Al-Mustansiriyah University
College of Medicine - Department of MedicineDivision of Radiology
IMAGING OF ACUTE ABDOMEN
DR. ABDULLATEEF AL-BAYATITeaching Board Member
CABMS-RAD
6
Right upper quadrant pain
• The primary diagnostic consideration in adult patients with right upper quadrant (RUQ) pain is acute cholecystitis.
• Ultrasound is the most sensitive investigation for the presence of gallstones and is therefore the investigation of choice for suspected acute cholecystitis.
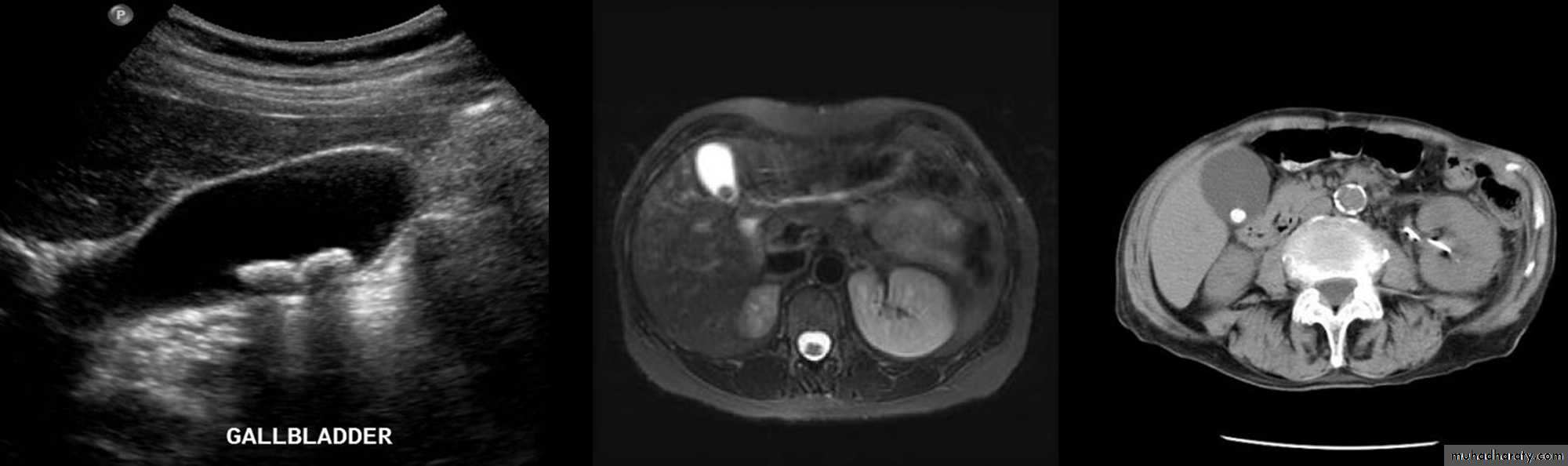
Gall Stones
• Gall stones are more frequent in middle age females.
• 20% of gall stones are visible on plain film.
• On US, stones are strongly echogenic with acoustic shadow (which is not seen with polyps).
• US is not reliable for detecting stones in CBD which are better demonstrated by MRCP.
Cholecystitis
• US features of early or uncomplicated acute cholecystitis:
• Gall stones (which may be impacted in the GB neck or cystic duct)
• Gall bladder wall thickening
• Gall bladder distension
• Positive sonographic Murphy's sign (focal tenderness over the GB when compressed by the US transducer)
• US features of advanced or complicated acute cholecystitis:
• Pericholecystic fluid collection
• Striated appearance of the thickened GB wall
• Intraluminal membranes caused by sloughed GB mucosa
• Gas in GB wall or lumen resulting in emphysematous cholecystitis
• US features of chronic cholecystitis are thick wall and GB contraction.
• Acute cholecystitis is diagnosed on scintigraphy with 99mTc-labelled iminodiacetic acid (IDA) scan by non-visualization of the gallbladder with good visualization of the common bile duct and duodenum 1 hour after injection.
• CT is much less sensitive than US for the detection of gallstones.
• CT signs of gallbladder inflammation include thickening of the gallbladder wall with infiltrative streaking in adjacent fat.
Right lower quadrant pain
The commonest cause of acute right lower quadrant (RLQ) pain is acute appendicitis.
Acute appendicitis
• Differential diagnosis includes inflammatory bowel disease, mesenteric adenitis, and gynecological pathology in female patients.
• Although most cases of acute appendicitis are confidently diagnosed on clinical grounds, imaging may significantly lower the number of negative appendicectomies.
• Imaging is particularly useful in patients with atypical features on history and/or in young females where gynecological pathologies, such as ectopic pregnancy or pelvic inflammatory disease, are suspected.
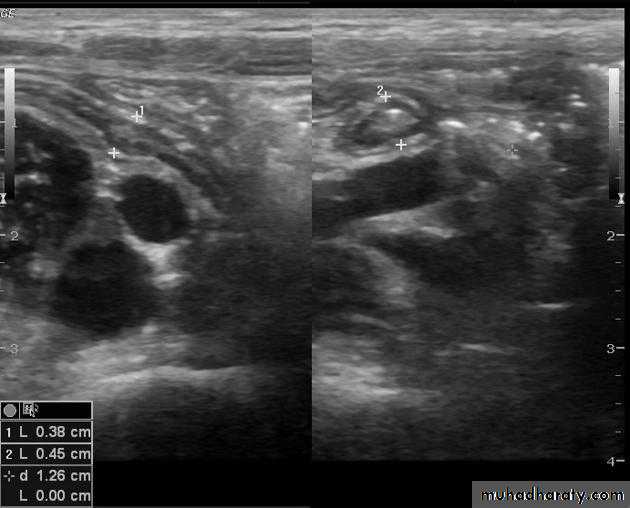
• Where imaging is required, US is the initial investigation of choice in children, thin patients and women of childbearing age.
• Accuracy of US is increased by the use of compression and color Doppler imaging and by concentrating the examination to the point of maximal tenderness as indicated by the patient.
Signs of acute appendicitis on US:
• Thickened edematous appendix [diameter > 6 mm].
• Non-compressible blind ending tubular structure.• Appendicolith.
• Local free peritoneal fluid.
• Sentinel dilated bowel loop.
• Complication: abscess, inflammatory mass.
Limitations of US:
• The normal appendix is often not visualized• Retrocecal appendicitis may be obscured.
• The negative predictive value of a negative US examination is not as high as for CT.
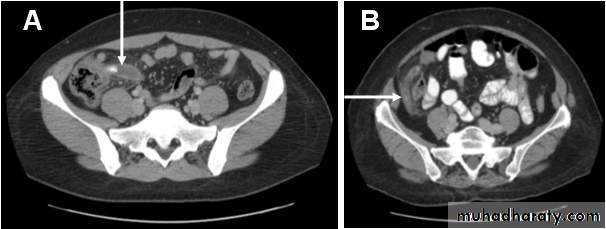
• For most adult patients, excluding women of childbearing age, CT is the imaging investigation of choice in the assessment of RLQ pain.
Advantages of CT include:
• Its proven accuracy in the diagnosis of appendicitis.
• Its ability to diagnose alternative causes of RLQ pain.
• The ability of CT to identify a normal appendix in the majority of patients.
• Its high level of sensitivity to inflammatory change mean that a negative CT has a very high negative predictive value.
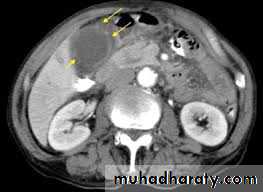
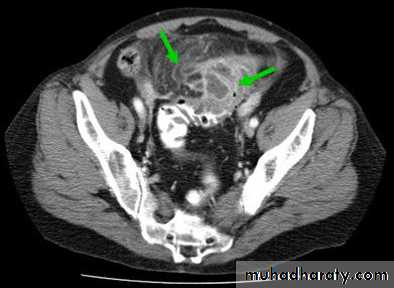
CT findings of acute appendicitis:
• CT shows a swollen appendix.
• Soft tissue stranding pattern in adjacent Fat. This stranding pattern is a highly useful sign on
• CT indicating edema in fat adjacent to inflammation.
• Large fecoliths at the base of the appendix.
• Complication: abscess, inflammatory mass.
Left lower quadrant pain
The primary diagnostic consideration for the patient with left lower quadrant (LLQ) pain is acute diverticulitis.
Acute diverticulitis:
• The term ‘acute diverticulitis’ encompasses a range of inflammatory pathologies that occur secondary to diverticulosis, including:
• Bowel wall and pericolonic inflammation,
• Perforation
• Abscess formation
• Formation of sinus or fistula tracts.
• US should be used in women of childbearing age in whom gynecological pathology, such as ectopic
Pregnancy or pelvic inflammatory disease, would be more likely than acute diverticulitis.
• CT is otherwise the investigation of choice for assessment of acute LLQ pain.
• CT is highly accurate for the diagnosis of acute diverticulitis and where diverticulitis is not present it may suggest alternative diagnoses, such as small bowel obstruction, pelvic inflammatory disease, renal colic, etc.
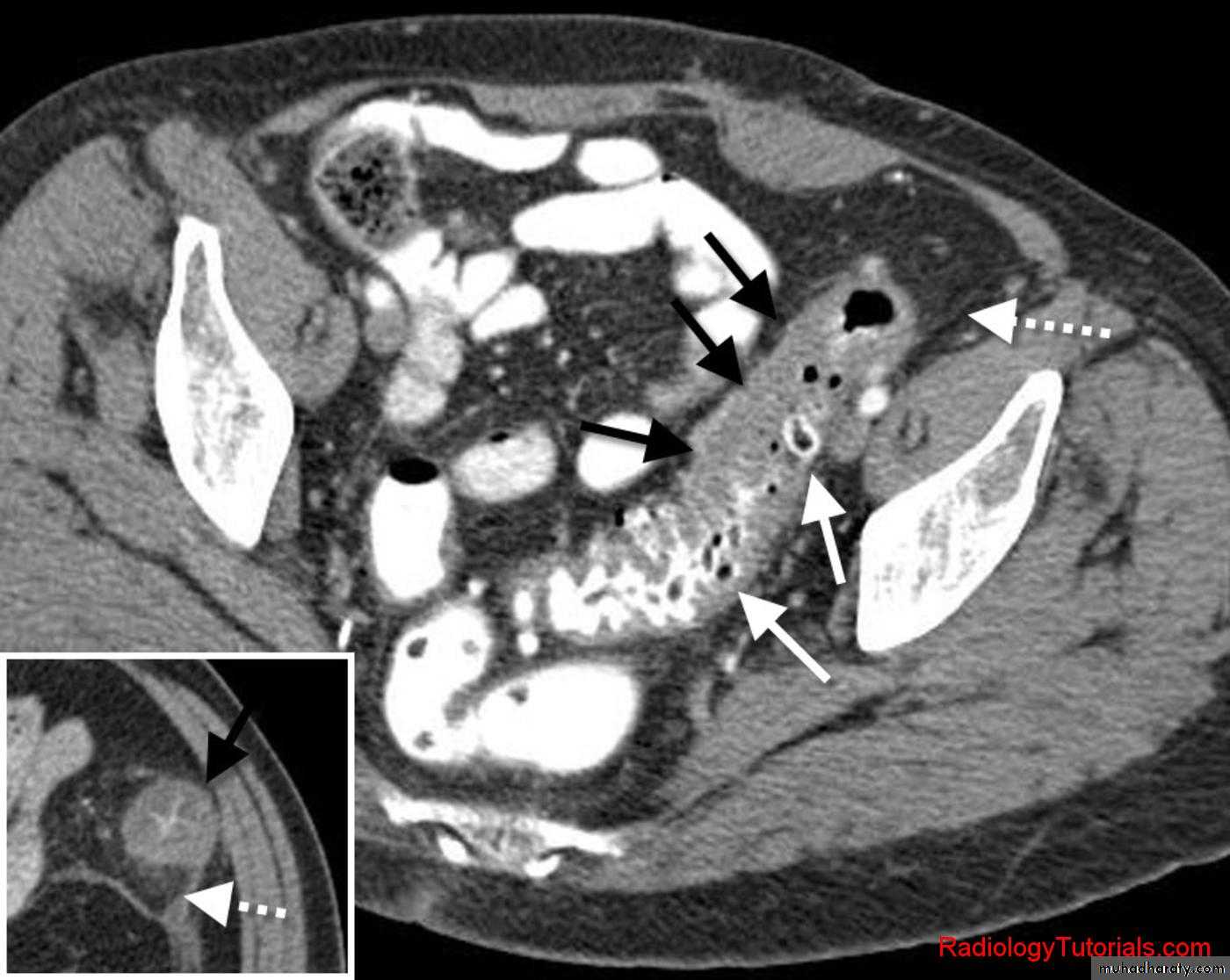
CT signs of acute diverticulitis include
• Localized bowel wall thickening• Soft tissue stranding or haziness in pericolonic fat.
• Gas in the bladder may indicate formation of a colovesical fistula.
• Abscess.
Epigastric pain
Acute pancreatitis usually presents with severe acute epigastric pain.
Acute pancreatitis
• Risk factors for the development of acute pancreatitis include heavy alcohol intake and the presence of gallstones.
• Initial evaluation for suspected pancreatitis consists of biochemical tests, including amylase and lipase levels.
• US is initial investigation of choice.
• CT is the imaging investigation of choice for the diagnosis of acute pancreatitis.
• CT signs in early pancreatitis may precede serum enzyme elevations.
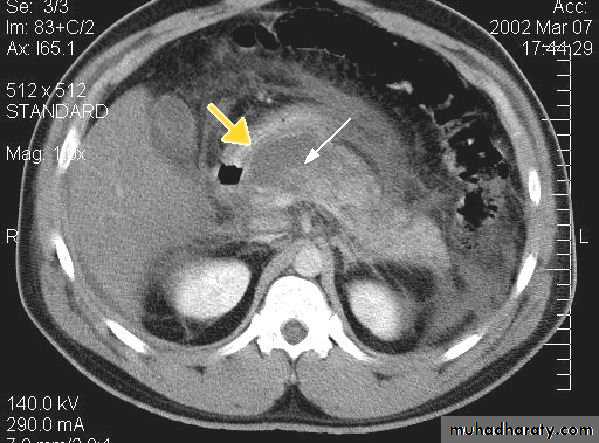
CT signs of acute pancreatitis include
• Diffuse or focal pancreatic swelling
• Indistinct pancreatic margins
• Thickening of surrounding fascial planes.
• CT performed during infusion of contrast material can differentiate necrotic non-enhancing tissue from viable enhancing tissue; the presence of pancreatic necrosis is associated with a significantly increased mortality.
• Complications of pancreatitis, such as phlegmon, abscess and pseudocyst, splenic vein thrombosis, arterial erosion and pseudoaneurysm are well shown on CT.
• Pseudocyst could be thick or thin walled cysts of variable sizes.
• Many pseudocysts resolve in the weeks following an attack of acute pancreatitis, some persist and may need surgical or percutaneous drainage.
• CT can also be used to guide percutaneous aspiration and drainage procedures.
• Indications for percutaneous drainage of a fluid collection associated with acute pancreatitis include:• Suspected abscess
• Enlarging cyst on follow-up imaging
• Symptoms due to mass effect on adjacent structures.
• US is usually indicated in patients with acute pancreatitis, primarily to search for gallstones and to assess the biliary tree.
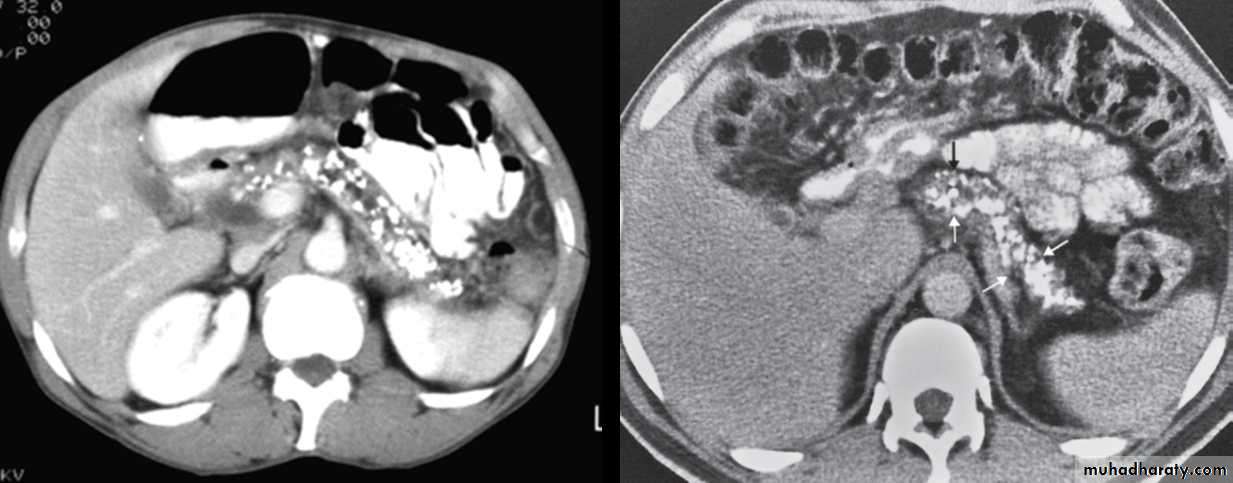
Chronic pancreatitis
• It result in fibrosis, calcifications, and ductal stenosis and dilatation.
• Pseudocysts are seen.
• The calcification often recognizable on plain x-ay film, but more obvious on CT.
• The gland may enlarge focally or generally.
• The gland may atrophied.
• The pancreatic duct may be enlarged and irregular.
Generalized abdominal pain
Acute mesenteric ischemia
• Acute mesenteric ischemia (AMI) is caused by abrupt disruption of blood flow to the bowel.
• AMI usually presents with sudden onset of severe abdominal pain and bloody diarrhea.
• The goal of diagnosis and therapy in AMI is prevention or limitation of bowel infarction.
• Prompt diagnosis requires a high index of suspicion and early referral for angiography in patients with clinical evidence of AMI.
• The most common causes of AMI are superior mesenteric artery (SMA) embolus, SMA thrombosis and non-occlusive SMA vasospasm.
• In the case of SMA embolus, the patient may have a history of cardiac disease, previous embolic event or simultaneous peripheral artery embolus.
• SMA thrombosis is usually associated with an underlying stenotic atherosclerotic lesion in the SMA.
• Depending on the cause and clinical situation, particularly the presence or absence of peritoneal signs, treatment will be immediate surgery or interventional radiology.
• Interventional radiology consists of thrombolysis via a selective catheter, which may be followed by angioplasty of any underlying stenosis or papaverine infusion for SMA vasospasm.
Renal colic and acute flank pain
• Acute flank pain describes pain of the posterolateral abdomen from the lower thorax to the pelvis.
• The most common cause of acute flank pain is ureteral obstruction caused by an impacted renal calculus. For this reason, the terms ‘acute flank pain’ and ‘renal colic’ are often used interchangeably.
• The term ‘acute flank pain’ more accurately reflects the fact that non-renal causes may produce similar symptoms to genuine renal colic.
• In the patient with acute flank pain, initial assessment is directed towards confirming or excluding urinary tract obstruction secondary to a ureteric calculus.
• Other renal causes of acute flank pain include acute pyelonephritis, transitional cell carcinoma (TCC) of the ureter causing obstruction and ‘clot colic’, i.e. ureteric colic due to a blood clot complicating hematuria.
• Non-renal causes of acute flank pain include appendicitis, torsion or hemorrhage of ovarian cyst, diverticulitis, inflammatory bowel disease and pancreatitis.
• Renal colic diagnosis is usually confirmed by imaging modalities.
• US should be used as the first imaging modality in patients with renal colic.• US allows correct diagnosis in most cases without using radiation It is a portable, non-invasive and non-expensive imaging technique.
• CT without contrast enhancement is the imaging test of choice for acute flank pain.
• Imaging diagnosis of renal colic is based on the detection of ureteral stones.
• CT is the most accurate imaging technique to identify ureteral stone size and position.
• Virtually all renal stones are identified on CT including cystine, urate, xanthine and matrix stones, which are generally not seen on AXR. The only exceptions are stones due to crystal precipitation in HIV patients on indinavir medication.
• CT signs of urinary tract obstruction:
• Dilatation of the ureter above the calculus• Dilatation of renal pelvis and collecting system
• Soft tissue stranding in the perinephritic fat due to distended lymphatic channels.
A major advantage of CT is that non-renal causes of acute flank pain may also be diagnosed
• Radiograph of kidneys, ureters and bladder (KUB) refers to a supine AXR done to diagnose and follow up renal or ureteric calculi.
• Where possible, follow-up of ureteric or renal calculi should be with KUB, as this will result in less radiation exposure than a repeat CT.
• KUB may also be performed after external shock wave lithotripsy or percutaneous calculus extraction to check for residual fragments in the urinary tract.
• Ninety per cent of renal calculi contain sufficient calcium to be radio-opaque, i.e. visible on KUB.
• Cystine stones (3 %) are faintly opaque and may be visualized on KUB with difficulty.
• Urate stones (5 %) are lucent, i.e. not visible on KUB.
• Rare xanthine and matrix stones are also lucent.
• Note that opacities seen on KUB/AXR thought to be renal or ureteric calculi need to be differentiated from other causes of calcification, such as arterial calcification, calcified lymph nodes and pelvic phleboliths (Phleboliths are small, round calcifications in pelvic veins. Phleboliths are extremely common, and are visible on AXR in most adults).