Management of SLE
Investigations• Antibody
• Antigen/epitope
• Prevalence (%)
• Clinical and other associations
• Intracellular
• DNA
• dsDNA
• (ssDNA)
40–90
• present in renal eluates. Pathogenic cross-reactions: LAMP/glomerular heparin sulfate
• Histone
• H1, 2A, 2B, 3, 4
• 30–80
• Drug induced lupus
• Sm
• A, B/B′
• Overall ~35
• SLE specific Afro-Caribbean
• U1RNP
• ribonucleoprotein
• 20–35
• Mild disease
• Ro/SS-A
• protein bound to cytoplasmic RNA )
• 25–40
• Renal involvement
• Antibody
• Antigen
• epitope
• Prevalence (%)
• Clinical and other associations
• Intracellular (Cont.)
• La/SS-B
• 10–15• Secondary Sjogren’s (2° SS)
• Heatshock proteins
• 40
• IgM > IgG
• Cell membrane
• Cardiolipin• Phospholipids
• DNA
• Recurrent abortion
• Thrombosis
• Red cell Platelet
• Non-Rh related
• Haemolytic anaemia
• ITP
Non-pharmacological management
General measures which may be useful for patients with SLE include the avoidance of excessive sunlight.This is particularly important in fair-skinned people since solar radiation may not only cause photosensitive rash, but also a more general flare of symptoms.
Rest as appropriate, a low-fat diet with added fish oil, and avoidance of oestrogen-containing contraceptive pills are also advised.
Vaccinations apart from 'live' vaccines in patients on greater than 10 mg prednisolone and/or immunosuppressives are safe but the use of hormone replacement in patients past the menopause is still controversial
Pharmacological management
Patients with SLE are treated with four main groups of drugs, often in combination. These are:Non-steroidal anti-inflammatory drugs (NSAIDs),
Antimalarials
Corticosteroids
Cytotoxic drugs.
Drug therapy in systemic lupus
NSAIDAntimalarial
Corticosteroids
Cytotoxic agents
Malaise
+
+
+
−
Fever
+
−
+
−
Serositis
+
−
+
−
Arthralgia
+
+
+
−
Arthritis
+
+
+
+
Myalgia
+
+
+
−
Myositis
−
−
+
+
Malar/discoid rash
−
+
+
−
• Pneumonitis
• −
• −
• +
• +
• Carditis
• −
• −
• +
• +
• Vasculitis
• −
• −
• +
• +
Drug therapy in systemic lupus
NSAID
AntimalarialCorticosteroids
Cytotoxic agents
CNS disease
−
−
? a
?
Renal
−
−
+
+
Haemolytic anaemia
−
−
+
+
Thrombocytopaenia
−
−
+
+
Raynaud's
−
−
?
?
Alopecia
−
−
?
?
a Widely prescribed but doubts remain that steroids are beneficial in many cases.
Note: + = usually beneficial; − = not beneficial; ? = dubious/controversial.
Recommendations for drug usage in lupus
Recommendations for drug usage in lupus
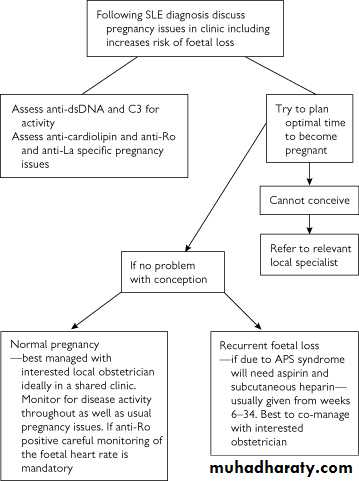
Recommendations for drug usage in lupusManagement in special situations-Pregnancy
Prognosis and survival
Studies on duration of disease and overall survival rates have frequently been confounded by the numbers of patients lost to follow-up and inadequate attention paid to the ethnic group, age of onset, and socio-economic status of individual patients.With these possible confounding factors in mind, and the division of lupus patients into those with overt nephritis and those without, it is reasonable to state that the five year survival in lupus is presently 90 per cent or greater,
but at 15 years only 60 per cent of those with nephritis will still be alive compared to around 85 per cent of those without nephritis.
In the United States, it has been claimed that black lupus patients, males, those from poorer socio-economic groups and possibly children, have poorer survival, especially if nephritis is present.
Prognosis and survival
It has also been suggested that there exists a bimodal mortality curve.Patients who die within 5 years usually have very active disease, with a requirement for substantial doses of steroids and other immunosuppressives.
Those patients dying much later tend to do so from cardiovascular disease and possibly infection. Overall, most lupus patients die from active generalized disease, malignancy, sepsis, nephritis, and cardiovascular disease.