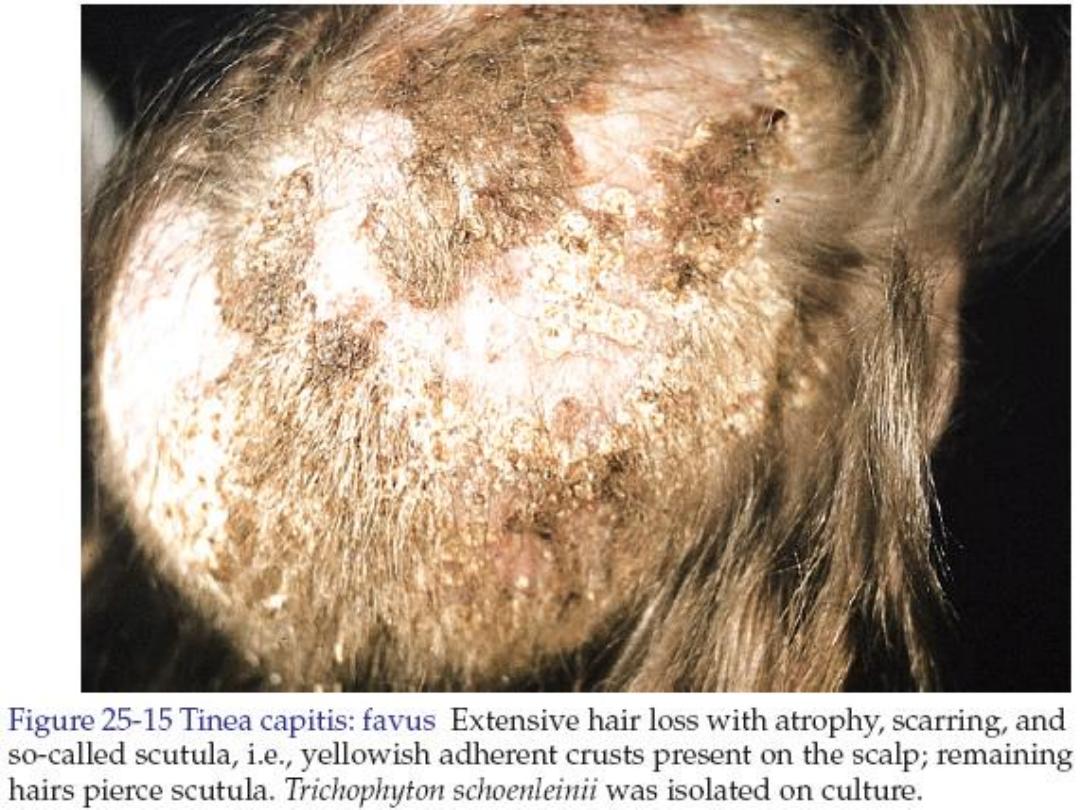
5. Favus:
is infection of the scalp with Trichophyton
schoenleinii. The infection characterized by the
presence of yellowish cup-shaped crusts known as
scutula. Each scutulum develops round a hair.
Adjacent crusts enlarge to become confluent and
form a mass of yellow crusting. The condition leads
to scarring alopecia if not treated early and promptly.

• Treatment options: is always systemic.
• Griseofulvin 15-25 mg/kg/day for 2 months.
Side effects are headache, GI upset and
photosensitivity. The drug is well absorbed after
fatty meal.
• Fluconazole (Diflucan) 8 mg/kg once weekly for
4-16 weeks.
• Terbinafine (Lamisil) 20-40 kg body weight: 125
mg daily 2-4 weeks, >40 kg body weight: 250
mg daily 2-4 weeks.

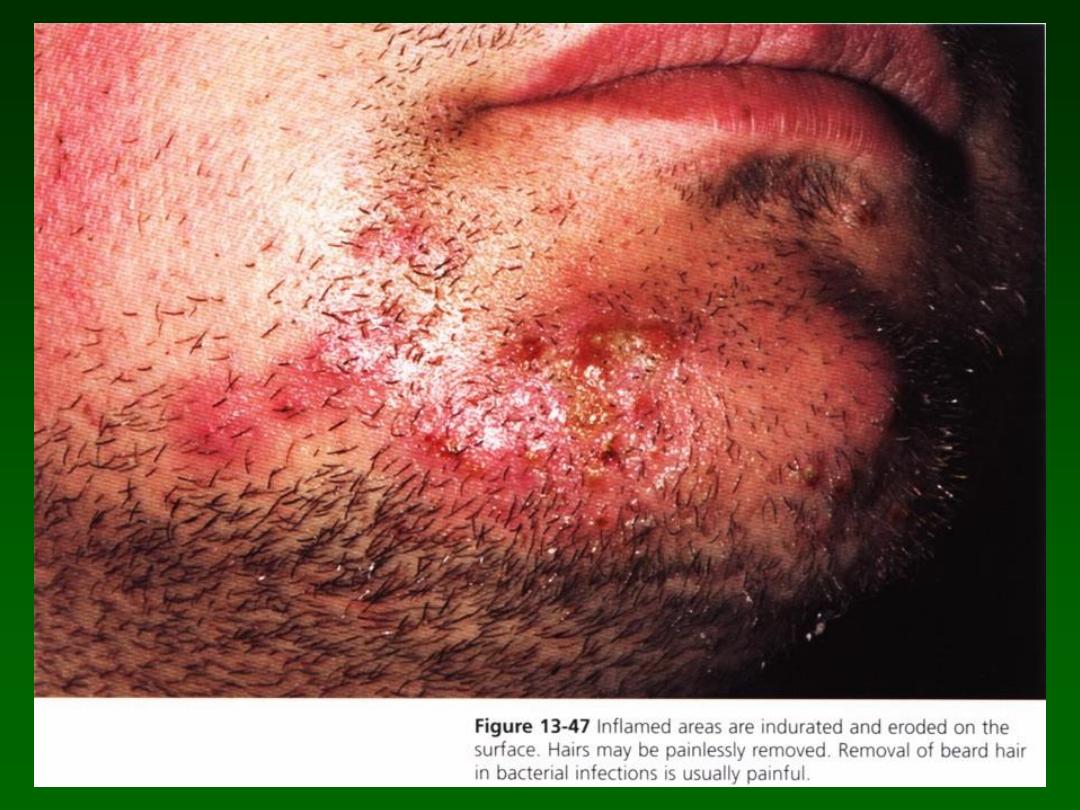
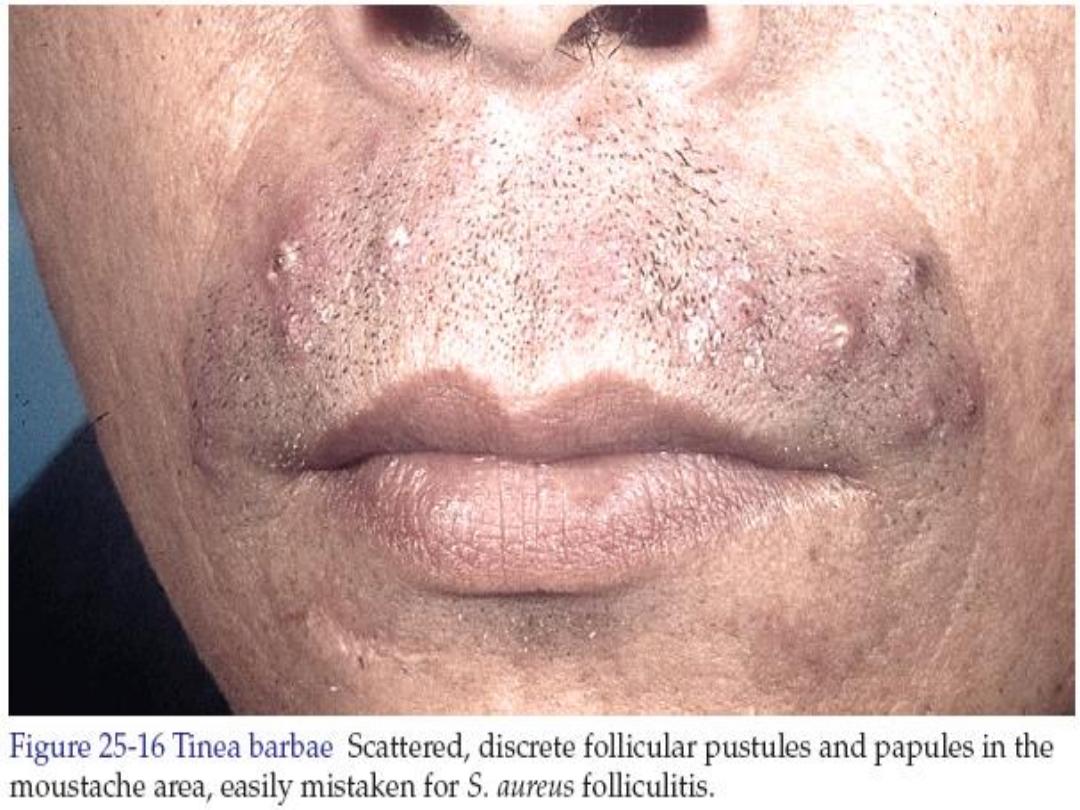
Tinea barbae
• It is fungal infection of the beard and mustache
areas. Like tinea capitis, the hairs are always
infected and easily removed. The hair in
bacterial folliculitis resist removal (or painful on
removal). Tinea begins with small group of
follicular pustules. The process become
confluent in time with development of a boggy
erythematous kerion with dense superficial
crust.
• Treatment: is similar to tinea capitis.

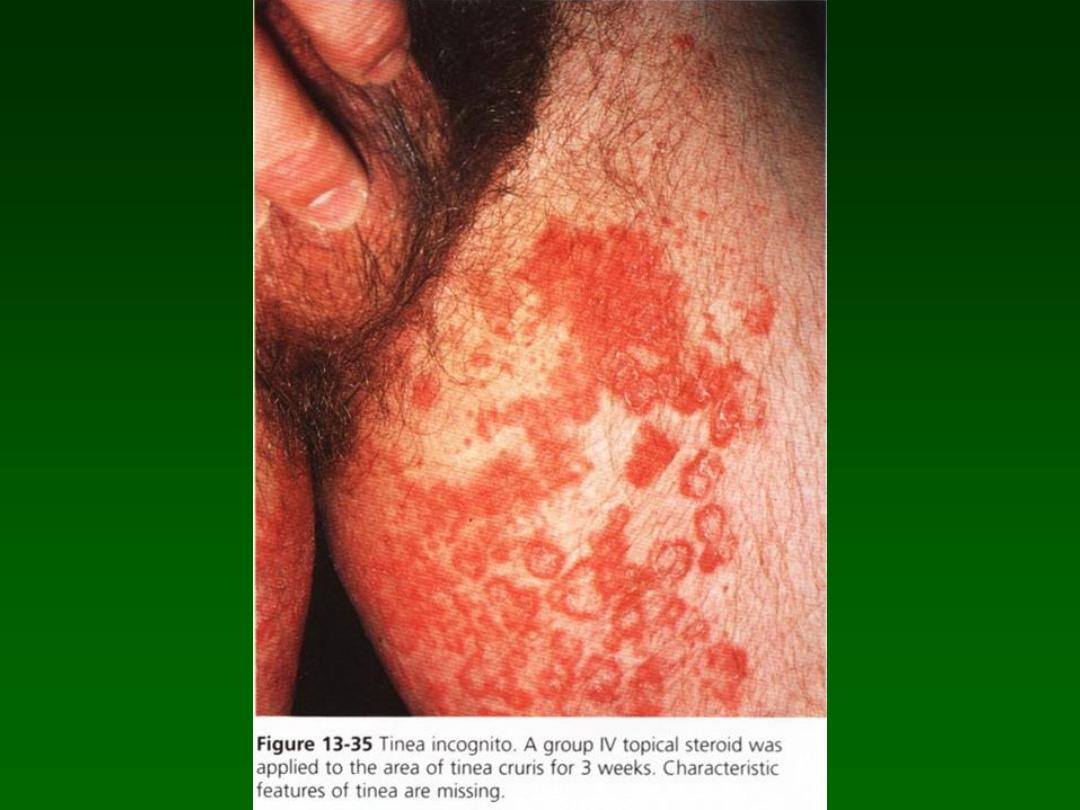
Tinea incognito
(steroid modified tinea)
• It is a condition caused by wrong
treatment of fungal infection with topical
steroids. Topical steroids lead to
disappearance of sings and symptoms
(masking the infection) but the fungus is
actually flourishing. Once the steroids is
stopped the disease reappears and may
even become more extensive and severe.

Candidiasis (Moniliasis)
• The yeast like fungus Candida albicans and few
other candida species are capable of producing
skin, mucous membrane and internal infections.
• The organism lives with the normal flora of the
mouth, vaginal tract and the gut.
• Pregnancy, oral contraception, antibiotic
therapy, diabetes, skin maceration, topical
steroid therapy, certain endocrinopathies and
factors related to depression of cell mediated
immunity may allow yeasts to become
pathogenic.

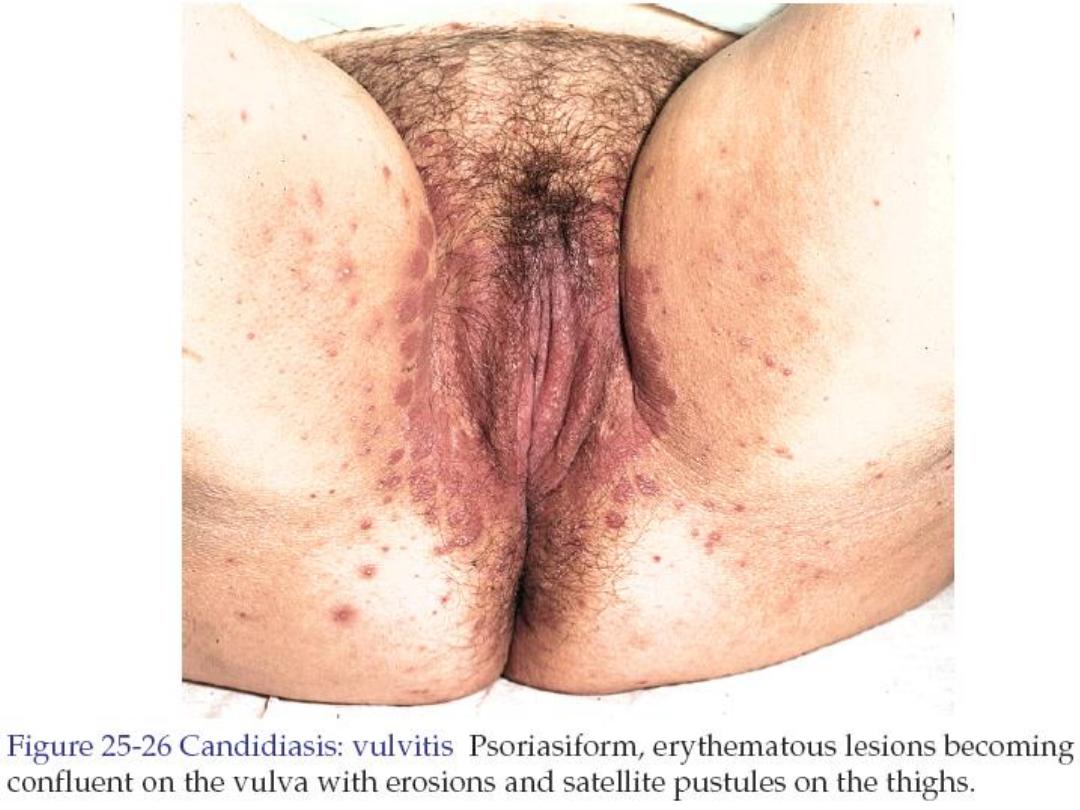
Monilial vulvovaginitis
• The female present with vaginal itching
and/or white thin to creamy discharge.
• Treatment is by miconazole intravaginal
cream or suppositories.
• Fluconazole 150 mg single oral dose.

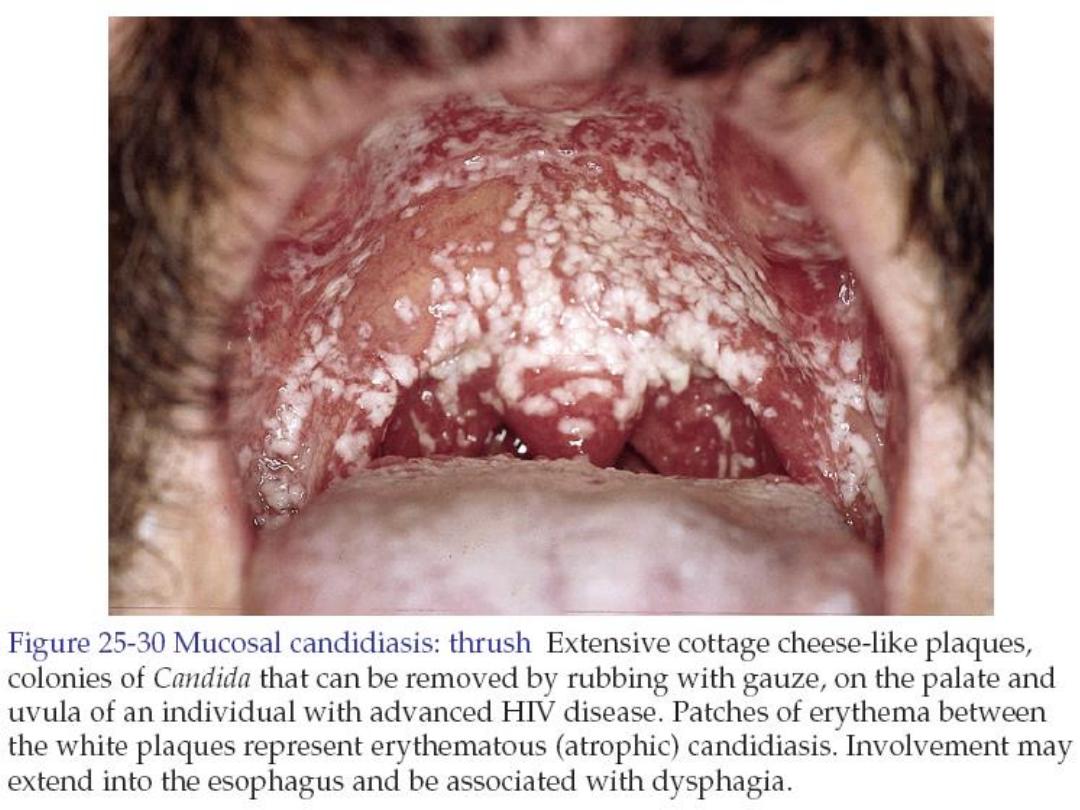
Oral candidiasis (thrush)
• Candida albicans can be transmitted to the infants oral
cavity during passage through the birth canal. Present
as white creamy exudates or white flaky adherent
plaques. In adult it is common in diabetics, depressed
cell mediated immunity, elderly, cancer, prolonged
corticosteroid therapy, immunosuppression, broad
spectrum antibiotic, inhalant steroid. The presentation
is similar to that in infants.
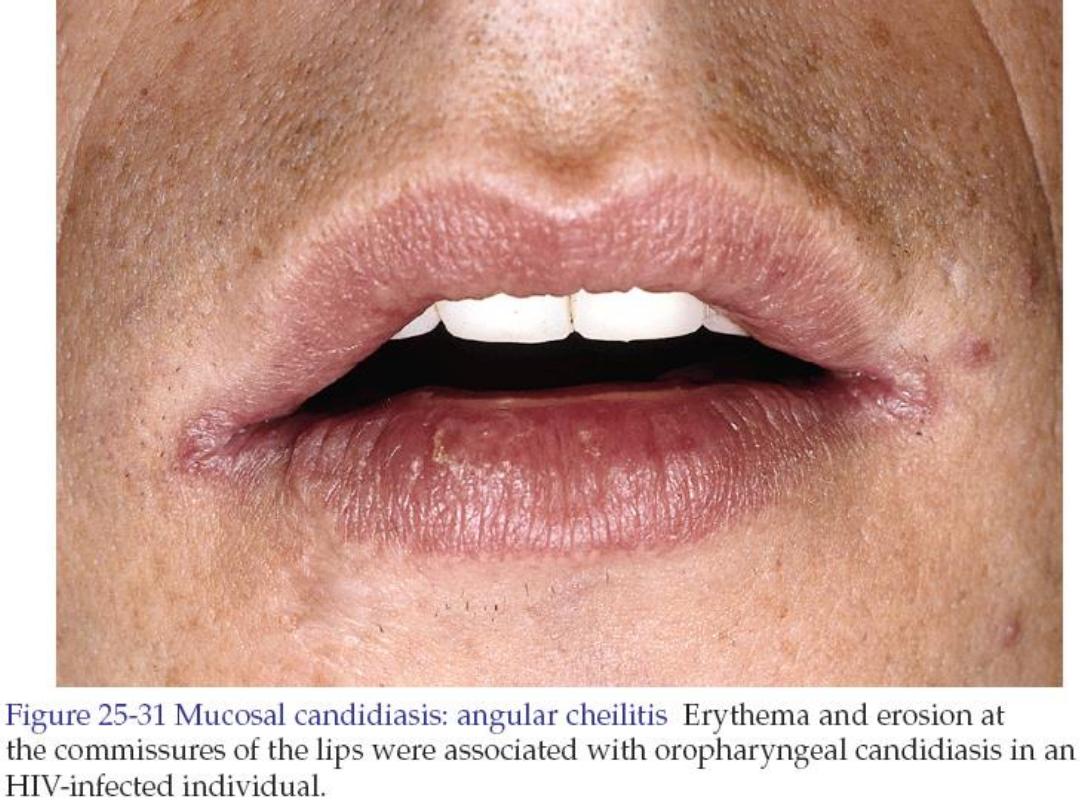
• It may spread onto the skin at the angle of the mouth
(perleche).
• Treatment is by oral nystatin suspension, or
clotrimazole troche, or miconazole oral gel.

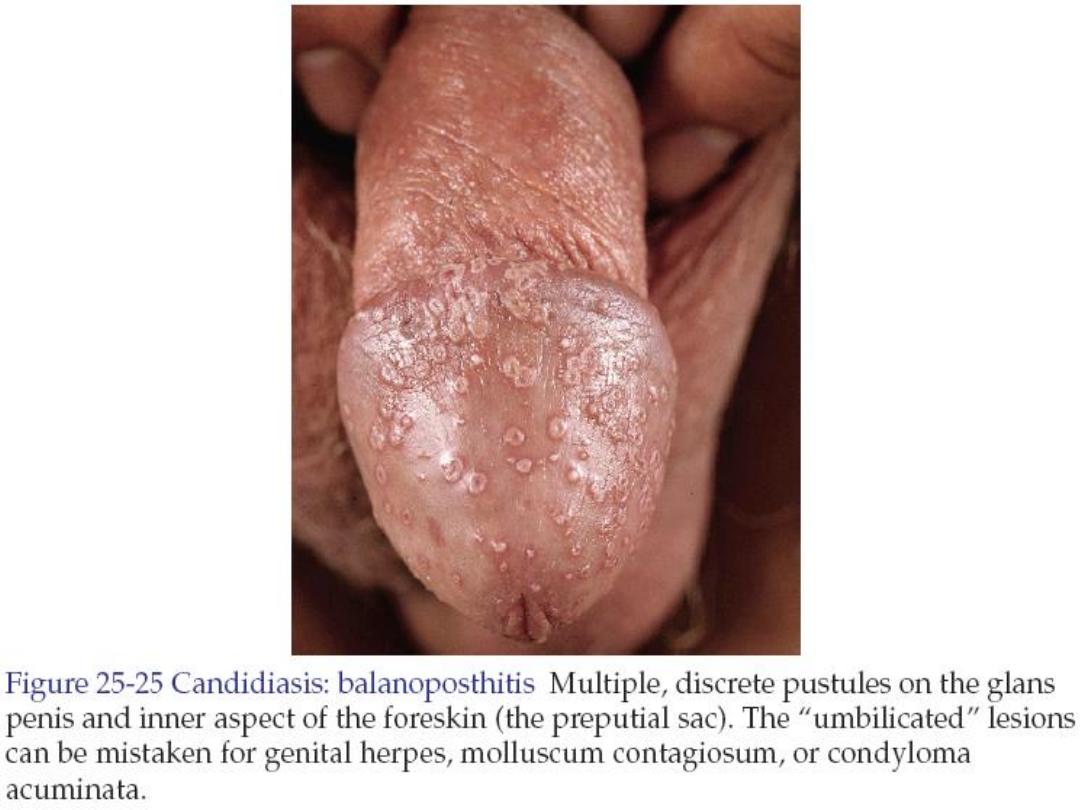
Candida balanitis
• It is common in uncircumcised penis which
provides the warm, moist environment.
Tender pinpoint red papules and pustules
appear on the glans and shaft of penis,
white exudates may be present.
• Treatment is by miconazole cream twice
daily for 7 days. Or single oral fluconazole
150mg capsule.

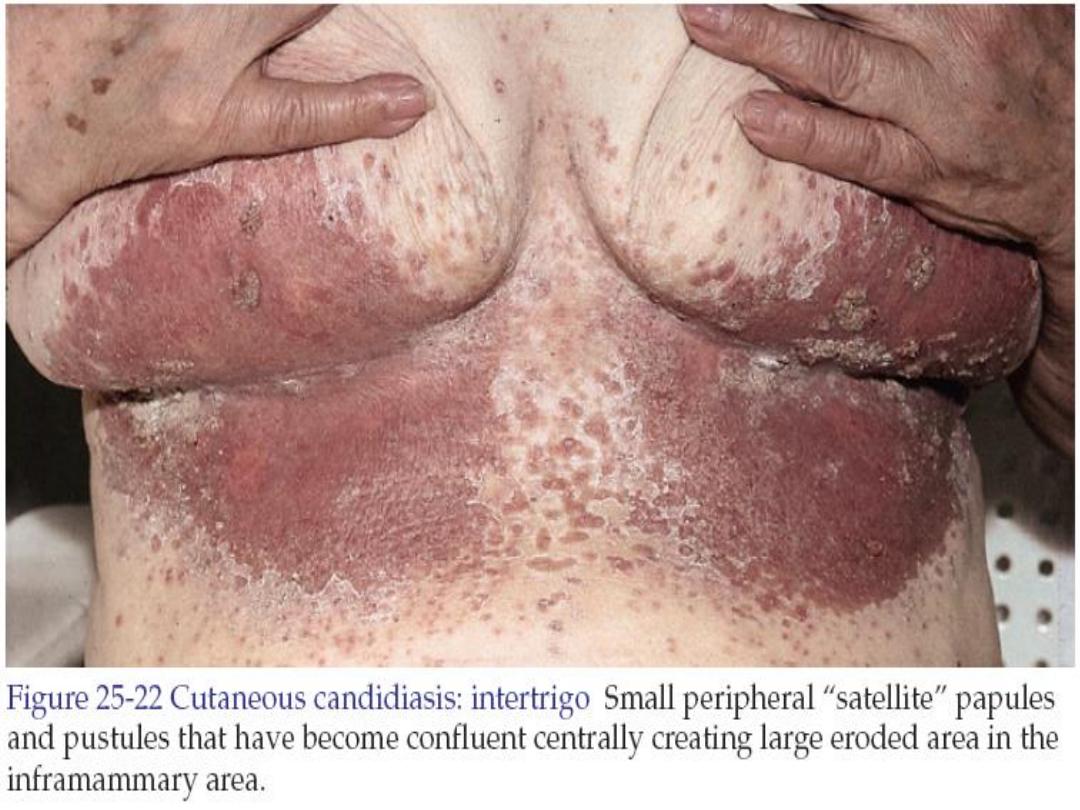
Candidiasis of the skin folds
(Candida intertrigo)
• Occurs under pendulous breasts, between
overhanging abdominal folds, in the groin and gluteal
area and axillae that have heat and moisture.
(Intertriginous areas are areas where skin touches
skin).
• Clinically there are macerated pustules and papules
under apposing skin surfaces with fringe of moist
scale at border. Intact pustules or papules found
outside the apposing skin surfaces, this is an
important diagnostic sign called
satellite lesions
. Also
the presentation may be as red moist glistening
plaque that extends to or just beyond the limits of
apposing skin folds.
• Treatment by maintaining dryness. Miconazole topical
cream twice daily until rash clears.

Diaper candidiasis
• An artificial intertriginous area is created under
wet diaper, predisposing the area to a candida
infection with the characteristic red base and
satellite pustules and papules.
• Treatment: dryness should be maintained by
changing the diaper frequently. Miconazole
antifungal cream should be applied twice daily
until the rash clears. Irritation treated with 1%
hydrocortisone cream alternately with the
antifungal cream.


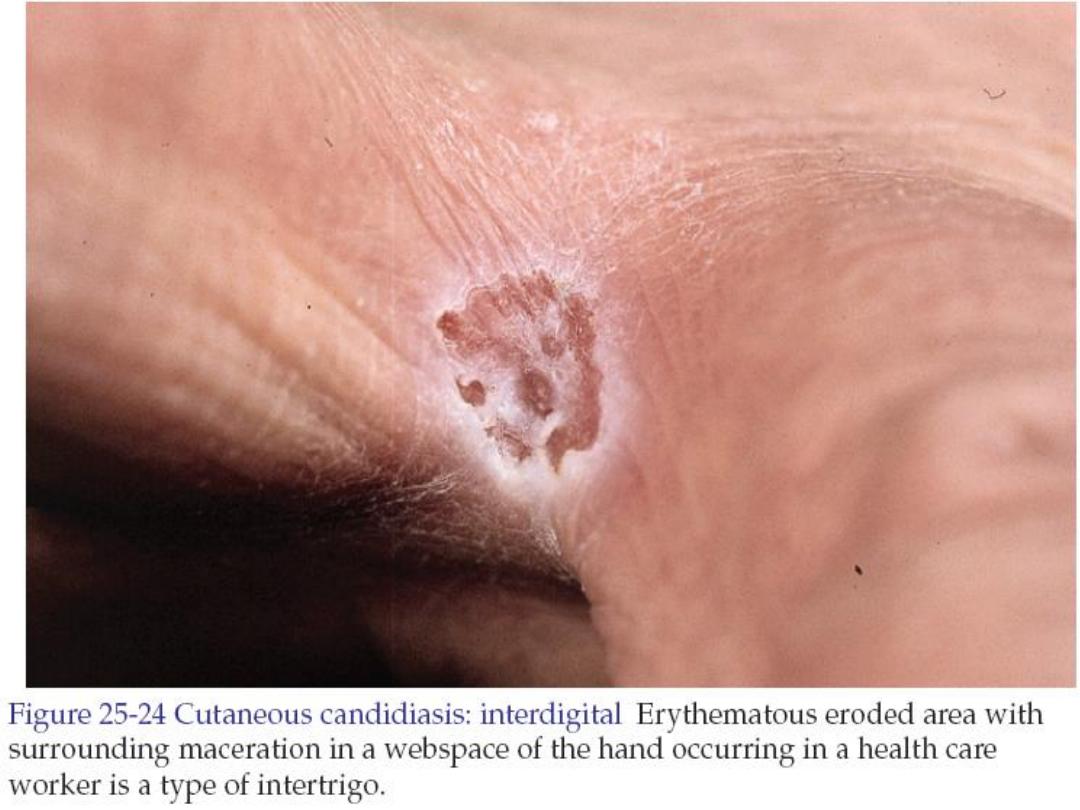
Finger and toe web candidiasis
(interdigital candidiasis)
• Any one who works in moist environment
is at risk like cook, dishwasher.
• White, tender macerated skin erodes
revealing a pink moist base.
• Treatment as above.

Pityriasis versicolor
• It is caused by dimorphic lipophilic yeast
pityrosporum orbiculare (round form) and
pityrosporum ovale (oval form). The
microorganism also called malassezia furfur.

• Lesions begin as multiple small circular
macules and patches of various colors
(white, pink or brown) that enlarge radially.
• The color is uniform in each individual.
• The upper trunk is most commonly
affected site, then the arms, neck and
abdomen.
• The lesions are asymptomatic but may be
itchy.
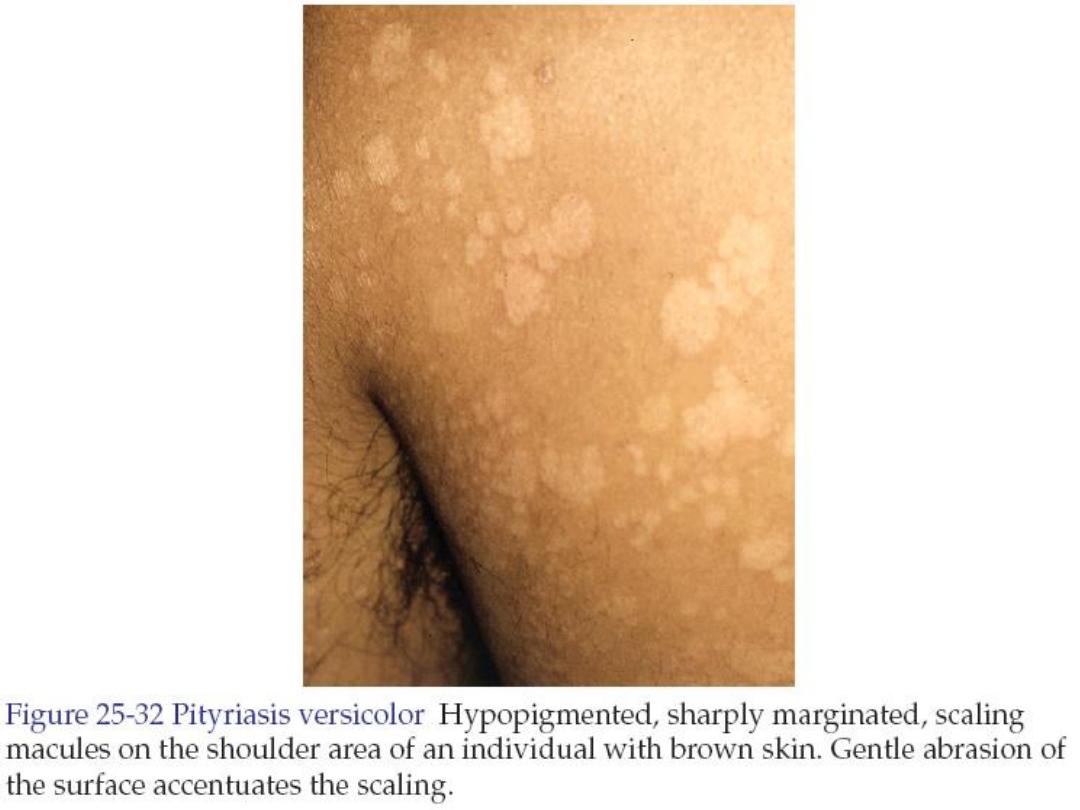
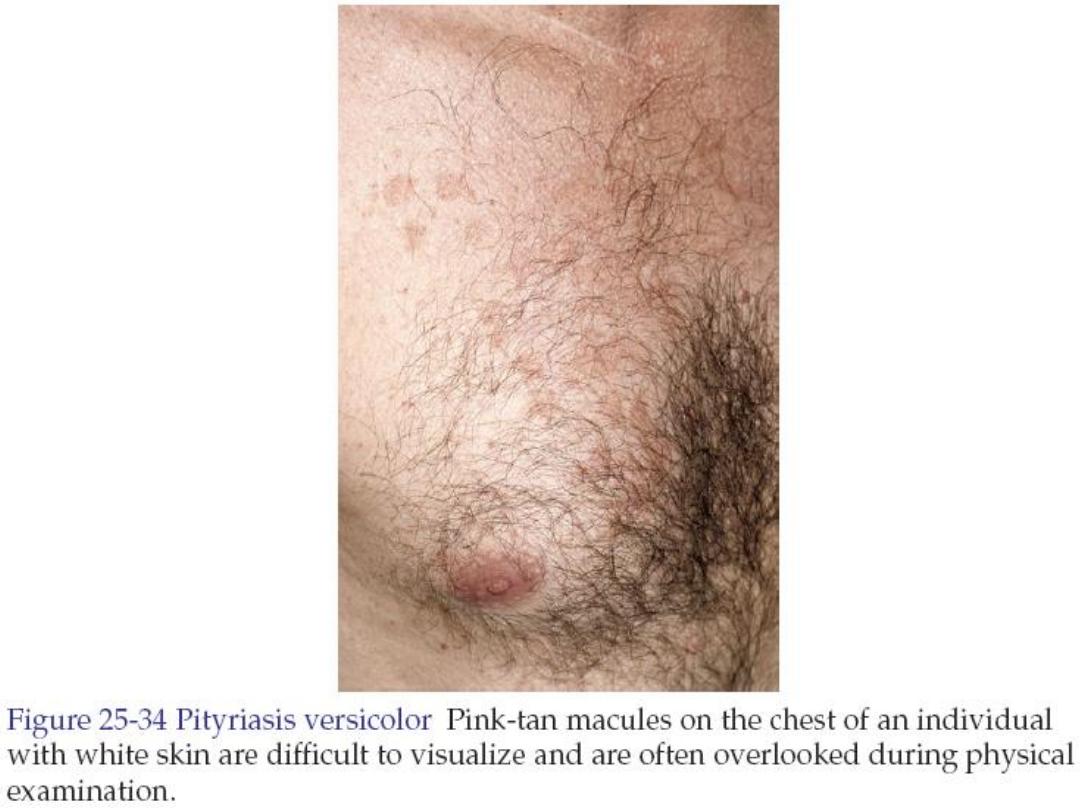

• The differential diagnosis: vitiligo, pityriasis
alba, seborrheic dermatitis, secondary syphilis,
and pityriasis rosea.
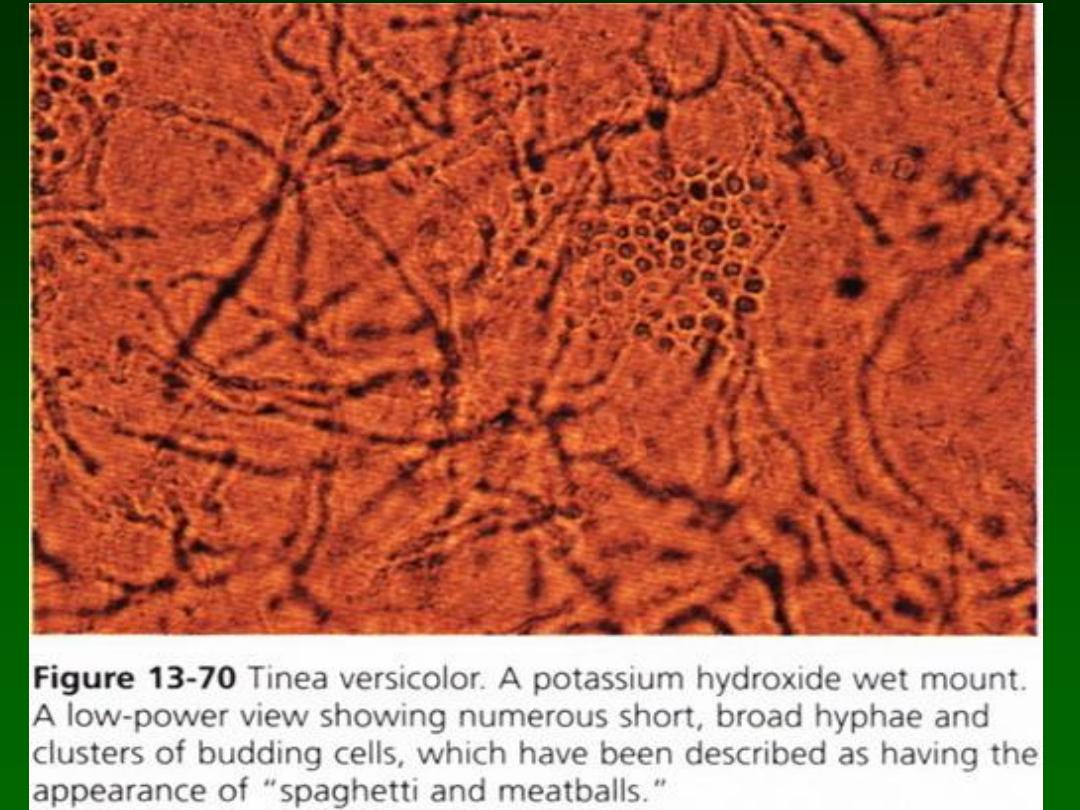
• Potassium hydroxide examination of the scale
shows numerous short hyphae intermixed with
round spores giving an appearance of
spaghetti-and-meatballs pattern.
• Wood’s light examination shows irregular pale
yellow-to-white fluorescence.
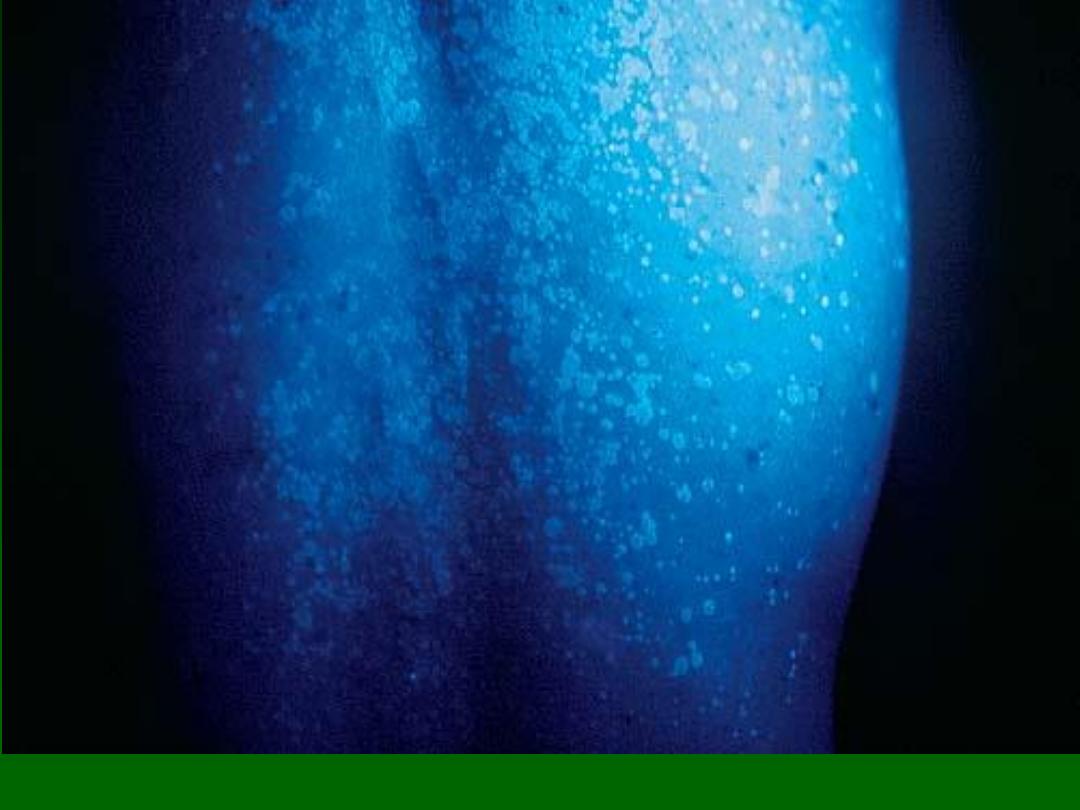
Pale yellow fluorescence on Wood’s lamp examination.

Treatment options
• Ketoconazole shampoo 2% daily application for
3 days.
• Selenium sulfide suspension 2.5% (Selsun)
applied for 10 minutes every day for 7
consecutive days.
• Itraconazole 200mg once daily for 7 days.
• Fluconazole 300mg single oral dose.
• Ketoconazole 400mg single oral dose.
