Ulcerated vesicular & bullous diseases
Vesicular & bullous lesions which affect the mouth tend to break down rapidly & present clinically as areas of ulcerations or erosions owing to the effect of saliva & oral musculature .Classifications:
1-Infective
Herpes simplex virus
Primary herpes or acute herpetic gingiva stomatitis
Recurrent herpes or secondary herpetic gingiva stomatitis or cold sore or recurrent herpes labialis
Varicella-Zoster Virus Infection
chickenpox (varicella)
shingles (herpes zoster [HZ]).
Coxsackie virus Infections
Herpangina
hand ,foot- and-mouth disease
Acute lymhponodular pharyngitis
2-Auto-immune
Pemphigus
Pemphigoid
3-Miscellaneous
Bullous lichen planus
Epidermolysis bullosa
Herpes virus Infections:
The Herpes viridae family of viruses contains nine different viruses that are pathogenic in humans. I n general, infections above the waist are caused by HSV-1and those below the waist by HSV-2, although with changing sexual practices, it is not uncommon to culture HSV-2 from oral lesions and vice versa. The primary infection, which occurs on initial contact with the virus, is acquired by inoculation of the mucosa, skin, and eye with infected secretions.
The virus then travels along the sensory nerve axons and establishes chronic, latent infection in the sensory ganglion(such as the trigeminal ganglion).Extra neuronal latency( HSV remaining latent in cells other than neurons such as the epithelium) may play a role in recurrent lesions of the lips. Recurrent HSV results when HSV-1 reactivates at latent sites and travels centripetally to the mucosa or the skin, where
it is directly cytopathic to epithelial cells, causing recrudescent HSV infection in the form of localized vesicles or ulcers. The most common sites of infection are the oral and genital mucosa and the eye. HSV infection of the cornea (keratitis) is a major cause of blindness in the world. HSV-1 or -2may cause herpes whitlow, an infection of the fingers when virus is inoculated into the fingers through a break in the skin.
This was a common occupational hazard (including within the dental profession)
Other HSV-1 infections include herpes encephalitis, HSV esophagitis, and HSV pneumonia. HSV is an important etiologic agent in erythema multiform, HSV has been recovered in the endoneurial fluid of 77% of patients with Bell's palsy. Treatment with antiviral therapy resulted in better outcomes, further supporting the concept of HSV involvement in the pathogenesis of Bell's palsy.
Immunocompromised Hosts
Recurrent InfectionPrimary Infection
Type of Virus
Unusual ulcers at any mucocutaneous site usually large and persistent
Herpes labialis intraoral ulcers, Keratoconjunctivitis Genital and skin lesion,
Gingivostomatitis, Keratconjunctivitis, Genital and skin lesion
Herpes simplex virus 1
Unusual ulcers at any mucocutaneous site usually large and persistent; disseminated infection,
Genital and skin lesionsGingivostomatitis, Aseptic meningitis
Genital and skin lesions, GingivostomatitisKeratoconjunctivitis, Neonatal infectionsAseptic meningitis
Herpes simplex virus 2
Disseminated infection
Zoster (shingles
Varicella (chickenpox
Varicella-zoster virus
Retinitis, gastroenteritis hepatitis, severe oral ulcers
Infectious mononucleosis, Hepatitis, Congenital disease
Cytomegalo virus
Hairy leukoplakia in AIDs patients, lymphoproliferative disorders
Infectious mononucleosis, Hepatiti, Encephalitis, African burkets lymphoma, Nasopharyngeal carcinoma,
Epstein-Barr virus
Fever; bone marrow suppression
Multiple sclerosis, Roseola infantum, Otitis media, Encephalitis
Human herpesvirus 6Roseola infantum
Human herpesvirus 7Kaposi’s sarcoma in AIDs patients, lymphoproliferative disorders; bone marrow suppression
Infectious mononucleosis, Febrile exanthema
Human herpesvirus 8Mucocutaneous lesions, Encephalitis
Simian herpesvirus BHSV1, HSV2, and varicella-zoster
Are viruses that are known to cause oral mucosal disease. Classically, HSV1 causes a majority of cases of oral ,pharyngeal infection, meningo encephalitis, &dermatitis above the waist; HSV2 is implicated in most genital infections. Both types can cause Primary Or Recurrent Infection of either the oral or the genital area, and both may cause recurrent disease at either site. Primary infection may also occur concurrently in both oral and genital sites from either HSV1 or HSV2, although HSV1 recurs more frequently in the oral region and HSV2 more frequently in the genital region. Humans are the only natural reservoir of HSV infection, and spread occurs by direct intimate contact with lesions or secretions from an asymptomatic carrier. This latter method of spread of HSV is common; between [2- 9%] of asymptomatic individuals shed HSV in saliva or genital secretions. Latency,A characteristic of all herpes viruses, occurs when the virus is transported from mucosal or cutaneous nerve endings by neurons to ganglia where the HSV viral genome remains present in a non-replicating state. Reactivation of the latent virus occurs when HSV switches to a replicative state; this can occur as a result of a number of factors including peripheral tissue injury from trauma or sunburn, fever, or immune suppression &menstruation .
CarcinogenesisThere is evidence linking HSV to carcinogenesis. Epidemiologic studies have demonstrated an increased incidence of HSV2 serum antibodies or positive HSV2 cultures in patients with cervical carcinoma .
Primary herpetic stomatitis
This is a common viral infection caused by HSV1. It affects the mouth, pharynx & skin . It is most often seen in children, although young adults are sometimes affected but rarely occur before 6 month due to maternal antibodies .Clinical manifestations:
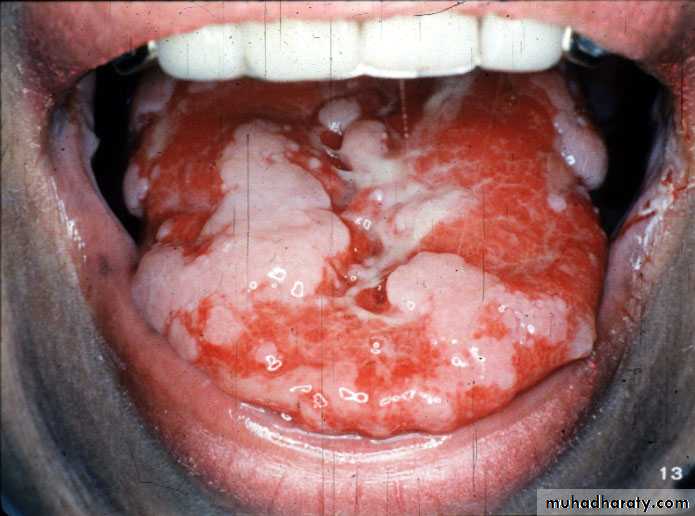
Primary herpes manifests as an acute illness with fever, irritability, headache & lymphadenopathy . Typically, there are initial symptoms of malaise associated with aches & a sore throat followed after (2-3) days by multiple small oral vesicles which rapidly breakdown to form well defined yellow base ulcer with a red margin . They may affect hard palate, tongue, lips & circum oral skin. In addition to the ulcerations, the whole mucosa is bright-red & painful with a marked edematous gingivitis . The lesions are self-limiting & usually disappear in ( 7-10) days .
Multifactorial ulceration present on movable & bound mucosa . Note the intensely erythematous gingiva without significant plaque
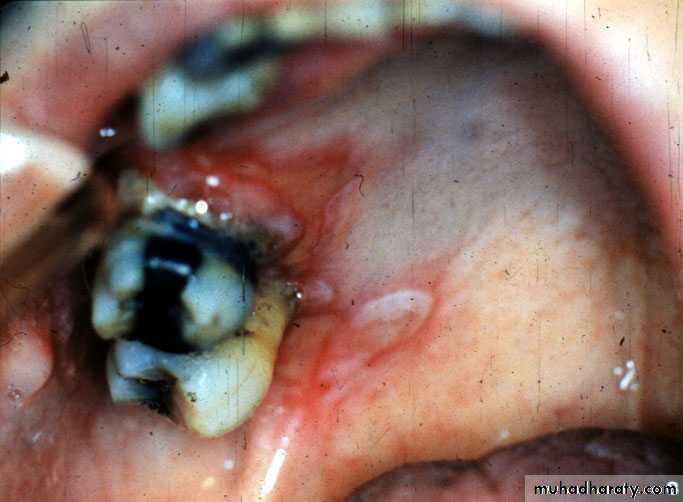
Palatal mucosa demonstrating numerous small ulceration that tend to cluster . Not the significant erythema & ulceration of the palatal gingiva
Diagnosis of herpes :
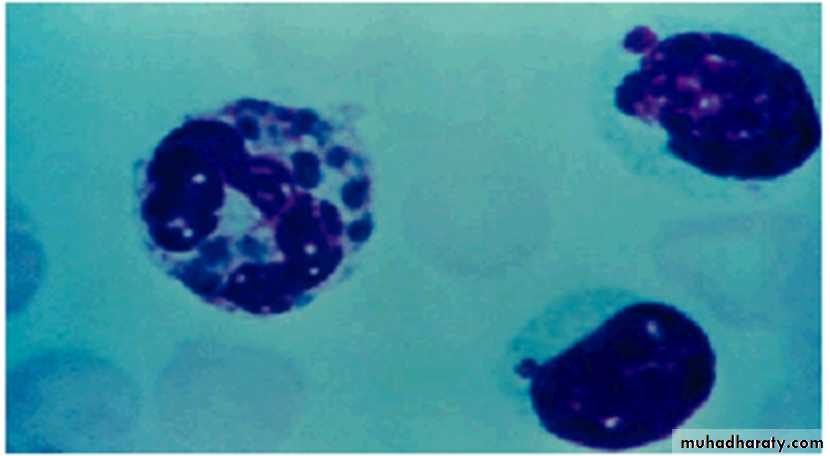
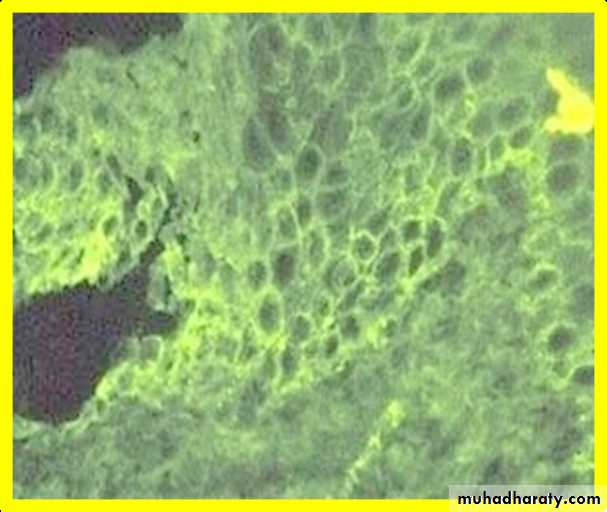
Cytology: For cytology, a fresh vesicle can be opened and a scraping made from the base of the lesion and placed on a microscope slide. The slide may be stained with [Giemsa, Wright’s or Papanicolaou’s stain ]and searched for multi nucleated giant cells & ballooning degeneration of the nucleus.Cytology smear stained with Giemsa, demonstratingmultinucleated giant cells
H SV Isolation: Isolation and neutralization of a virus in tissue culture is the most positive method of identification and has a specificity and sensitivity of 100%. A clinician mustremember that isolation of HSV from oral lesions does not necessarily mean that HSV caused the lesions. Patients who have lesions from other causes may also be asymptomatic shedders of HSV.
Antibody TitersSerum specimen should be obtained within 3or 4 days of the onset of symptoms. The absence of detectable antibodies plus the isolation of HSV from lesions is compatible with the presence of a primary HSV infection. Antibody to HSV will begin to appear in a week and reach a peak in 3weeks. A convalescent serum can confirm the diagnosis of primary HSV infection by demonstrating at least a fourfold rise in anti-HSV antibody. If anti-HSV antibody titers are similar in both the acute and convalescent sera, then the lesions from which HSV was isolated were recurrent lesions.Recurrent herpes
It manifests as attenuated version of primary infection with no systemic symptoms. It is thought that there is a latent virus situated in the trigeminal ganglion which is reactivated by inciting factors such as:-
Sun exposure
Menstruation
Febrile conditions
Clinical feature :
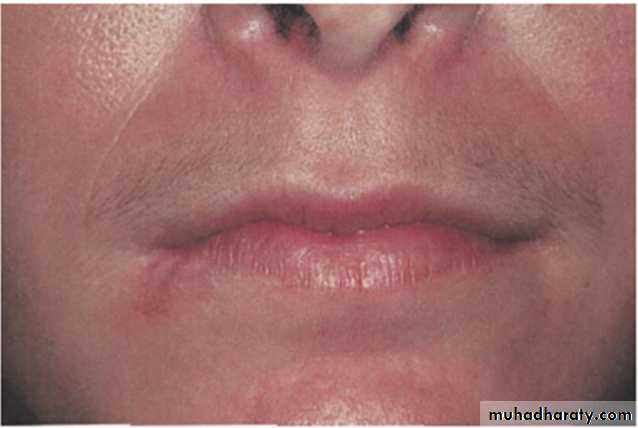
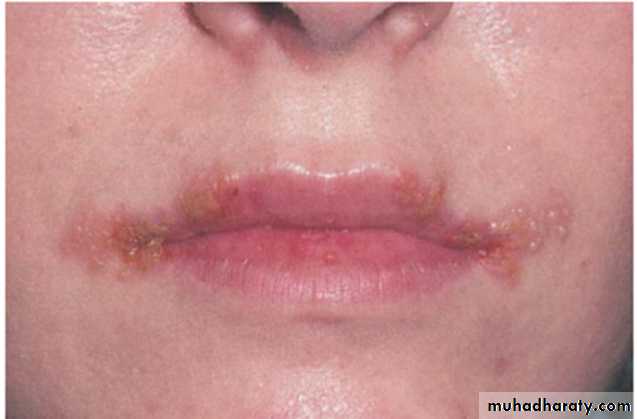
Early lesion characterized by Area of erythema of the right side of the lower lip that has been present for less than one day .Followed by Multiple fluid-filled vesicles and erythema of the right side of the lower lip . This picture depicts the same patient 24 hours after
Wide spread bilateral fluid-filled vesicles of both upper & lower lips . Many of the vesicles have ruptured & formed crusts
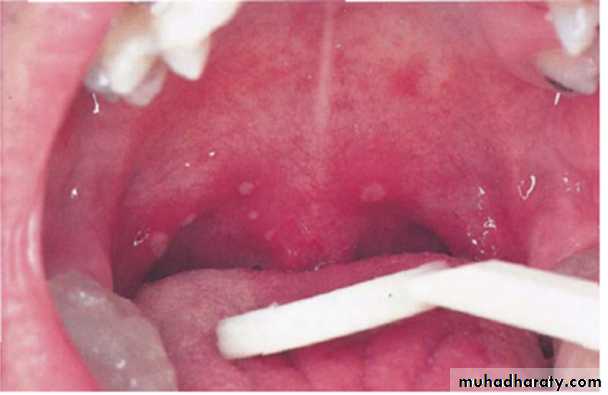
A cluster of multiple small ulceration of the hard palate
Treatment:
A significant advance in the management of herpes simplex infections was the discovery of acyclovir,which has no effect on normal cells but inhibits DNA replication in HSV-infected cells. Acyclovir has been shown to be effective in the treatment of primary oral HSV in children when therapy was started in the first 72 hours. Acyclovir significantly decreased days of fever, pain, lesions, and viral shedding .Newer antiherpes drugs are now available, including valacyclovirand famciclovir. The advantage of the newer drugs is increased bioavailability, allowing for effective treatment with fewer doses.
Milder cases can be managed with supportive care only.
Routine supportive measures include
aspirin or acetaminophen for feverfluids to maintain proper hydration and electrolyte balance.
If the patient has difficulty eating and drinking, a topical anesthetic may be administered prior to meals.
Dyclonine hydrochloride 0.5% has been shown to be an excellent topical anesthetic for the oral mucosa.
If this medication is not available, a solution of diphen hydramine hydrochloride 5 mg/mL mixed with an equal amount of milk of magnesia also has satisfactory topical anesthetic properties.
Infants who are not drinking because of severe oral pain should be referred to a pediatrician for maintenance of proper fluid and electrolyte balance.
Antibiotics are of no help in the treatment of primary herpes infection, and use of corticosteroids is contraindicated.Future therapy may include prevention of the infection with use of a genetically disabled HSV vaccine.
Oral lesion should be treated with topical acyclovir cream 5% five times daily
Varicella-Zoster Virus Infection
VZV is a herpes virus, and, like other herpes viruses, it causes both primaryand recurrent infection and remains latent in neurons present in sensory ganglia. VZV is responsible for two major clinical infections of humans
chickenpox (varicella)
shingles (herpes zoster [HZ]).
Chickenpox is a generalized primary infection that occurs the first time an individual contacts the virus. After the primary disease is healed, VZV becomes latent in the dorsal root ganglia of spinal nerves or extra medullary ganglia of cranial nerves. A child without prior contact with VZV can develop chickenpox after contact with an individual with HZ.
Clinical Manifestations:
ChickenpoxIs a childhood disease characterized by mild systemic symptoms and a generalized intensely pruritic eruption of maculopapular lesions that rapidly develop into vesicles on an erythematous base. Oral vesicles that rapidly change to ulcers may be seen, but the oral lesions are not an important symptomatic, diagnostic, or management problem.HZCommonly has a prodromal period of 2 to 4 days, when shooting pain, paresthesia, burning, and tenderness appear along the course of the affected nerve. Unilateral vesicles on an erythematous base then appear in clusters, chiefly along the course of the nerve, giving the characteristic clinical picture of shingle dermatome involvement. Some lesions spread by viremia occur outside the dermatome. The vesicles turn to scabs in 1 week, and healing takes place in 2 to 3 weeks. The nerves most commonly affected with HZ are C3, T5, L1, L2, and the first division of the trigeminal nerve
Diagnosis of HZ:
Clinical feature ; lesion along the distribution of the involved nerve.Fluorescent antibody test .
PCR
The most common complication of HZ
Post herpetic neuralgia ;which is defined as pain remaining for over a monthafter the mucocutaneous lesions have healed, although some clinicians do not use the term post herpetic neuralgia unless the pain has lasted for at least 3 months after the healing of the lesions. The overall incidence of post herpetic neuralgia is [12- 14%], but the risk increases significantly after the age of 60years, most likely due to the decline in cell-mediated immunity.HZ of the geniculate ganglion called Ramsay Hunt syndrome, It is a rare form of the disease characterized by
Bell’s palsy .
unilateral vesicles of the external ear.
vesicles of the oral mucosa .
Herps zoster ophthalmicus ; It is serious complication of the HZ because it may lead to blindness &use of I.V acyclovir to prevent such complication
Treatment of HZ:
Intra Oral Ulceration Unilateral
Antiviral drugs such as acyclovir 800mg 5 times daily & symptomatic treatment.
Facial lesions of herpes zoster involving the third division of the trigeminal nerve
Facial lesions of herpes zoster involving the second divisionof the trigeminal nerve
Coxsackievirus InfectionsCoxsackie viruses are (RNA) entero viruses . Coxsackie viruses have been separated into two groups A and B. There are 24 known types of coxsackie virus group A and 6types of coxsackie virus group B. These viruses cause hepatitis, meningitis, myocarditis, pericarditis, and acute respiratory disease.Three clinical types of infection of the oral region that have been described are usually caused by group A coxsackieviruses:
herpangina
hand ,foot, and-mouth disease
acute lymphonodular pharyngitis.
Herpangina
Coxsackievirus A4 has been shown to cause a majority of cases of herpangina. Unlike herpes simplex infections, which occur at a constant rate, herpangina frequently occurs in epidemics that have their highest incidence from June to October. The majority of cases affect young children ages 3 through, but infection of adolescents and adults is not uncommon.Clinical Manifestations: After a 2- to 10-day incubation period, the infection begins with generalized symptoms of fever, chills, and anorexia. The patient complains of sore throat, dysphagia, and occasionally sore mouth. Lesions start as macules, which quickly evolve into papules and vesicles involving the posterior pharynx, tonsils, faucial pillars, and soft palate. Within 24 to 48 hours, the vesicles rupture, forming small 1 to 2 mm ulcers.
Diagnosis :
Clinical diagnosis , lesion are summed in posterior part of the oral mucosa .The disease is usually mild and heals without treatment in 1 week. It is self-limiting & only supportive care is indicated .Multifocal area of ulceration & erythema of the soft palate . The patient report sore throat , fever , headache and vomiting
Acute Lymphonodular Pharyngitis
This is a variant of herpangina caused by coxsackievirus A10. The distribution of the lesions is the same as in herpangina, but yellow-white nodules appear that do not progress to vesicles or ulcers. The disease is self-limiting, and only supportive care is indicated. Symptomatic treatment directed toward antipyretic & topical anesthetic , also patient should be given proper hydration .Tow pink nodules immediately superior to the uvula with lateral adjacent erythema of the soft palat
Hand-Foot-And-Mouth Disease
Is caused by infection with coxsackievirus A16 .In a majority of cases, the disease is characterized byLow-Grade Fever
Oral Vesicles And Ulcers
Nonpruritic Macules & Papules
Vesicles, Particularly On The Extensor Surfaces Of The Hands and Feet. mainly the palm of the hand & sole of the feet
The oral lesions are more extensive than are those described for herpangina, and lesions of the hard palate, tongue, and buccal mucosa are common.
Treatment: self-limiting disease & supportive care only is indicated
Multiple ulcer of the lateral tongue
In a 3year-old child who also had
Vesicular lesion of the fingers and toes
Multiple vesicles and erythema of the fingers in same patient
Pemphigus
Pemphigus is a potentially life-threatening disease that causes blisters and erosions of the skin and mucous membranes. These epithelial lesions are a result of autoantibodies that react with desmosomal glycoproteins that are present on the cell surface of the keratinocyte. The immune reaction against these glycoproteins causes a loss of cell-to-cell adhesion, resulting in the formation of intraepithelial bullae. The highest incidence occurring in the fifth and sixth decades of life, although rare cases have been reported in children and the elderly. Pemphigus occurs more frequently in the Jewish population in whom studies have shown a strong association with major histocompatibility complex (MHC) class II alleles HLA-DR4 and DQW3. Familial pemphigus has also been reported.The major variants of pemphigus:
pemphigus vulgaris (PV)
pemphigus vegetans
pemphigus foliaceus
pemphigus erythematosus,
Paraneoplastic pemphigus (PNPP)
drug –related pemphigus.
Pemphigus vegetans is a variant of pemphigus vulgaris, and pemphigus erythematosus is a variant of pemphigus foliaceus. Each form of this disease has antibodies directed against different target cell surface antigens, resulting in a lesion forming in different layer of the epithelium. In pemphigus foliaceus, the blister occurs in the superficial granular cell layer, whereas, in pemphigus vulgaris, the lesion is deeper, just above the basal cell layer. Mucosal involvement is not a feature of the foliaceus and erythematous forms of the disease.
Pemphigus Vulgaris (PV)Is the most common form of pemphigus, accounting for over 80% of cases. The underlying mechanism responsible for causing the intraepithelial lesion of PV is the binding of IgGautoantibodies to desmoglein 3, a transmembrane glycoprotein adhesion molecule present on desmosomes. The presence of desmoglein 1 autoantibodies is a characteristic of pemphigus foliaceus, but these antibodies are also detected in patients with long-standing PV. The mechanism by which antidesmoglein antibodies cause the loss of cell-to-cell adhesion is controversial. Some investigators believe that binding of the PV antibody activates proteases, whereas more recent evidence supports the theory that the PV antibodies directly block the adhesion function of the desmogleins. The separation of cells, called acantholysis, takes place in the lower layers of the stratum spinosum [ prickle cell layer] .
Clinical Manifestations :The classical lesion of pemphigus is a thin-walled bulla arising on otherwise normal skin or mucosa. The bulla rapidly breaks but continues to extend peripherally, eventually leaving large areas of denuded skin. A characteristic sign of the disease may be obtained by application of pressure to an intact bulla. In patients with PV, the bulla enlarges by extension to an apparently normal surface. Another characteristic sign of the disease is that pressure to an apparently normal area results in the formation of a new lesion. This phenomenon, called the Nikolsky sign, results from the upper layer of the skin pulling away from the basal layer. The Nikolsky sign is most frequently associated with pemphigus but may also occur in epidermolysisbullosa.
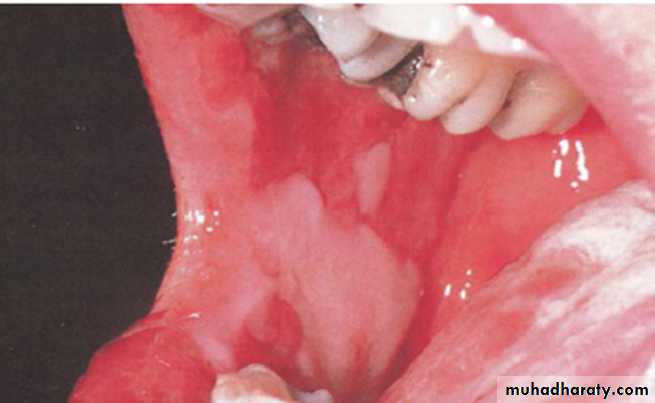
Oral Manifestations : Eighty to ninety percent of patients with pemphigus vulgaris develop oral lesions sometime during the course of the disease, and, in 60% of cases, the oral lesions are the first sign. The oral lesions may begin as the classic bulla on a non-inflamed base; more frequently, the clinician sees shallow irregular ulcers because the bullae rapidly break. Most commonly the lesions start on the buccal mucosa, often in areas of trauma along the occlusal plane. The palate and gingiva are other common sites of involvement. In some cases, the lesions may start on the gingiva and called desquamative gingivitis. It should be remembered that desquamative gingivitis is not a diagnosis in itself; these lesions must be biopsied to rule out the possibility of*Pemphigus vulgaris *Bullous pemphigoid*Mucous membrane pemphigoid*Erosive lichen planus
Laboratory Tests :
PV is diagnosed by [ Biopsy]done on intact vesicles and bullae less than 24 hours old; however, because these lesions are rare on the oral mucosa, the biopsy specimen should be taken from the advancing edge of the lesion, where areas of characteristic suprabasilar acantholysismay be observed by the pathologist. Specimens taken from the center of a denuded area are nonspecific histologically as well as clinically. Sometimes several biopsies are necessary before the correct diagnosis can be made. If the patient shows a positiveNikolsky sign, pressure can be placed on the mucosa to produce a new lesion; biopsy may be done on this fresh lesion . A second biopsy, to be studied by DIF, should be performed whenever pemphigus is included in the differential diagnosis. This study is best performed on a biopsy specimen that is obtained from clinically normal-appearing perilesionalmucosaor skin. In this technique for DIF, fluorescein-labeled antihumanimmunoglobulins are placed over the patient’s tissue specimen. In cases of PV, the technique will detect antibodies, usually IgG and complement, bound to the surface of the keratinocytes.Indirect immune fluorescent antibody tests :Have been described that are helpful in distinguishing pemphigus from pemphigoid and other chronic oral lesions and in following the progress of patients treated for pemphigus. In this technique, serum from a patient with bullous disease is placed over a prepared slide of an epidermal structure (usually monkey esophagus). The slide is then overlaid with fluorescein-tagged antihuman gamma globulin . Patients with pemphigus vulgaris have antikeratinocyte antibodies against intercellular substances that show up under a fluorescent microscope. The titer of the antibody has been directly related to the level of clinical disease.
ELISA (enzyme-linked immune sorbent assay):
Has been developed that can detect desmoglein 1 and 3 in serum samples of patients with PV. These laboratory tests should provide a new tool for the accurate diagnosis of PV and may also prove useful in monitoring the progress of the disease.
Treatment:
CorticosteroidsThe mainstay of treatment remains high doses of systemic corticosteroids,
usually given in dosages of 1 to 2 mg/kg/d.
Adjuvant Therapy
When substantial doses of steroids must be used for long periods of time, adjuvant therapy is recommended to reduce the steroid dose and their potential serious complications. The most commonly used adjuvants are immunosuppressive drugs such as mycophenolatemofetil, azathioprine [Imuran 50 mg] , or cyclophosphamide. Prednisone is used initially to bring the disease under control, and once this is achieved, the dose of prednisone is decreased to the lowest possible maintenance levels. The need for systemic steroids may be lowered further in cases of oral pemphigus by combining topical with systemic steroid therapy, either by allowing the prednisone tablets to dissolve slowly in the mouth before swallowing or by using potent topical steroid creams. Other therapies that have been reported as beneficial are
Parenteral gold therapy
Dapsone
Tetracycline
Plasmapheresis. is particularly useful in patients refractory to corticosteroids.
8-methoxypsoralen followed by exposure of peripheral blood to ultraviolet radiation (therapy described by Rook and colleagues).
PARANEOPLASTIC PEMPHIGUSPNPP is a severe variant of pemphigus that is associated with an underlying neoplasm most frequently non-Hodgkin’s lymphoma, chronic lymphocytic leukemia, are also associated with cases of PNPP. Patients with this form of pemphigus develop severe blistering and erosions of the mucous membranes and skin. Treatment of this disease is difficult, and most patients die from the effects of the underlying tumor, respiratory failure due to acantholysis of respiratory epithelium, or the severe lesions that do not respond to the therapy successful in managing other forms of pemphigus.
Paraneoplastic pemphigus , crusting hemorrhagic lip lesion
Paraneoplastic pemphigus , extensive erosive lesions of the buccal mucosa
Drug-related Pemphigus like reactions
Drugs implicated in the induction of Pemphigus like reactions areAmpicillin, procaine Penicillin, Benzyl Penicillin, Penicillamine, Piroxicam , Captopril , Diclofenac , Rifampicin , Goldsalt & Garlic .
Subepithelial Bullous DermatosesSubepithelial bullous dermatoses are a group of mucocutaneous autoimmune blistering diseases that are characterized by a lesion in the basement membrane zone. The diseases in this group include
bullous pemphigoid (BP)
mucous membrane (cicatricial) pemphigoid (MMP)
linear IgA disease (LAD)
chronic bullous dermatosis of childhood (CBDC)
erosive and bullous lichen planus.
There is significant overlap among these diseases, and the diagnosis often depends on whether the disease is categorized by clinical manifestations combined with routine histopathology or the newer techniques of molecular biology. Recent research into pathologic mechanisms is defining the specific antigens in the basement membrane complex involved in triggering the autoantibody response.
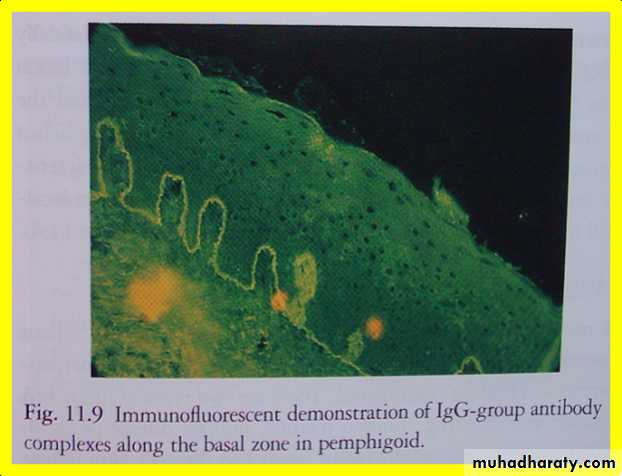
Bullous Pemphigoid:BP, which is the most common of the subepithelial blistering diseases, occurs chiefly in adults over the age of 60 years; it is self-limited and may last from a few months to 5 years. BP may be a cause of death in older debilitated individuals. BP has occasionally been reported in conjunction with other diseases , particularly multiple sclerosis and malignancy, or drug therapy, particularly diuretics. In pemphigoid, the initial defect is not intraepithelial as in PV, but it is sub epithelial in the lamina lucida region of the basement membrane . There is no acantholysis, but the split in the basement membrane is accompanied by an inflammatory infiltrate that is characteristically rich in eosinophils .
Mucous membrane pemphigoid (cicatricial pemphigoid)MMP is a chronic autoimmune subepithelial disease that primarily affects the mucous membranes of patients over the age of 50 years, resulting in mucosal ulceration and subsequent scarring. The primary lesion of MMP occurs when autoantibodies directed against proteins in the basement membrane zone, acting with complement (C3) and neutrophils, cause a subepithelial split and subsequent vesicle formation. The antigens associated with MMP are most frequently present in the lamina lucida portion of the basement membrane, but recent research has demonstrated that the identical antigen is not involved in all cases, and the lamina densa may be the primary site of involvement in some cases. The circulating autoantibodies are not the same in all cases, and subsets of MMP have been identified by the technique of immunofluorescent staining of skin that has been split at the basement membrane zone with the use of sodium chloride. The latter antigen has been identified in MMP in epiligrin (laminin 5), an adhesion molecule that is a component of the anchoring filaments of the basement membrane.
Clinical Manifestations:The subepithelial lesions of MMP may involve any mucosal surface, but they most frequently involve the oral mucosa .The conjunctiva is the second most common site of involvement and can lead to scarring and adhesions developing between the bulbar and palpebral conjunctiva called symblepharon. Corneal damage is common, and progressive scarring leads to blindness in close to 15% of patients. Lesions may also affect the genital mucosa, causing pain and sexual dysfunction. Laryngeal involvement causes pain, hoarseness, and difficulty breathing, whereas esophageal involvement may cause dysphagia, which can lead to debilitation and death in severe cases. Skin lesions, usually of the head and neck region, are present in 20 to 30% of patients .
Oral Manifestations: Oral lesions occur in over 90% of patients with MMP. Desquamative gingivitis is the most common manifestation and may be the only manifestation of the disease. Since these desquamative lesions resemble the lesions of erosive lichen planus and pemphigus, all cases of desquamative gingivitis should be biopsied and studied with both routine histology and direct immunofluorescence to determine the correct diagnosis. Lesions may present as intact vesicles of the gingival or other mucosal surfaces, but more frequently they appear as nonspecific-appearing erosions. The erosions typically spread more slowly than pemphigus lesions and are more self-limiting.
Diagnosis: Patients with MMP must have a biopsy done for both routine and directimmune fluorescent study. Routine histopathology shows sub-basilar cleavage. Using the direct immune fluorescent technique, biopsy specimens taken from MMP patients demonstrate positive fluorescence for immunoglobulin and complement in the basement membrane zone in 50 to 80% of patients. The direct immune fluorescent technique is excellent for distinguishing MMP from pemphigus .Only 10% of MMP patients demonstrate positive indirect immunofluorescence for circulating antibasement membrane zone antibodies .
Treatment: Management of MMP depends on the severity of symptoms. When the lesions are confined to the oral mucosa, systemic corticosteroids will suppress their formation. Unlike pemphigus, MMP is not a fatal disease, and long-term use of steroids for this purpose must be carefully evaluated, particularly because most cases are chronic, most patients are elderly, and treatment is required for a long period of time.Patients with mild oral disease should be treated with topical and intralesional steroids. Desquamative gingivitis can often be managed with topical steroids in a soft dental splint that covers the gingiva, although the clinician using topical steroids over large areas of mucosa must closely monitor the patient for side effects such as candidiasis and effects of systemic absorption. When topical or intralesional therapy is not successful, dapsone therapy may be attempted [ Since dapsone causes hemolysis and methe-moglobinemia, glucose-6-phosphate dehydrogenase deficiency must be ruled out and the patient’s hemoglobin must be closely monitored ]. Methemoglobinemia can be reduced with the use of cimetidine and vitamin E. Another rare side effect of dapsone is dapsone hypersensitivity syndrome. Patients resistant to dapsone should be treated with a combination of systemic corticosteroids and immunosuppressive drugs, particularly when there is risk of blindness from conjunctival involvement, or significant laryngeal or esophageal damage. Reports suggestthat tetracycline and nicotinamide may also be helpful in controlling the lesions of MMP .
M.M.P
Erythematous &erosive gingival lesion [desquamative gingivitis]M.M.P
Lesion of the palateM.M.P
Symblepharon formation of the eyePemphigus Vulgaris
B.M.M. Pemphigoid
Epidermolysisbullosa:
It is a dermmatological disorder in which bullae or vesicles occur on skin or M.M surface spontaneously, shortly after minor trauma. There is defect in attachment mechanism of epithelial cell. The term epidermolysisbullosa [EB] is used for group of mechanobullos diseases characterized by the development of blisters in area of minor trauma . At least 23 distinct forms of the disease have been recognized . Most of these have a hereditary basis , with onset of blistering lesions at birth or within the first few years of life . Epidermolysisbullosa acquista is not hereditary , however , and appear to be an autoimmune disorder , with lesions typically arising during adolescence or adulthood . The various types are characterized by spontaneous or trauma-induced blister formation caused bydegeneration of basal or Para basal epithelial cells [EB simplex]
lack of hemi desmosome [junctional EB]
defects in anchoring fibrils in the connective tissue [dystrophic EB] .
Oral manifestations are more common in the junctional and dystrophic forms. Oral lesions present as bullae, usually in areas of friction, which rupture, leaving shallow ulcers, and later atrophy and scarring. Oral lesion are common in several types of EB and may result in painful erosion and severe scarring . Enamel hypoplasia is a common finding in junctional forms of EB . Rampant dental caries frequently is seen in patients with junctional EB and severe recessive dystrophic EB . Development of squamous cell carcinoma of the tongue has been reported in several cases of recessive dystrophic EB . Skin lesions are characterized by the formation of bullae, followed by ulcerations and scarring, particularly in areas exposed to low-grade chronic trauma. Nail involvement,
deformities of hands and feet, milia formation, and involvement of the larynx, pharynx, and esophagus are common in the recessive dystrophictype. The prognosis for EB depends on the specific subtype of EB .
Classification:
Epidermolysisbullosa SimplexEpidermolysisbullosa Dystrophic, dominant.
Epidermolysisbullosa Dystrophic , recessive.
Junctional Epidermolysisbullosa.
Epidermolysisbullosa acquisita (acquired)
Epidermolysisbullosa simplex: hemorrhagic bulla on thebuccal mucosa.
Epidermolysisbullosa, recessive dystrophic form: bulla and scarring on thetongue.Treatment: Supportive. Systemic steroids in severe cases.
Bullous Lichen Planus
Bullous lichen planus is a rare form of lichen planus. It is clinically characterized by the formation of bullae that soon rupture, leaving painful shallow ulcerations .The bullae usually arise on a background of papules or striae with the typical pattern of lichen planus.Dermatitis herpetiformis: intact bulla on the lower lip mucosa and smallerosions on the gingiva.