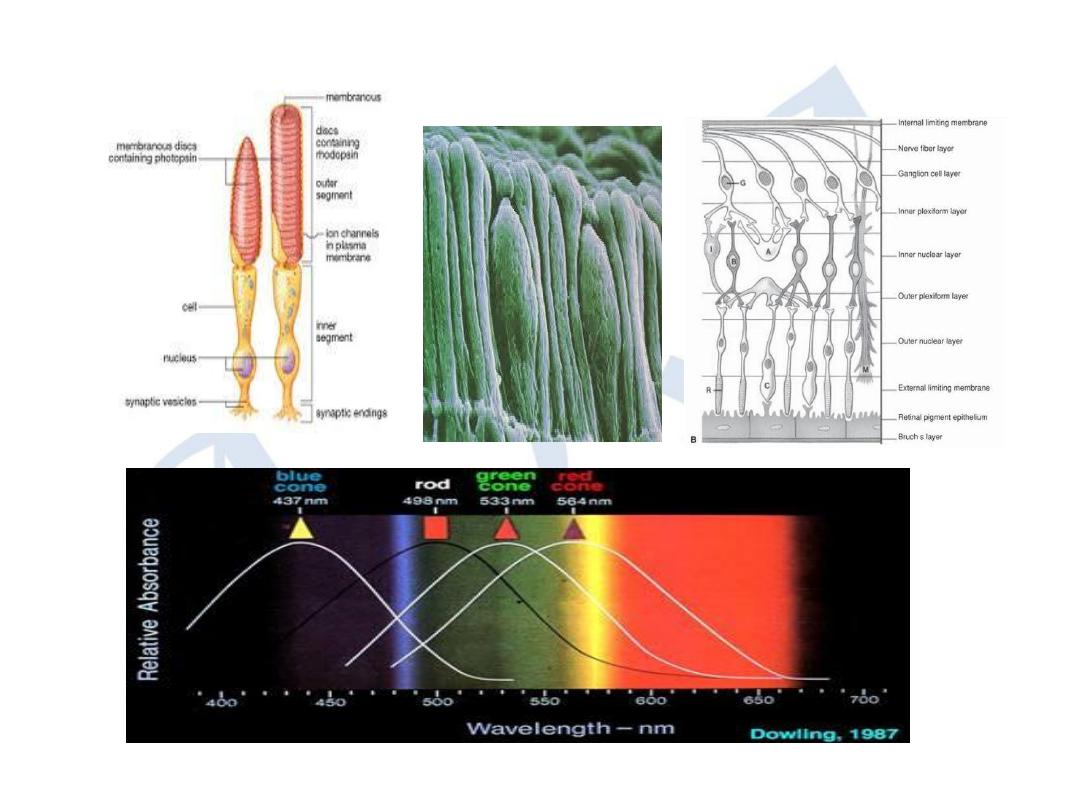
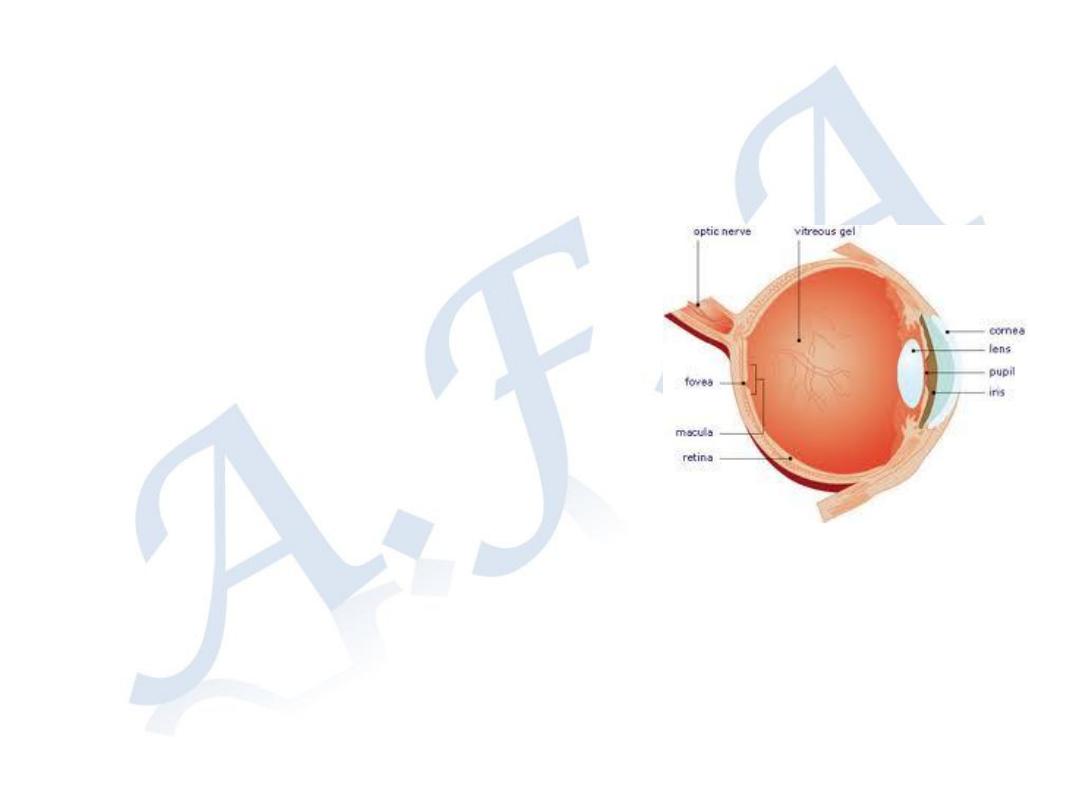
Retina
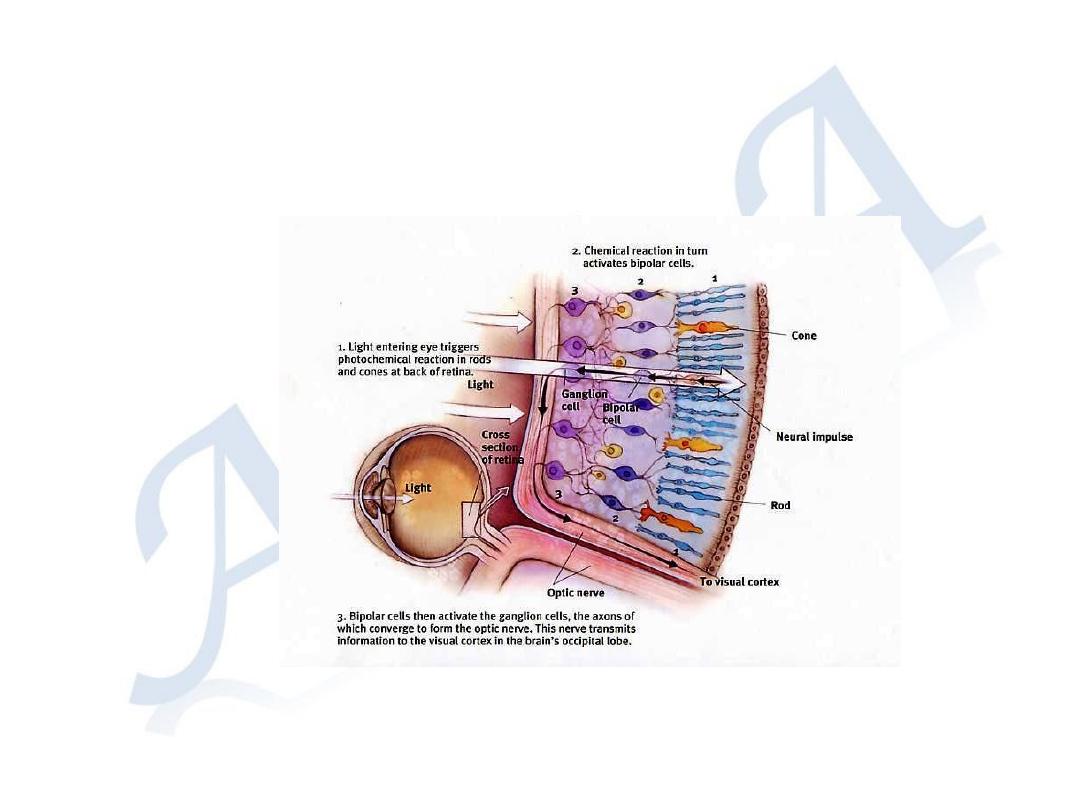
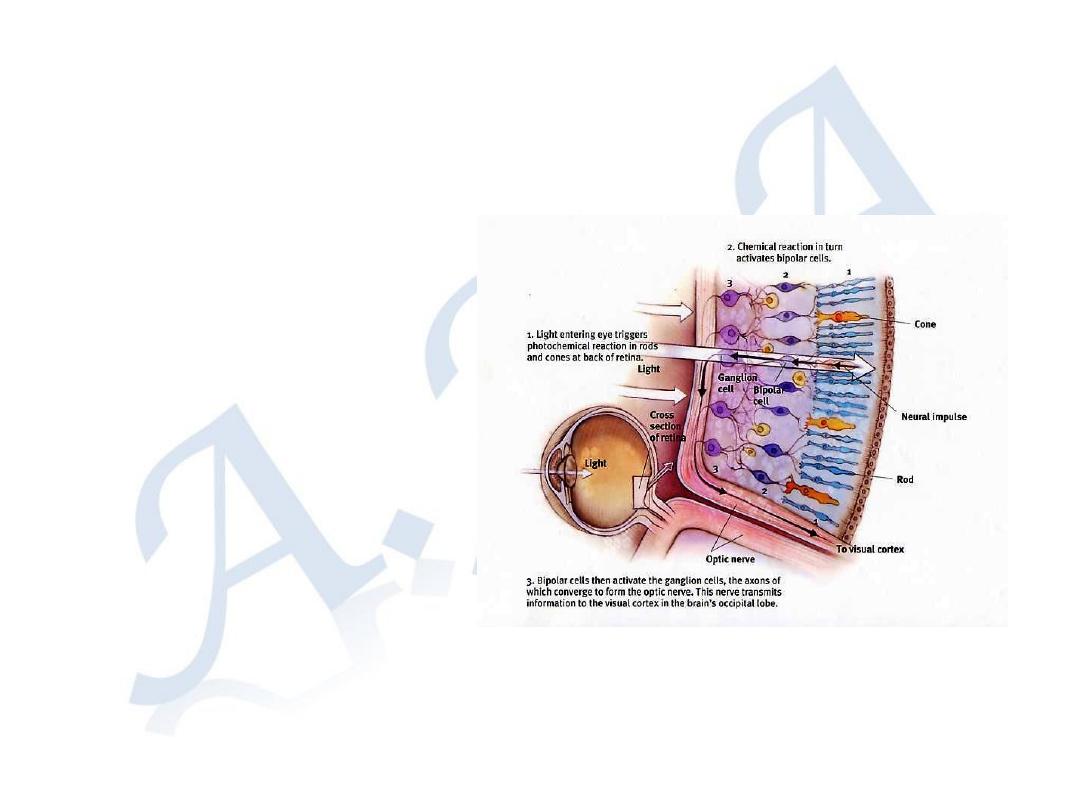
The retina is the photosensitive layer of the eye where light energy is
converted to electrical impulses, which transmitted to the brain through the
optic nerve.
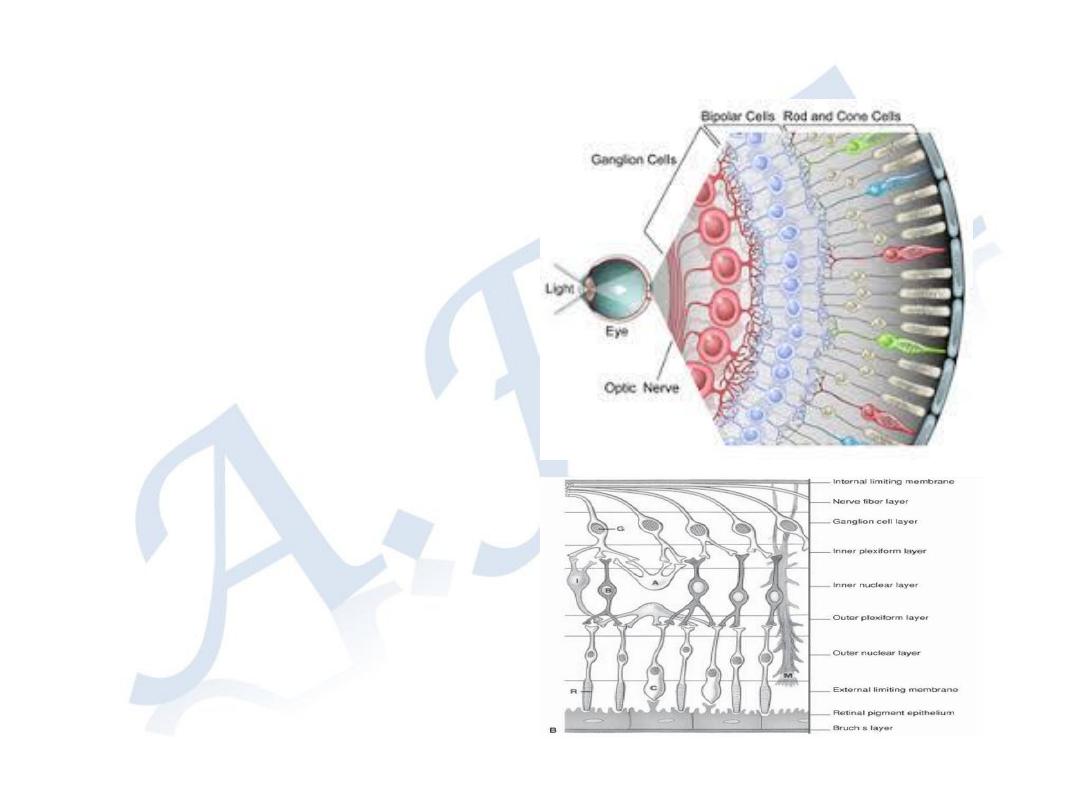
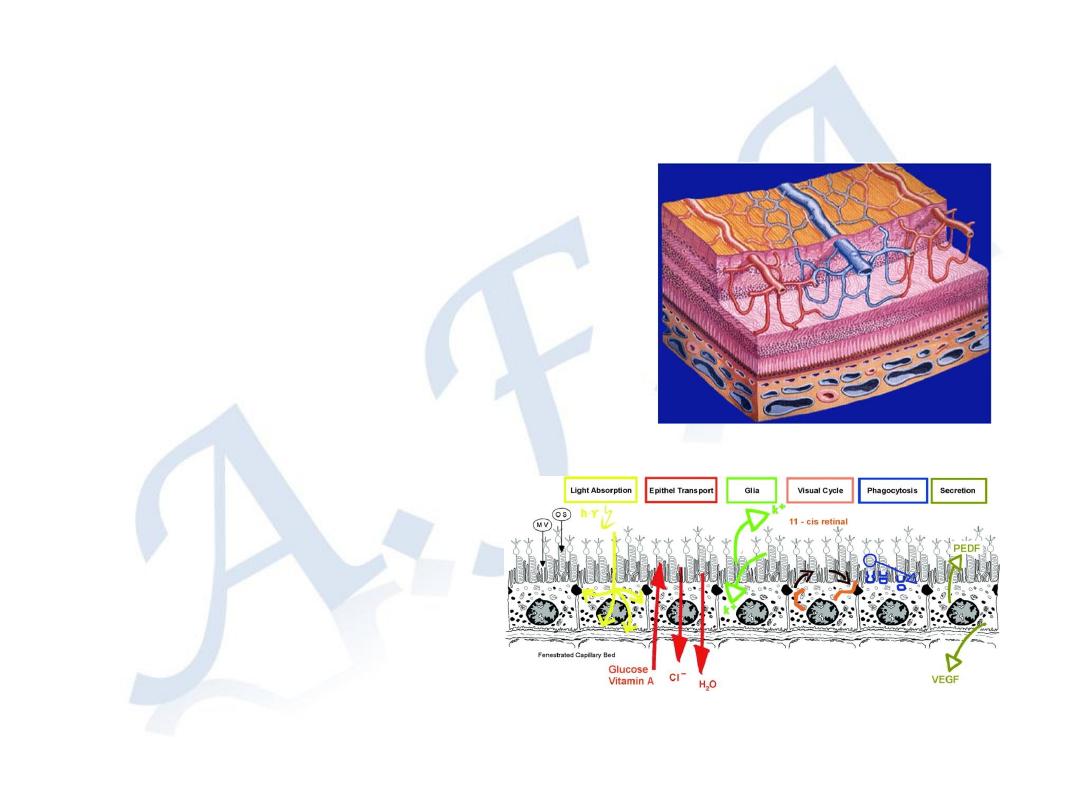
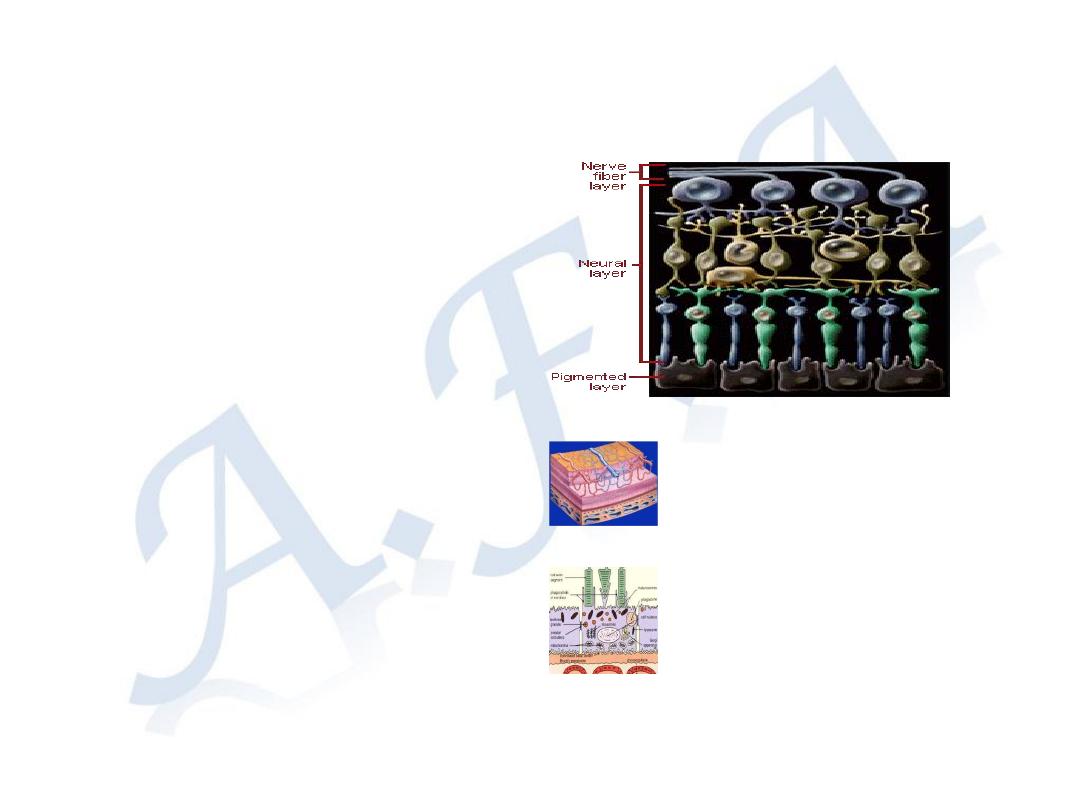
Retina consists of two main
layers:
A-The outer layer the
Retinal pigment layer
(RPE)
B-The inner layer the
Sensory layer,
1-Photoreceptors (Cones and
Rods)
2-Outer limiting membrane
3-Outer nuclear layer
4-Outer plexiform layer
5-Inner nuclear layer
6-Inner plexiform layer
7-Ganglion layer
8-Nerve fiber layer
9-Inner limiting membrane
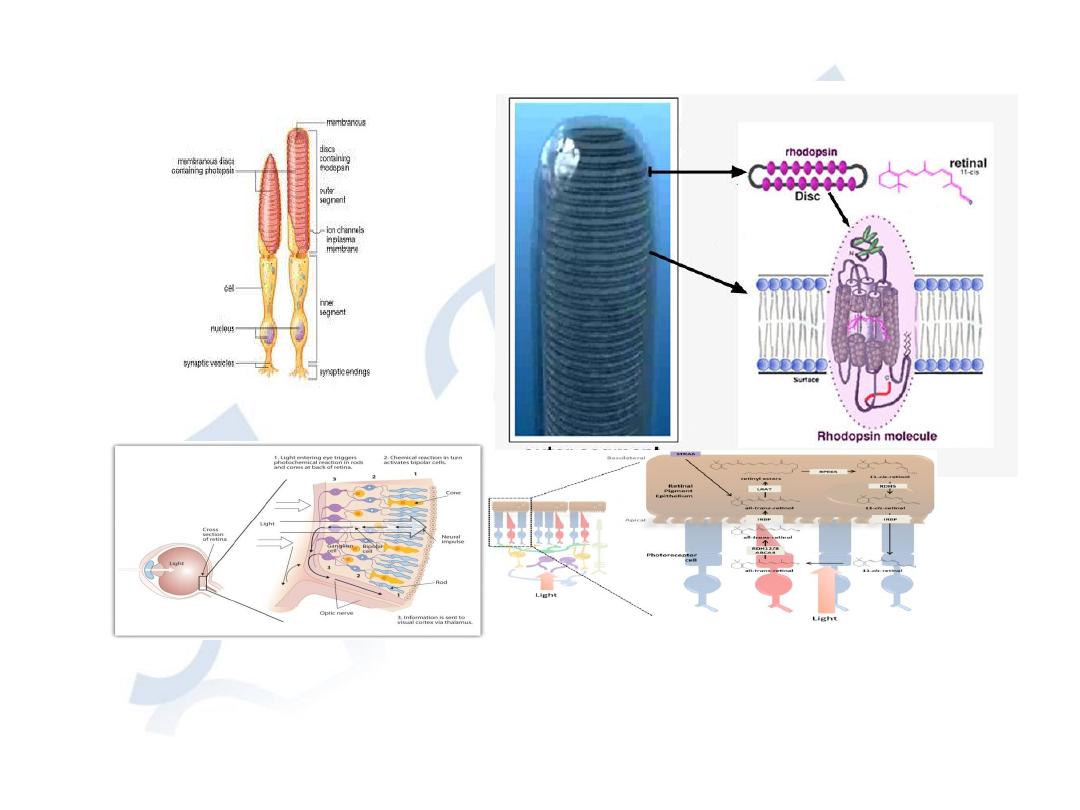
Phototransduction
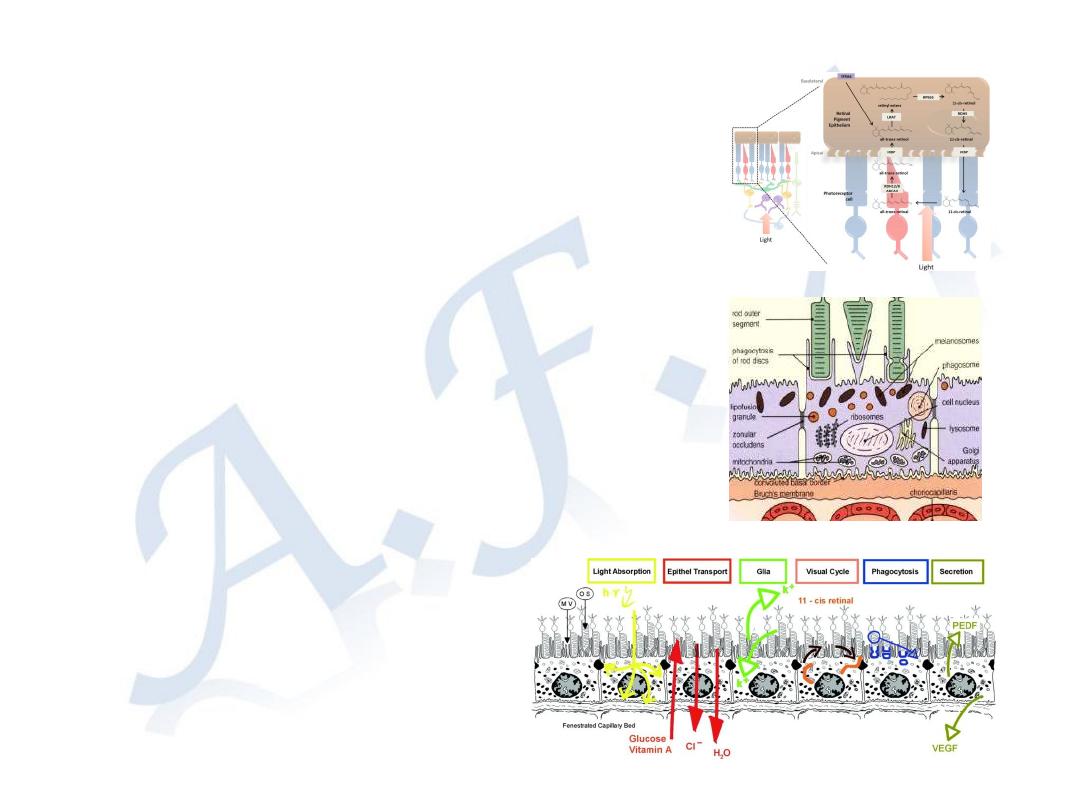
Visual cycle. Absorption of light by visual pigments (rhodopsin or cone
opsin) causes isomerization of 11-cis-retinal to all-trans-retinal,
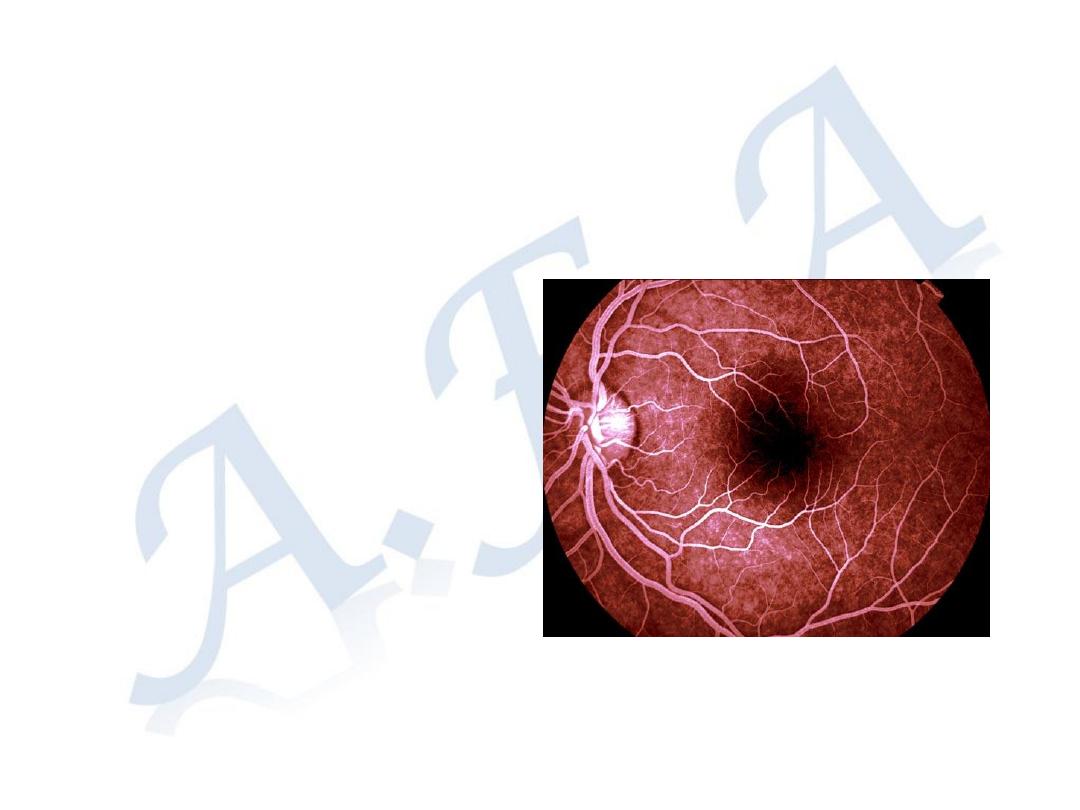
Oxygen and nutrients supply:
Inner layers
supplied by central retinal
artery
Photoreceptors
supplied by
choriocapillaries
Retina consists of
densely packed cells
Extra-cellar space is
only 1%
Retinal-Blood Barrier:
-Inner: tight junctions
between the endothelial
cells of retinal capillaries
- Outer: tight junctions
between the retinal
pigment epithelial cells
Retinal vessels are
End arterioles
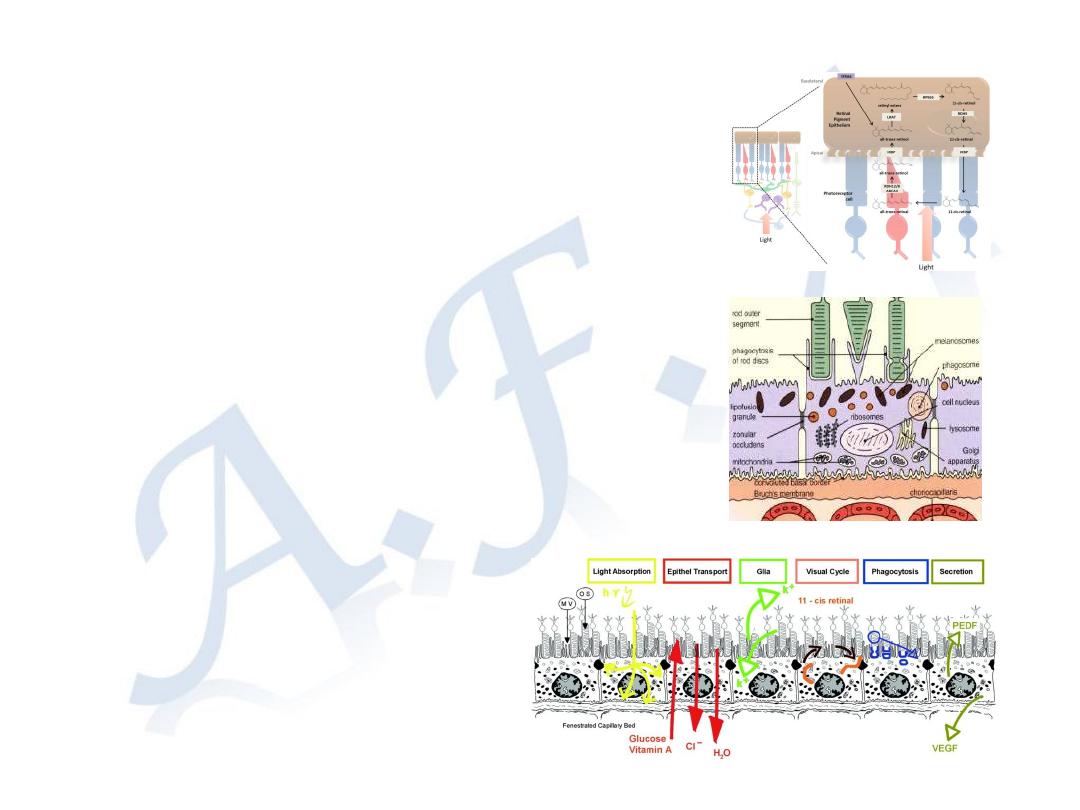
Functions of Retinal pigment
epithelium:
1- Regenerates the visual pigments after
phototransduction
2- Passage of O2 and nutrients from choroid
to the photoreceptors
3- Outer retinal blood barrier
4- Absorb scattered light
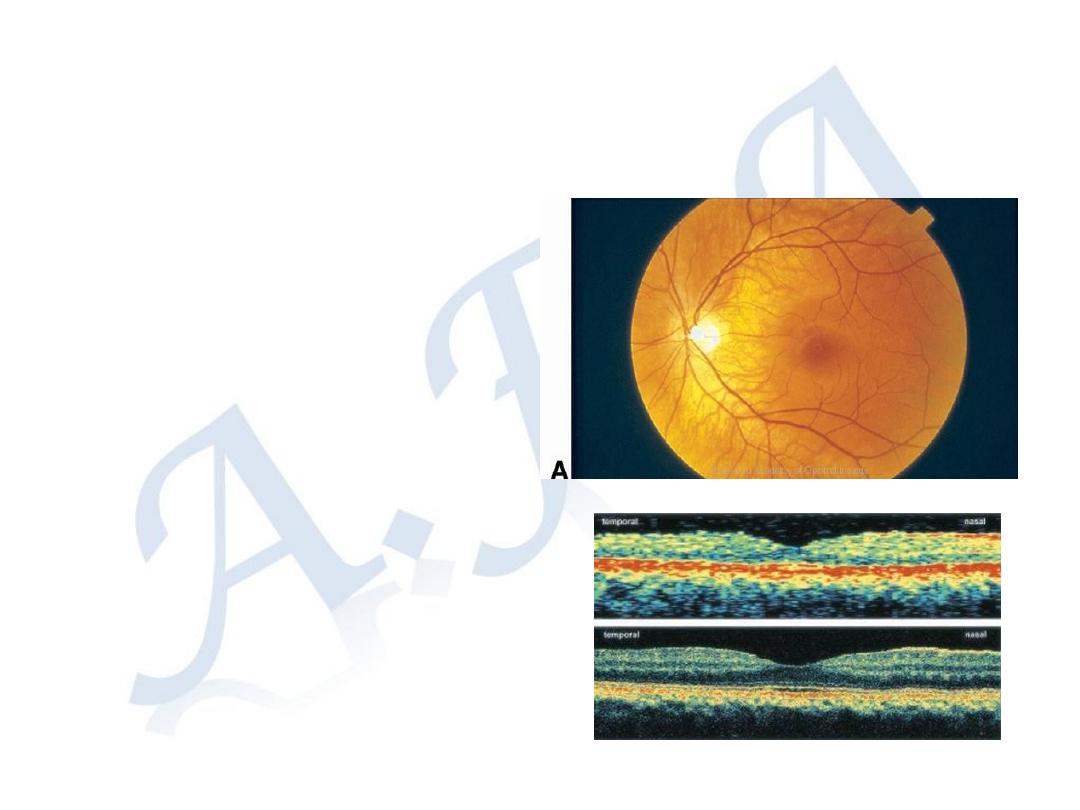
Macula; an oval area in the
posterior pole about 5 mm in
diameter, correspond to
central 15
o
of visual field.
Fovea; central part in the
macula about 1.5 mm in
diameter correspond to the
central 5
o
in the visual field.
Foveola: central depression
in the fovea about 0.35 mm
in diameter contains cones
only, and correspond to the
central 1
o
of the most precise
vision in the visual field.
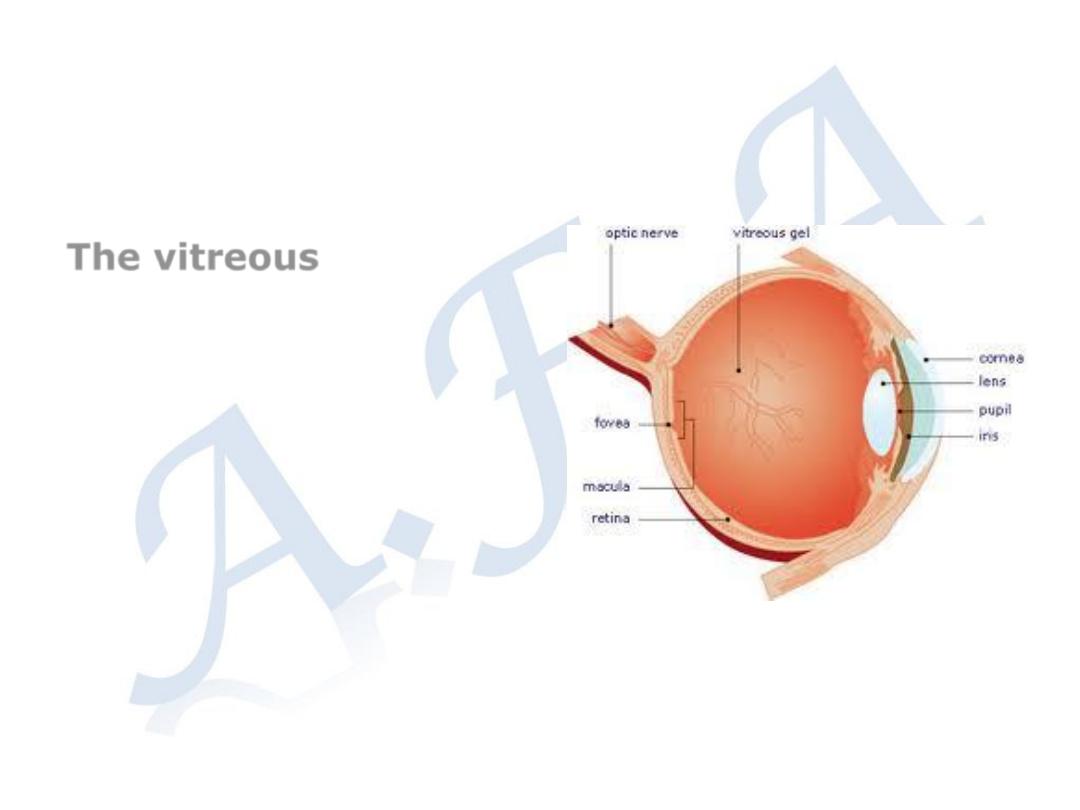
The vitreous
:
a clear gel occupying two-
thirds of the globe, consists:
- water 98%.
- hyaluronic acid
- fine collagen network
- There are few leukocytes.
Vitreous firmly Attached to
the peripheral retina, and
around the optic disc
.

Symptoms of retinal disorders:
1- Painless impairment of vision.
2 - Distorted vision (
metamorphopsia) caused by a disturbance in
the
arrangement of the photoreceptors in macular diseases
such as reduction (
micropsia) or enlargement (macropsia) of
object size
3-Impairment of color vision which occurs in macular diseases
4- Visual field defects
5-Floaters (perception of moving images in the field of vision,
caused by vitreous opacities that cast a shadow on the retina).
6-Photopsia (perception of flashes of light)
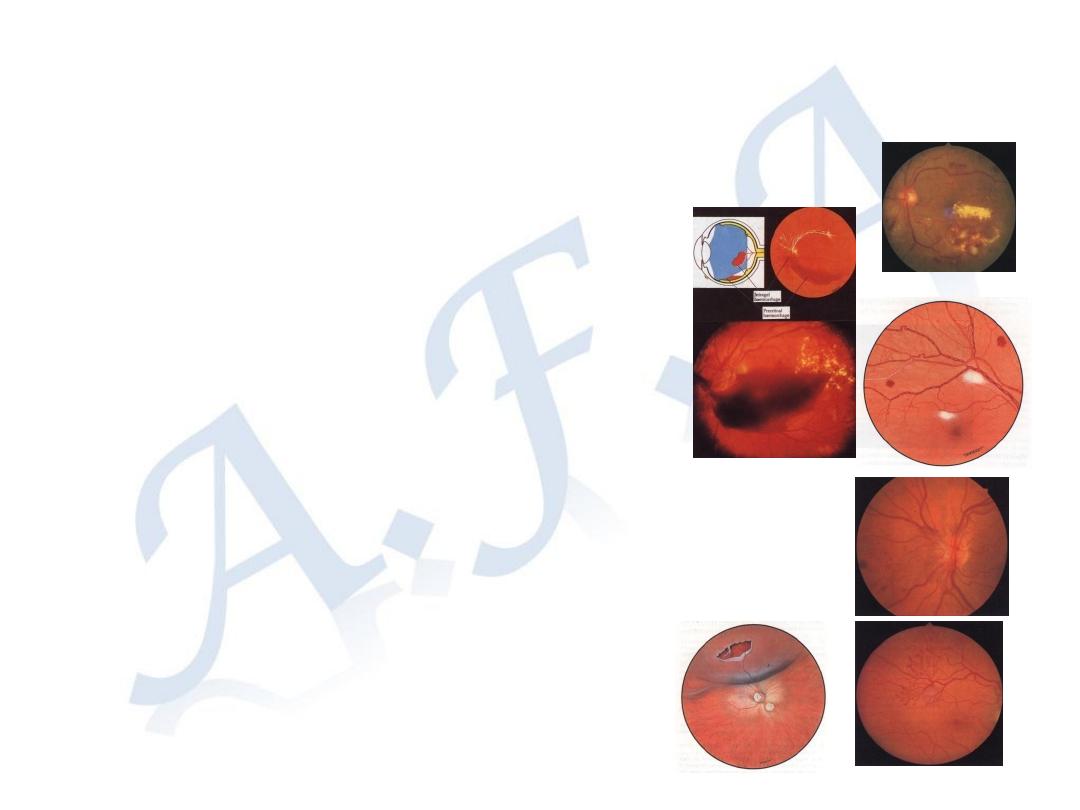
Signs
1-Depressed Visual acuity
2-Impairment of Pupillary light reflex
3-Vitreous opacities
Hemorrhage
WBC
Pigment dots (Tobacco dust)
4-Retinal hemorrhage
- Hard exudates: yellow spots well demarcated margins , deposition
of lipoproteins, or lipid, are sign s of abnormal vascular leakage
- Cotton wool spots: fluffy white spots with indistinct margins,
accumulation of axoplasmic debris in the nerve fiber layer , they
are sins of retinal ischemia (micro-infraction of the nerve fiber layer)
5-Abnormal position (Retinal detachment)
6-Neo-vascularization: retinal ischemia ; secretion of vaso-formative factors
NVD (neo-vascularization on the surface of the optic disc)
NVE (neo-vascularization
on the surface of the retina).
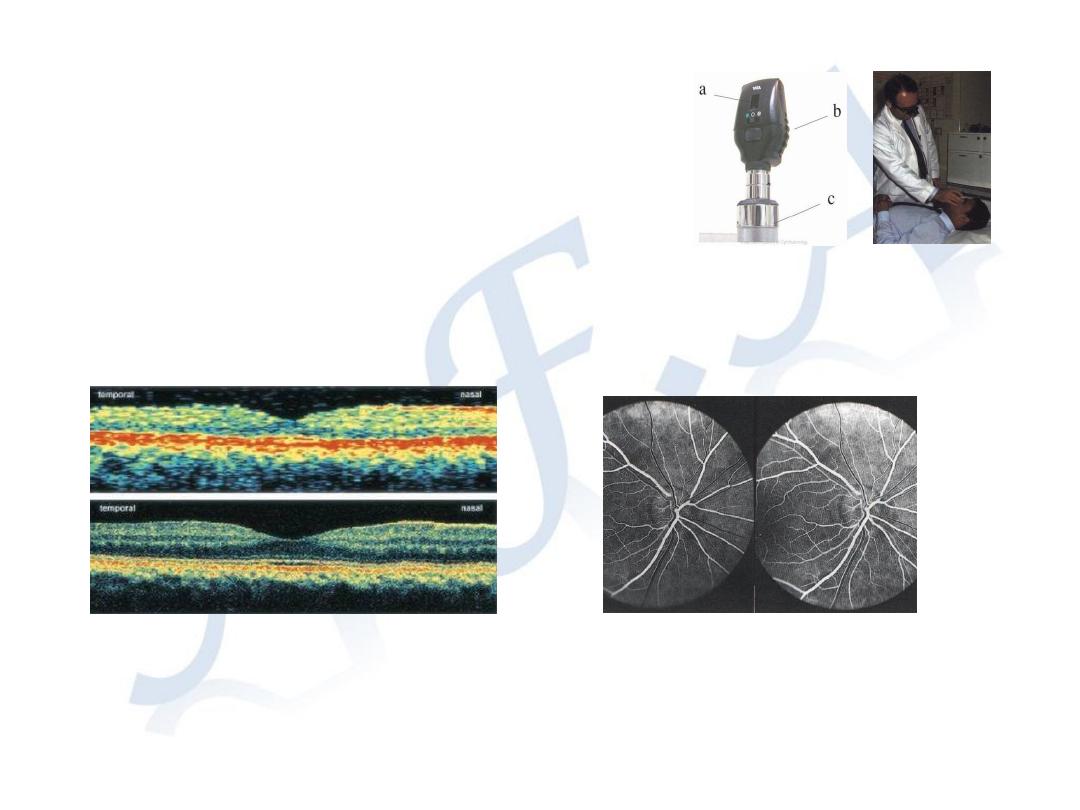
Examination of the retina
Direct ophthalmoscope
Indirect ophthalmoscope
Investigations
Fluorescein angiography-FA
Optical coherence tomography-OCT
Diabetic Retinopathy
One of the most important causes of blindness
Risk factors:
1-Duration of diabetes. After 10 years 50% have retinopathy,
while after 30 years 90% have retinopathy
2-Poor metabolic control
3-Hypertension
4-Nephropathy
5-Pregnancy
6-Others; smoking, obesity, hyperlipidaema.
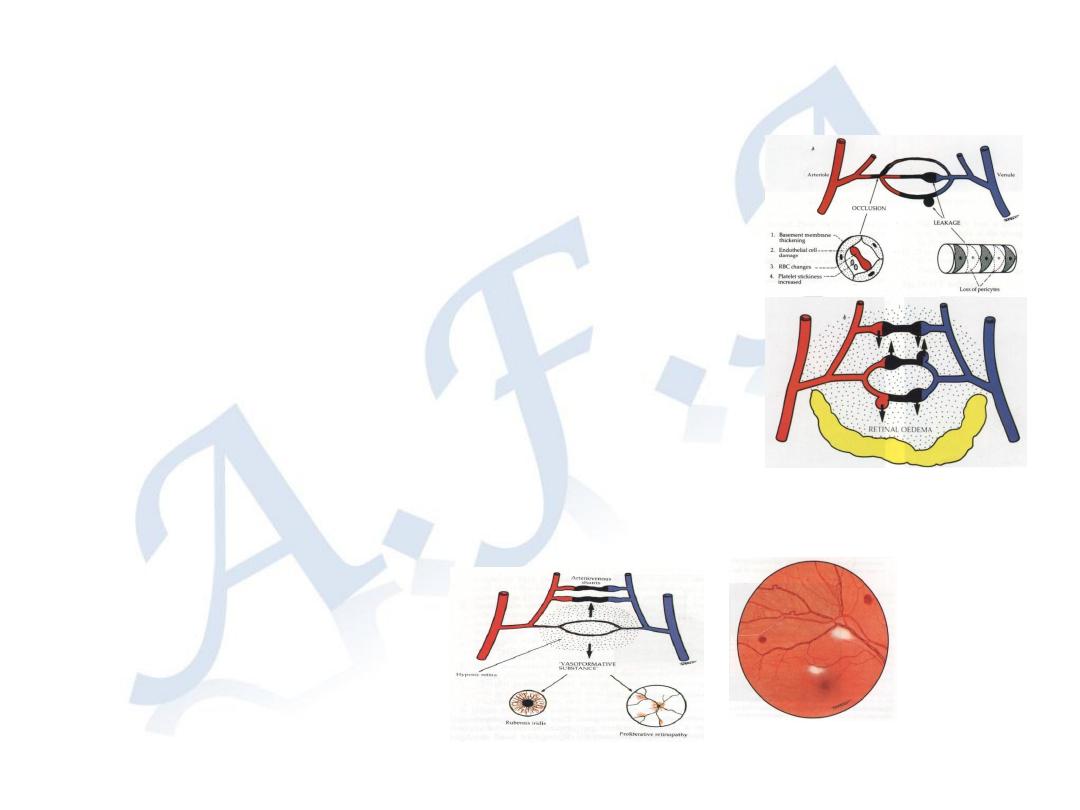
1- Micro-vascular leakage
-microaneurysms
-Hard exudates
2- Micro-vascular occlusion
Cotton wool spots
Formation of abnormal neo-
vasculartization on the surface of the
retina (NVE) and on the optic disc (NVD).
Pathogenesis:
It is a microangiopathy, affecting pre-capillary arterioles,
capillaries, and post-capillary venules.
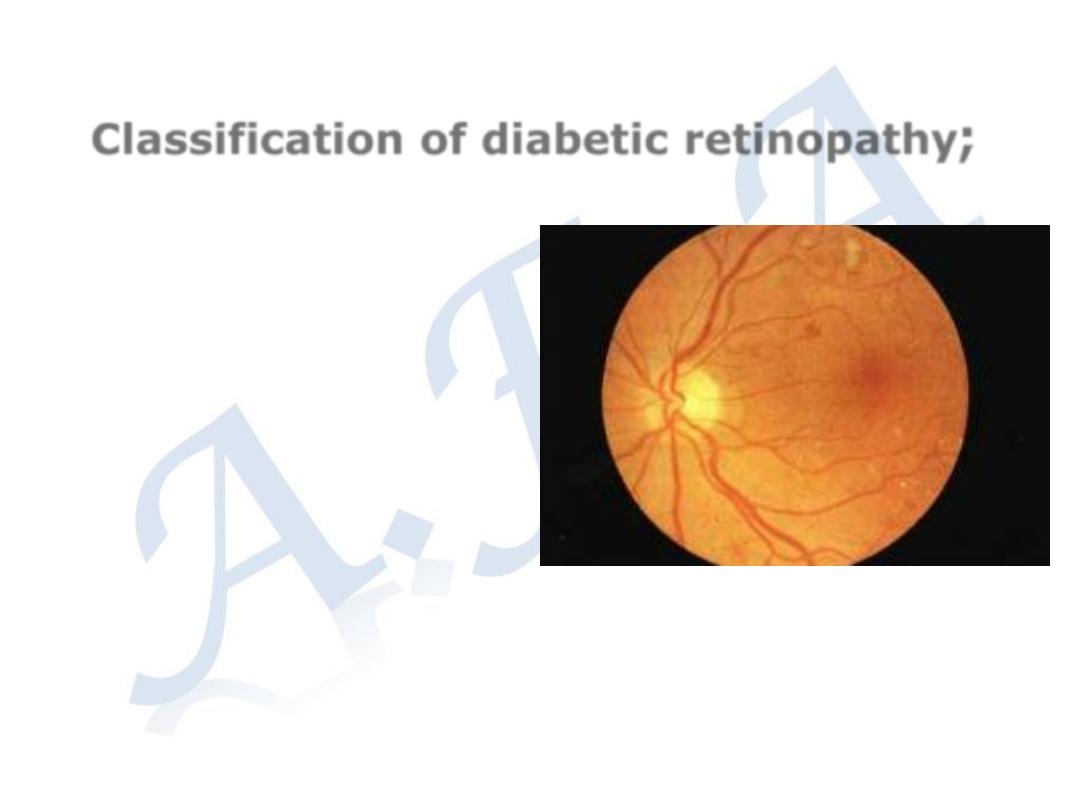
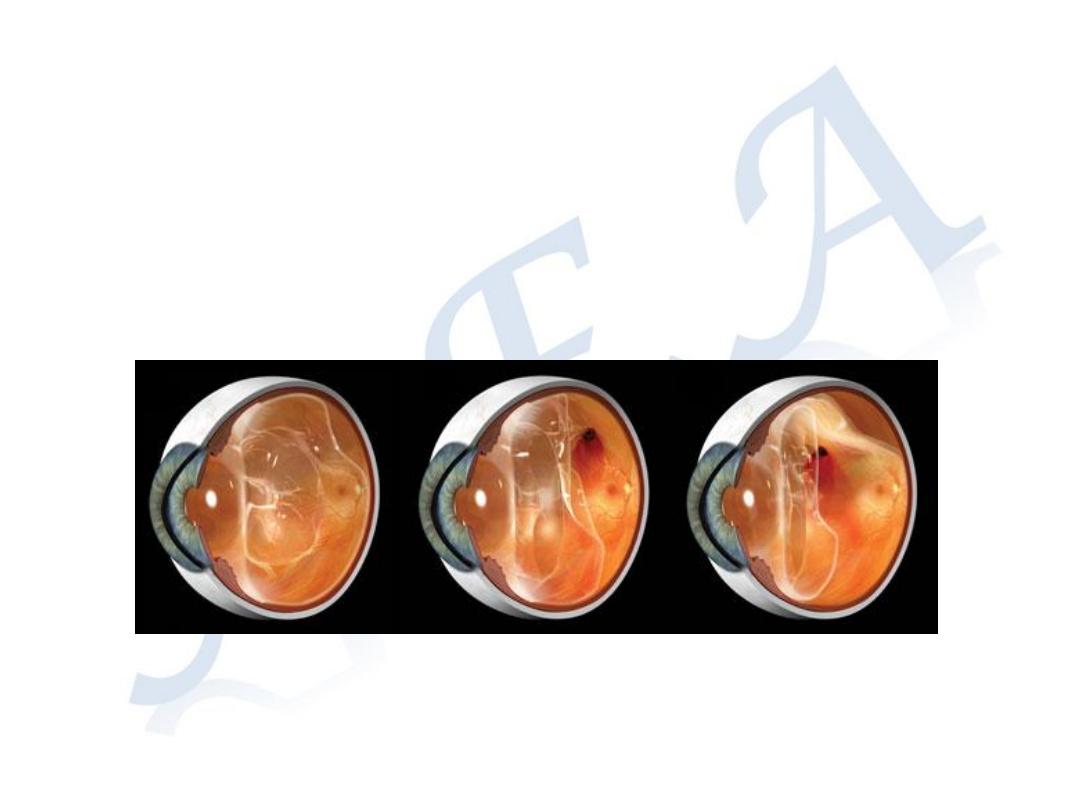
Classification of diabetic retinopathy
;
1-Background (non-
proliferative)
microaneurysms,
Retinal
hemorrhages (blot
and dots ), and
hard exudates.
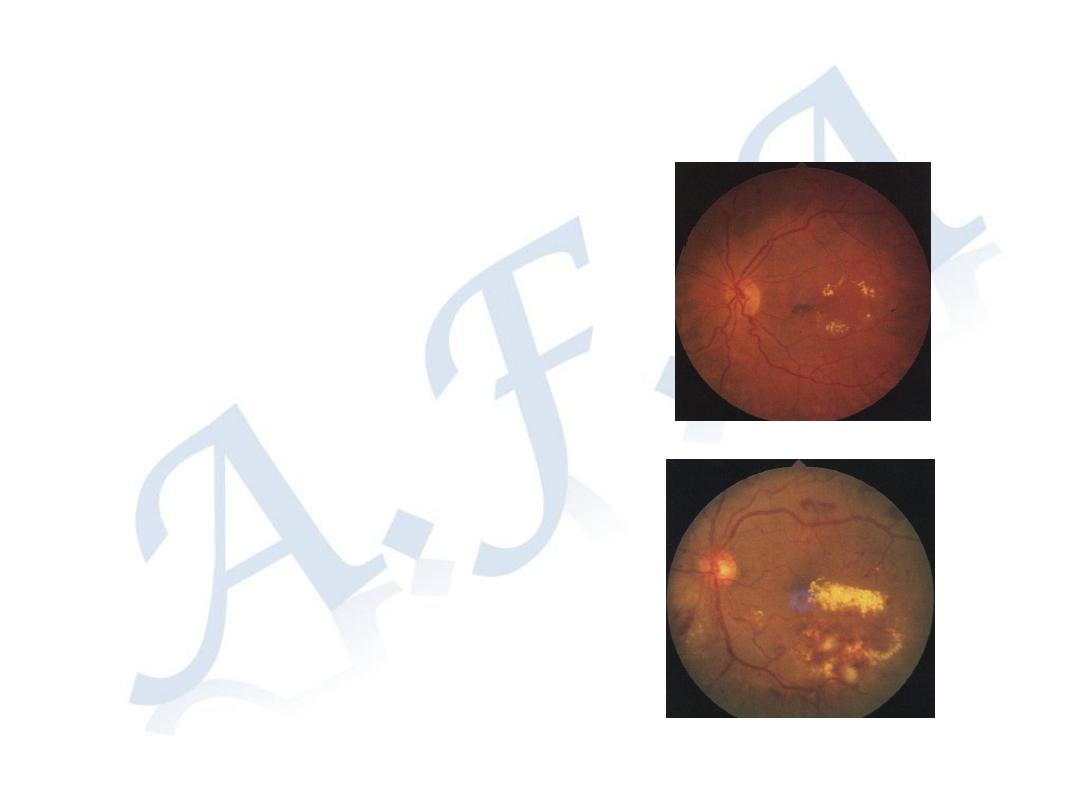
2-Maculopathy, (clinical significant
macular edema). Microaneurysms,
hemorrhages, and hard exudates at
the macula.
Vision is impaired
3-Pre-proliferative. Large
retinal hemorrhage, cotton
wool spots
(infarction in the nerve
fiber layer), venous
congestion and dilatation.
4-Proliferative retinopathy.
Abnormal neo-
vasculartization on the
surface of the retina (NVE)
and on the optic disc (NVD).
5-Advanced diabetic retinopathy.
Vitreous hemorrhage and tractional retinal detachment.
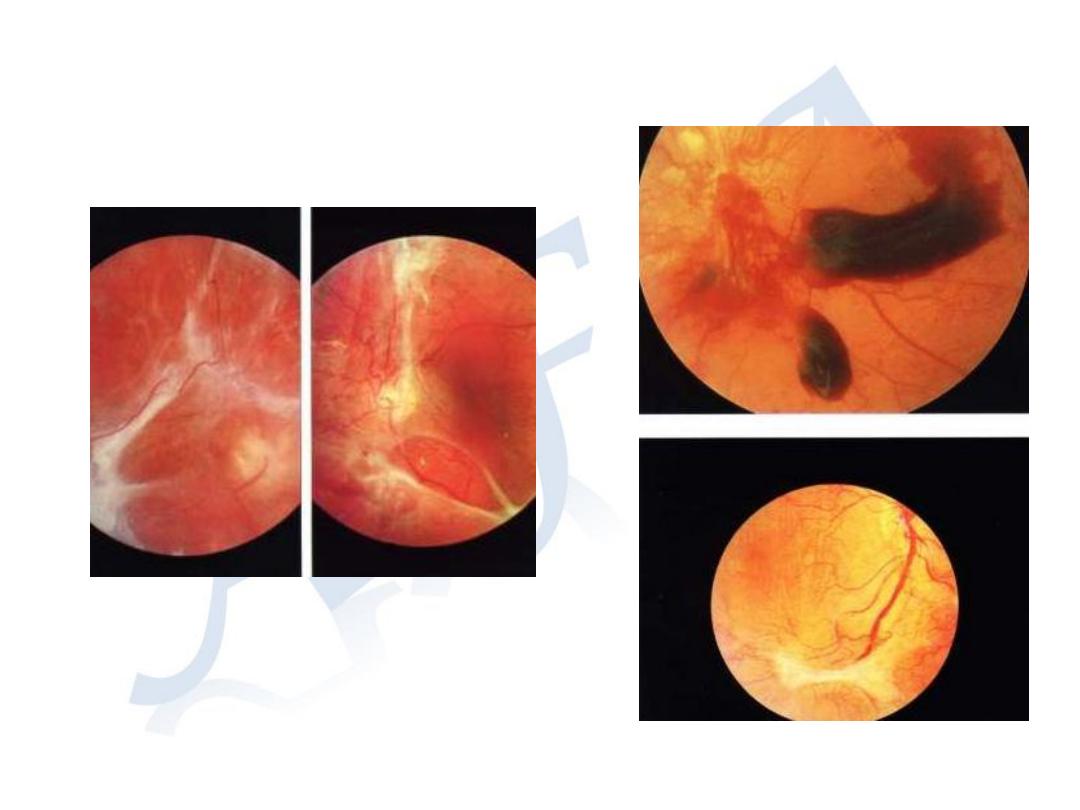
Advanced diabetic retinopathy

Management:
Management:
Essential Important Point is:
Early Detection of Diabetic Retinopathy
The treatment is more effective and the prognosis is
better in early stages.
Every diabetic patient must has regular ophthalmic
examination for detection retinopathy.
Background; good diabetic control
Control of other risk factors
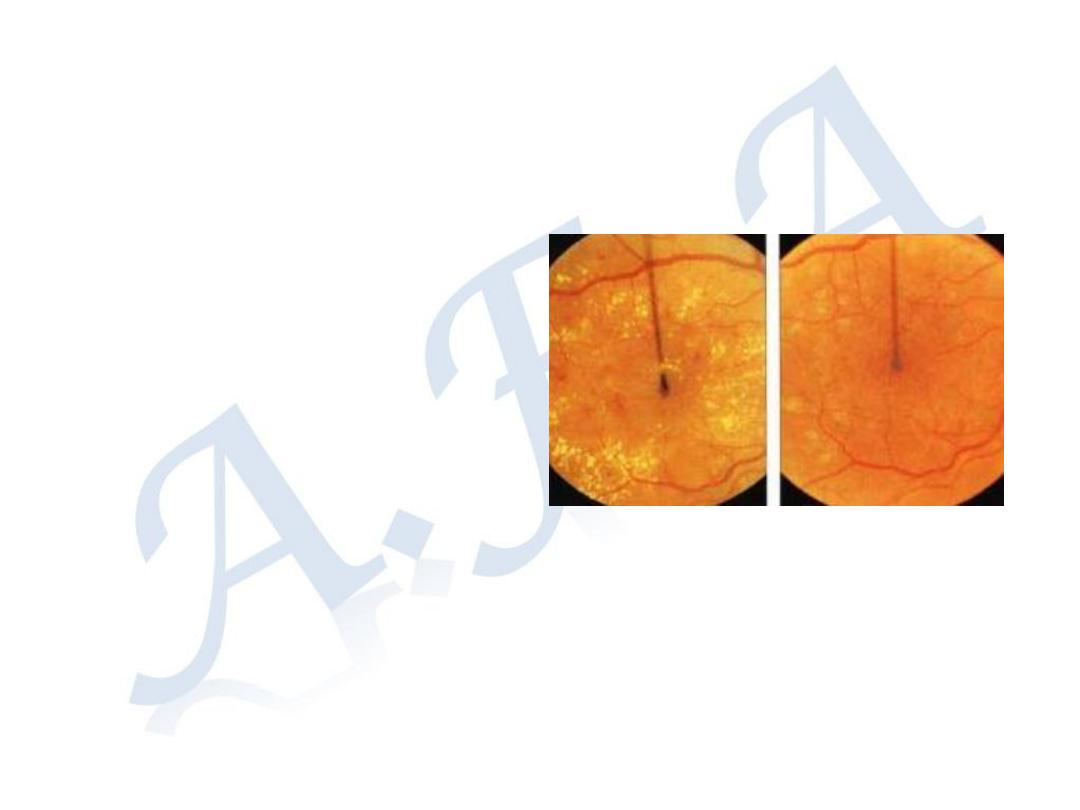
Maculopathy:
Laser phototherapy.
Laser burns are directed
at the sites of leakage
( micro-aneurysms),
avoiding the central fovea.
Intra-vitreal injection of
Anti-vascular endothelial
growth factor (Anti-VGEF
)
Pre-proliferative and Proliferative
retinopathy;
Laser phototherapy.
The entire retina is treated with laser
burns except the macula and area adjacent
to the optic disc Pan retinal
photocoagulation (PRP).
The Laser burns destroy the ischemic
retina and prevent release of vaso-
formative factors and causing regression of
the abnormal vessels.
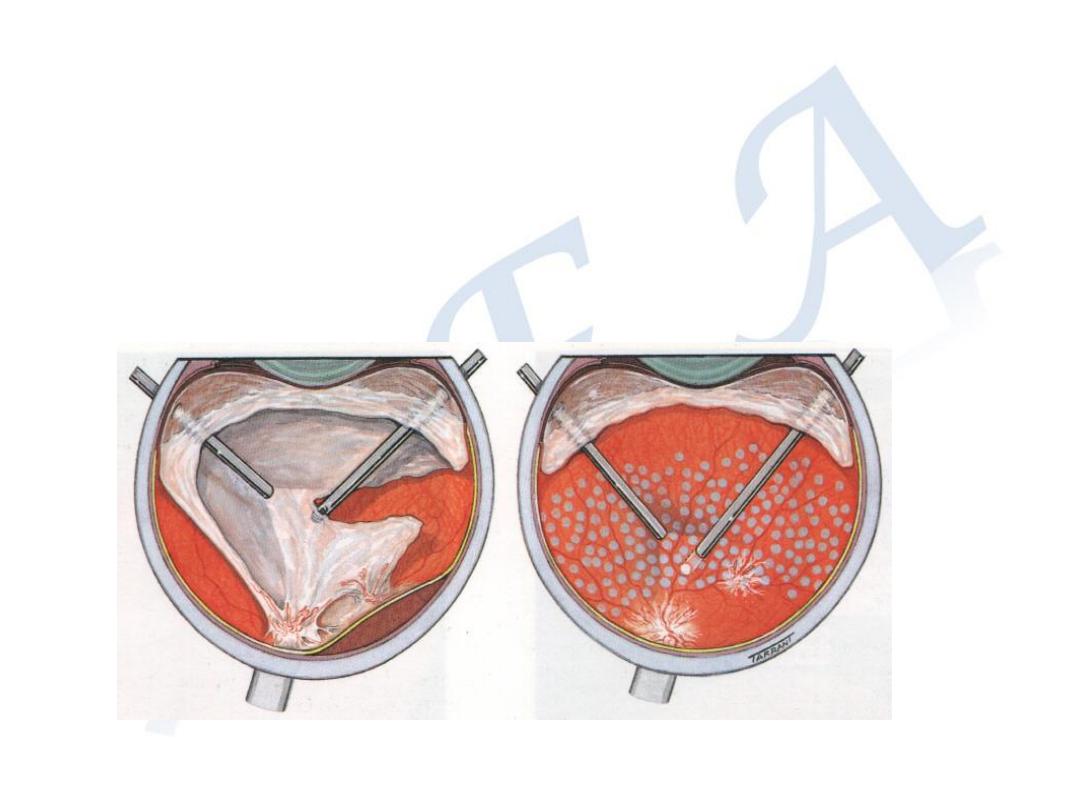
Advanced retinopathy; Surgery (Pars Plana
Vitrectomy).
Removal of the vitreous hemorrhage,
vitro-retinal bands and endo-laser through small
incisions at pars plana (posterior part of the ciliary
body).
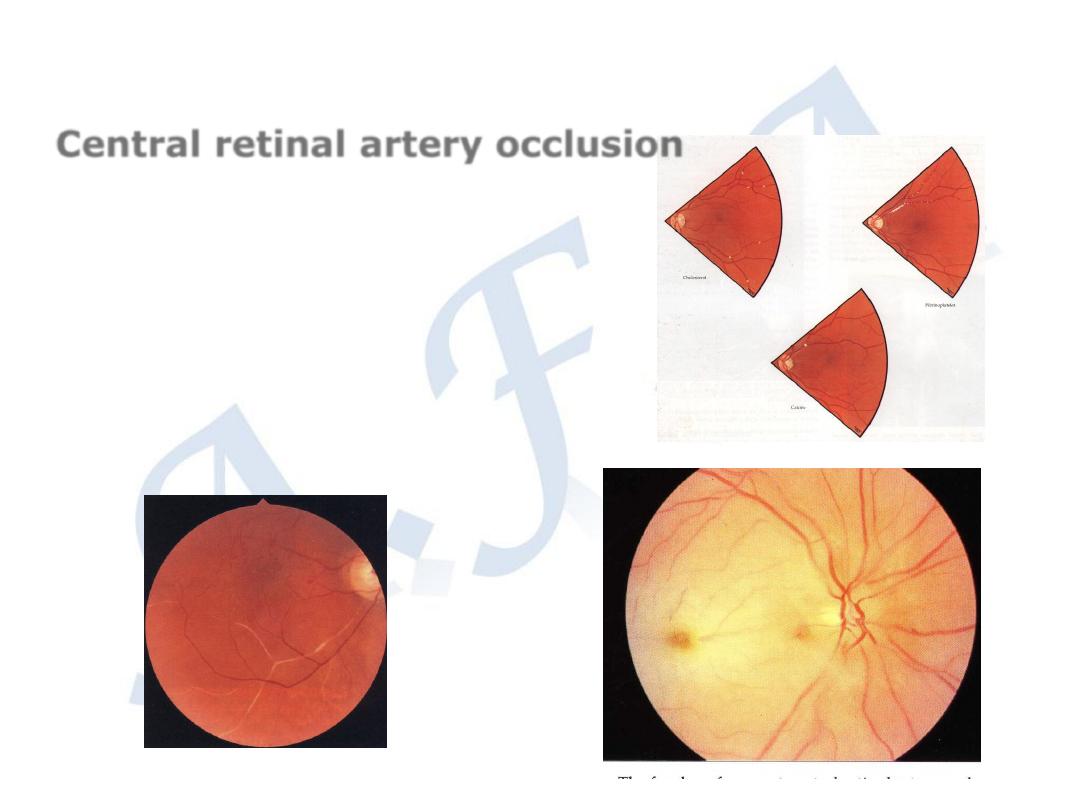
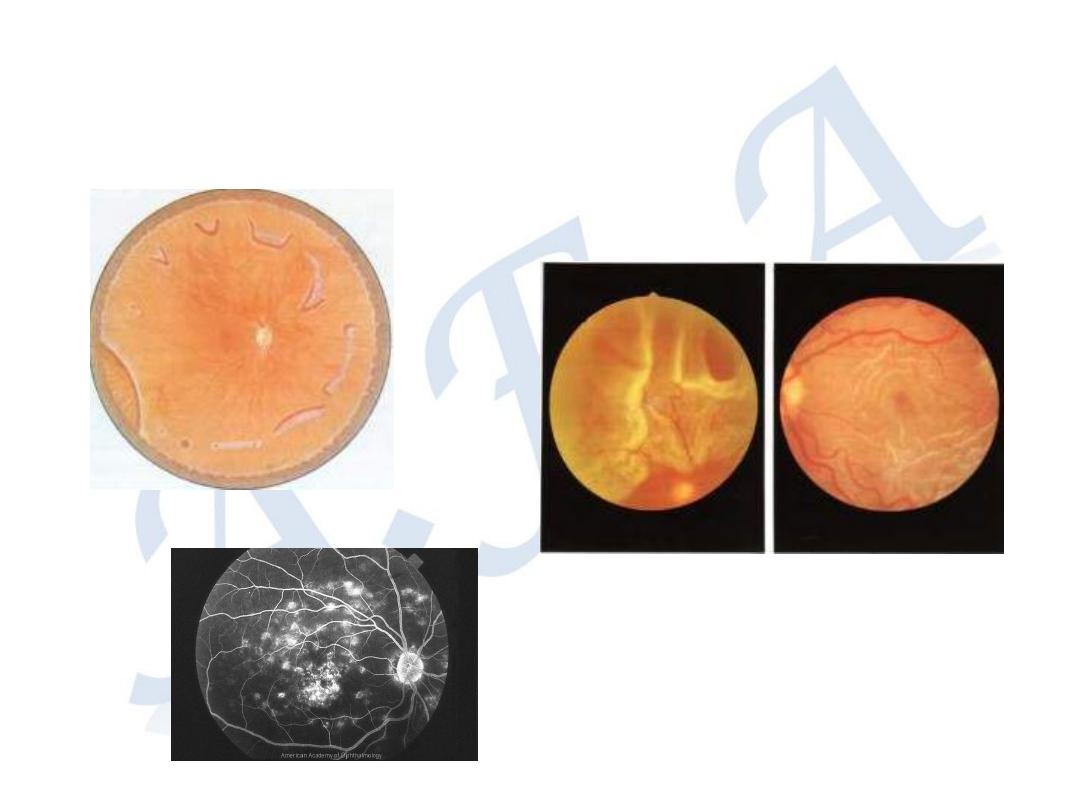
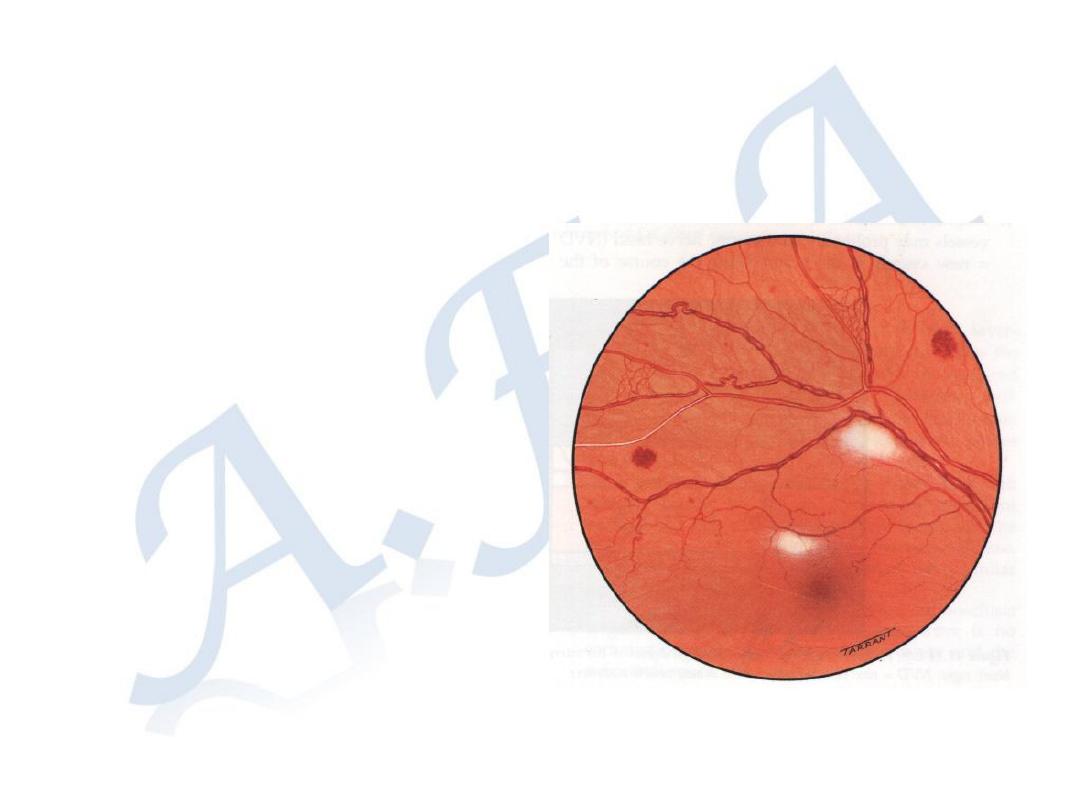
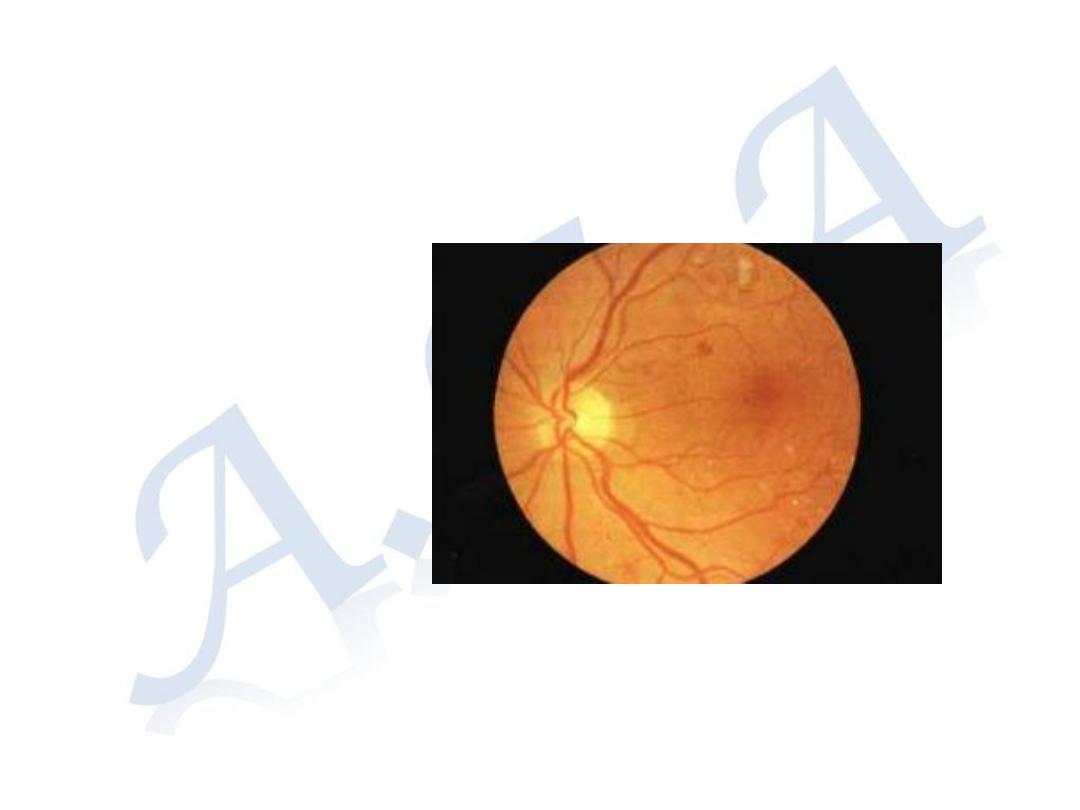
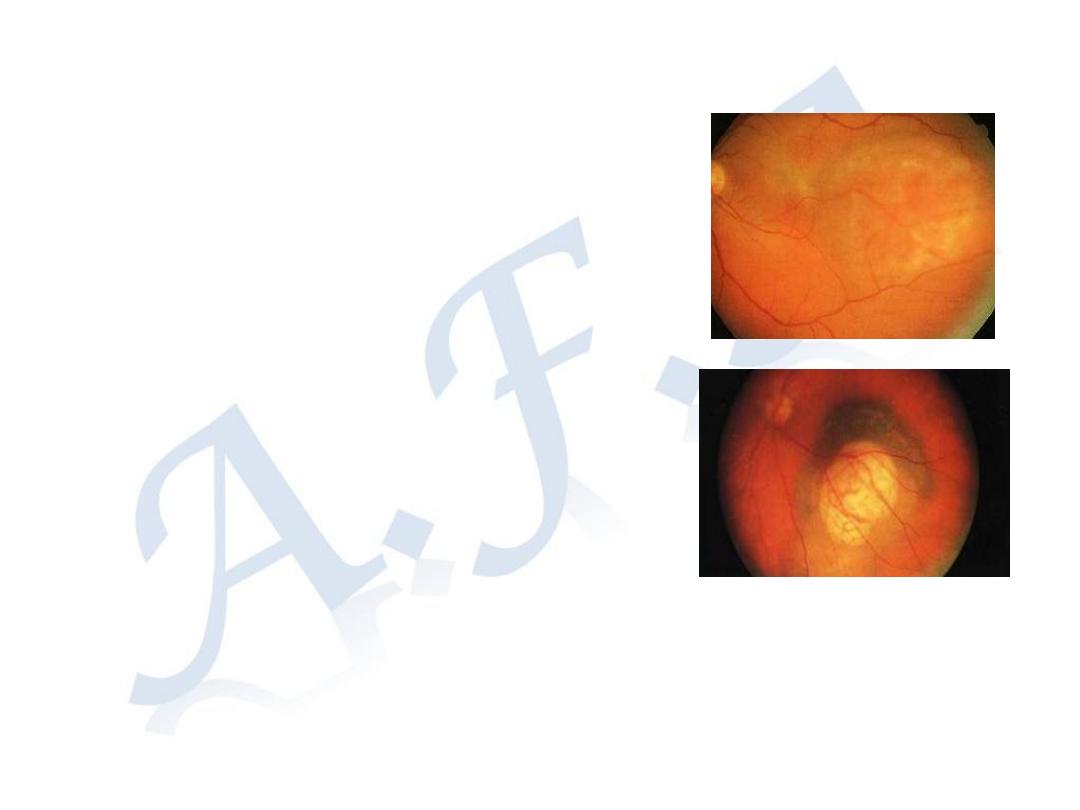
Retinal arterial occlusion
Aetiology; Atherosclerosis, or Embolism
Symptoms: Sudden, painless loss of vision
Signs: Retinal edema, Cherry red spot
Old cases; atrophic retina, attenuated
arterioles, and pale disc
Treatment; must be given within 48 hours
Ocular massage
Acetazolamide 500mg i.v.
Anterior chamber paracentesis
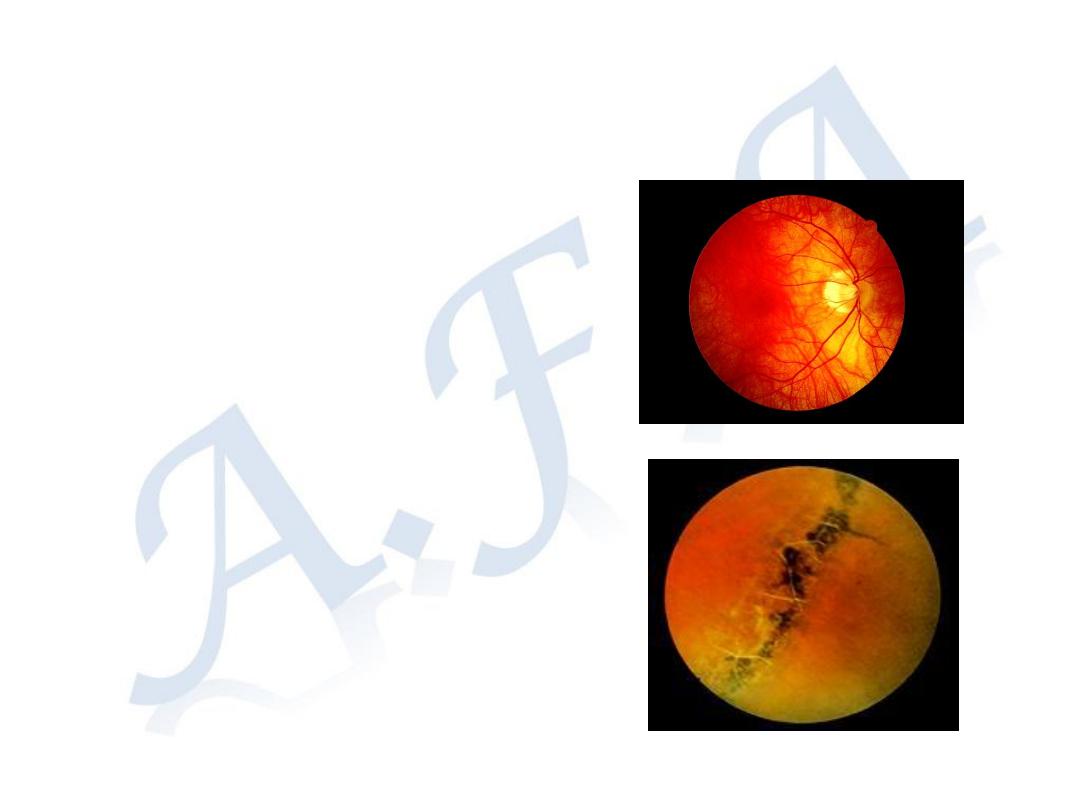
Central retinal artery occlusion
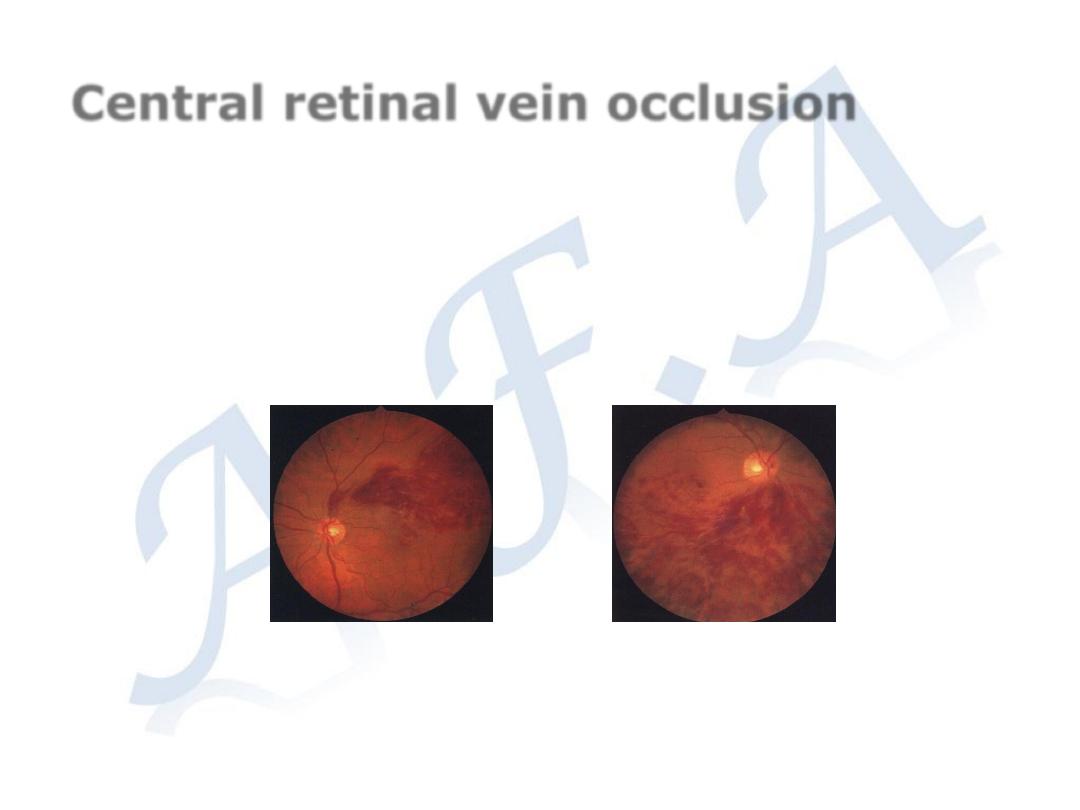
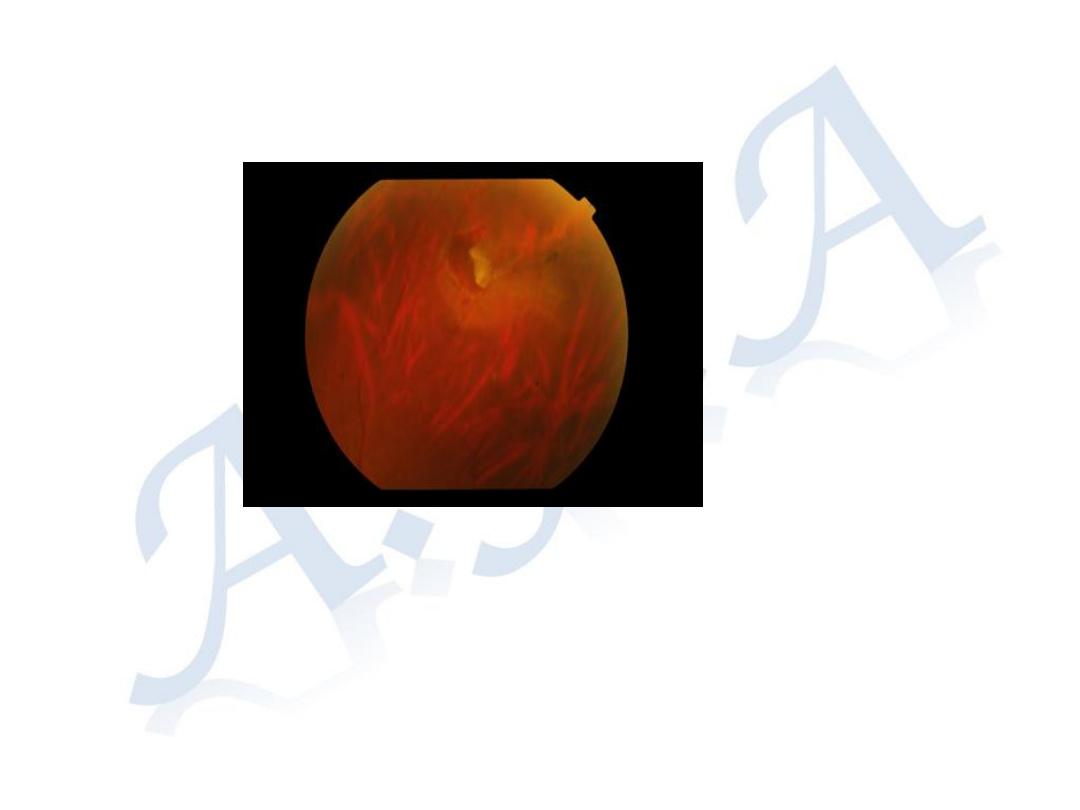
Central retinal vein occlusion
Predisposing factors; Glaucoma, Hyper-viscosity of
blood
Symptoms: Sudden painless drop of vision
Signs: Engorged retinal veins
Retinal hemorrhage
Cotton wool spots
Complications of Retinal venous
occlusion:
- Chronic macular edema
(cystoids macular edema)
- Neo-vascular glaucoma
(Rubeotic Glaucoma)
Treatment: Intra-vitreal injection
of Anti-vascular endothelial
growth factor (Anti-VGEF) for
treatment of Chronic macular
edema.
Laser therapy (PRP) for
prevention of Neo-vascular
glaucoma (Rubeotic Glaucoma)
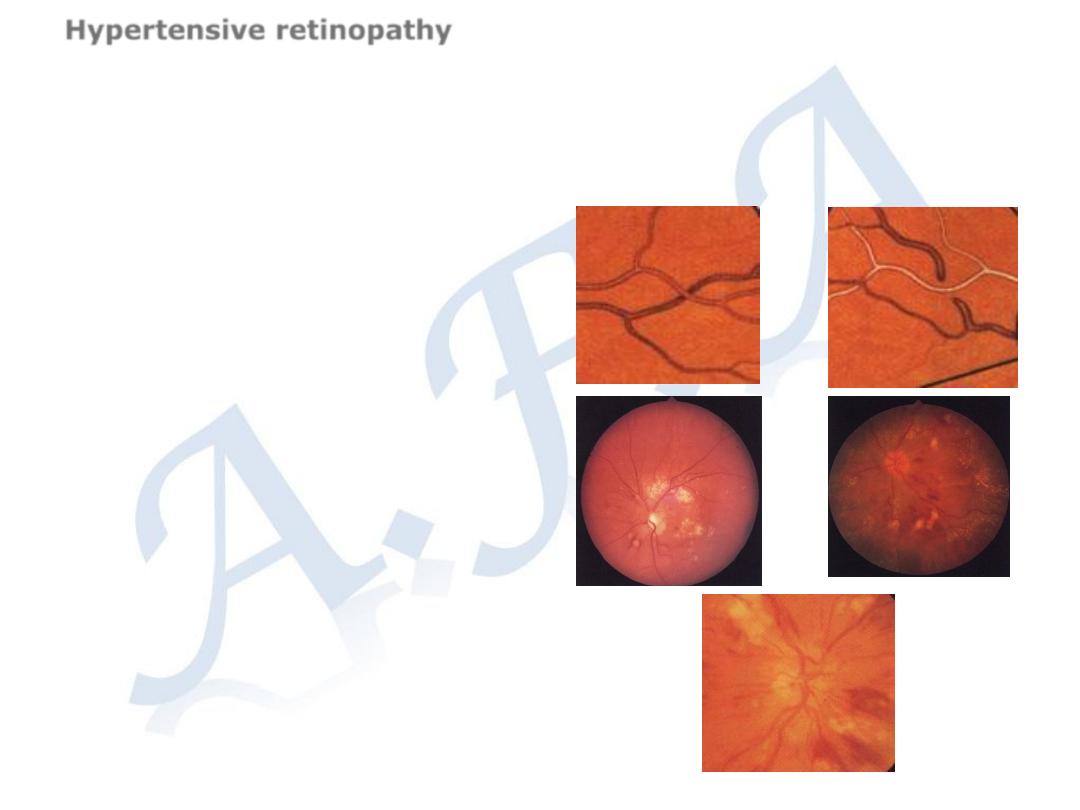
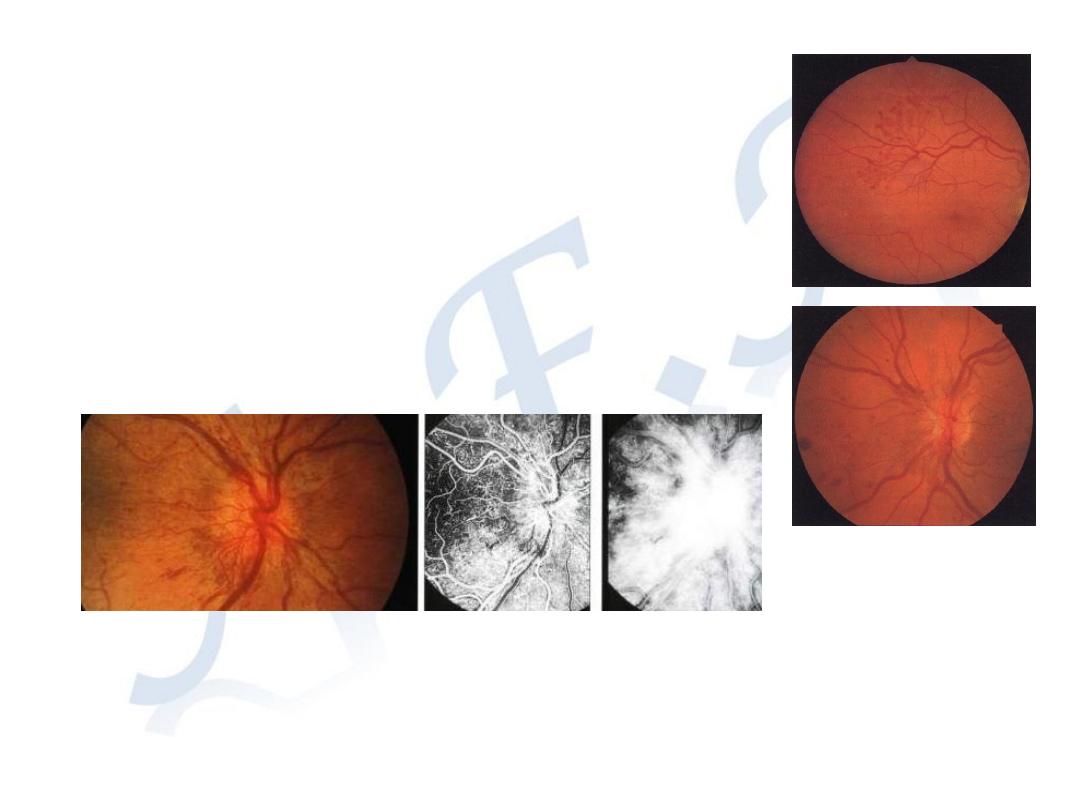
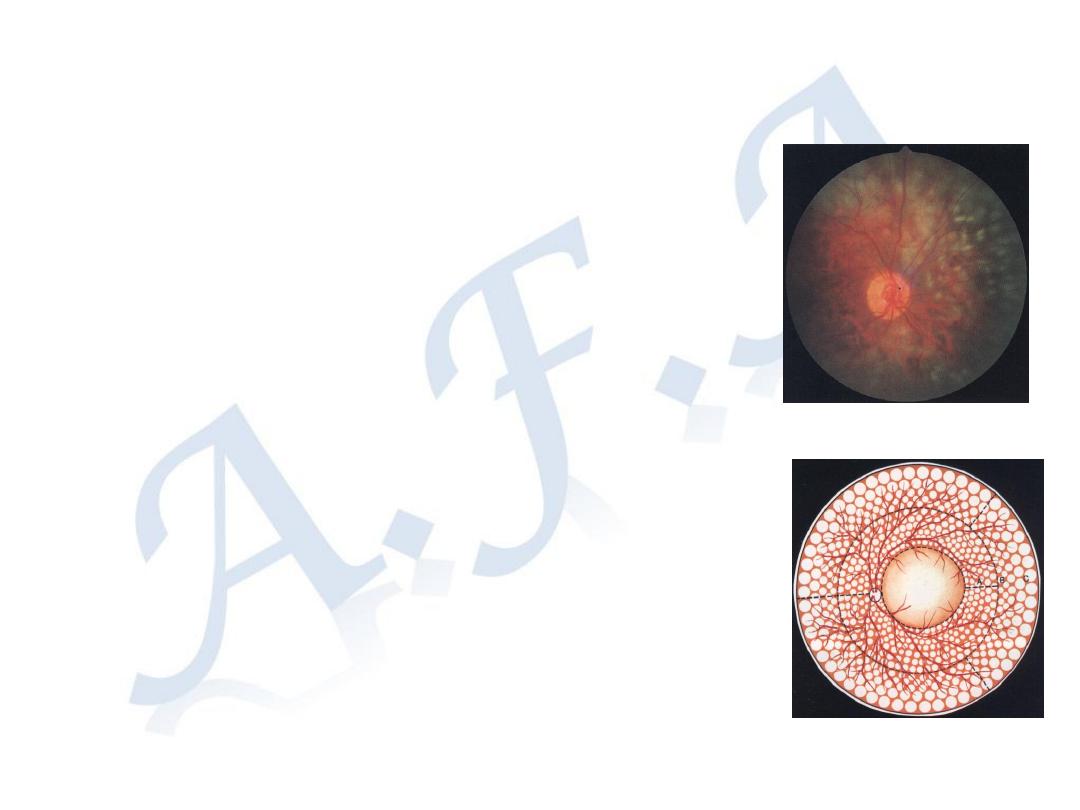
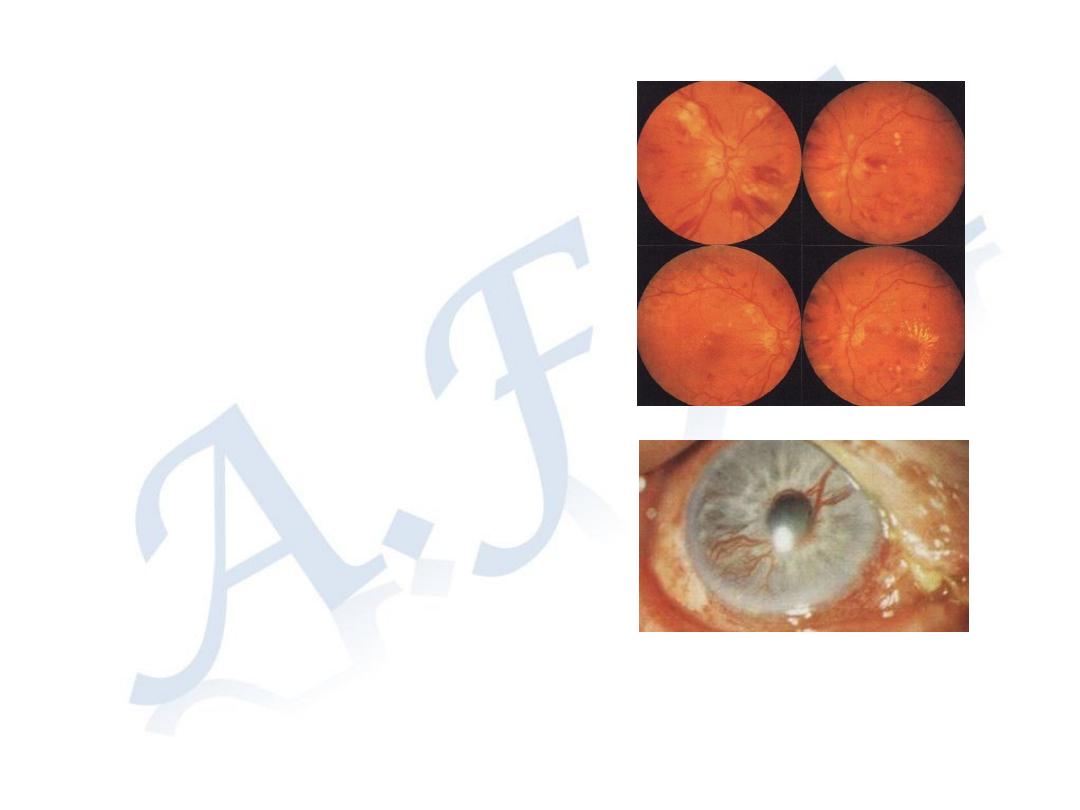
Hypertensive retinopathy
Hypertensive retinopathy depends on; age of the patient,
pre-existing arteriosclerosis, severity and duration of
hypertension
.
1-Narrowing of retinal arterioles,
either focal or diffuse.
2- Artero-veinous crossing
changes (nipping,
concealment)
3-Retinal hemorrhage, hard
exudates, and cotton-wool
spots
4-Optic disc swelling in
accelerated hypertension
Retina consists of two main
layers:
A-The outer layer the
Retinal pigment layer
(RPE)
B-The inner layer the
Sensory layer,
Retinal Detachment (RD)
Retinal pigment epithelium
-
Regenerates the visual pigments
after phototransduction
-
Passage of O
2
and nutrients
from choroid to the
photoreceptors
- Outer retinal blood barrier
-
Absorb scattered light
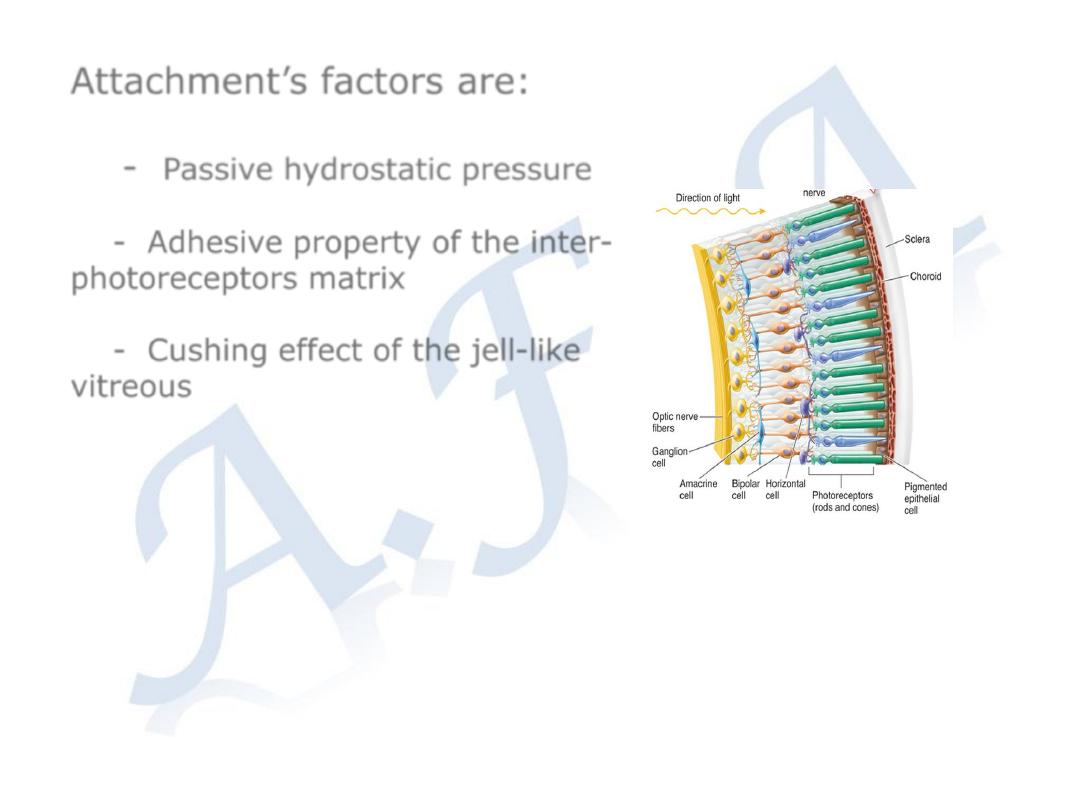
Attachment’s factors are:
-
Passive hydrostatic pressure
- Adhesive property of the inter-
photoreceptors matrix
- Cushing effect of the jell-like
vitreous
The vitreous:
a clear gel occupying two-thirds of the
globe.
98% water.
The remainder consists of hyaluronic acid
and a fine collagen network.There are few
cells.
Attached firmly at:
the peripheral retina (
ora serrata
), and
around the optic disc (
Wiess ring)
.
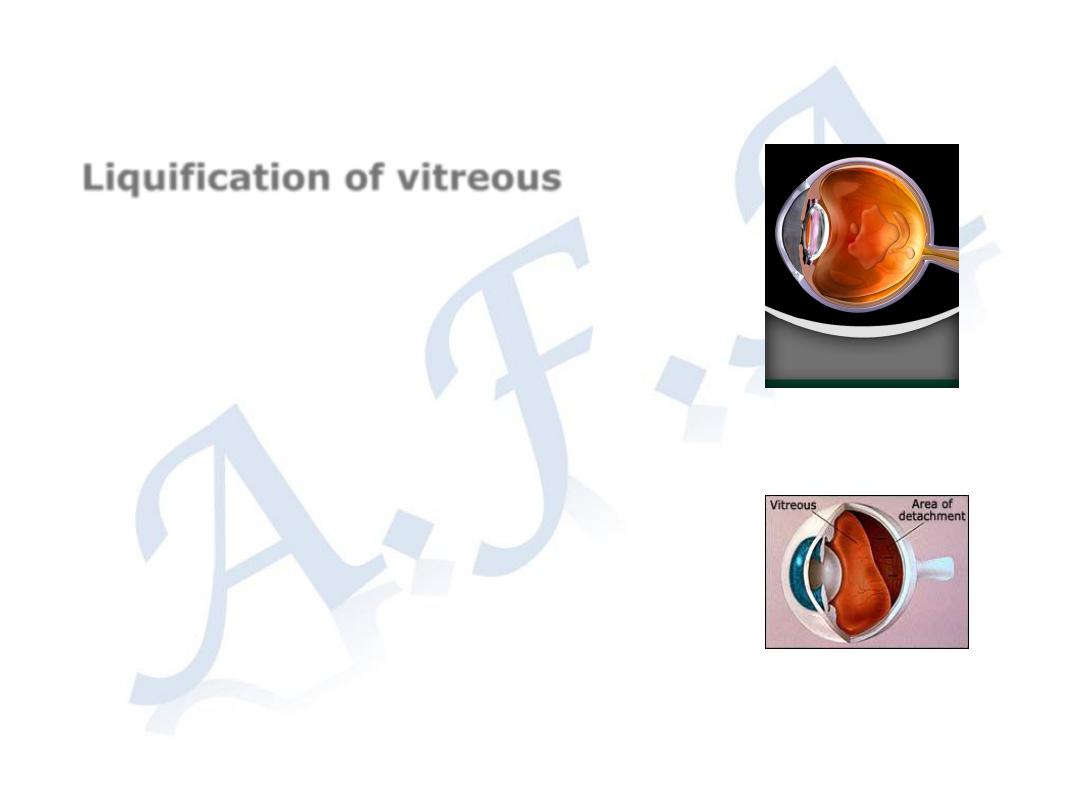
Liquification of vitreous
Degenerative process occurs in elderly
Post-traumatic
High myopia
Vitreo-retinal dystrophies
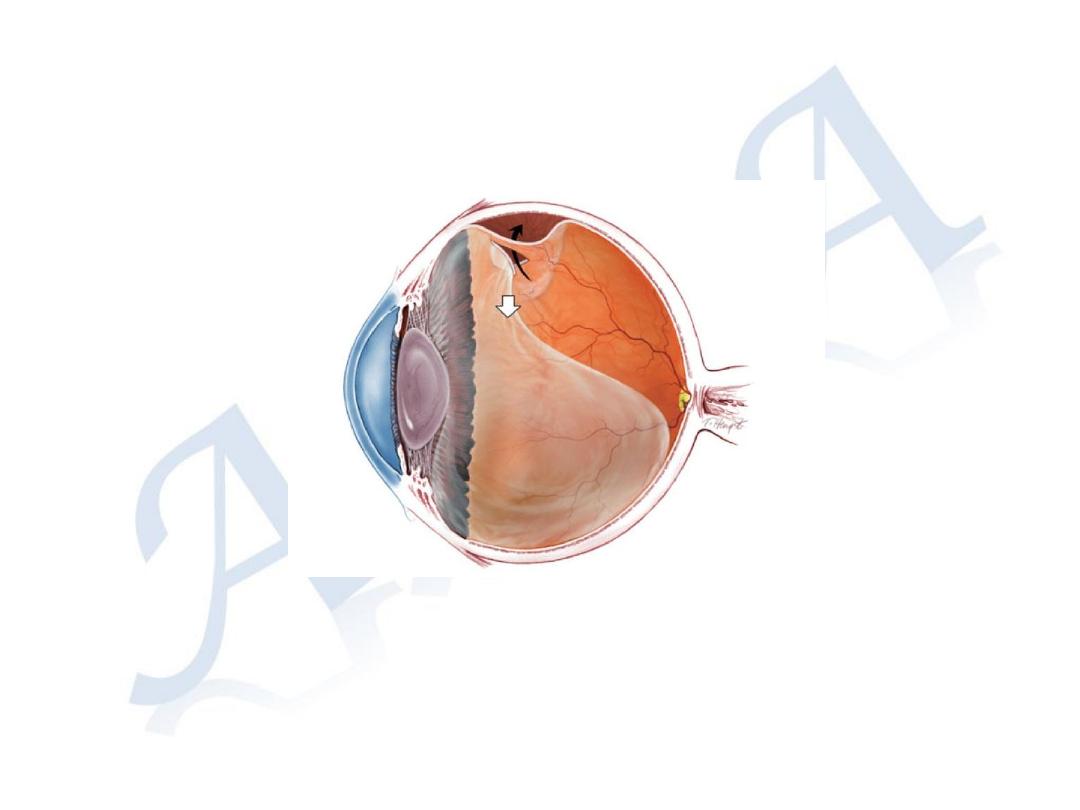
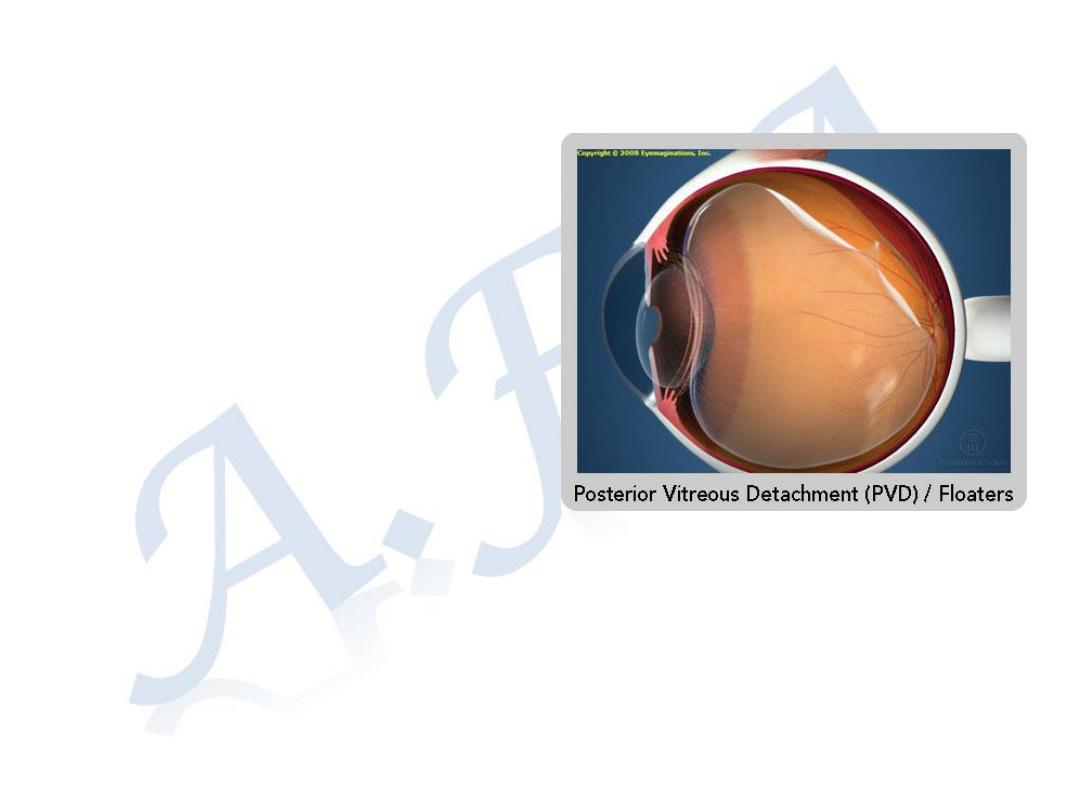
Posterior vitreous Detachment (PVD)
Separation of the posterior vitreous face from the surface of
the retina
Asymptomatic (Majority)
Floaters and photopsia (sometimes)
May predispose to retinal detachment (rarely)

.
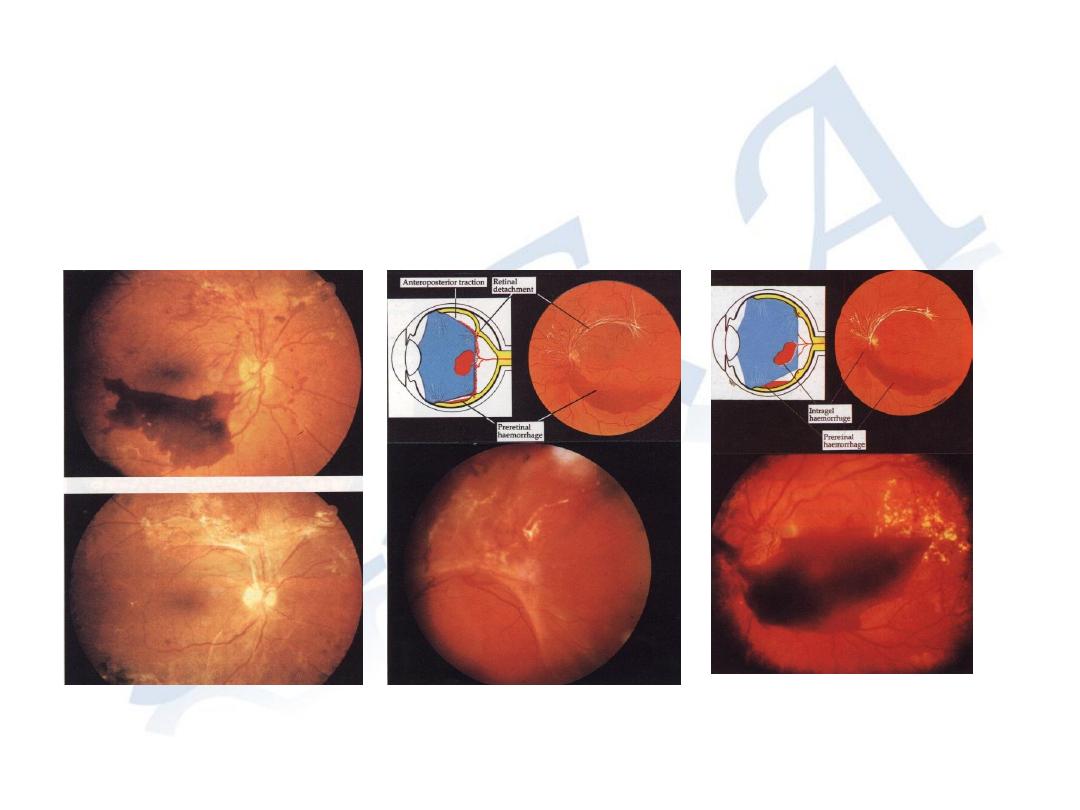
Retinal Detachment (RD
)
Separation of the sensory retina from the
RPE
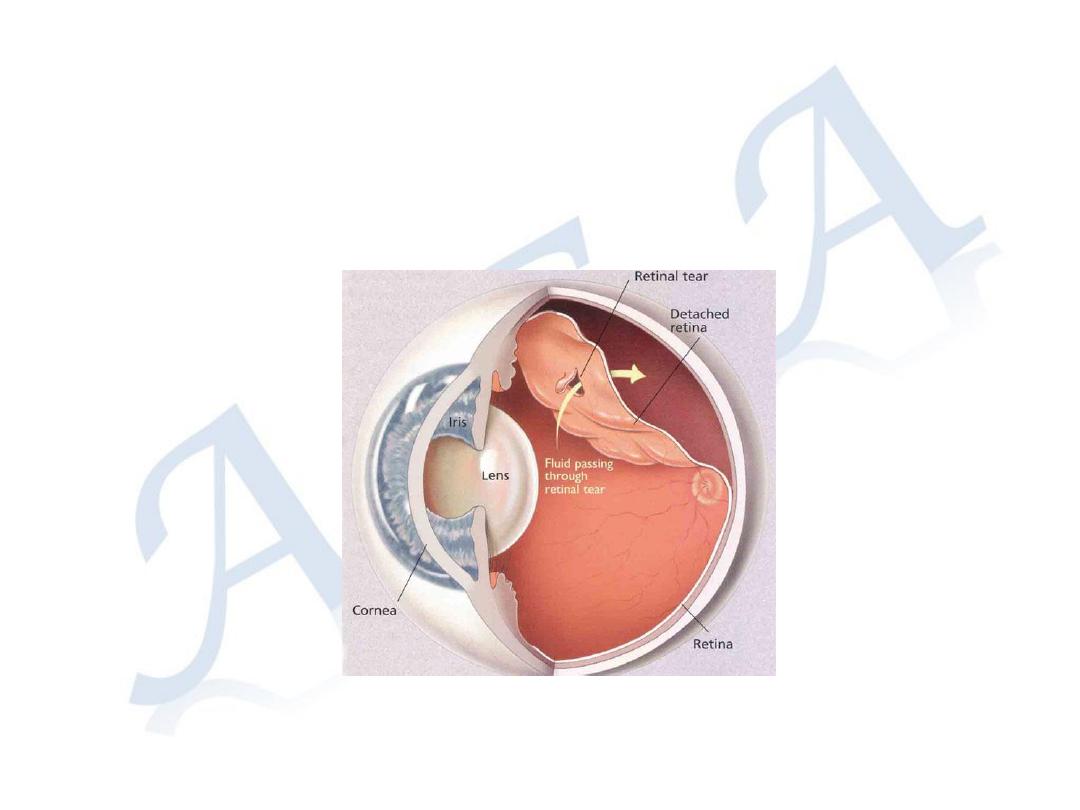
Rhegmatogenous R.D.
is separation of the sensory retina from the RPE by subretinal
fluid derived from liquefied vitreous pass through full thickness
break in the sensory retina.

Predisposing factors:
A- Vitreous liquefaction
Degenerative process occurs in
elderly
Post-traumatic
High myopia
Vitreo-retinal dystrophies
B- Retinal break
a-Underlying retinal weakness
-Diffuse retinal thinning in high
myopia.
-Localized retinal thinning
e.g. Lattice, Snail tract
degeneration (developmental
spindle shape thinning in the
peripheral retina),
b-Posterior vitreous Detachment (PVD)
with abnormal vitre-retinal adhesions
may predispose to retinal break
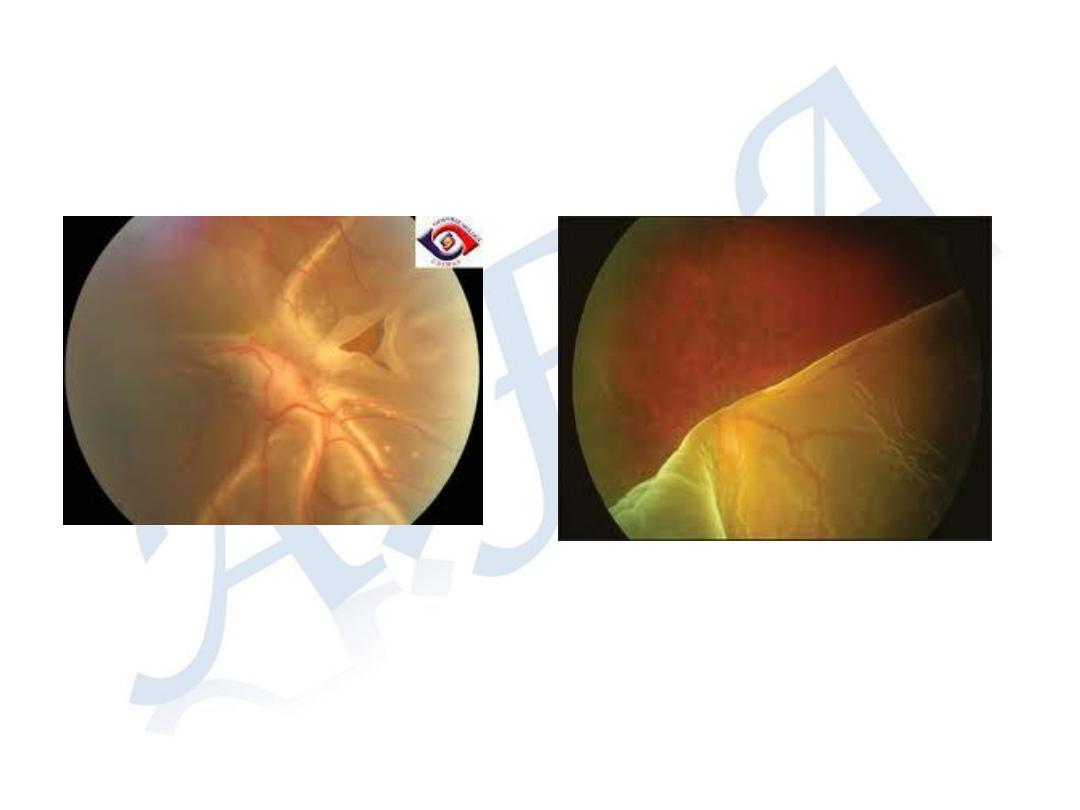
Clinical features:
Symptoms
1-Painless drop of vision
2-Visual field defect
3-Photopsia (perception of flashes of light)
4- Floaters (perception of moving images in
the field of vision, caused by vitreous
opacities that cast a shadow on the retina)
Signs
1-Depressed Visual acuity
2-Impairment of Pupillary light reflex
3-Vitreous opacities
- Pigment cells (Tobacco dust)
4-Abnormal position, elevated retina
with corrugated surface.
5- Retinal break
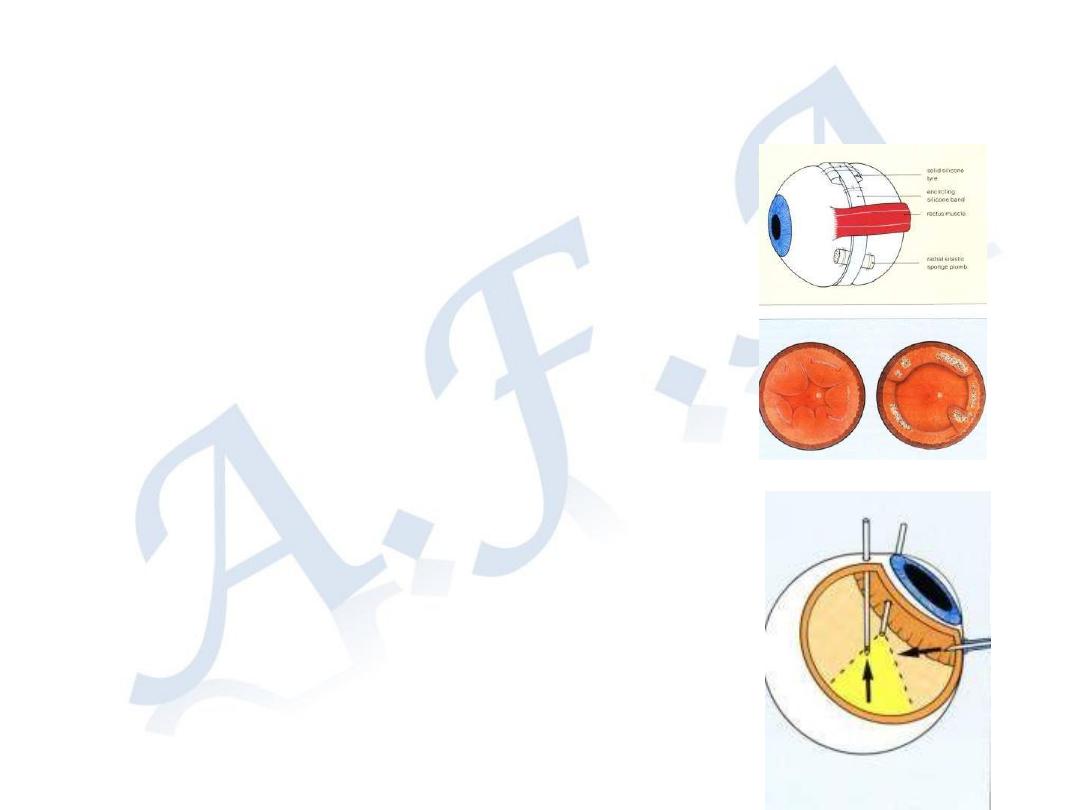
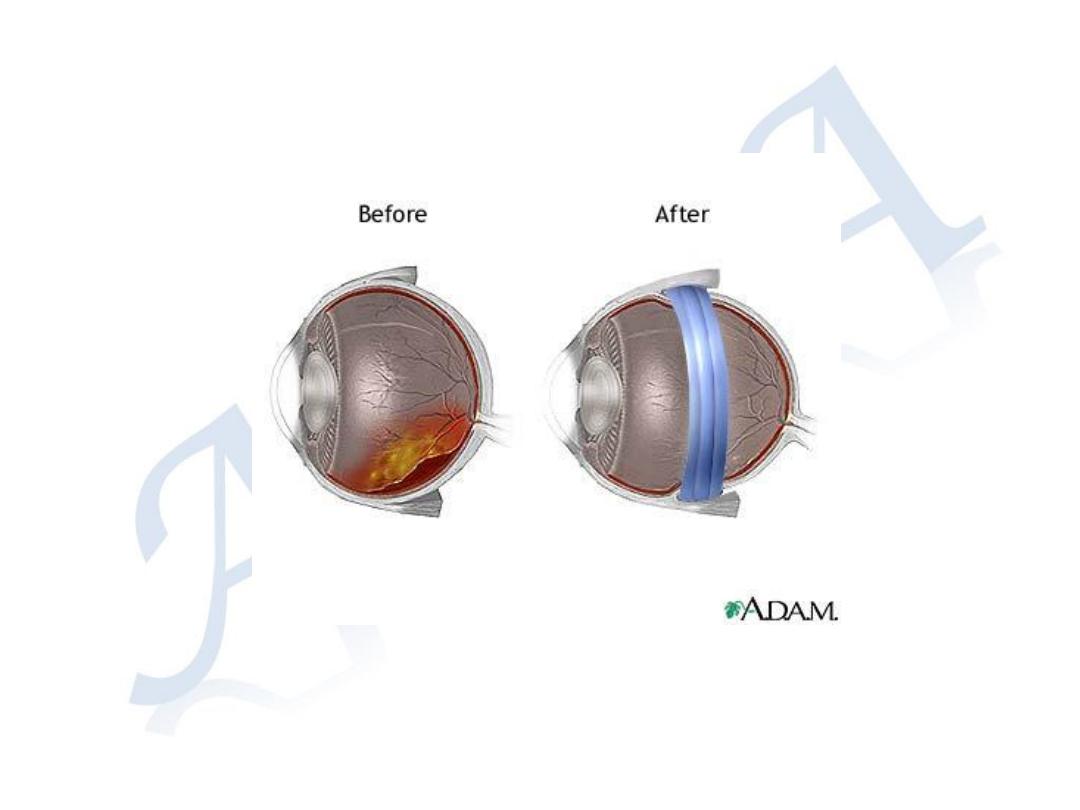
Treatment is surgery:
Repositioning of sensory retina over the
RPE
Drainage of sub-retinal fluid
Sealing of retinal break(s).
Procedures for management of R.R.D.
- Scleral Buckling, for fresh detachment
- Pars Plana Vitrectomy, for long standing
R.D.
◦
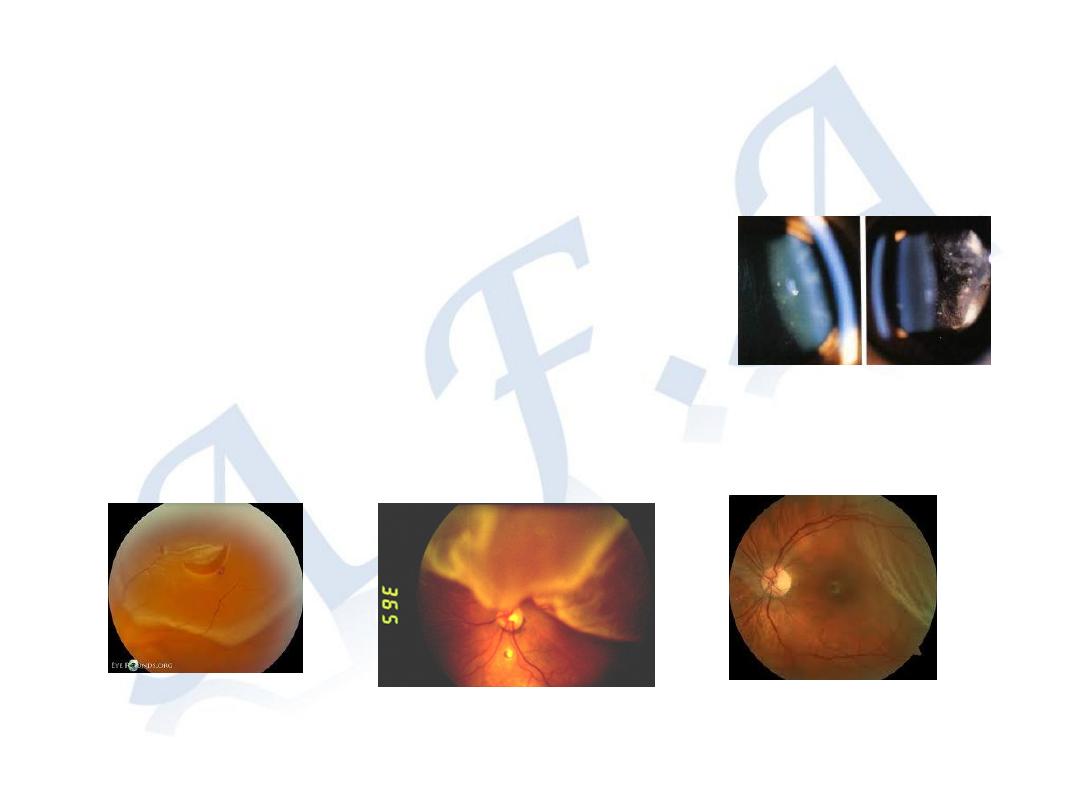
Exudative RD
Separation of the sensory
retina from the RPE by
subretinal fluid derived from
the choroid.
Causes
A- Choroditis
B- Tumors e.g malignant
melanoma of the choroid
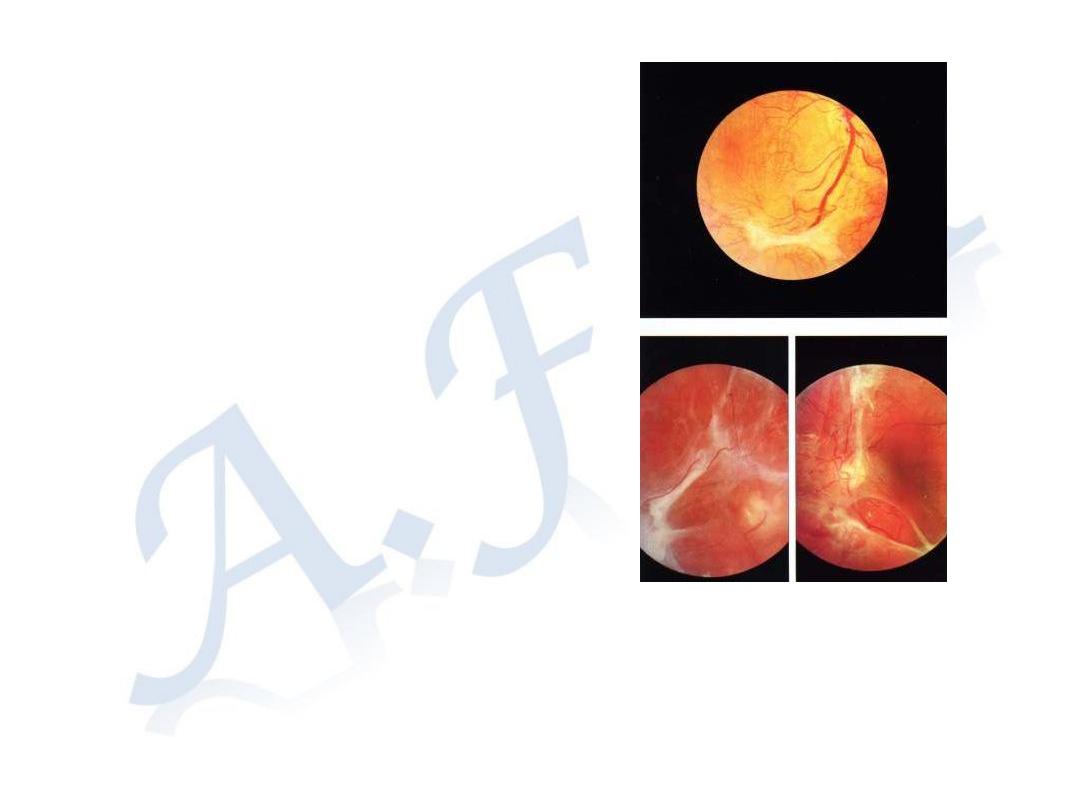
Tractional RD
Separation of the sensory
retina from the RPE due to
contractions of vitreo-retinal
membranes
Causes
Perforated eye trauma
Advanced diabetic
retinopathy
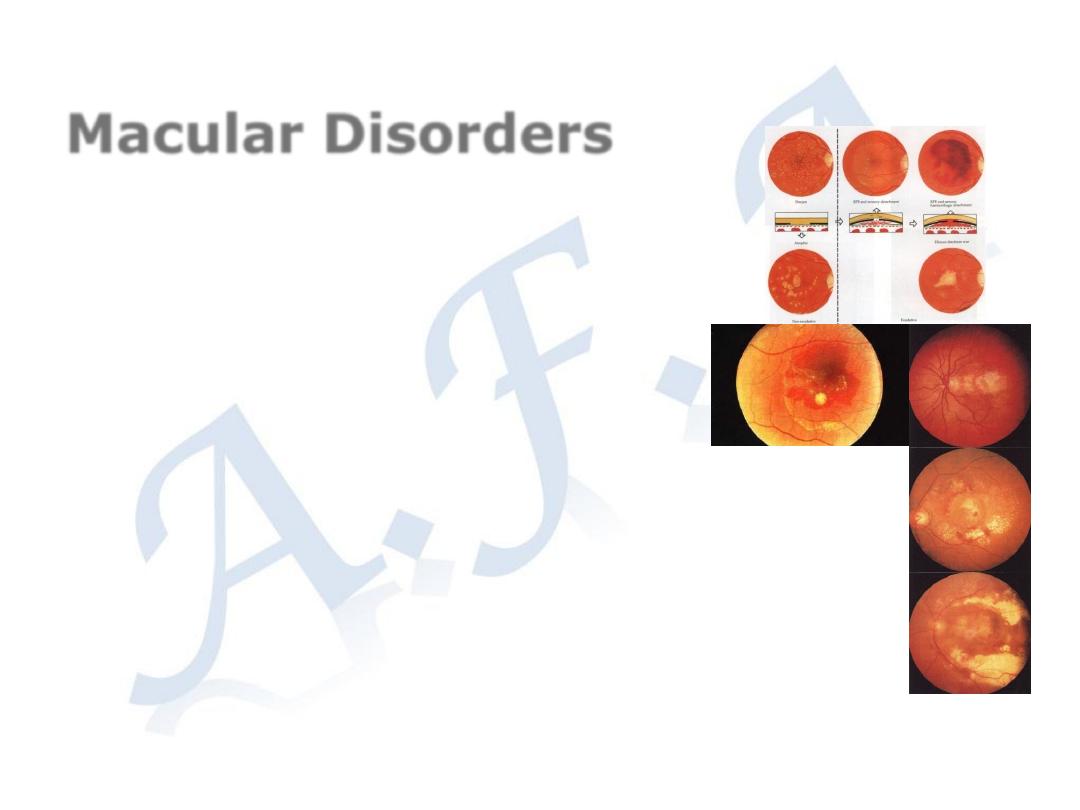
Macular Disorders
Age related macula degeneration
Formation of abnormal neo-vessels derived from
the choroid pass under the sensory retina at
the macular region.
Complications
Retinal and subretinal hemorrhage
subretinal fibrosis
Onset after age 50 years with gradual painless
drop of central vision.
Treatment
Intra-vitral injection of Anti-VEGF
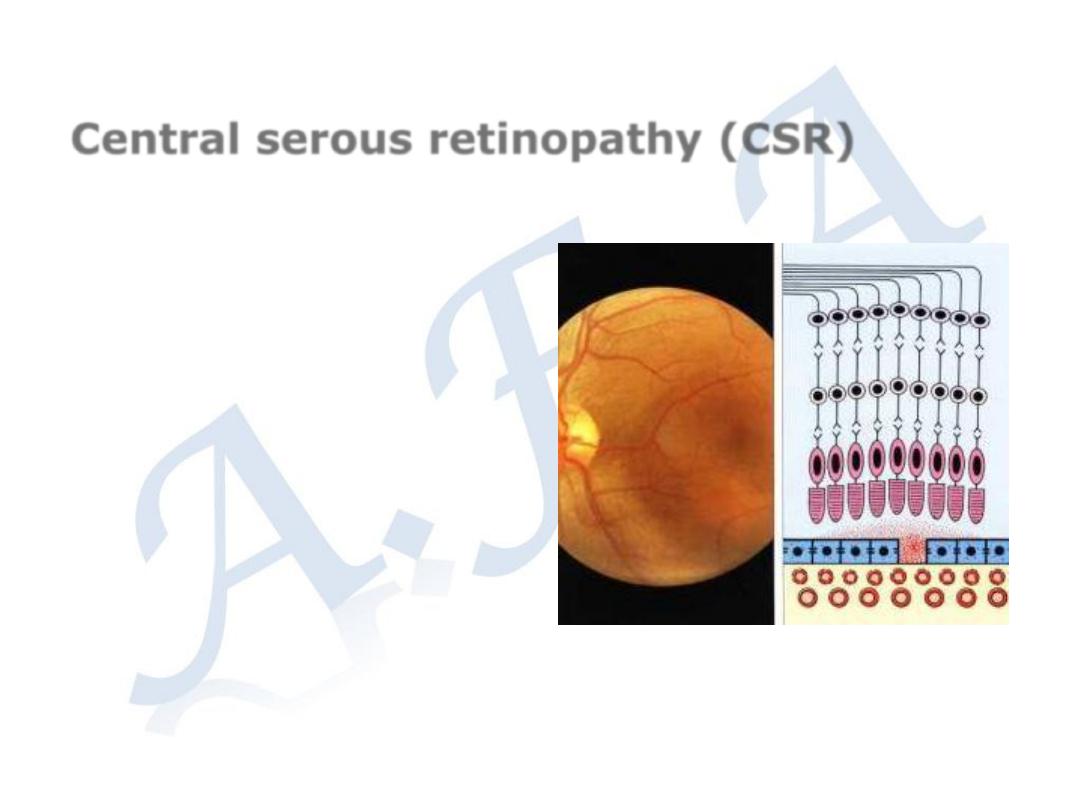
Central serous retinopathy (CSR)
Idiopathic serous detachment of
the sensory retina at the macula
Clinical features:
Young adults
Painless drop of central vision
Treatment:
Spontaneous recovery in the
majority of cases within 6
months.
Laser therapy in resistant cases
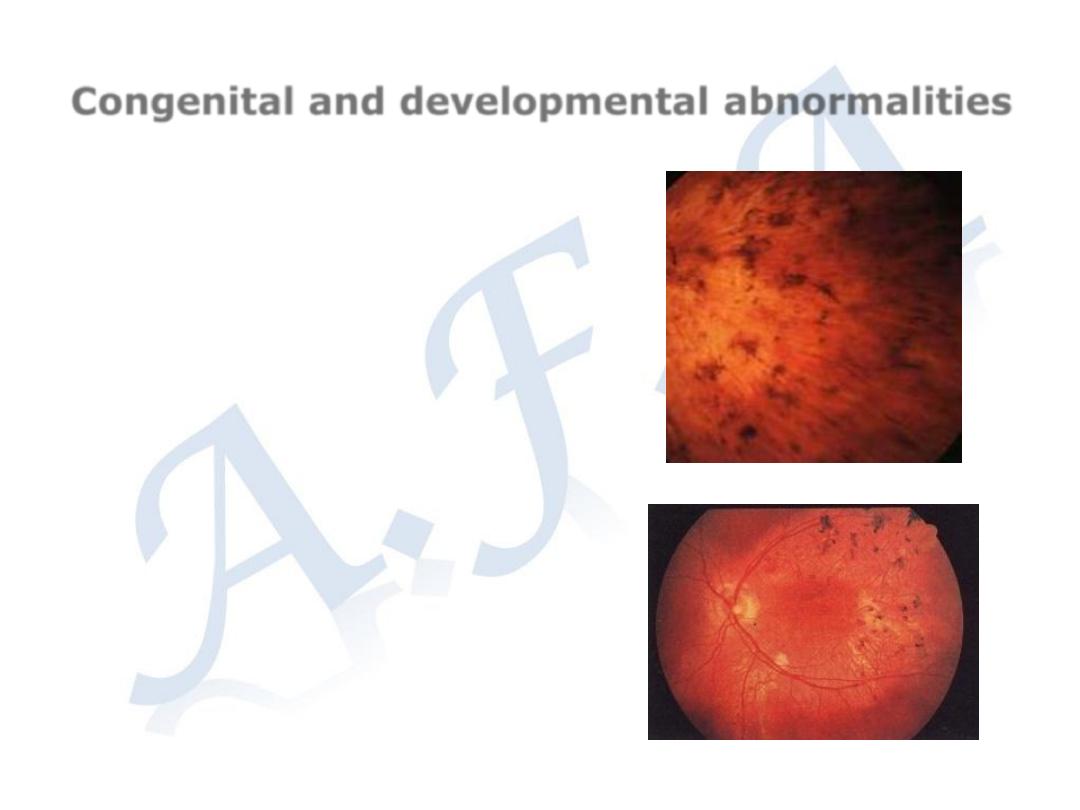
Congenital and developmental abnormalities
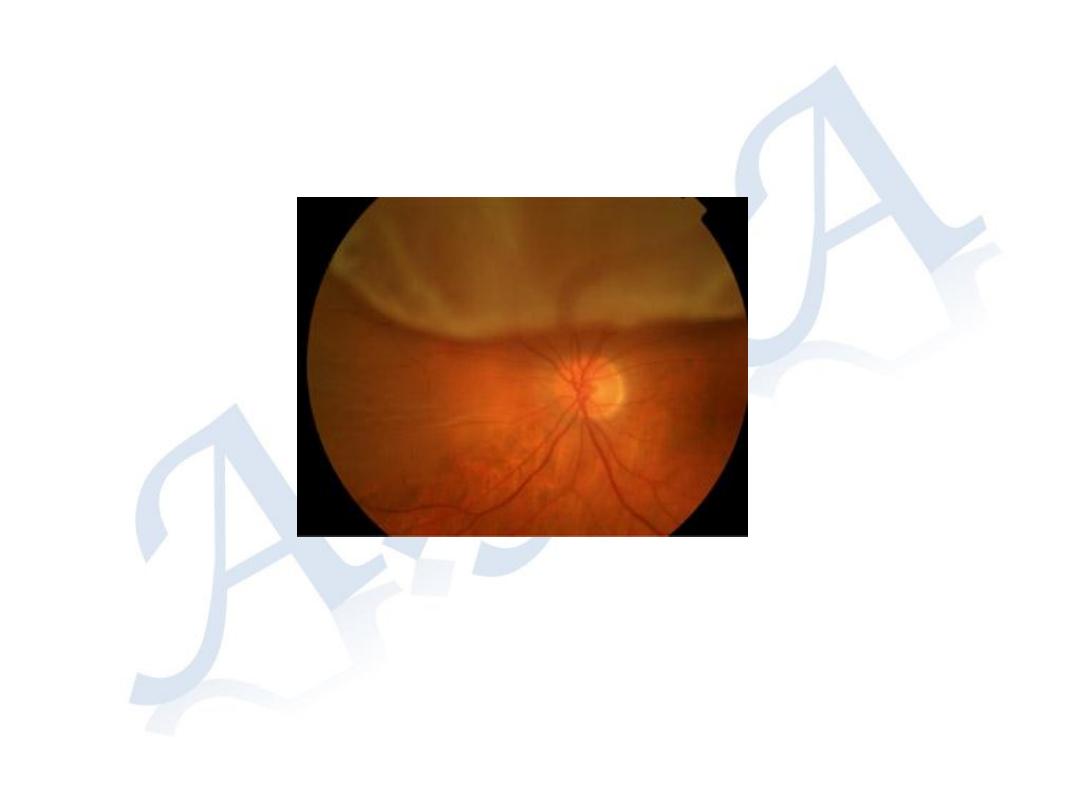
Retinitis pigmentosa
Hereditary
Bilateral
Clinical features:
Night blindness, constriction of visual
field, and drop of central vision
Retina; Bone-specules pigmentation
Attenuated blood vessels
Waxy pale disc
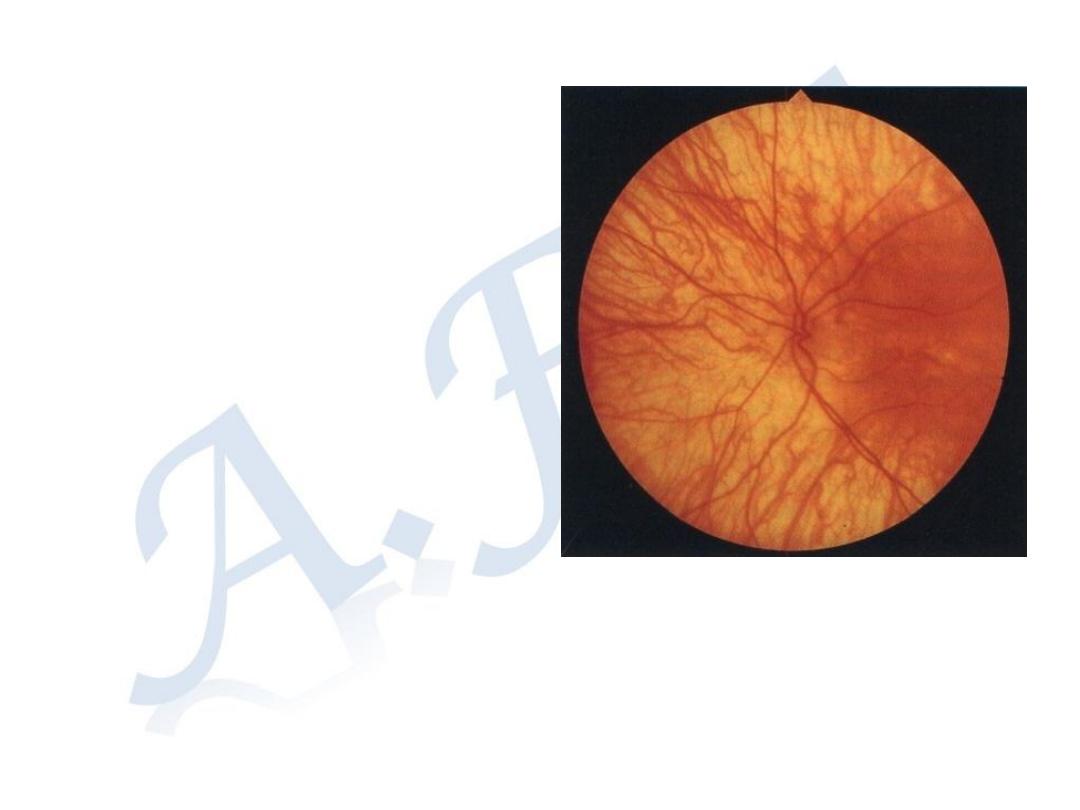
Albinism
Inborn error of metabolism of
melanin
Tyrosinase enzyme deficiency
Ocular or oculo-cutaneous
Bilateral
Poor vision,
Photophobia
Nystagmus (bilateral
involuntary rhythmical
oscillation of the eyes)
Absence of pigmentation in
the iris choroid and RPE
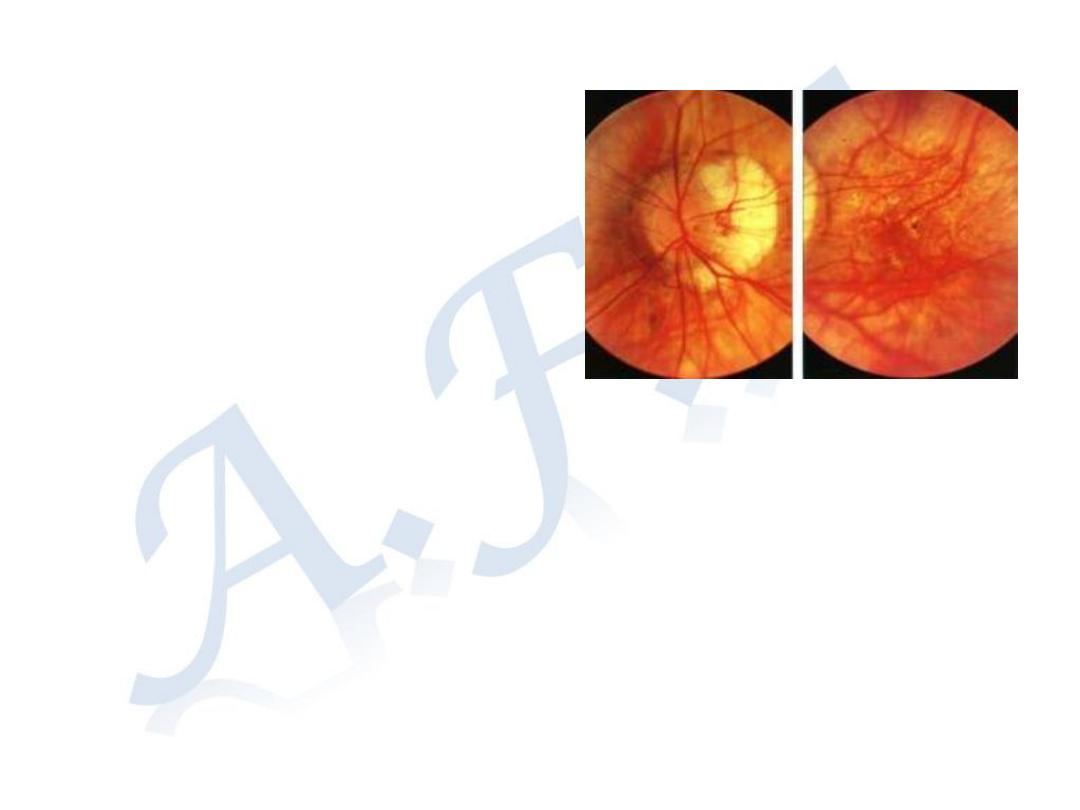
Degenerative Myopia
Autosomal recessive
Manifested early in life
Rapidly progressive during puberty
Clinical features
Symptoms;
Blurring of distant image
Signs:
-Large eye, large cornea and deep anterior chamber
- Sublaxated lens
- Higher prevalence of primary open angle glaucoma
- The entire retina appears attenuated
- Patches of choro-retinal atrophy
- Optic disc is large with myopic crescent
- Retinal degeneration predisposed for retinal breaks and
rhegmatogenous retinal detachment.
.
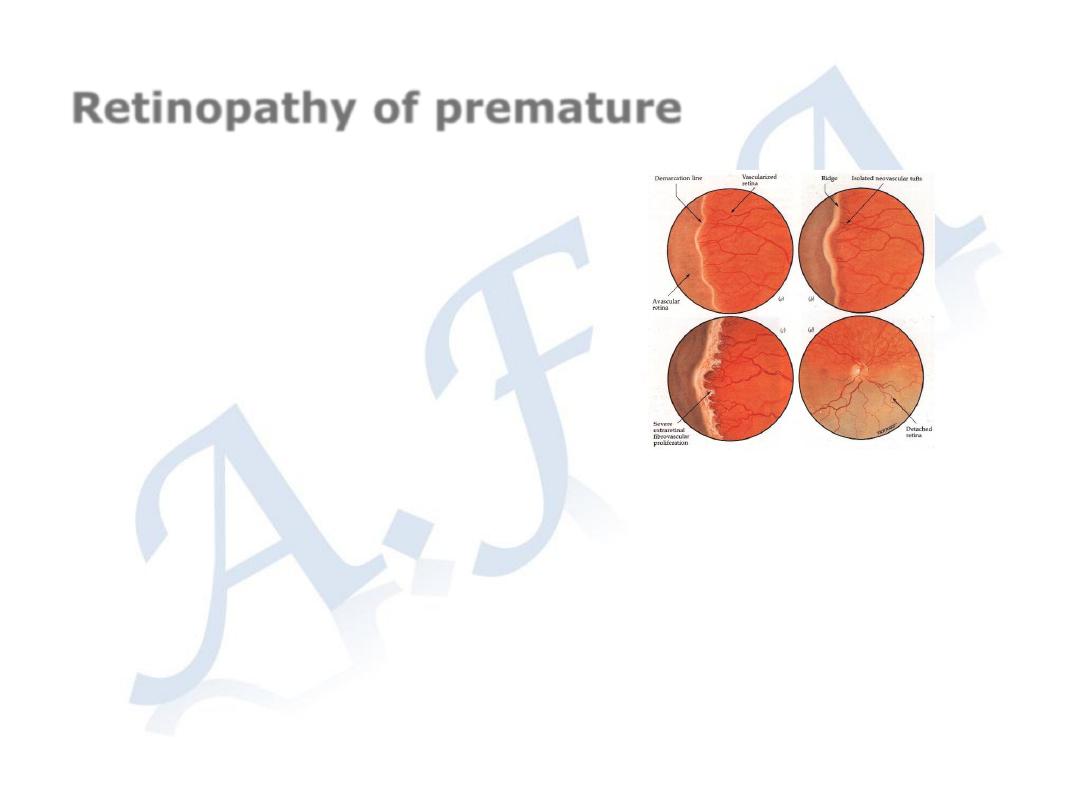
Retinopathy of premature
Risk factors;
1- Gestation less than 32 weeks
2- Birth weight below 1500 gm
3- Exposure to supplemental oxygen
Signs
Abnormal retinal new vasculartization
Retinal and vitreous hemorrhage
Tractional retinal detachment
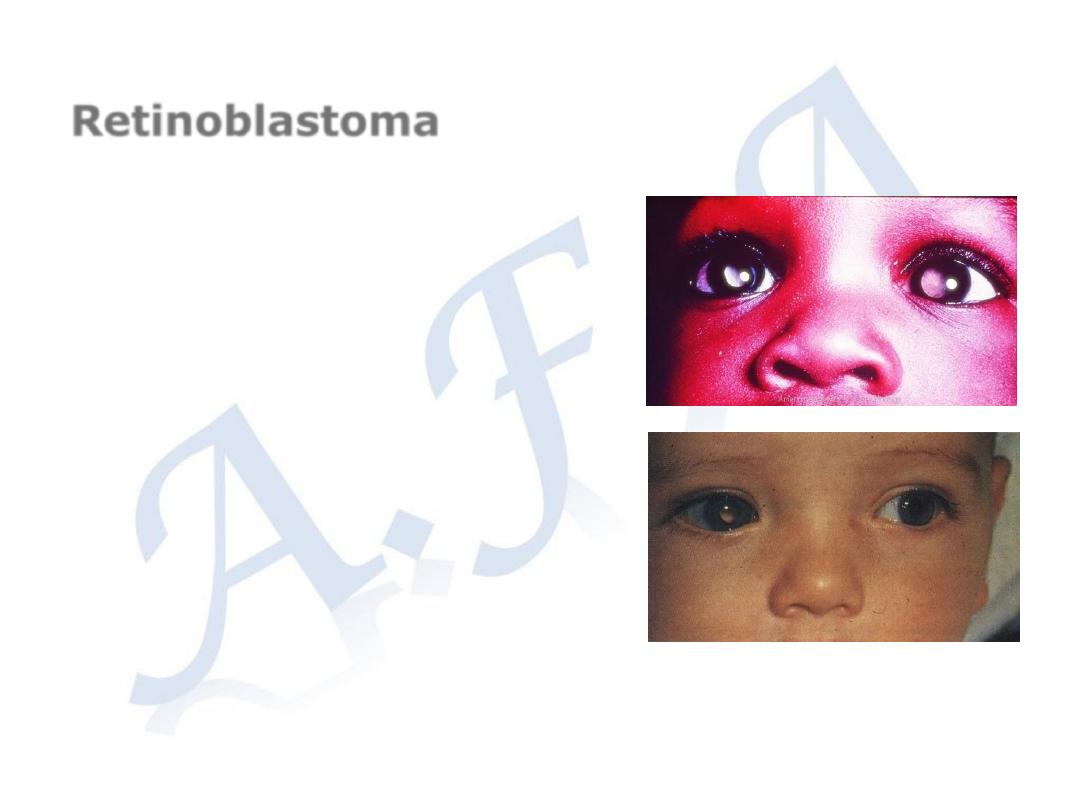
Retinoblastoma
The most common primary ocular tumors
Usually presented before age 2 years
Mode of presentation:
-Leukocorea ; white pupil
-Proptosis; protrusion of the eye-ball
-Pseudo-hypopyon
-Squint
-Secondary glaucoma
Treatment
Laser photo-destruction for small lesions,
Enoculation (removal of the eye-ball) for
large tumors
Chemotherapy
Retinal break
b- Posterior vitreous
detachment- PVD
causes traction over
areas of abnormal
vitreo-retinal adhesions.
This may lead to a
peripheral retinal break,
when the vitreous pulls
away a piece of the
underlying retina