pulpitis
Air r.i. is 1.00Water r.i. is 1.33
Enamel r.i. is 1.62
Refractive index
1-dental caries.
2-traumatic exposure of the pulp.3-fracture of the crown or cusp.
4-cracked tooth syndrome.
5-thermal or chemical irritation.
Causes of pulpitis
Traumatic exposure. The pulp has been exposed during cavity preparation.
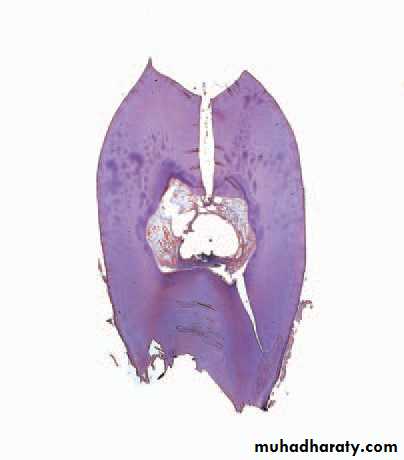
Cracked tooth. The pulp died beneath this crack which was undetectedclinically but which has opened up after decalcifi cation of the tooth.
Acute closed pulpitis.
Chronic closed pulpitis.Open pulpitis.
Chronic hyperplastic pulpitis(pulp polyp).
(gingival polyp)?
Pathology of pulpitisPulpal hyperaemia. While bacteria are still some distance from thepulp, acid permeating along the dentinal tubules gives rise to hyperaemia,oedema and a light cellular infl ammatory infi ltrate in the pulp.
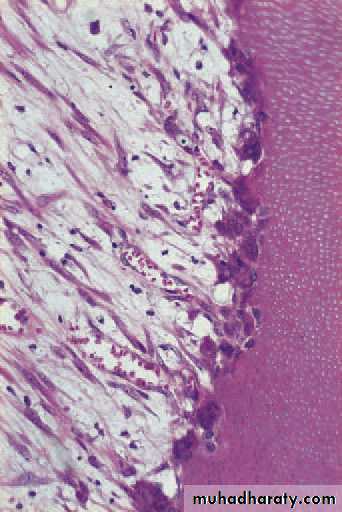
Early acute pulpitis showingthe widely dilated pulp vessels and earlyemigration of leucocytes. There is patchyoedema of the dying odontoblast layer.
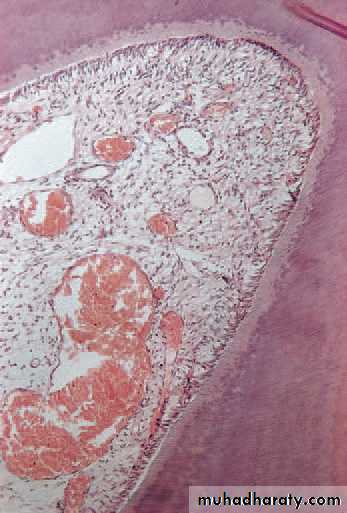
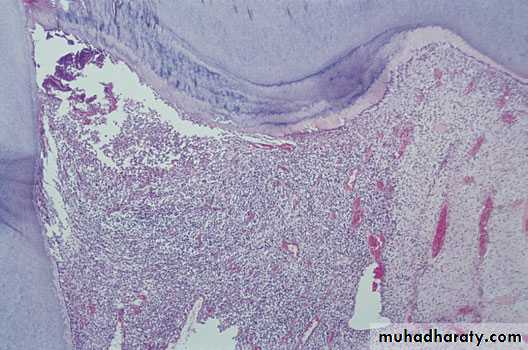
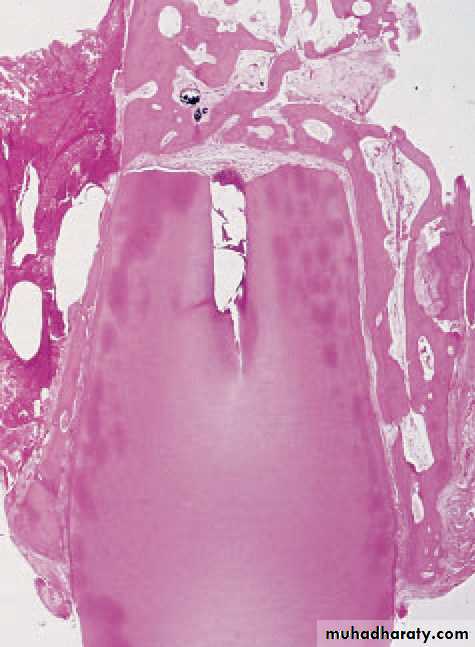
Acute pulpitis. Low-power view showing occlusal caries penetratingto the pulp through a layer of reactionary dentine. There is acuteinfl ammation localised to the pulp horn.
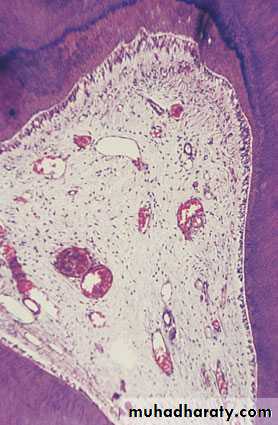
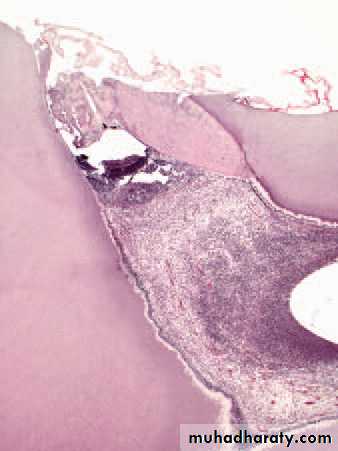
Acute pulpitis. Beneath the carious exposure (top right) a denseinfl ammatory infi ltrate is accumulating. More deeply, the pulp is intenselyhyperaemic.
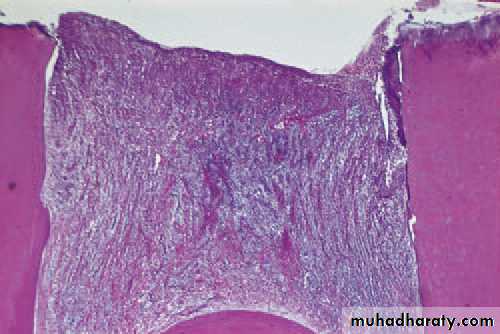
Chronic pulpitis as indicated by the tertiary (reactionary) dentineformation. A predominantly chronic (mononuclear) inflammatory infiltrate isgradually extending across and has largely replaced the normal coronal pulp tissue.
Calcifi c barriers. (A) Another pulpitisand formation of a thick calcifi c barrier, butwith an abscess immediately below it. Therest of the pulp is inflamed.
(B) This higherpowerview of another barrier induced bypulp capping shows the calcifi c barrier inmore detail, in particular its irregular structureand failure to hold back the infection.
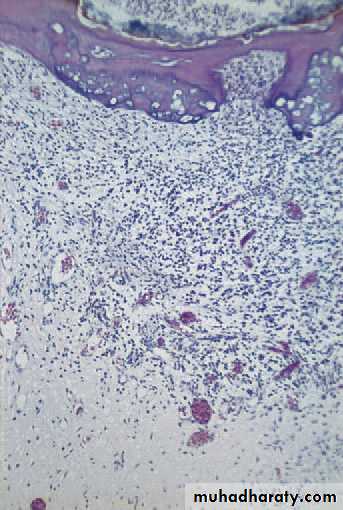
Open pulpitis. Beneath the wide exposure the pulp has survivedin the form of granulation tissue with the most dense infl ammatory infiltrate beneath the open surface.
Pulpitis is caused by infection or irritation of the pulp.
Severe stabbing pain in a tooth,triggered by hot or cold food or starting spontaneously,indicates ACUTE IRREVERSIBLE pulpitis.
Pulp pain is poorly localized,WHY?
CHRONIC PULPITIS is often symptomless,why?
Key features of pulpitis
Untreated pulpitis usually leads to DEATH of the pulp and spread of infection to the periapical tissue.
Can chronic change to acute?
Key features of pulpitis1-
2-
3-
4-
5-
Treatment options for pulpitis
Pulp capping. The procedure has allowed the pulp to surviveuntil reactionary dentine has proliferated greatly beside the exposure.Failure of the procedure is indicated by the infl ammatory cells concentratedbelow the opening.Local periapical periodontitis is____?
Chronic marginal periodontitis is_____?Periapical periodontitis
Infection.Trauma.acute calcific degeneration.
Chemical irritation.
Causes of apical periodontitis is
Symptoms include:
First tooth is uncomfortableThen becomes increasingly tender.
Hot or cold substances do not cause pain , Unless in multi- rooted teeth sometimes.
Then pain becomes throbbing.
Unlike PULPITIS,the pain is localized,
Acute apical periodontitis
Regional lymph nodes may be enlarged and tender.
But general symptoms are slight or absent.Further spread of infection can cause inflammation of surrounding bone(osteomyelitis) ?or (cellulitis)?
What is Ludwig’s angina?
Acute apical periodontitis
Suppuration.
Regional lymphadenopathy.Spreading of infection.
Possible complications of apical periodontitis
Possible complications :
1-periapical granuloma.2-radicular cyst.
3-suppuration and sinus formation.
4-acute exacerbations
Chronic apical periodontitis
Oedema due to acute apical periodontitis. An acute periapicalinfection of a canine has perforated the buccal plate of bone causingoedema of the face; this quickly subsided when the infection was treated.
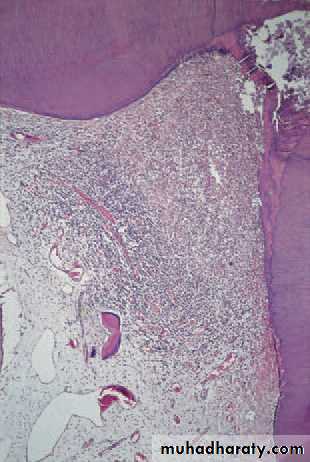
Acute apical periodontitis. In this early acute lesion, inflammatorycells, mainly neutrophils, polymorphonuclear leucocytes, are seen clusteredaround the apex of a non-vital tooth. The infl ammatory cells are spreadingaround and into bone and there has not yet been time for significant bone resorption to develop.
Low-power detail shows the effects of apicectomy. The chronicinflammatory reaction has entirely cleared. New bone has formed toreplace the excised apex and there is a condensation of connective tissue across the deep end of the root canal filling.
persistent skin sinus from a lower incisor rendered non-vitalby a blow some time previously. This young woman was seen and treatedunsuccessfully for 2 years by her doctor, surgeons and dermatologists before anyone looked at her teeth.
Epithelial proliferation in an apical granuloma. Inflammationinduces proliferation of odontogenic epithelium in rests of Malassez. This change may lead to cyst formation.
Non-vital incisor teeth, in this case as a result of trauma.Haemorrhage and products of autolysis of the pulp discolour the dentine and darken the teeth.
Infl ammatory resorption of the root apex induced by periapicalperiodontitis resulting from the non-vital pulp.
Resorption during periapical periodontitis. Active osteoclasticresorption of dentine is continuing in the presence of infl ammatory exudate.This is a common change but usually minor in extent.
• Periapical periodontitis. The most common cause, but is usually
slight• Impacted teeth pressing on the root of an adjacent tooth
• Unerupted teeth. Over the course of years these may undergo
resorption or hypercementosis, or both
• Replanted teeth. These are sometimes rapidly and grossly
resorbed
• Neoplasms. Resorption of related teeth is a typical sign of an
intraosseous neoplasm such as an ameloblastoma
• Idiopathic. Peripheral and internal
Important causes of resorption of permanent teeth
Define
Are they always single?Attrition,abrasion,and erosion
for your attention
Thank you