Periodontal Flap Surgery
Periodontal flaps are designed to preserve gingival integrity and to gain access to root surfaces for residual calculus removal and to thoroughly remove granulation tissue so bone defects can be visualized and treated.When flaps need to be repositioned apically or less often, coronally, then the flaps must sit passively at the appropriate level before suturing. To ensure this, buccal and lingual flaps need to be elevated beyond the mucogingival junction so the elasticity of the mucosa allows for flap mobility.
Vertical incisions can aid in flap positioning by allowing the clinician to suture the flap at a different level to the adjacent untreated gingiva.
Palatal flaps are less mobile because of the absence of oral mucosa so that the apical position of the flap depends on how much marginal gingival tissue is discarded using a reverse bevel incision.
A periodontal flap is a section of gingiva and/or mucosa surgically separated from the underlying tissues to provide visibility of and access to the bone and root surface. The flap also allows the gingiva to be displaced to a different location in patients with mucogingival involvement.
Objectives
Flaps are used in pocket therapy for the following:1. Increase accessibility to root deposits for scaling and root planing.
2. Eliminate or reduce pocket depth by resection of the pocket wall.
3. Gain access for osseous resective surgery if it is necessary.
4. Expose the area to perform regenerative methods.
CLASSIFICATION OF FLAPS
Periodontal flaps can be classified based on the following:
• Bone exposure after flap reflection
• Placement of the flap after surgery• Management of the papilla
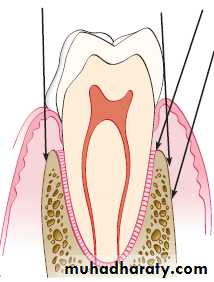
Based on bone exposure after reflection, the flaps are classified as either full-thickness (mucoperiosteal) or partial-thickness (mucosal) flaps.
In full-thickness flaps, all the soft tissue, including the periosteum, is reflected to expose the underlying bone. This complete exposure of and access to the underlying bone is indicated when resective osseous surgery is contemplated.
The partial-thickness flap includes only the epithelium and a layer of the underlying connective tissue. The bone remains covered by a layer of connective tissue, including the periosteum. This type of flap is also called the split-thickness flap. The partial-thickness flap is indicated when the flap is to be positioned apically or when the operator does not want to expose bone.
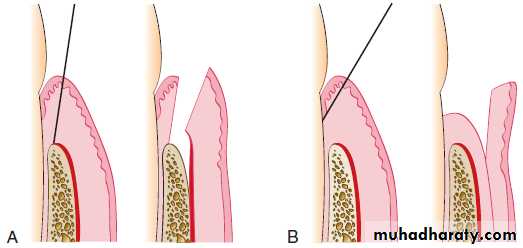
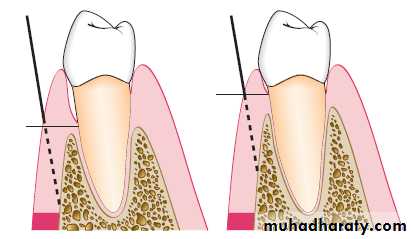
A, Diagram of the internal bevel incision to reflect a full-thickness (mucoperiosteal) flap. Note that the incision ends on the bone to allow for the reflection of the entire flap.
B, Diagram of the internal bevel incision to reflect a partial-thickness flap. Note that the incision ends on the root surface to preserve the periosteum on the bone.
When bone is stripped of its periosteum, a loss of marginal bone occurs, and this loss is prevented when the periosteum is left on the bone. Although usually not clinically significant, the differences may be significant in some cases. The partial-thickness flap may be necessary when the crestal bone margin is thin and exposed with an apically placed flap, or when dehiscences or fenestrations are present. The periosteum left on the bone may also be used for suturing the flap when it is displaced apically.
Based on flap placement after surgery, flaps are classified as
• nondisplaced flaps, when the flap is returned and sutured in its original position, or• displaced flaps, which are placed apically, coronally, or laterally to their original position. Both full-thickness and partial-thickness flaps can be displaced, but to do so, the attached gingiva must be totally separated from the underlying bone, thereby enabling the unattached portion of the gingiva to be movable. However, palatal flaps cannot be displaced because of the absence of unattached gingiva.
Apically displaced flaps have the important advantage of preserving the outer portion of the pocket wall and transforming it into attached gingiva. Therefore these flaps accomplish the double objective of eliminating the pocket and increasing the width of the attached gingiva.
Based on management of the papilla, flaps can be conventional or papilla preservation flaps.
In the conventional flap, the interdental papilla is split beneath the contact point of the two approximating teeth to allow reflection of the buccal and lingual flaps. The incision is usually scalloped to maintain gingival morphology and retain as much papilla as possible. The conventional flap is used (1) when the interdental spaces are too narrow, thereby precluding the possibility of preserving the papilla and (2) when the flap is to be displaced.
Conventional flaps include the modified Widman flap, the undisplaced flap, the apically displaced flap, and the flap for reconstructive procedures.
The papilla preservation flap incorporates the entire papilla in one of the flaps by means of crevicular interdental incisions to sever the connective tissue attachment and a horizontal incision at the base of the papilla, leaving it connected to one of the flaps.
FLAP DESIGN
The design of the flap is dictated by the surgical judgment of the operator and may depend on the objectives of the procedure. The necessary degree of access to the underlying bone and root surfaces and the final position of the flap must be considered in designing the flap. Preservation of good blood supply to the flap is also an important consideration.Two basic flap designs are used. Depending on how the interdental papilla is managed, flaps can either split the papilla (conventional flap) or preserve it (papilla preservation flap).
In the conventional flap procedure, the incisions for the facial and the lingual or palatal flap reach the tip of the interdental papilla or its vicinity, thereby splitting the papilla into a facial half and a lingual or palatal half.
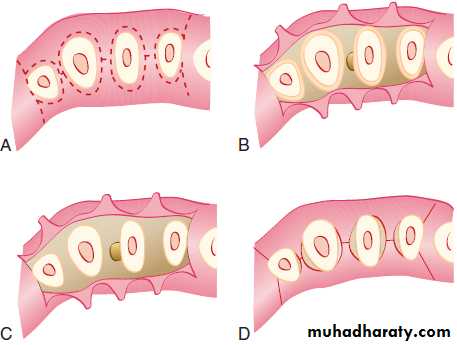
Flap design for conventional or traditional flap technique.
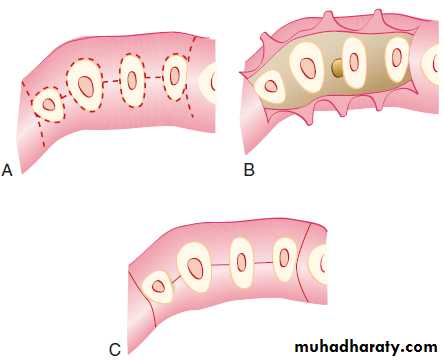
A, Design of incisions: internal bevel incision, splitting the papilla, and vertical incisions are drawn in interrupted lines. B, The flap has been elevated, and the wedge of tissue next to the tooth is still in place. C, All marginal tissue has been removed, exposing the underlying bone. D, Tissue returned to its original position. Proximal areas are not totally covered.Flap design for sulcular incision flap.
A, Design of incisions: sulcular incisions and vertical incisions are depicted by interrupted lines. B, The flap has been elevated, exposing the underlying bone. C, Tissue returned to its original position covers the entire interdental spaces.INCISIONS
Periodontal flaps use horizontal and vertical incisions.
Horizontal Incisions
Horizontal incisions are directed along the margin of the gingiva in a mesial or a distal direction. Two types of horizontal incisions have been recommended: the internal bevel incision, which starts at a distance from the gingival margin and is aimed at the bone crest, and the crevicular incision, which starts at the bottom of the pocket and is directed to the bone margin. In addition, the interdental incision is performed after the flap is elevated.The internal bevel incision is basic to most periodontal flap procedures. It is the incision from which the flap is reflected to expose the underlying bone and root. The internal bevel incision accomplishes three important objectives:
(1) it removes the pocket lining;
(2) it conserves the relatively uninvolved outer surface of the gingiva, which, if apically positioned, becomes attached gingiva; and(3) it produces a sharp, thin flap margin for adaptation to the
bone-tooth junction.
1
This incision has also been termed the first incision because it is the initial incision in the reflection of a periodontal flap, and the reverse bevel incision because its bevel is in reverse direction from that of the gingivectomy incision. The #15 surgical blade is used most often to make this incision. That portion of the gingiva left around the tooth contains the epithelium of the pocket lining and the adjacent granulomatous tissue. It is discarded after the crevicular (second) and interdental (third) incisions are performed.
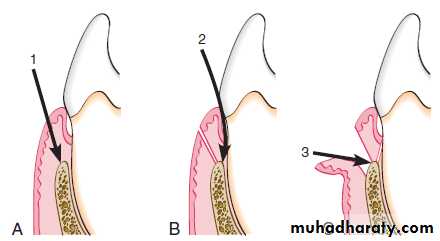
Three incisions necessary for flap surgery. A, First (internal bevel) incision; B, second (crevicular) incision; C, third (interdental) incision.
The internal bevel incision starts from a designated area on the gingiva and is directed to an area at or near the crest of the bone. The starting point on the gingiva is determined by whether the flap is apically displaced or not displaced.
The crevicular incision, also termed the second incision, is made from the base of the pocket to the crest of the bone. This incision, together with the initial reverse bevel incision, forms a V-shaped wedge ending at or near the crest of bone. This wedge of tissue contains most of the inflamed and granulomatous areas that constitute the lateral wall of the pocket, as well as the junctional epithelium and the connective tissue fibers that still persist between the bottom of the pocket and the crest of the bone. The incision is carried around the entire tooth. The beak-shaped blade is usually used for this incision.
2
A periosteal elevator is inserted into the initial internal bevel incision, and the flap is separated from the bone. The most apical end of the internal bevel incision is exposed and visible.
With this access, the surgeon is able to make the third incision, or interdental incision, to separate the collar of gingiva that is left around the tooth. The Orban knife is usually used for this incision. The incision is made not only around the facial and lingual radicular area but also interdentally, connecting the facial and lingual segments to free the gingiva completely around the tooth.
3
These three incisions allow the removal of the gingiva around the tooth (i.e., the pocket epithelium and the adjacent granulomatous tissue). A curette or a large scaler can be used for this purpose. After removal of the large pieces of tissue, the remaining connective tissue in the osseous lesion should be carefully curetted so that the entire root and the bone surface adjacent to the teeth can be observed.
Flaps can be reflected using only the horizontal incision if sufficient access can be obtained in this way and if apical, lateral, or coronal displacement of the flap is not anticipated. If vertical incisions are not made, the flap is called an envelope flap.
Vertical Incisions
Vertical or oblique releasing incisions can be used on one or both ends of the horizontal incision, depending on the design and purpose of the flap. Vertical incisions at both ends are necessary if the flap is to be apically displaced.
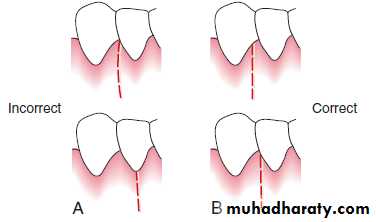
In general, vertical incisions in the lingual and palatal areas are avoided. Facial vertical incisions should not be made in the center of an interdental papilla or over the radicular surface of a tooth.
Incisions should be made at the line angles of a tooth either to include the papilla in the flap or to avoid it completely.
The vertical incision should also be designed to avoid short flaps (mesiodistal) with long, apically directed incisions because this could jeopardize the blood supply to the flap.
Incorrect (A) and correct (B) locations of a vertical incision.
This incision should be made at the line angles to prevent splitting of a papilla or incising directly over a radicular surface.Several investigators proposed the interdental denudation procedure, which consists of horizontal, internal bevel, nonscalloped incisions to remove the gingival papillae and denude the interdental space. This technique completely eliminates the inflamed interdental tissue. Healing is by secondary intention and results in excellent gingival contour. It is contraindicated when bone grafts are used for the graft material placed interdentally will not be covered.
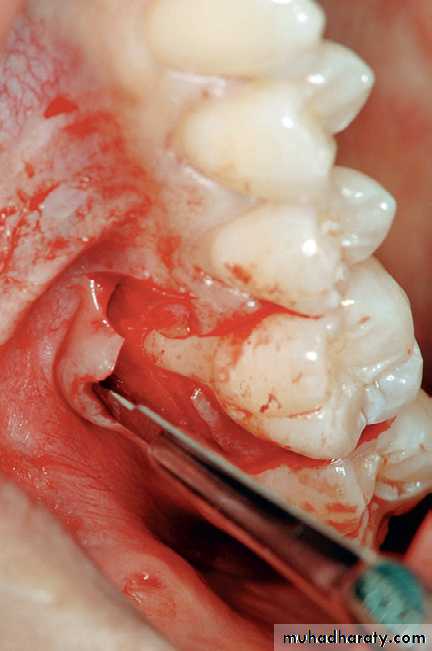
ELEVATION OF THE FLAP
When a full-thickness flap is desired, reflection of the flap is accomplished by blunt dissection. A periosteal elevator is used to separate the mucoperiosteum from the bone by moving it mesially, distally, and apically until the desired reflection is accomplished.Sharp dissection is necessary to reflect a partial-thickness flap. A surgical scalpel (#15) is used.
HEALING AFTER FLAP SURGERY
Immediately after suturing (up to 24 hours), a connection between the flap and the tooth or bone surface is established by a blood clot, which consists of a fibrin reticulum with many polymorphonuclear leukocytes, erythrocytes, debris of injured cells, and capillaries at the edge of the wound. Bacteria and an exudate or transudate also result from tissue injury.One to 3 days after flap surgery, the space between the flap and the tooth or bone is thinner and epithelial cells migrate over the border of the flap, usually contacting the tooth at this time. When the flap is closely adapted to the alveolar process, there is minimal inflammatory response.
One week after surgery, an epithelial attachment to the root has been established by means of hemidesmosomes and a basal lamina. The blood clot is replaced by granulation tissue derived from the gingival connective tissue, the bone marrow, and the periodontal ligament.
Two weeks after surgery, collagen fibers begin to appear parallel to the tooth surface. Union of the flap to the tooth is still weak because of the presence of immature collagen fibers, although the clinical aspect may be almost normal.
One month after surgery, a fully epithelialized gingival crevice with a well-defined epithelial attachment is present. There is a beginning functional arrangement of the supracrestal fibers.
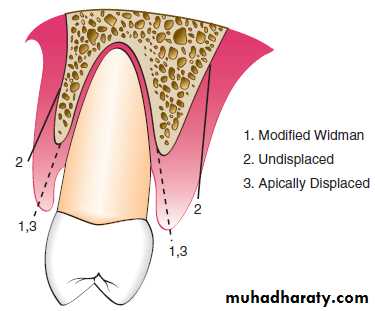
MODIFIED WIDMAN FLAP
As called by Ramfjord and Nissle in 1974. This technique offers the possibility of establishing an intimate postoperative adaptation of healthy collagenous connective tissue to tooth surfaces and provides access for adequate instrumentation of the root surfaces and immediate closure of the area.Step 1: The initial incision is an internal bevel incision to the alveolar crest starting 0.5 to 1 mm away from the gingival margin. Scalloping follows the gingival margin. Care should be taken to insert the blade in such a way that the papilla is left with a thickness similar to that of the remaining facial flap. Vertical relaxing incisions are usually not needed.
Step 2: The gingiva is reflected with a periosteal elevator
Step 3: A crevicular incision is made from the bottom of the
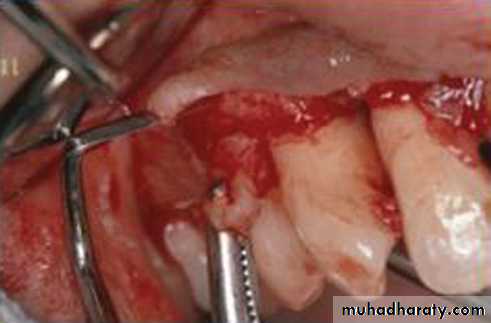
pocket to the bone, circumscribing the triangular wedge of tissue containing the pocket lining.Step 4: After the flap is reflected, a third incision is made in the interdental spaces coronal to the bone with a curette or an interproximal knife and the gingival collar is removed.
Step 5: Tissue tags and granulation tissue are removed with a curette. The root surfaces are checked, then scaled and planed if needed. Residual periodontal fibers attached to the tooth surface should not be disturbed.
Step 6: Bone architecture is not corrected, except if it prevents good tissue adaptation to the necks of the teeth. Every effort is made to adapt the facial and lingual interproximal tissue adjacent to each other in such a way that no interproximal bone remains exposed at the time of suturing. The flaps may be thinned to allow for close adaptation of the gingiva around the entire circumference of the tooth and to each other interproximally.
Step 7: Continuous, independent sling sutures are placed in both the facial and palatal and covered with a periodontal surgical pack.
UNDISPLACED FLAP
Currently, the undisplaced flap may be the most frequently performed type of periodontal surgery. It differs from the modified Widman flap in that the soft tissue pocket wall is removed with the initial incision; thus it may be considered an “internal bevel gingivectomy.”To perform this technique without creating a mucogingival problem, the clinician should determine that enough attached gingiva will remain after removal of the pocket wall.
Step 1: The pockets are measured with the periodontal probe, and a bleeding point is produced on the outer surface of the gingiva to mark the pocket bottom.
Step 2: The initial, or internal bevel, incision is made after scalloping the bleeding marks on the gingiva. The incision is usually carried to a point apical to the alveolar crest, depending on the thickness of the tissue.
Step 3: The second, or crevicular, incision is made from the bottom of the pocket to the bone to detach the connective tissue from the bone.
Step 4: The flap is reflected with a periosteal elevator (blunt dissection).
Step 5: The third, or interdental, incision is made with an interdental knife.
Step 6: The triangular wedge of tissue created by the three incisions is removed with a curette.
Step 7: The area is debrided, removing all tissue tags and granulation tissue using sharp curettes.
Step 8: After the necessary scaling and root planing, the flap edge should rest on the root-bone junction.
Step 9: A continuous sling suture is used to secure the facial and
the lingual or palatal flaps. Then, periodontal dressing is placed.
Palatal Flap
The surgical approach to the palatal area differs from that for other areas because of the character of the palatal tissue and the anatomy of the area. The palatal tissue is all attached, keratinized tissue and has none of the elastic properties associated with other gingival tissues. Therefore the palatal tissue cannot be apically displaced, and a partial-thickness (split-thickness) flap cannot be accomplished. The location of the initial incision is important for the final placement of the flap. The initial incision for the palatal flap should allow the flap, when sutured, to be precisely adapted at the root-bone junction.Flaps should be thin to adapt to the underlying osseous tissue and provide a thin, knifelike gingival margin. It is best to thin the flaps before their complete reflection because a free, mobile flap is difficult to hold for thinning. This can accomplished by proper placement of incisions
If thinning the palatal flap needed after it has been reflected, it can be accomplished by holding the inner portion of the flap with a mosquito hemostat or Adson forceps as the inner connective tissue is carefully dissected away with a sharp #15 scalpel blade.
APICALLY DISPLACED FLAP
With some variants, the apically displaced flap technique can be used for (1) pocket eradication and/or (2) widening the zone of attached gingiva. Depending on the purpose, it can be a full-thickness (mucoperiosteal) or a split-thickness (mucosal) flap. The split-thickness flap requires more precision and time, as well as a gingival tissue thick enough to split, but it can be more accurately positioned and sutured in an apical position using a periosteal suturing technique.Indications / Specific
• Crown lengthening• Defected attached ingiva
• Altered alveolar ridge
• Implant surgery (Immediate load)
• Frenotomy
• Vestibular deepening
• Root denudation
• Root sensitivity
• Esthetic problems
Step 1: An internal bevel incision is made no more than about 1 mm from the crest of the gingiva and directed to the crest of the bone.
Step 2: Crevicular incisions are made, then interdental incisions are performed, and the wedge of tissue that contains the pocket wall is removed.
Step 3: Vertical incisions are made extending beyond the mucogingival junction to provide adequate mobility to the flap for flap apical displacement.. If the objective is a full-thickness flap, it is elevated by blunt dissection with a periosteal elevator. If a split-thickness flap is required, it is elevated using sharp dissection with a knife to split it, leaving a layer of connective tissue, including the periosteum, on the bone.
Step 4: After removal of all granulation tissue, scaling and root planing, and osseous surgery if needed, the flap is displaced apically.
Step 5: If a full-thickness flap was performed, a sling suture around the tooth prevents the flap from sliding to a position more apical than that desired, and the periodontal dressing can avoid its movement in a coronal direction.
A partial thickness flap is sutured to the periosteum using a direct loop suture or a combination of loop and anchor suture. A dry foil is placed over the flap before covering it with the dressing to prevent the introduction of pack under the flap.