Supracondylar Fractures
of the HumerusInter-active
Part I
• Basic concepts
• Management of the fractures• The prevention and management of the Complications will be covered in Part II.
In this first part we are going to cover:
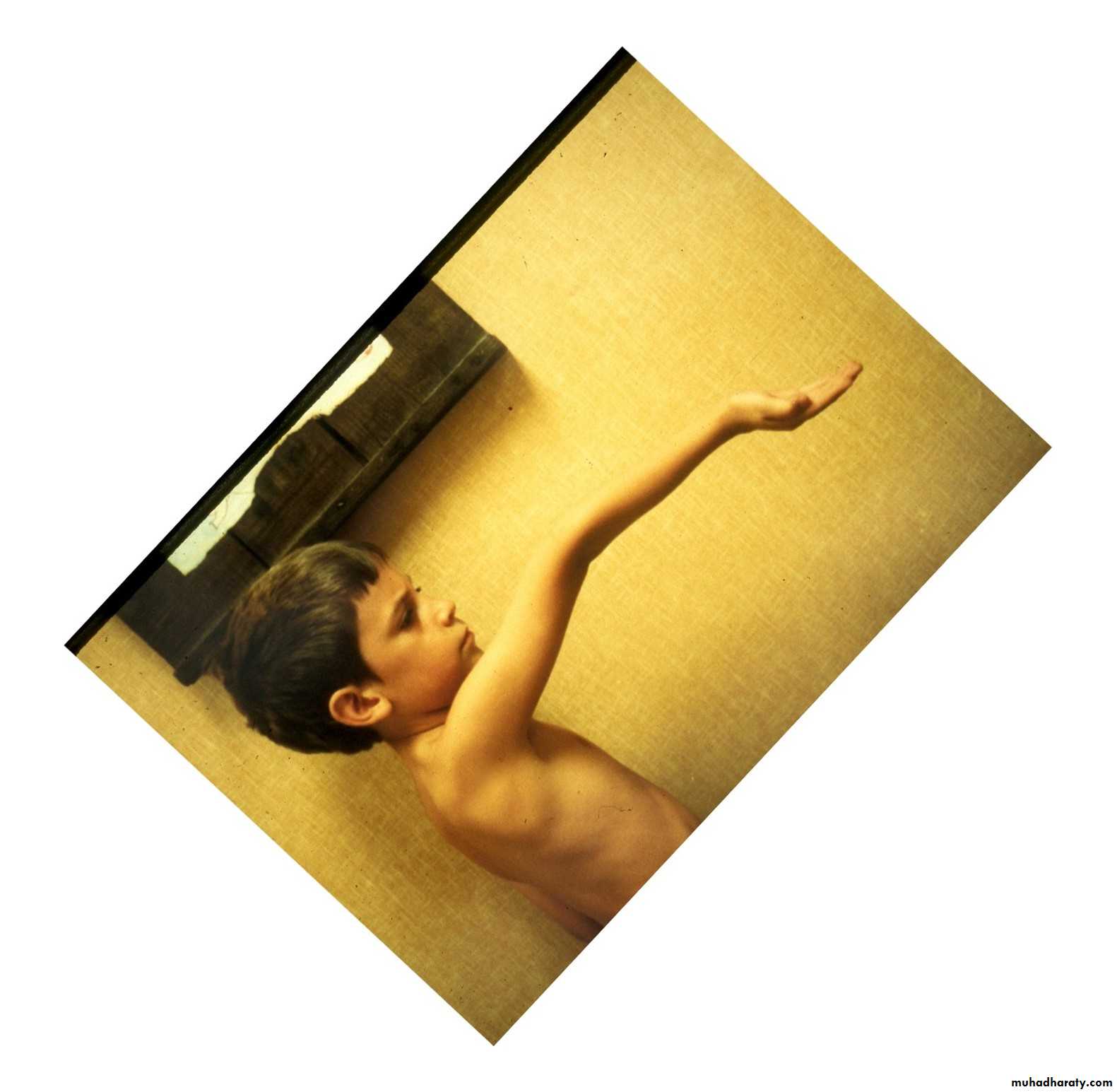
The incidence peaks at
I. IncidenceAt what age do supracondylar fractures
most commonly occur ?
Why?
3 years
7 years.
10 years
That is the age when children reach
their maximum ligamentous laxity.
When a child falls on their extended upper extremity,
which ones are most likely to sustainsupracondylar fractures?
Those who have cubitus recurvatum.
When a child falls on their extended upper extremity,
which ones are most likely to sustaindistal radius fractures?
distal radius fractures?
Those who lack full elbow extension.
Mechanism of Injury
What other factor contributesto the development of
fractures in the supracondylar area?
The supracondylar area consists
of weak metaphyseal bone.
Very thin
corticalstructure
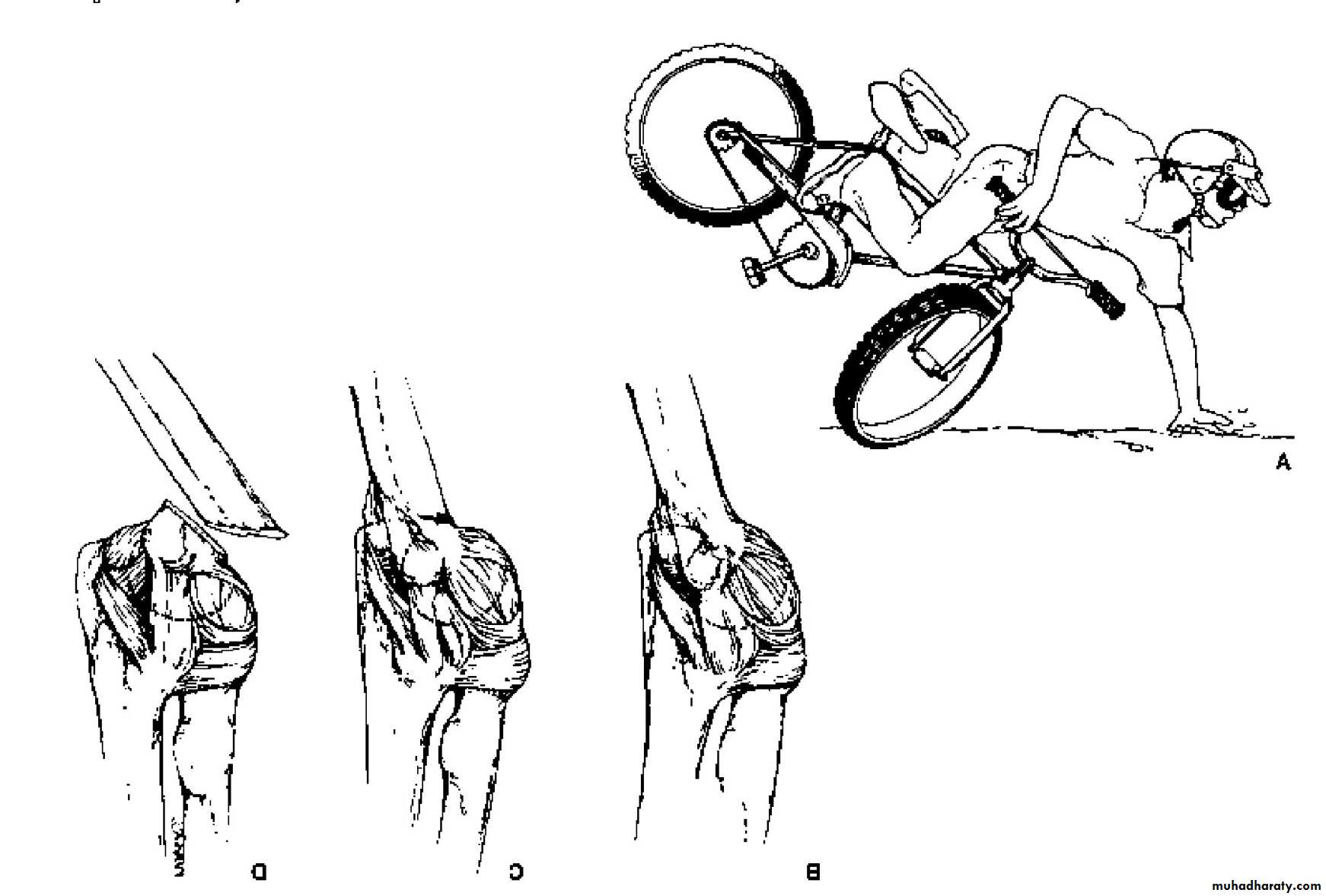
II. Mechanism of Injury
What is the mechanism of injury
for extension type supracondylar fractures ?As the
extended extremityattempts to break
the fall,
the olecranon
is forced
deep into its fossa.
This causes
the humerus to failin the weak metaphyseal
supracondylar area.
Into what two major types are supracondylar
fractures commonly sub-classified?
The extension type is
the
most common type.
What
type ?Exten
sion
III. Classification
What is this less common type?
Flexion
How are the extension type supracondylar
humeral fractures further classified?*
*Gartland,JJ:.
Surg Gynecol Obstet 109:145,1959.
What does his classification represent ?
How are the extension type supracondylar
humeral fractures further classified?His types represent
no more than the
three stages
of displacement.
What are the
three stages
of displacement?
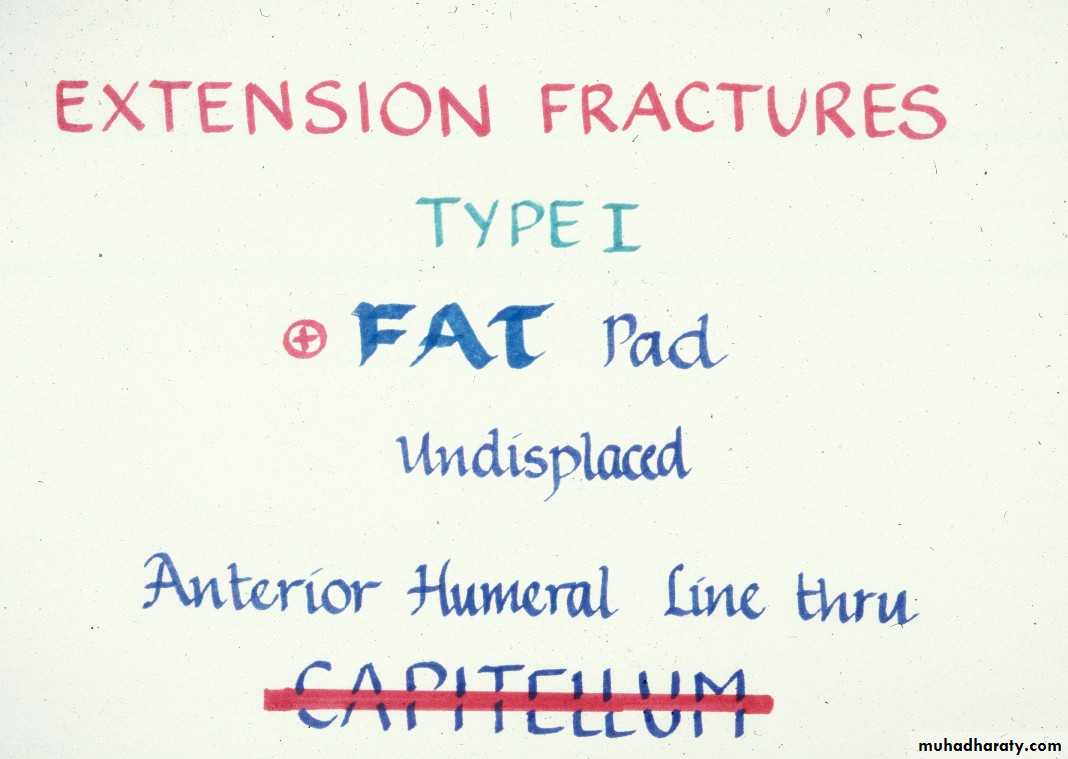
Type I
No displacementType II
Incomplete
displacement
Type III
Complete
displacement
Why all this
emphasison the classification?
It dictates
the
method of
treatment.
*
*Abraham E, Powers T, Witt P, Ray RD
Clin Orthop 171:309, 1982.
Let us examine the treatment
based upon the
Gartland Types.IV. Extension type supracondylar fractures
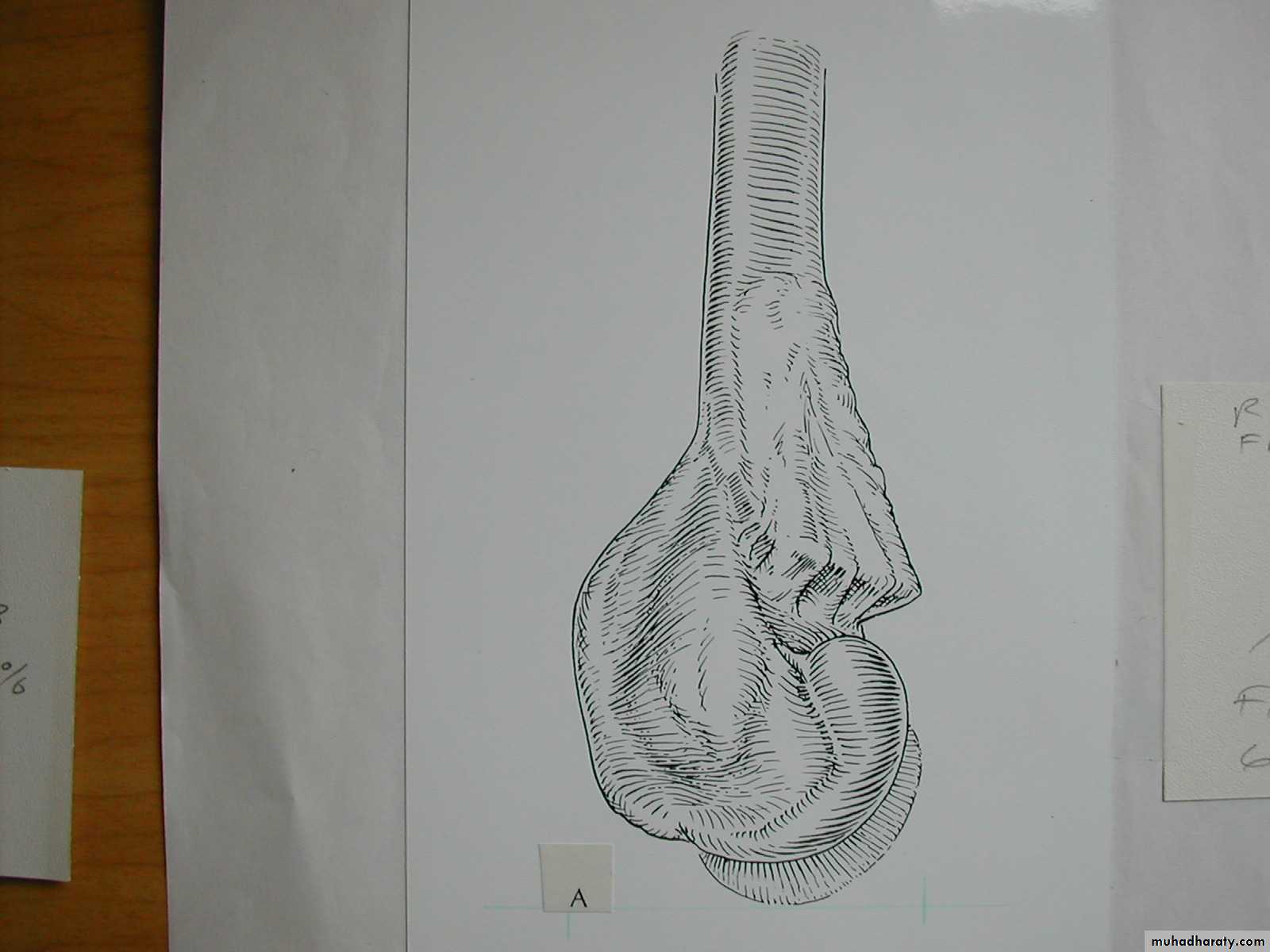
What are the criteria for Type I Fractures ?
+
What are the criteria for Type I Fractures ?
What are the criteria for Type I Fractures ?
What are the criteria for Type I Fractures ?
Absence of
a crescent sign
If there was no definite fracture
seen on the injury films,what confirms the presence
of a suspected Type I fracture?
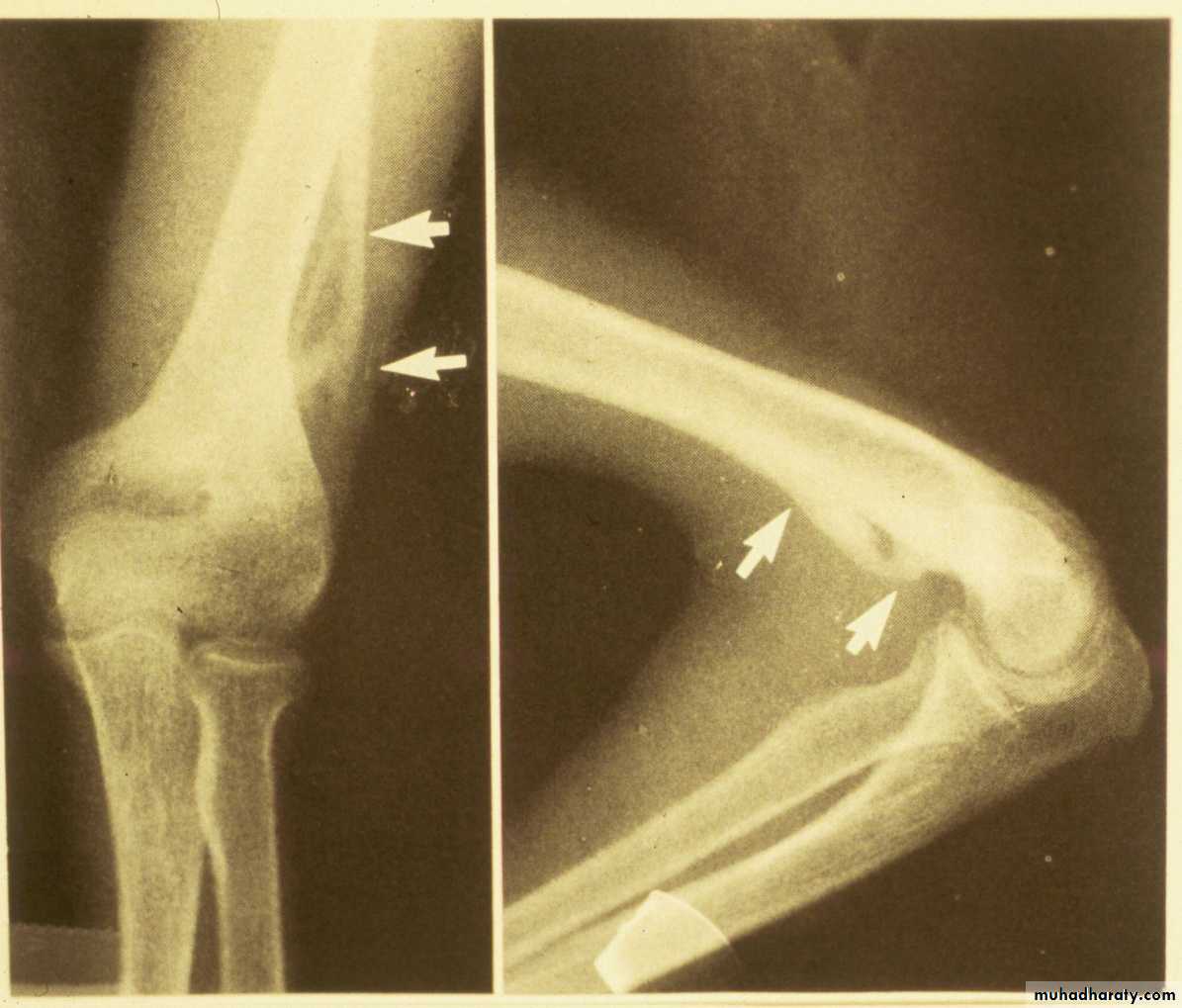
Injury film
3 wks post fracture
fat pads displaced
Type I suspectedPeriosteal new bone
The original suspicions of
a fracture are now confirmed.
How are the Type I
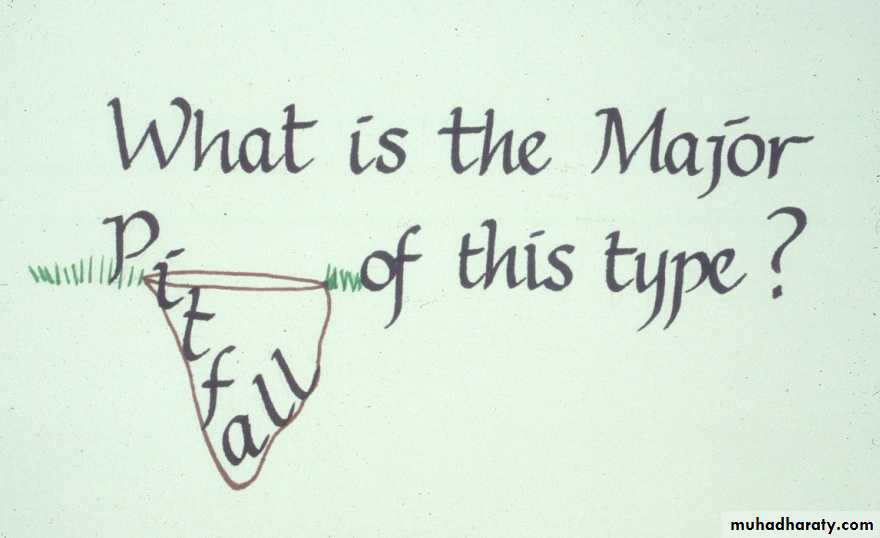
fractures usually treated?Originally felt
to be undisplacedThe major pitfall is
a failure to recognize
the true nature
of the fracture pattern.
What are the two major displacement deformities occurring in Type I injuries ?
1. Medial greenstick collapse
2. Hyperextension of the condyles
This can accentuate the varus.
A more careful evaluationof our original “undisplaced” fracture
reveals both deformities were present
on the original x-rays.
Medial greenstick collapse
+Distal hyperextension
The crescent sign
indicates a varus alignment.
All of this combines to form a
veryunappealing
clinical appearance
How can one avoid this complication?
Is thisacceptable?
Is there varus?
Is the
crescent sign real?
The anterior
humeral line
barely passes
through the
capitellum.
The surgeon needs to perform both
careful x-ray and clinical assessments.
Or is it the result of
a poorly
taken x-ray?
The clinical examination involves
This allows the surgeon to determine thatthe carrying angle has been maintained.
carefully coaxing the elbow into extension.
However, displacement in thesaggital plane may be difficult
to determine clinically.
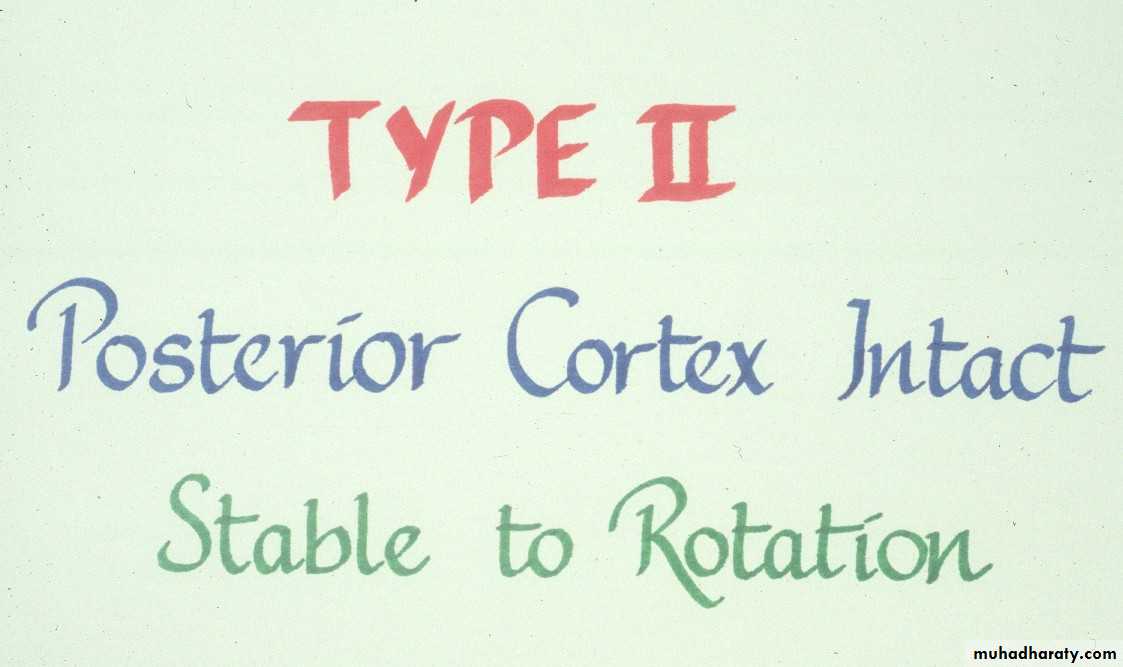
What are the
criteria for
Type II fractures ?
Usually some
cortical
integrity
remains.
This integrity must
be sufficient
to prevent rotation
of the distal
fragment.
How must Type II fractures
be managed?Treatment
1. Manipulate to obtain a reduction
then
2. Stabilize the reduction
Treatment
150
What must be accomplished with
the manipulative process?
First
This is usually accomplished
by first forcing the forearminto pronation.
The deformities in both planes
need to be corrected.
Some manipulative correction
may need to be accomplished
in the coronal plane as well.
150
One usually meets resistance,
at the point where the shaft condylar malalignment limits flexion.First
Then
The deformities in both planes
need to be corrected.This usually re-establishes the saggital
alignment (shaft-condylar angle) of the distal fragment.To obtain a complete reduction in the
saggital plane, one must
To obtain a complete reductionin the
saggital plane one must
400
How does one determine
if this fracture can beimmobilized with a cast
alone?
Following this hyper flexion, the elbow is then extended
and examined to be sure the carrying angle
has been corrected as well.
Full
.The reduction has been maintained
at 1200 of flexionand 900 of external rotation.
Determine if it is
400
.
If the reduction is stable
at 1200 of flexion,and there is no evidence
of
vascular compromise,
how can these fractures
be best immobilized
post reduction?
Stabilization with a
may not be adequate !!The elbow must be flexed to 120 0
Injury filmReduced at 1200
Reduction lost
at 900WARNING
Flexing to > 1200 may increase the riskof vascular problems.
*
*Millis MB, Singer IJ, Hall JE.
Clin Orthop 188:90–97,1984.
to maintain the reduction .
Thus these fractures need to be immobilized
with a figure
8cast.
Always incorporate
the sling intothe cast.
Mommy,
this slingis
bothering me!
That’s
muchbetter !
But,
loss of
elbow
flexion
may
result in
a loss of
reduction.
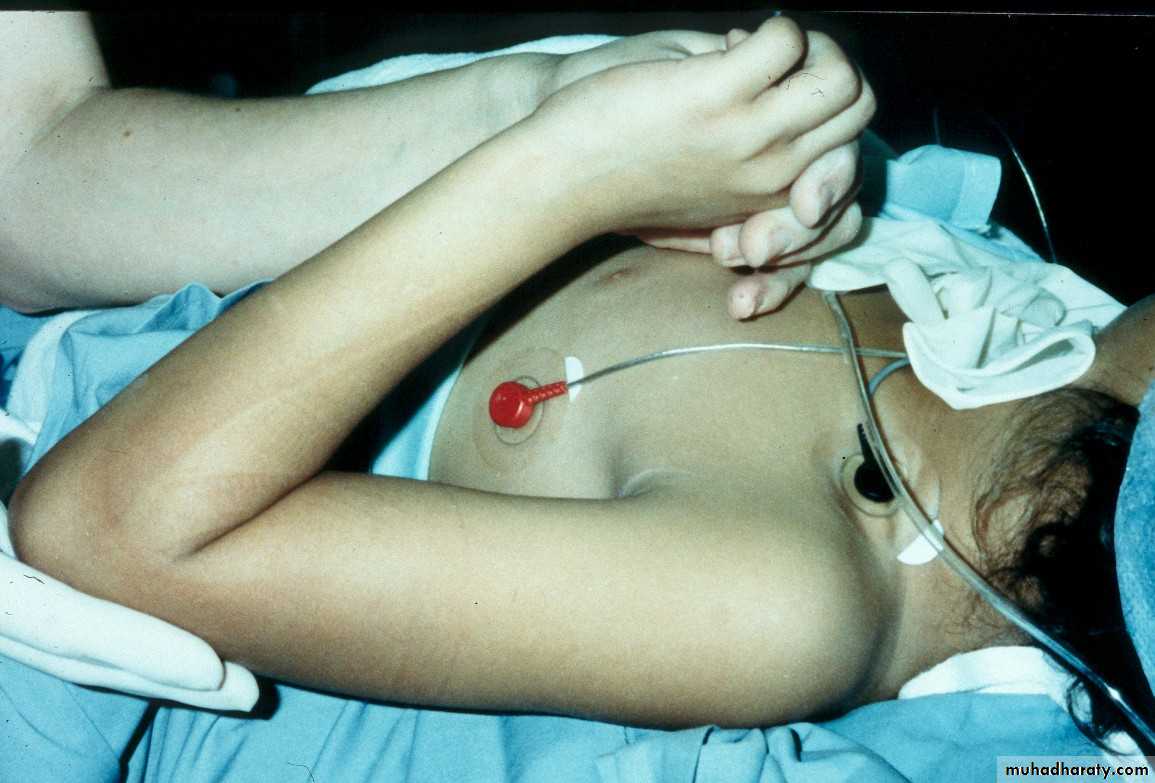
With Type II fractures, if
there is any concern about
vascular compromise
or fracture stability
due to the severe swelling,
then secure the fragments
with percutaneous pins,
so that the extremity can be
immobilized at 90 degrees.
In fact, a recent study has demonstrated
that asymptomatic pressures of > 30mm Hg. mayoccur in the deep volar forearm compartment,
even when
the elbow is flexed to just above 90 degrees.
*
*Battaglia TC, Armstrong DG, Schwend RM.
Journal of Pediatric Orthopedics 22:431,2002.
For this reason, some surgeons advocate
stabilizing all Type II fractures with pins.
What are the criteria for
fractures?How are Type III extension supracondylar
fractures sub-classified?Yes
Posteromedial vs. Posterolateral
• Nerve, Vessel Injured
• Surgical Approach
• Rate of Complications
In what aspects is there a difference?
What type has a greater
potential for complications?
The rate of complications is greater with the posterolateral fractures.
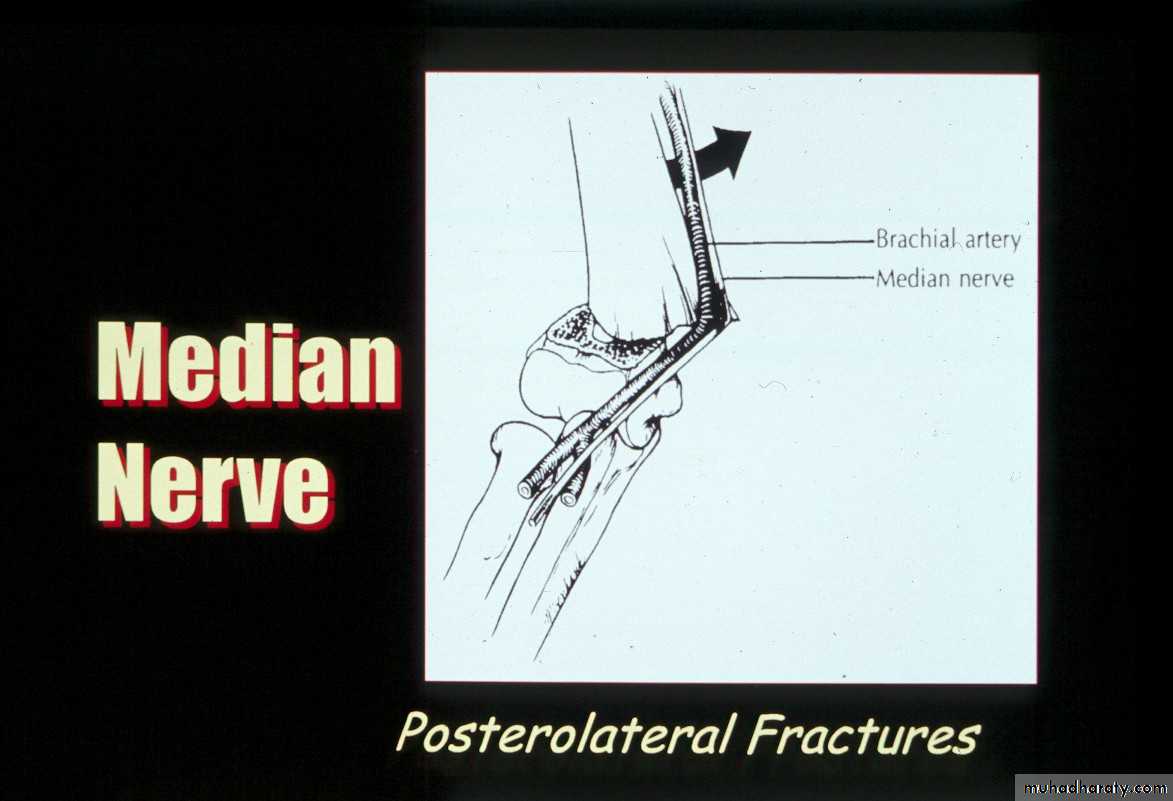
Posterolateral Pattern
Higher Risk of:1.Vascular injuries
What’s the major concern with the posterolateral pattern ??
What’s the major concern with posterolateral pattern ??
Posterolateral PatternHigher Risk of:
2.Irreducibility
What is the major concern
with the posteromedial fractures ?The radial nerve
is more vulnerable
to injury.
Treatment
How are Type III fracturesbest treated?
Simple
1. Obtain the reductionthen
2. Maintain the reduction
Do these fractures have to be reduced
in the middle of the night?No, as long as there is no evidence of
any vascular compromise.
Several studies have demonstrated that
a delay of 6-8 hours in reducing these fractures,
does not increase the incidence of
complications or unsatisfactory results.
*
* Leet AI, Frisancho J, Ebramzadeh E.
Journal of Pediatric Orthopedics. 22:203,2002.
Mehlman CT, Strub WM, Roy DR, Wall EJ, Crawford AH..
Journal of Bone & Joint Surgery.83A:323,2001.
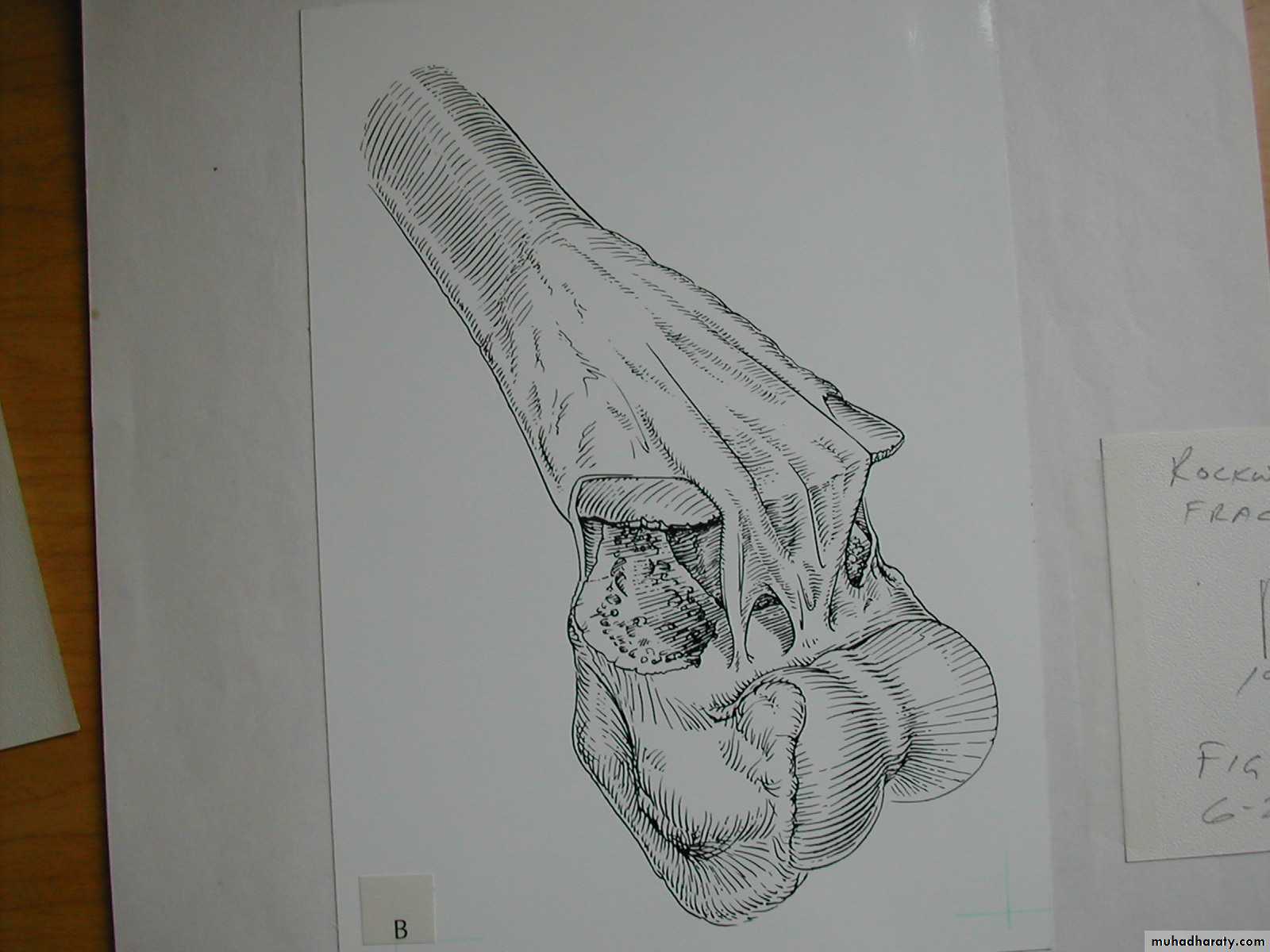
It consists of four steps:
Reduction of the fracture
What does the manipulative
process entail ?
With the elbow in extension, align the distal fragment
to the proximal fragment in the coronal plane.1. Correct coronal plane alignment
2. Re-establish Length
TractionCounter-Traction
This usually requires
an assistant.
3.Correct Angulation
andPosterior Displacement
Apply longitudinal traction
with the elbow semi- flexed,while applying posterior
pressure on the proximal fragment.
Then, slowly flex the elbow to bring
the distal fragment into alignment.4. Temporary stabilization and assessment
to lock the distalfragment to the
proximal fragment.
Once the fragments are reduced,
hyper-flex the elbow
withhyper-pronation
Then, confirm the reduction
in full external rotationon the monitor.
Warning!!
If unable to obtainfull flexion
STOP!!
There may be
interposed tissue
between the fragments!!
Now-- how do we
maintain thereduction?
Using a cast alone for post-reduction,
produces the poorest resultswhen compared with other methods.
*Pirone AM, Graham HK, Krajbich JI. J Bone Joint Surg 70A:641,1988.
Kurer MH, Regan MW. Clinical Orthopaedics & Related Research. 256:205,1990.
*
How much
flexion is needed
to prevent rotation
of the distal fragment?
This immobilization
device is nolonger commercially
available.
Full flexion
is requiredto prevent
rotation of
the distal
fragment.
Percutaneous
pin
fixation
If a cast is inadequate,
then what is the standard for maintaining the reduction?
• Advantages ?
• Most stable construct• Post-operative, one is able to fully extend elbow to visualize coronal alignment
• Disadvantages ?
• Ulnar nerve injury
Medial-lateral
pins
In what manner may the pins be used?
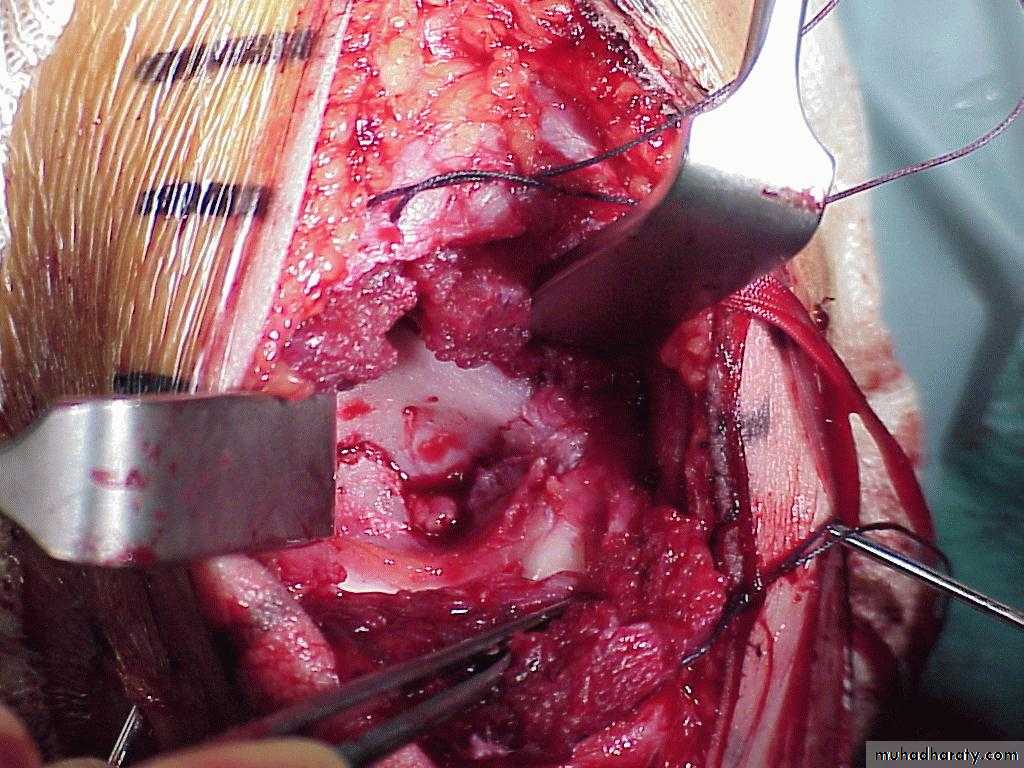
How can the danger of ulnar nerve
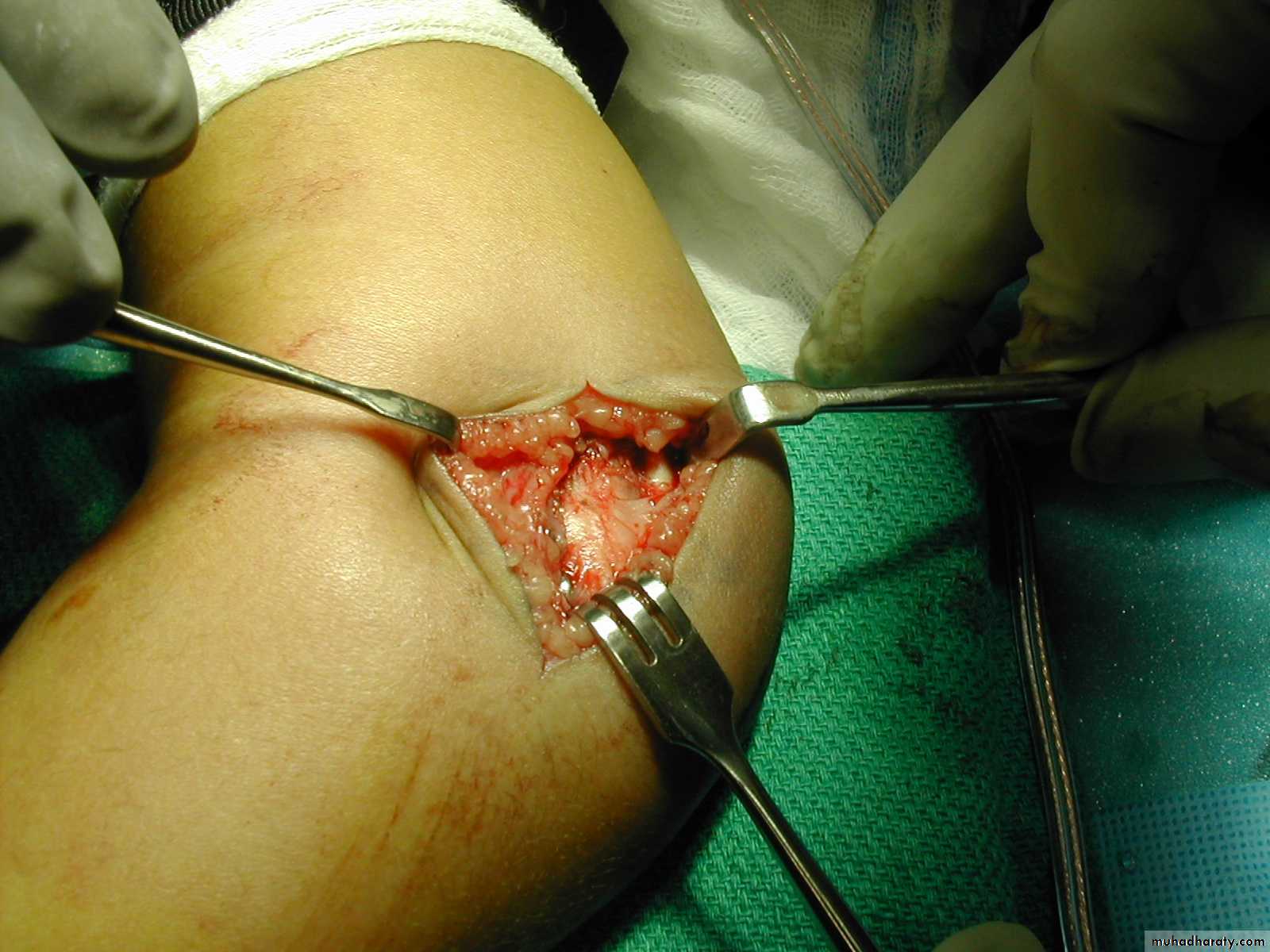
injury be minimized?By
making an incision
directly over the
medial epicondyle,
to locate the
medial epicondyleby direct vision.
Then, insert the medial pin by direct vision
into the center of the medial epicondyle.while the ulnar nerve
is
retracted posteriorly.
The pin is inserted,
Advantages ?
Easy to applyAlmost no risk of nerve injury
Disadvantages
Poor rotational stabilityPins must be parallel
or divergent
Two lateral
pinsPins crossing at the
fracture lack stability
*Cheng J, Lam T, Shen W.
J Orthop Trauma 9:511,1995.
*
What are the principles of lateral pin fixation?
Loss of rotation of distal fragment
These three pins with
no separation allowed rotation.But, since the coronal alignment has been maintained,
in addition to the shaft condylar angle,this rotational malalignment
is usually ofno clinical significance.
Advantages ?
Almost as strong as medial-lateral pins
Disadvantages?
The larger patients may still have rotational instability,requiring supplementation with a medial pin.
*Zionts LE, McKellop HA, Hathaway R.
J Bone Joint Surg [Am];76:253,1994.
How can the rotational stability with lateral pin be enhanced?
By separating the pins
and adding a third pin.
*
Is there a way to put X pins
without producing this scar?Lateral Antegrade pin
Following pin fixation,
how are these fractures managed ?For three weeks
What is this physical finding ??
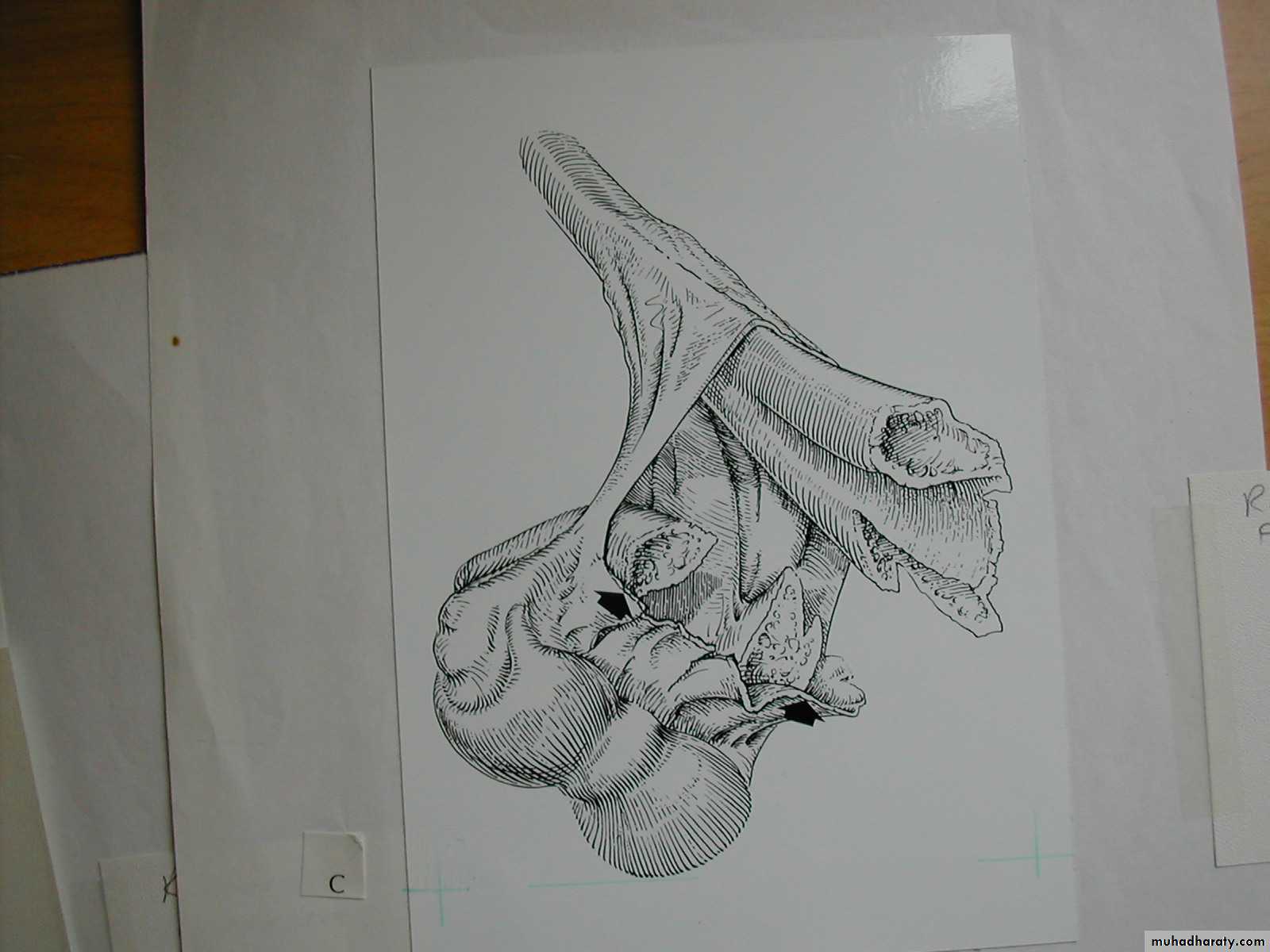
The “Pucker Sign” which may indicate irreducibility.How may the proximal spike be
dis-impaledBy performing the “milking ” maneuver.
The “milking ” maneuver
The distal humeral spike
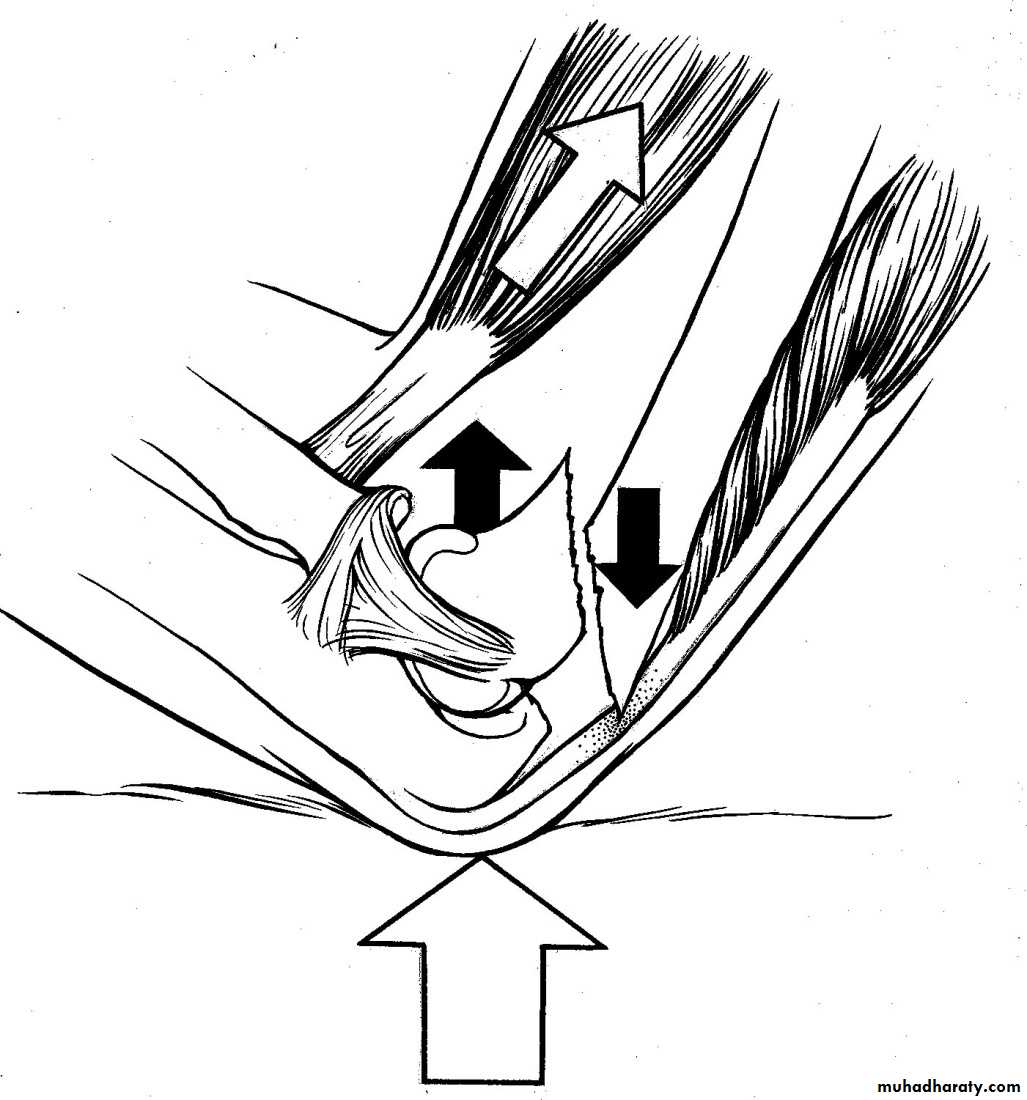
is impaled throughthe brachialis muscle.
With the milking maneuver
*Archibeck,MJ et. al.:Jour Pedi Orthop 17:298,1997.
*
The brachialis is milked distally
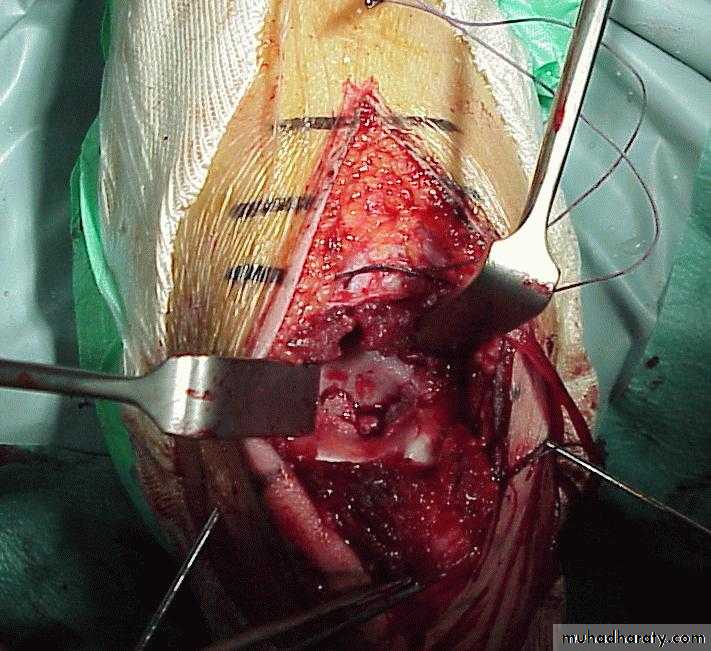
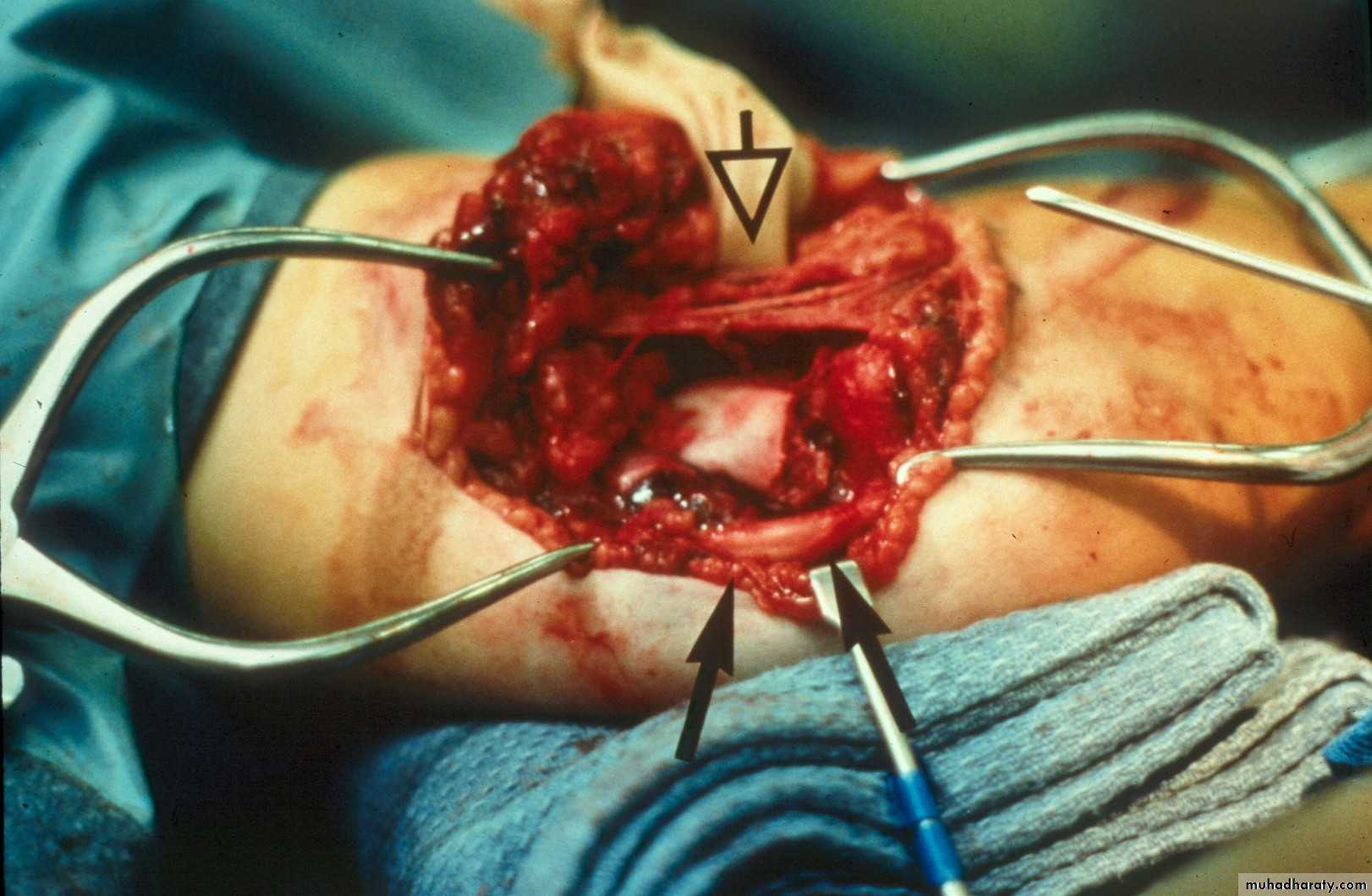
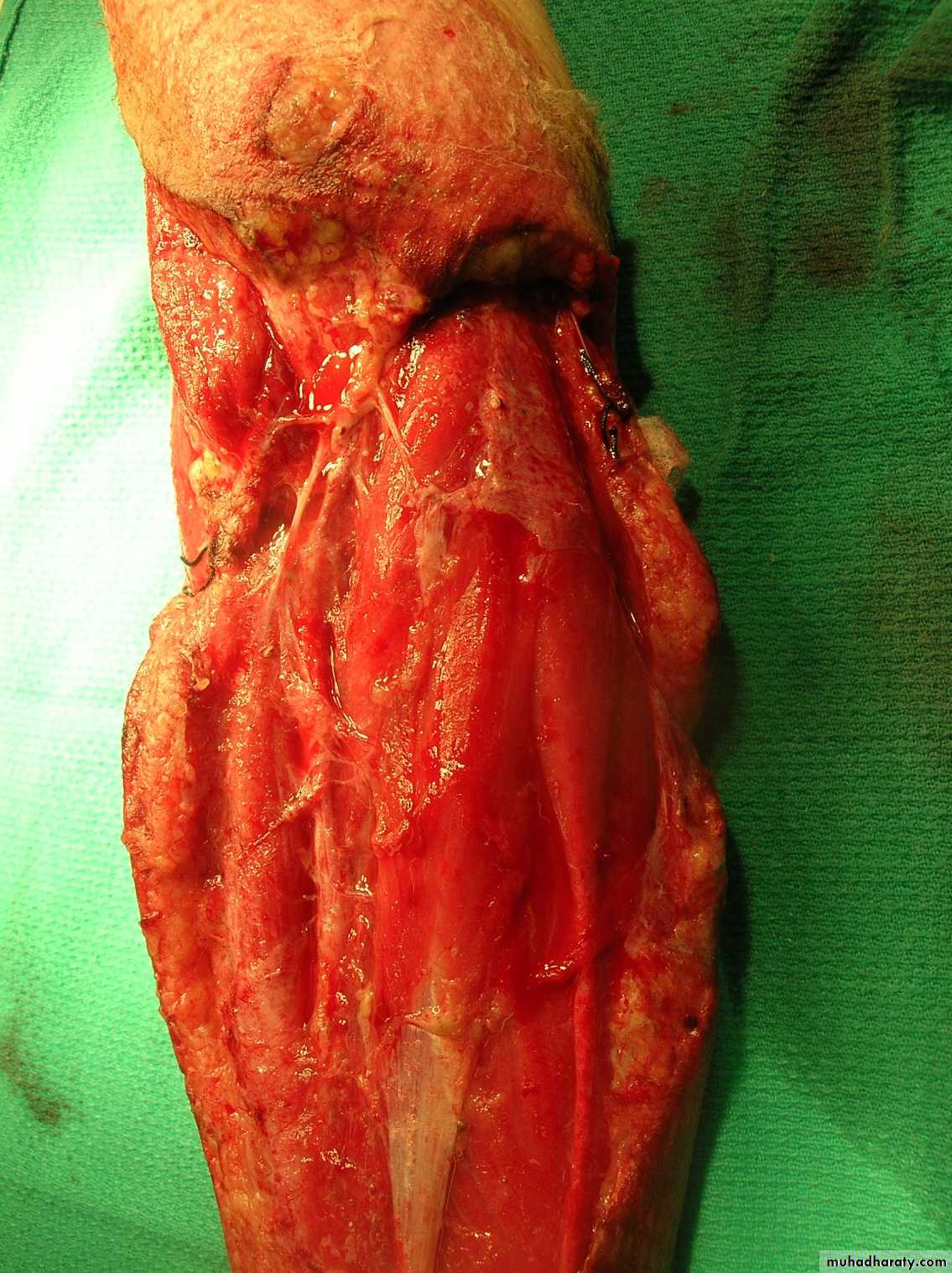
past the impaled fragment.In those irreducible fractures, what dictates the preferred surgical approach?
Anteromedial incision
Anterolateral Incision
The ability to visualize
the interposed vital structures is essential.Post-Lat Fracture:
Post-Medial Fracture
Medial humeral
spike
Lateral humeral
spikeWhat about the posterior approach?
This fracture
was irreducibleby closed
manipulation.
Injury film
The posterior
tricepssplitting
approach
Advantages:
Easy approach
Direct
visualization
of fracture site
Disadvantages:
Injures virgin
tissue
Unable to
visualize
anterior A. & N.
*Compliments of Jamie Maclean(Pearth ,Scotland)
*What is the primary purpose of an open reduction?
• The goals are to• remove the interposed structures which
• facilitates a closed reduction and
• a percutaneous pinning.
What is one of the main tissues
preventing an anatomical reduction?The periosteum
tears proximally,
and remains as
big wad
attached distally.
Post-reduction
Gap persists
6 weeks3 months
Gap has remodeled
X-ray evidence of this periosteal interposition
often is demonstrated as a gap in many fractures
Gap with interposed
periosteum
Mind the Gap!
While the periosteum tears proximally,
This flap of periosteum
can serve as a guide tolocating and reducing
the distal fragment.
it remains attached distally as a large flap.
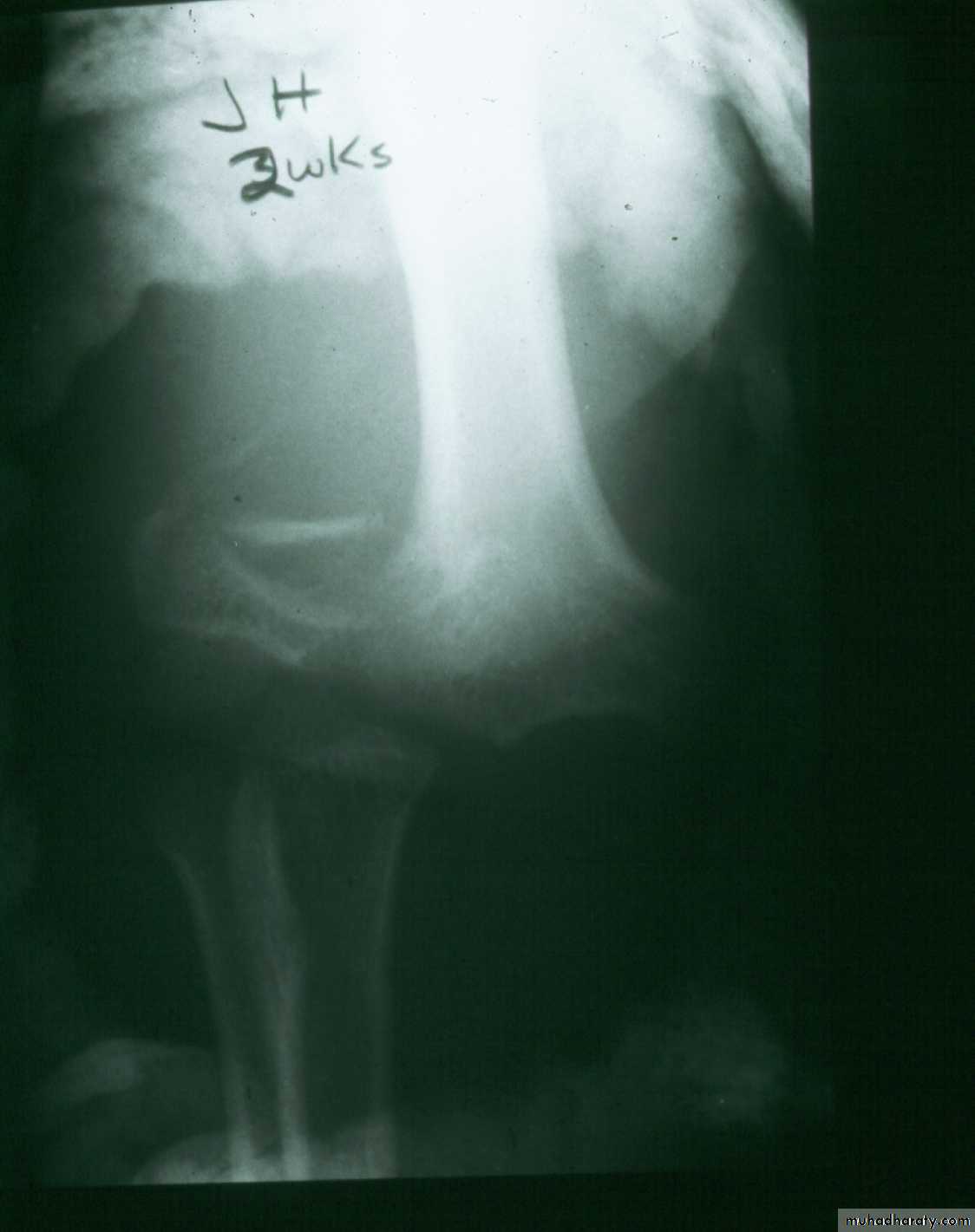
What about late-appearing fractures ?2 wks. post
closed reductionWhat now?
Repeat
closed reduction?
Open reduction?
Periosteal
new bone
Wait. Remodeling can change things.
He had only slight valgus alignment with full elbow motion
What are the risksof doing a late open reduction ?
Myositis Ossificans
**Lal, G.M. Bhan,S.:
Int.Ortho.15:89,1991.
The dilemma when one of these
fractures presents late is:
1.Do a delayed open reduction
and risk loss of motion from myositis.
or
2.Wait and do a corrective osteotomy
when the patient has recovered
full motion.
In addition to evaluating the neurovascular
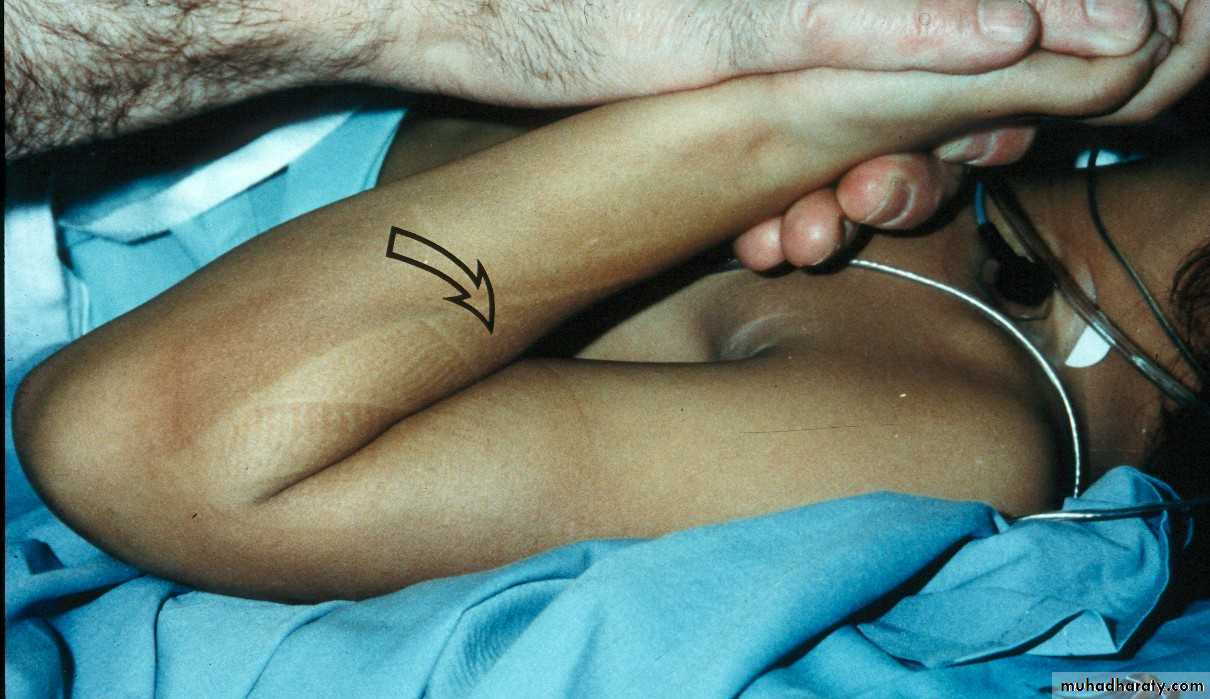
function, what else needs to be done ?Always check for ipsilateral fractures.
Do the patients with ipsilateral
fractures have more of a riskfor compartment syndromes?
The answer is not clear!
In three series, there was
no increase in vascular complications.
*
*Harrington P, Sharif I, Fogarty EE, Dowling FE, Moore DP.:
Archives of Orthopaedic & Trauma Surgery. 120:205, 2000.
Roposch,A et.al.: Jour Pediatr Orthop 21:307,2001.
Siemers,F et.al.: Zentralblatt fur Chirugie 127:212,2002.
The answer is not clear!
In two other series
compartment syndromes developed.
*
Because ipsilateral fractures
are usually the result of trauma
of greater magnitude,
they need to be followed closely.
Both fractures need
to be stabilized surgically
to eliminate the need for
constrictive cast.
*Blakemore,LC et.al.: Clin. Orthop and RR 376:32,2000.
Ring,D et.al.: Jour Pediatr Orthop 21:456,2001.
Do the patients with ipsilateral
fractures have more of a risk
for compartment syndromes?
Ipsilateral shaft fractures
Yes. One has to establish a lever arm first.
12
1
2
In what order do they need
to be stabilized?
Distal radius
Are they treated differently ?
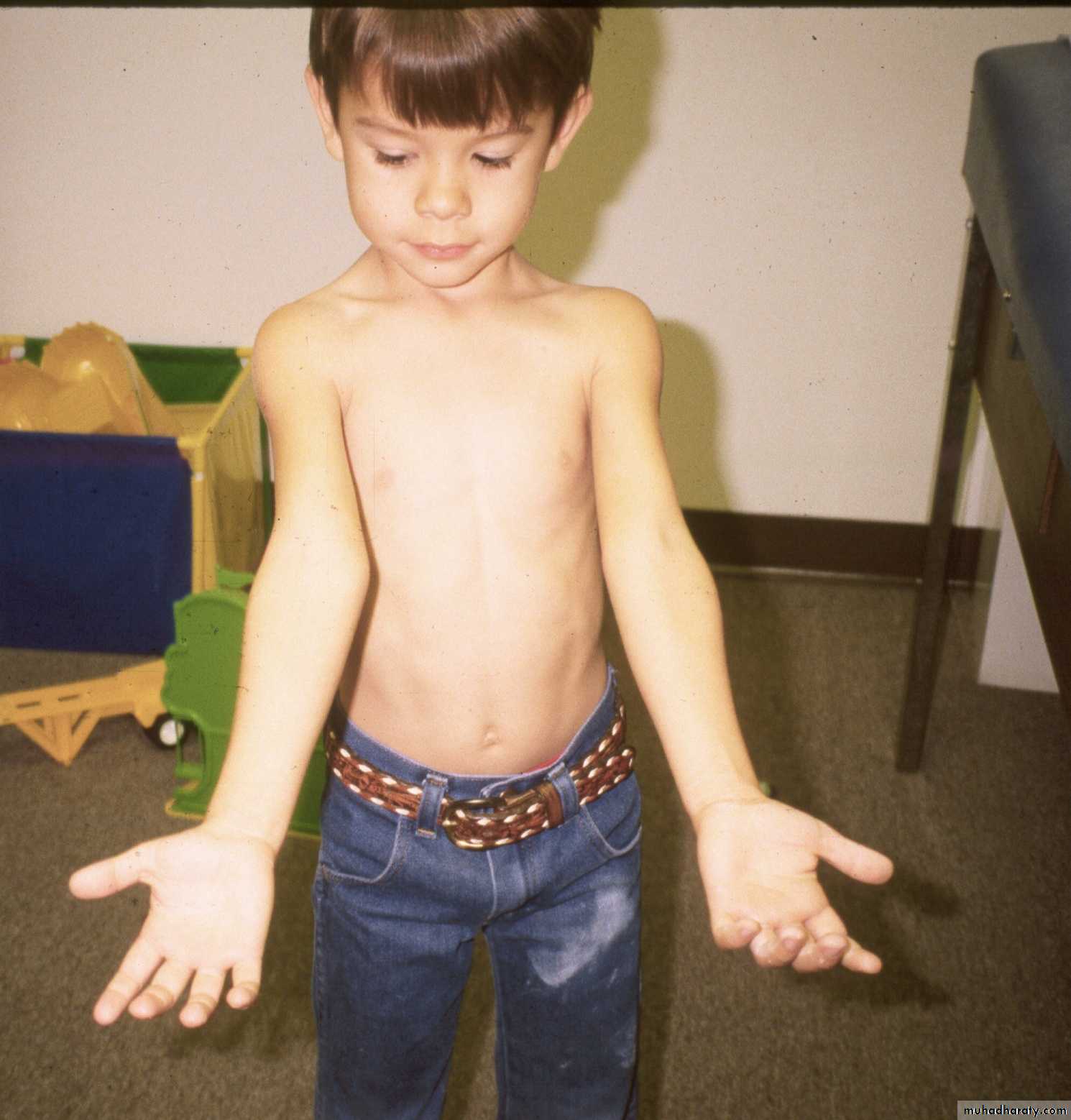
What type of supracondylar fracture
does this patient have?Flex
ionHow do the flexion patterns present?
Type I:Criteria?
They are undisplaced. Therefore no reduction is needed.
Type II:
Criteria?
There is enough intrinsic stability to be treated with a cast alone.
Type III:
Criteria
They have no intrinsic stability, thus they need surgical stabilization.
They present
in the same manner as the extension types.Type I Flexion Injury
What are the limits of acceptability ?No good data
Greater than 20 0 of an increase of the shaft-condylar angle
probably should be corrected.
550
Tendency toward
valgus alignmentIncrease in the shaft
condylar angle
Because, if the flexion of the condyle is not aggressively
corrected, the elbow may lose extension.
Type II Flexion Injury
What is the
management?The treatment entails a closed reduction
+
a long arm extension cast.
This classical Type III pattern
is obviously a flexion injury.With these one needs to be
prepared to do an open reduction !!
8 y.o.
Is this a simple extension
type supracondylar fracture ??
It also has
anterolatateraldisplacement !!
The distal fragment is
not flexed,but also it is not extended to any degree.
This also is a Type III Flexion Pattern.
What is differentabout this fracture?
But, if not recognized as such, it may be a problem.
This fracture was irreducible,
and required an open reduction !!!
There are some clues to these occult flexion injuries.
1. The distal fragment is not extended,
however,it may not be flexed to any degree.
It may be
rotated!!2. The distal fragment is in valgus.
3. The medial spike of the proximal fragment is usually posterior.
4. There may be clinical signs of ulnar nerve dysfunction.
Why are these fractures irreducible ?
The location of the proximal medial spike is critical.The medial spike
is pressing againstthe ulnar nerve.
It is also posterior to the
intermuscular septum.
What is the operative approach ?
It involves an anteromedial incision.
Ulnar NerveAnterior N.V. Bundle
Medial
spike
One needs to be able to see the:
So what’s the message here?If critically evaluated
flexion SC fractures
may be more common.
Be prepared to
perform open reduction
on Type III flexion injuries.
Exotic methods of stabilization
ofSupracondylar Fractures
This is how we treated these fractures
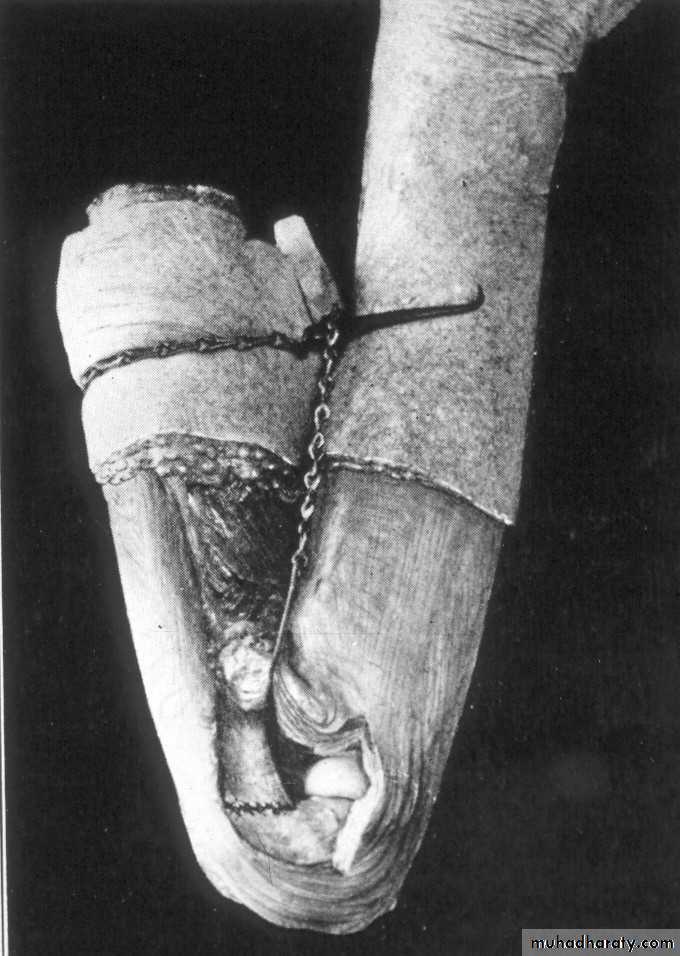
when I was a resident !!6 y.o. sustained this FX. NV intact.
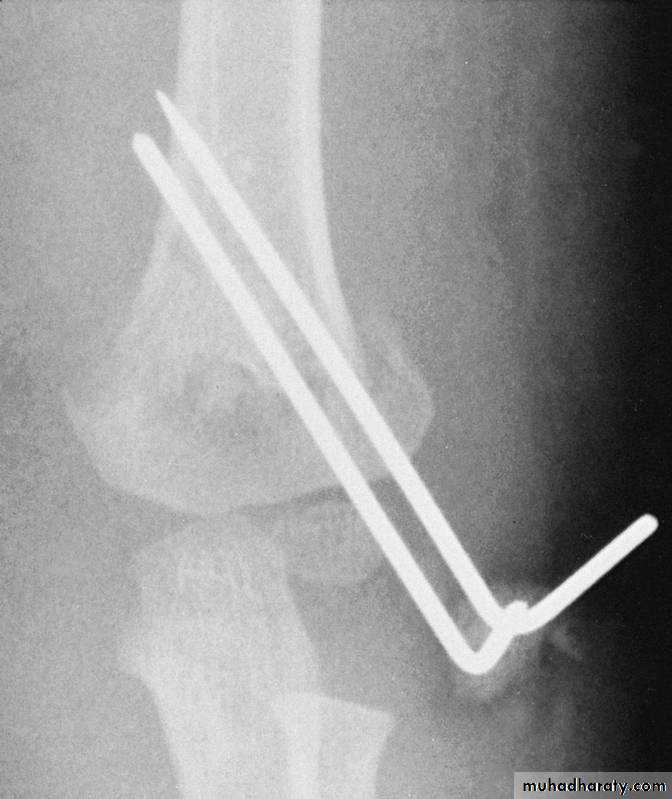
Following obtaining a satisfactory closed reduction how do you propose to stabilize it?• Medial-lateral pins
6 y.o. sustained this FX. NV intact.
Following obtaining a satisfactory closed reduction how do you propose to stabilize it?Multiple lateral pins
Outside fracture line ?6 y.o. sustained this FX. NV intact.
Following obtaining a satisfactory closed reduction how do you propose to stabilize it?
Cross pinsantegrade lateral
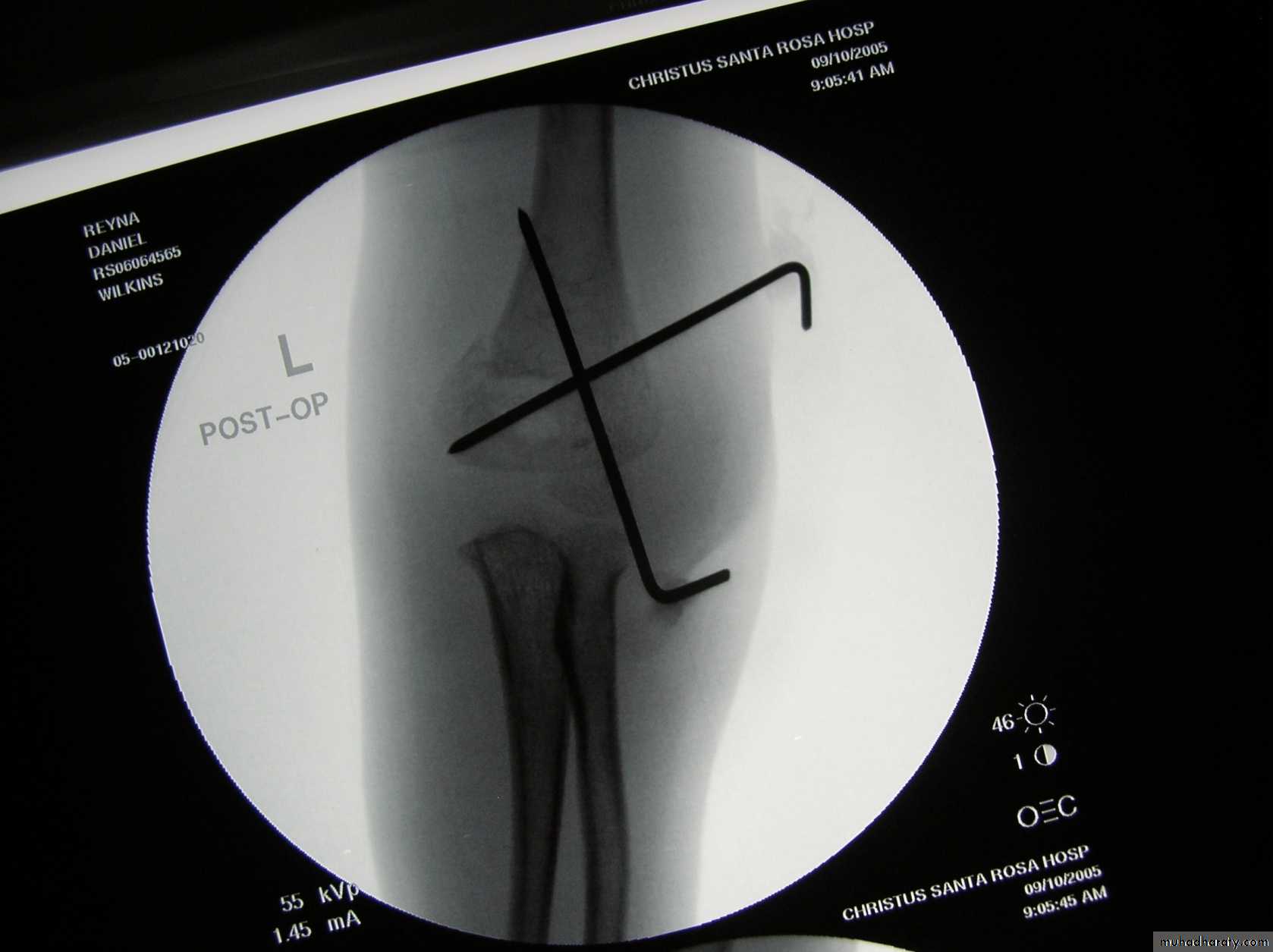
Five y.o. male with this fracture pattern
• Following obtaining a satisfactory closed reduction how do you propose to stabilize it?Multiple lateral pins
Stable ??Five y.o. male with this fracture pattern
• Following obtaining a satisfactory closed reduction how do you propose to stabilize it?
Medial-lateral
retrograde cross pinsDifficult and unstable
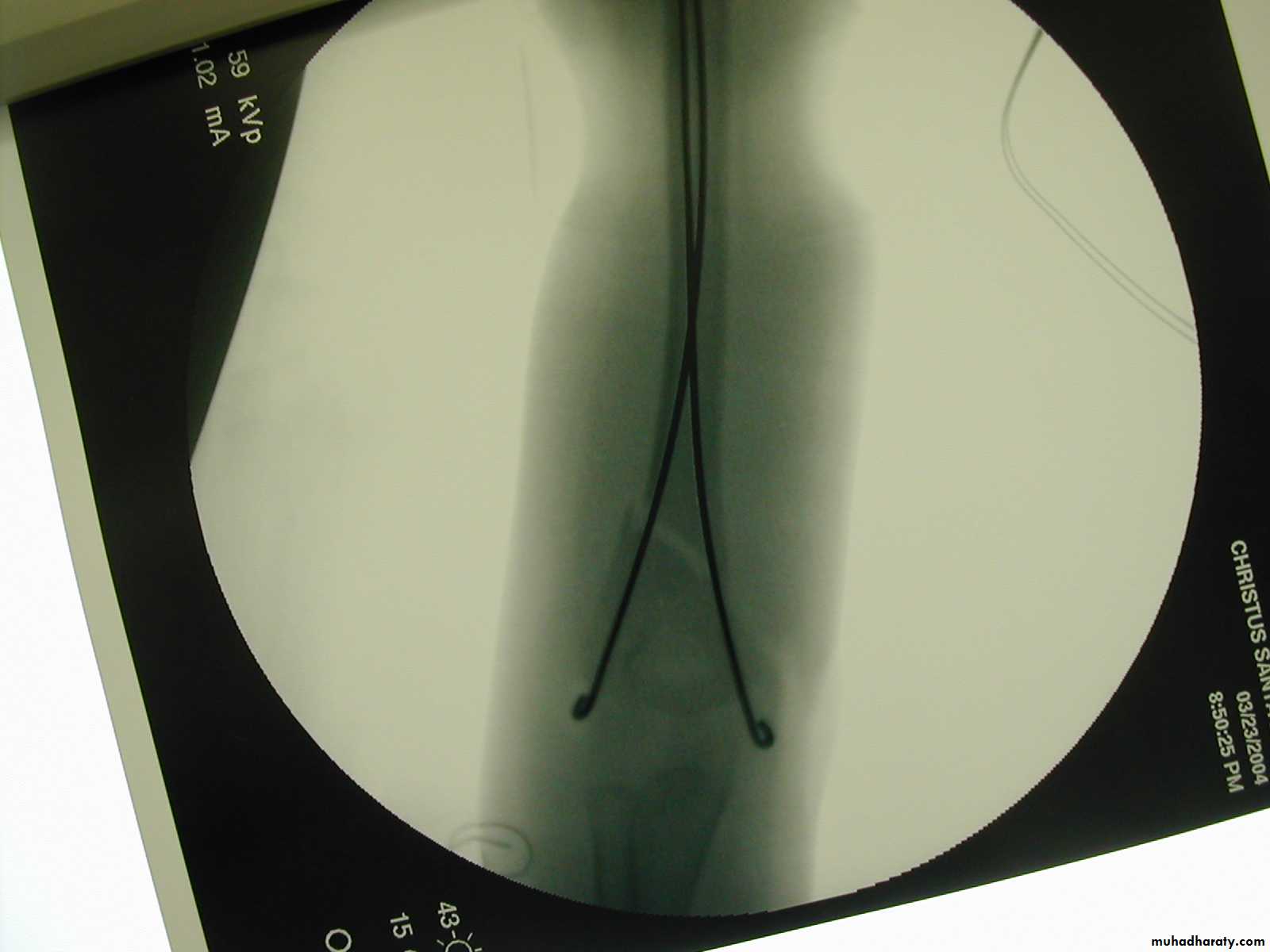
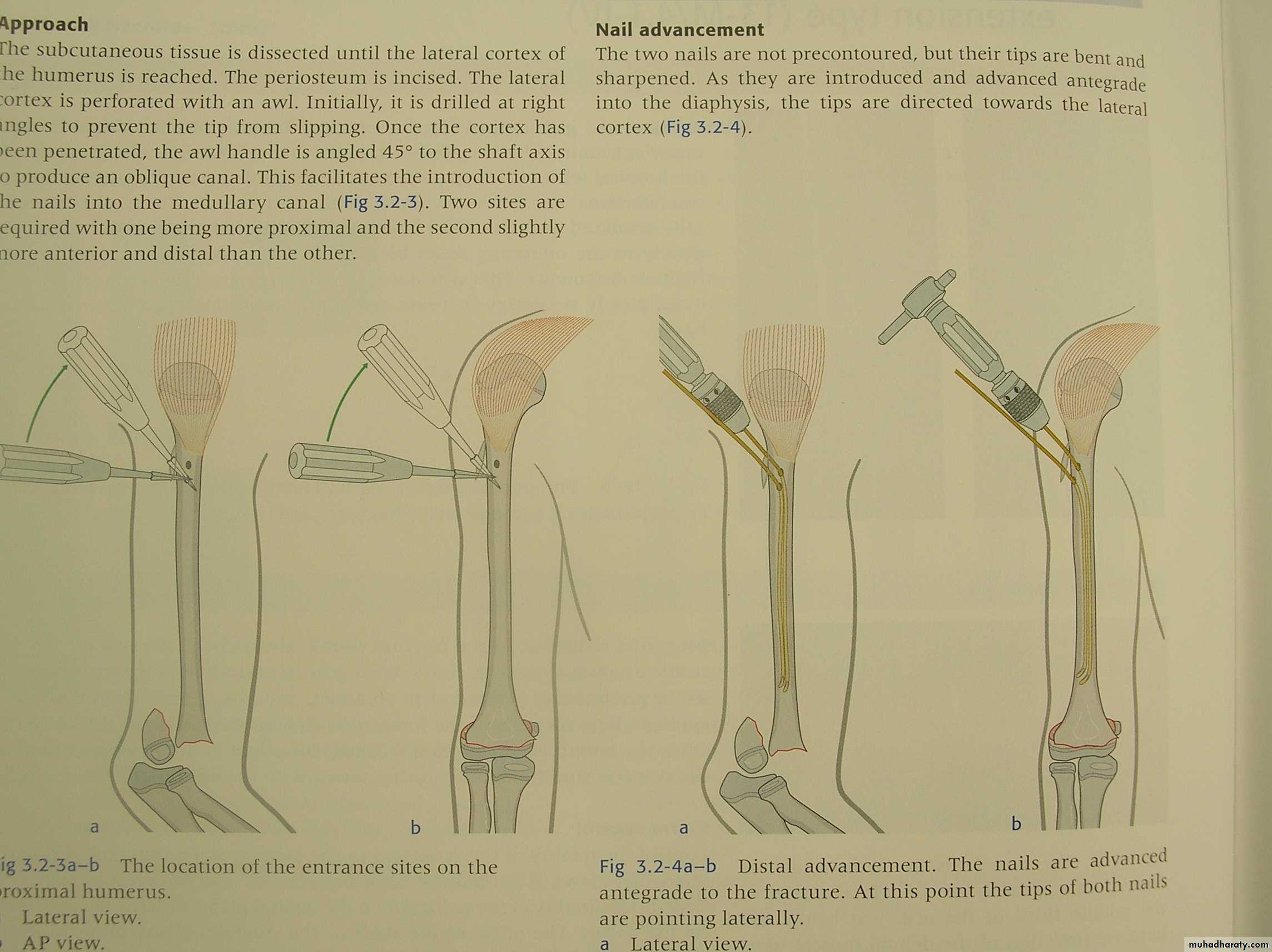
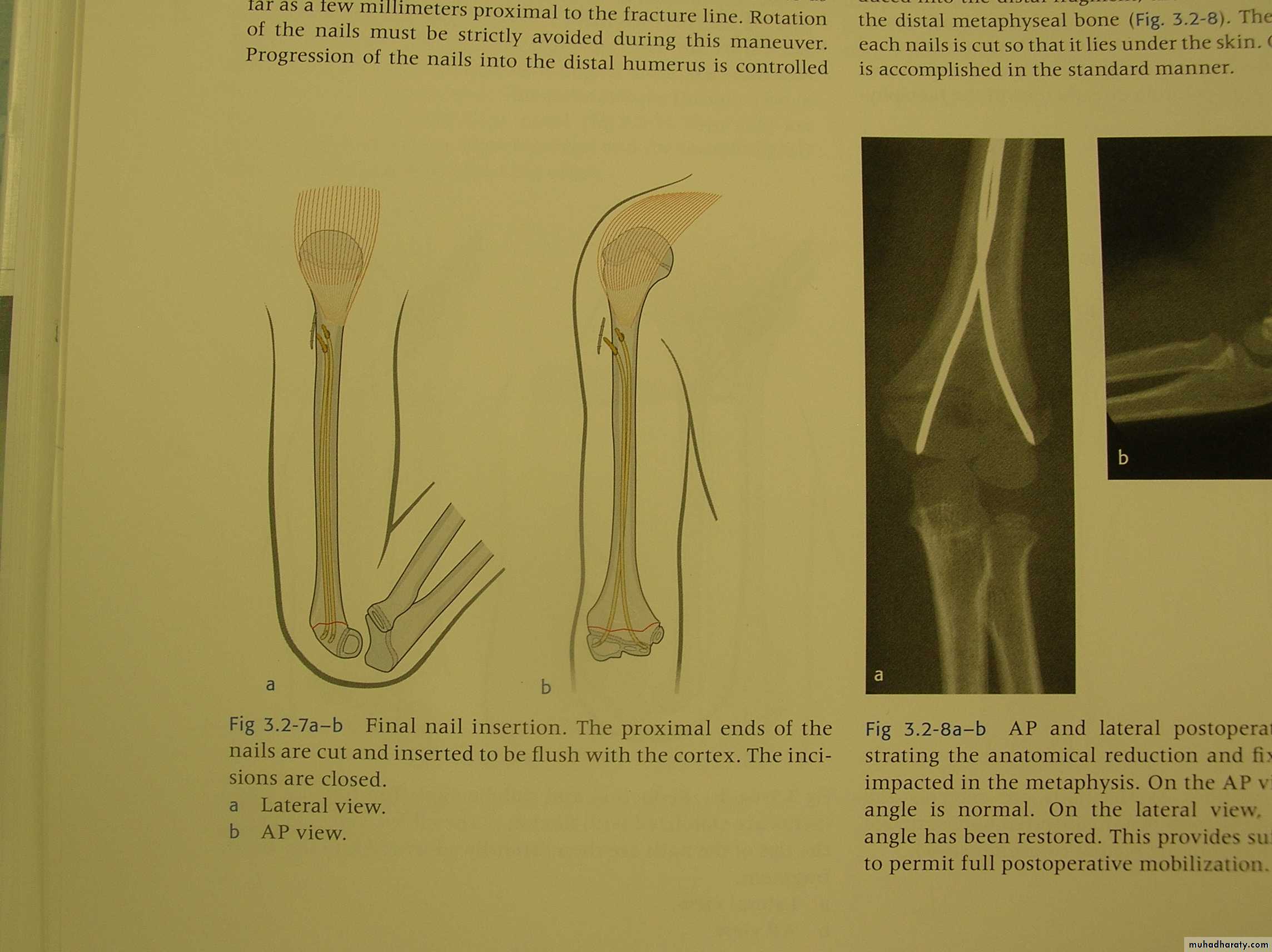
How about retrograde IM Fixation??
Must visualize the medial epicondyle
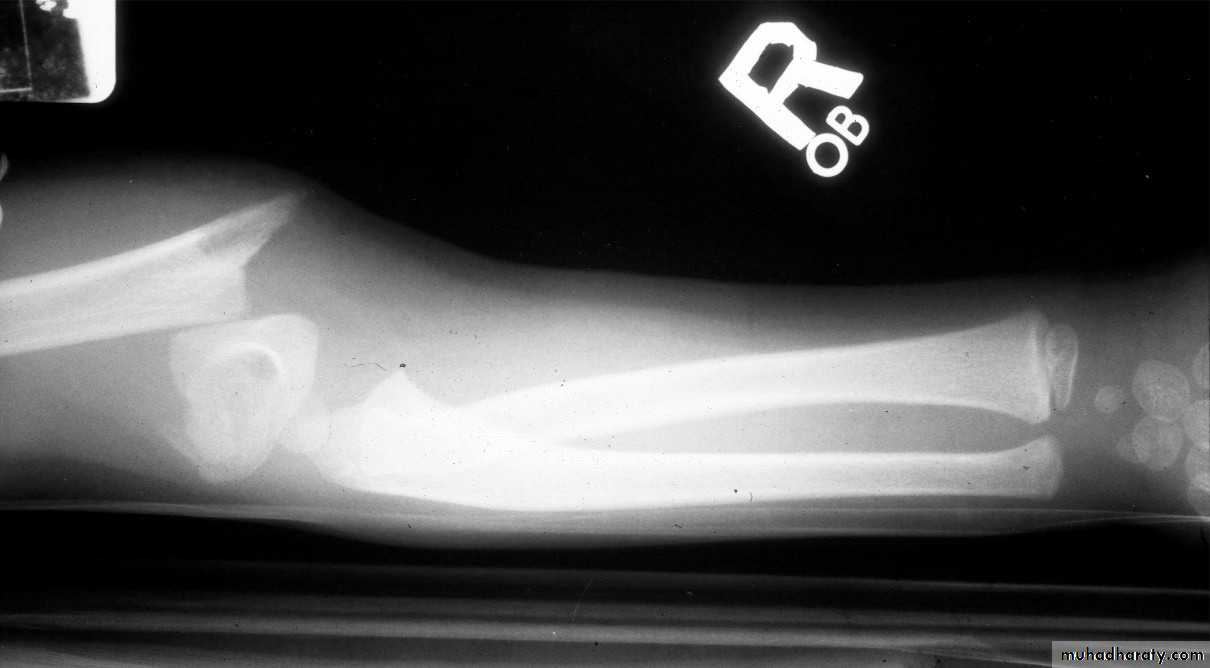
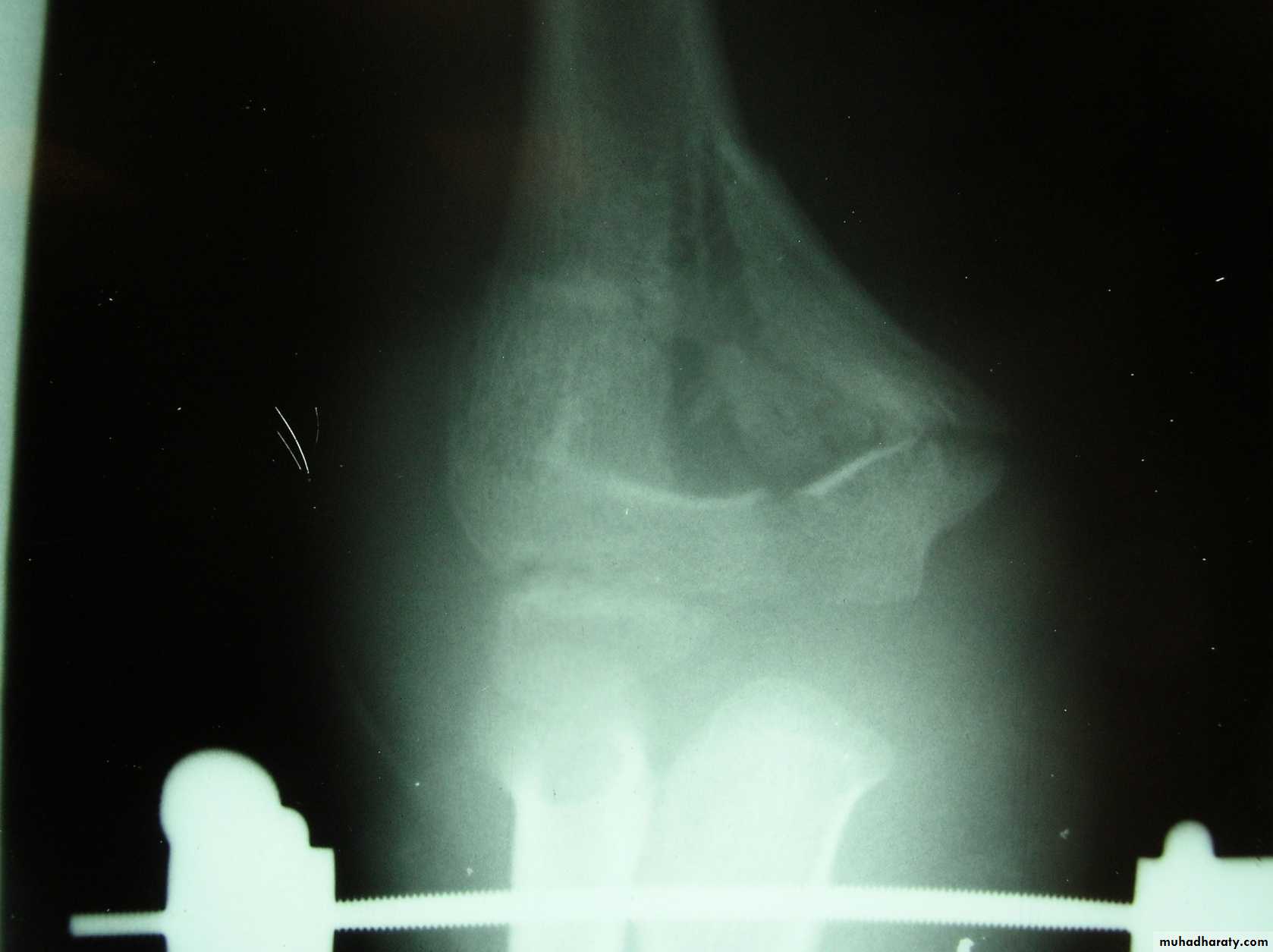
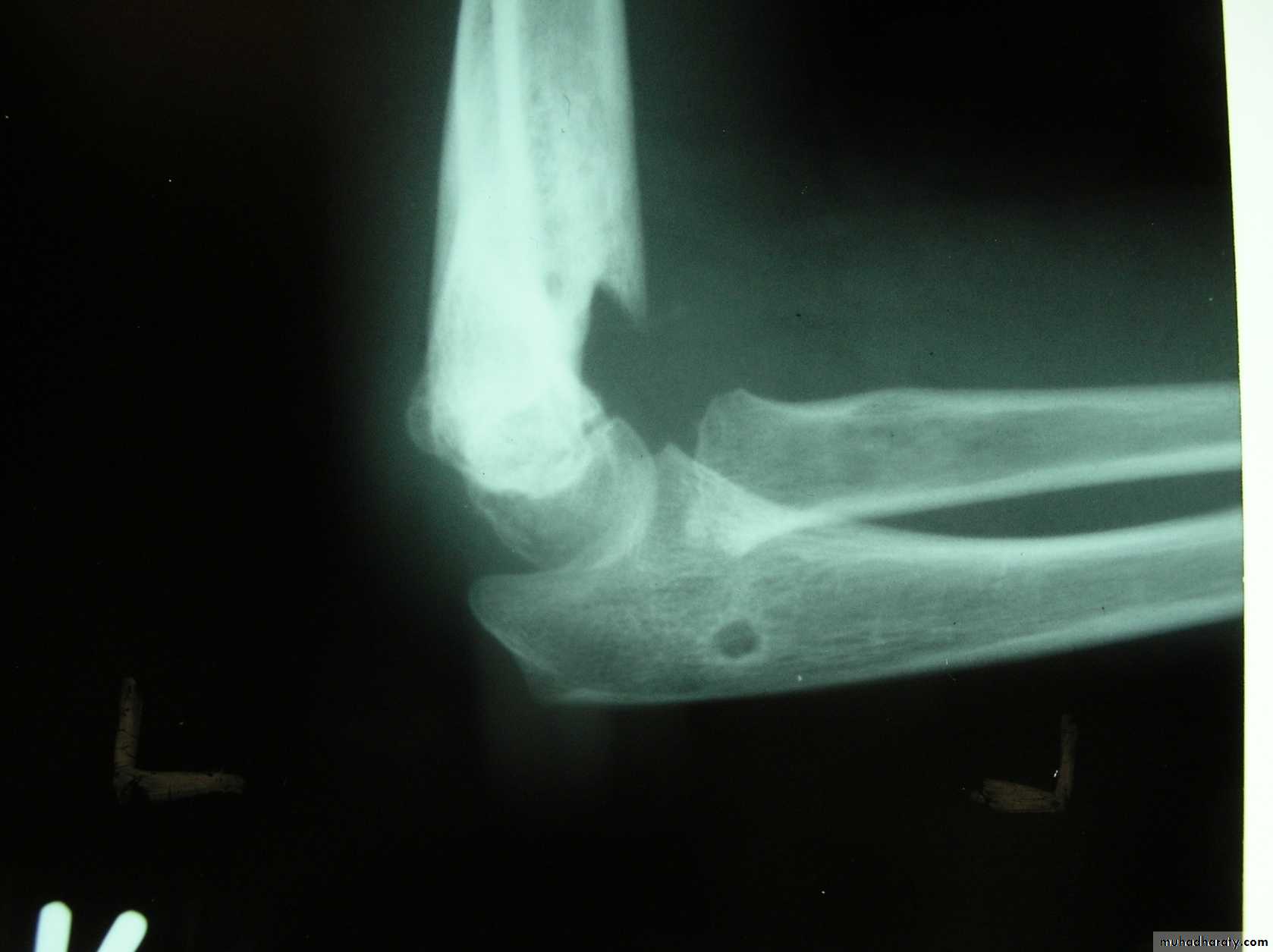
8 y.o. rolled over on an ATV
with mild closed head injuryClinical appearance
Only N-V deficit:
Anterior interosseous n. function weak
Radial A.
FCR Musc.Imaging Studies
How are we going to stabilize this boy’s fracture?
This is probably one of the few indication to use
Antegrade Flexible I M NailsOur Patient P.O.
Probably acts more
as an internal splintSix months post-operative
How is he doing clinically?
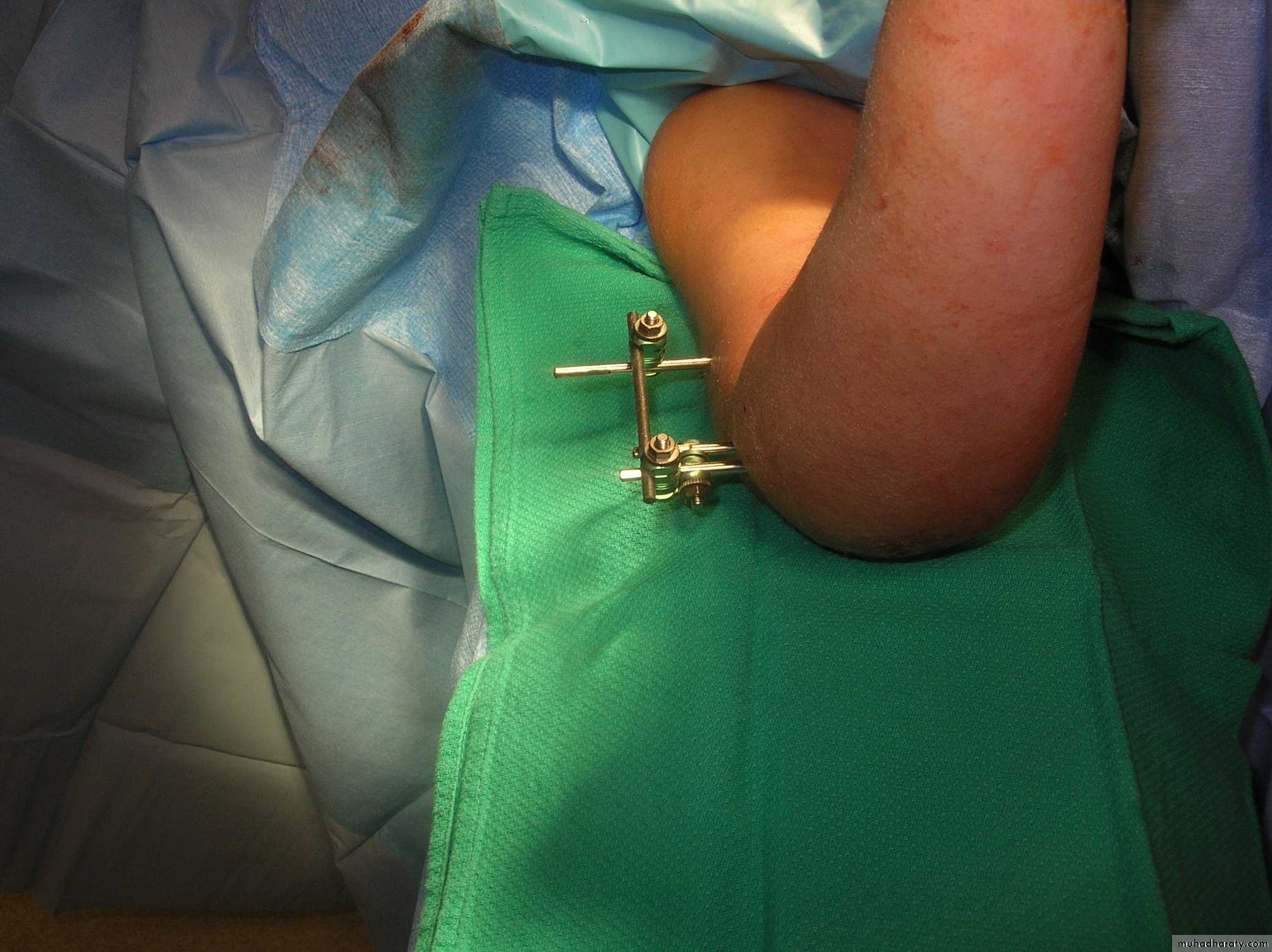
What is the place for an external fixatorif any?
Screws in proximal
and distal fragmentsSingle pin to control
rotation
Reported useful
to manipulatethe fragments
The place for an external fixator
May be effective
with
comminution of
distal humerus
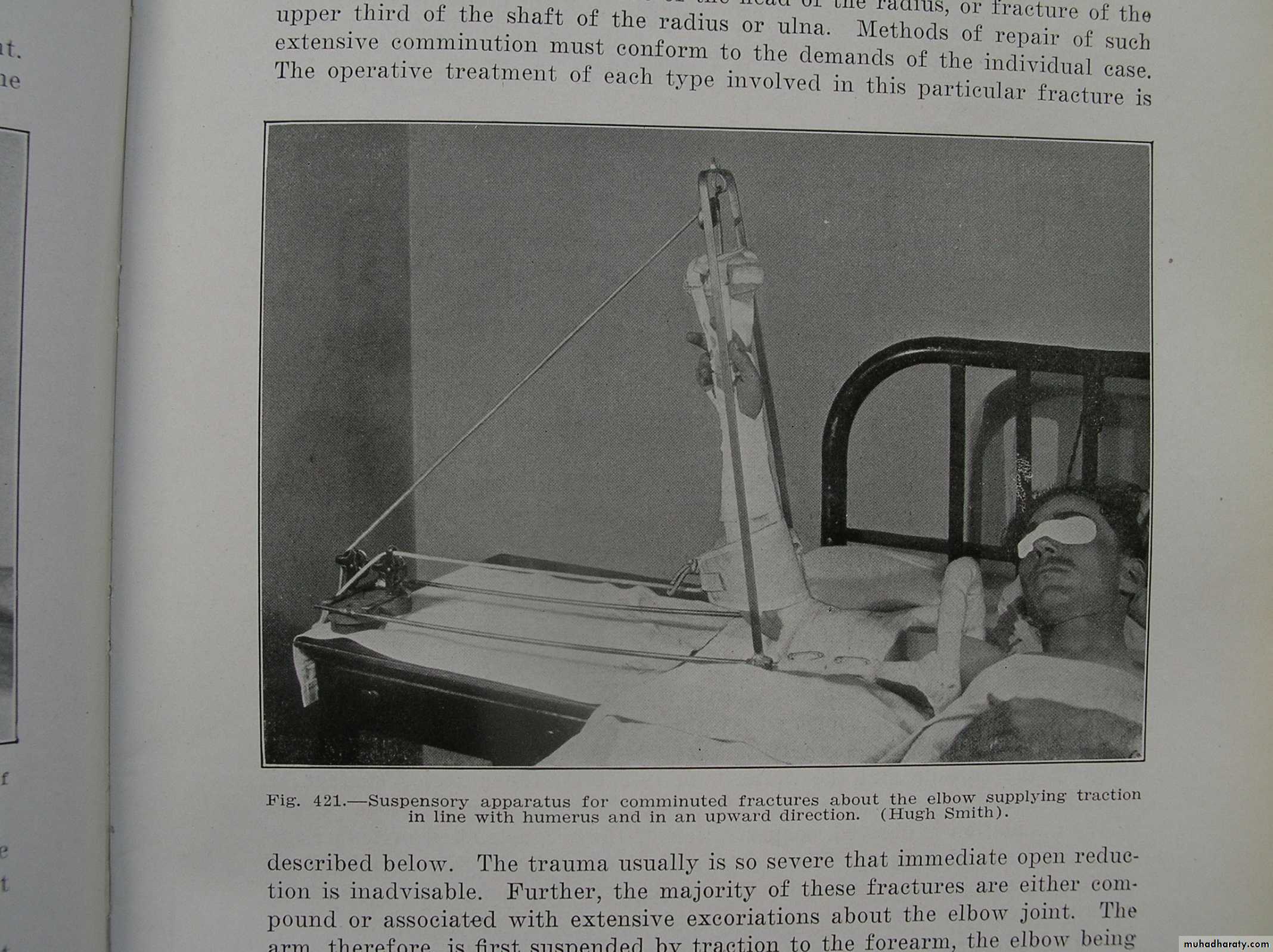
6 y.o. comminuted Supra/T condylar
Treated in skeletal tractionGood results achieved
In this time this may have been a candidate for ex-fix
Now you shouldbe prepared to treat
all the unusual cases
Thank you
Complications
Cubitus varus
Volkmann's
What arethe two most common complications?
The details of these complications
will be discussed in Part II of this module.