Breathing Circuits In Anaesthesia
Key conceptsBecause insufflation avoids any direct patient contact, there is no rebreathing of exhaled gases. Ventilation cannot be controlled and the inspired gas contains unpredictable amounts of entrained atmospheric air.
Long breathing tubes with high compliance increase the difference between the volume of gas delivered to a circuit by a reservoir bag or ventilator and the volume actually delivered to the patient.
The adjustable pressure limiting (APL) valve should be fully open during spontaneous ventilation so that circuit pressure remains negligible throughout inspiration and expiration.
Because a fresh gas flow equal to minute ventilation is sufficient to prevent rebreathing, the Mapleson A design is the most efficient Mapleson circuit for spontaneous ventilation.
Con.
The Mapleson D circuit is efficient during controlled ventilation, because fresh gas flow forces alveolar air away from the patient and toward the APL valve.The drier the soda lime, the more likely it will absorb and degrade volatile anesthetic.
Malfunction of either unidirectional valve in a circle system may allow rebreathing of carbon dioxide, resulting in hypercapnia.
With an absorber, the circle system prevents rebreathing of carbon dioxide at fresh gas flows that are considered low (FGF ≤ 1 L) or even FGF equal to the uptake of anesthetic gases and oxygen by the patient and the circuit itself (closed system anesthesia).
con
Because of the unidirectional valve, apparatus dead space in a circle system is limited to the area distal to the point of inspiratory and expiratory gas mixing at the Y-piece. Unlike Mapleson circuits, the circle system tube length does not directly affect dead space.
The fraction of inspired oxygen (FIO2) delivered by a resuscitator breathing system to the patient is directly proportional to the oxygen concentration and flow rate of the gas mixture supplied to the resuscitator (usually 100% oxygen) and inversely proportional to the minute ventilation delivered to the patient.
DEFINITION
A breathing system is defined as an assembly of components which connects the patient’s airway to the anaesthetic machine creating an artificial atmosphere, from and into which the patient breathes.
It primarily consists of
a) A fresh gas entry port/delivery tube through which the gases are delivered from the machine to the systems;b) A port to connect it to the patient’s airway;
c) A reservoir for gas, in the form of a bag or a corrugated tube to meet the peak inspiratory flow requirements;
d) An expiratory port/valve through which the expired gas is vented to the atmosphere;
e) A carbon dioxide absorber if total rebreathing is to be allowed and
f) Corrugated tubes for connecting these components.
Flow directing valves may or may not be used.
REQUIREMENTS OF A BREATHING SYSTEM
Essential:The breathing system must
a) deliver the gases from the machine to the alveoli in the same concentration as set and in the shortest possible time;
b) effectively eliminate carbon-dioxide;
c) have minimal apparatus dead space; and
d) have low resistance.
Desirable:
The desirable requirements area) economy of fresh gas
b) conservation of heat
c) adequate humidification of inspired gas
d) Light weight
e) convenience during use
f) efficiency during spontaneous as well as controlled ventilation
g) adaptability for adults, children and mechanical ventilators
h) provision to reduce theatre pollution.
• Classification
• Open
• No boundary and no dead space• Oxygen tubing near patient
• Semi-open• Partial boundary between airway and atmosphere
• Schimmelbusch mask• Semi-closed
• Fully bounded. Prevents entry of atmospheric air but vents excess fresh gas• Mapleson systems
• Closed• No venting of excess gas
• Circle systems at low flows
Many Configurations• No Soda Lime
• Soda Lime
• Uni
• Non - Rebreathing
• Circle System
• Circle System
• Bi
• a) Afferent reservoir systems.
• Mapleson A, B & C
• Lack’s system.
• b) Enclosed afferent reservoir systems
• Miller’s (1988)
• c) Efferent reservoir systems
• Mapleson D, E & F
• Bain’s system
• d) Combined systems
• Humphrey ADE
• Waters Canister
Schimmelbusch mask
Mapleson systems
Circle system
Components of a breathing system
Adjustable pressure-limiting valveReservoir bag
Tubing
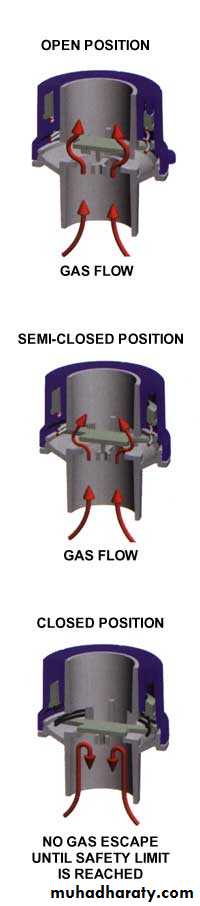
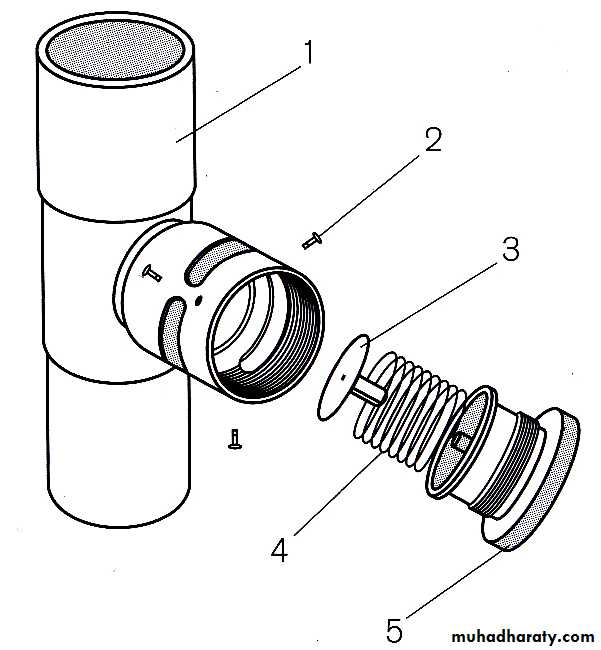
Adjustable pressure-limiting valve
Spill valve, pop-off valve, expiratory valve, relief valve.
Designed to vent gas during positive pressure.Pressure of less than 0.1 kPa activates the valve when open.
Components3 ports:
inlet, patient and exhaust port- latter can be open to atmosphere or connected to the scavenging systemLightweight disc sits on a knife-edge seating- held in place by a spring
Tension in the spring and therefore the valve’s opening pressure is controlled by the valve dial.
The Heidbrink valve
Male tapers at both ends
Retaining screwsDisc
Spring
Valve top
Single use APL valve( Inter - surgical)
Operation of an Inter - surgical single use APL valve
Neoprene flap valve
Valve topScrew threded insert
Overpressure relief valve
Spring
Valve in open position
Valve shut
Overpressure relief valve operatedMechanism of action
One-way, adjustable, spring-loaded valve
Valve allows gases to escape when the pressure in the breathing system exceeds the valve’s opening pressureDuring spontaneous ventilation, the patient generates a positive pressure during expiration, causing the valve to open
During positive pressure ventilation, a controlled leak is produced in inspiration by adjusting the valve dial, allowing control of the patient’s airway pressure
Reservoir bag
Antistatic rubber or plasticEllipsoid in shape
Standard adult size is 2 l (range from 0.5 to 6 l)Mechanism of action
Accommodates fresh gas flow during expiration acting as a reservoir available for the following inspiration.Acts as a monitor of patient’s ventilatory pattern during spontaneous breathing and also a very inaccurate guide to tidal volume
Used to assist or control ventilation
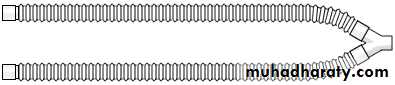
Tubing
Corrugated or smooth
Different lengths depending on system being usedAllow humidification of inspired air
Parallel and coaxial arrangements available
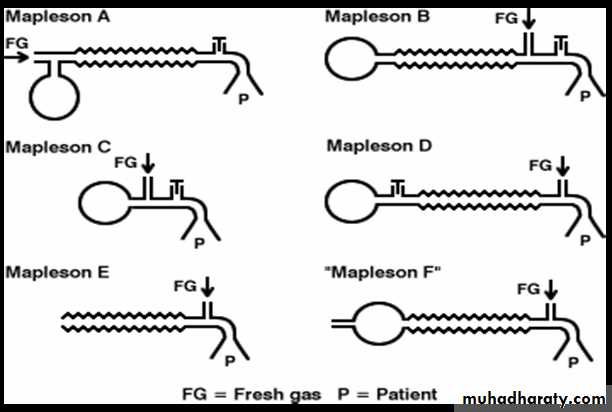
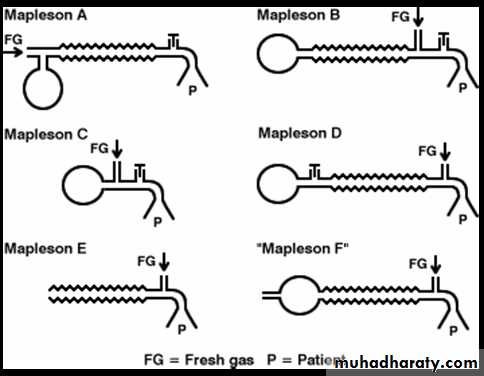
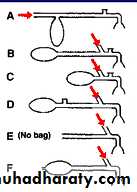
Mapleson classification
Mapleson classified breathing systems in 1954 into 5 types.Mapleson classification
Bi-directional flow
a) Afferent reservoir systems.
Mapleson A
Mapleson B
Mapleson C
Lack’s system.
B) Efferent reservoir systems
Mapleson DMapleson E
Mapleson F
Mapleson classification
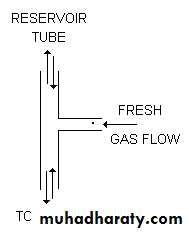
Is that part of the breathing system which delivers the fresh gas from the machine to the patient. If the reservoir is placed in this limb as in Mapleson A, B, C and Lack’s systems, they are called afferent reservoir systems (ARS).Afferent limb
Efferent limb
Is that part of the breathing system which carries expired gas from the patient and vents it to the atmosphere through the expiratory valve/port.
If the reservoir is placed in this limb as in Mapleson D, E, F and Bain systems, they are called efferent reservoir systems (ERS).
Bi - Directional Flow
Systems with bi-directional flow are extensively used.
These systems depend on the FGF for effective elimination of CO2.
Understanding these systems is most important as their functioning can be manipulated by changing parameters like Fresh gas flow, alveolar ventilation, apparatus dead space, etc.
Fresh Gas Supply
Fresh gas flow (FGF) forms one of the essential requirements of a breathing system.If there is no FGF into the system, the patient will get suffocated.
If the FGF is low, most systems do not eliminate carbon-dioxide effectively, and if there is an excess flow there is wastage of gas. So, it becomes imperative to specify optimum FGF for a breathing system for efficient functioning.
If the system has to deliver a set concentration in the shortest possible time to the alveoli, the FGF should be delivered as near the patient’s airway as possible.
Elimination Of Carbon-Dioxide
Normal production of carbon-dioxide in a 70 kg adult is 200 ml per minute and it is eliminated through the lungs.Normal end-tidal concentration of carbon-dioxide is 5%. Hence, for eliminating 200 ml of carbon-dioxide as a 5% gas mixture, the alveolar ventilation has to be:
200 x 100 = 4,000 ml.
5
This 4000 ml is the normal alveolar ventilation. Any breathing system connected to an adult’s airway should provide a minimum of 4 litres per minute of carbon-dioxide free gas to the alveoli for eliminating carbon-dioxide. If the alveolar ventilation becomes less than 4 litres per minute, it would lead to hypercarbia.
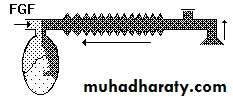
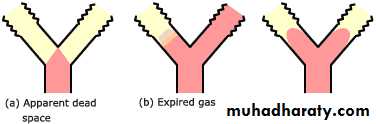
Apparatus Dead Space
It is the volume of the breathing system from the patient-end to the point up to which, to and fro movement of expired gas takes place.
Extent of dead space in various systems
In an afferent reservoir system with adequate FGF, the apparatus dead space extends up to the expiratory valve positioned near the patient.
Expiratory valve
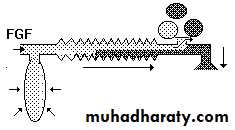
Patient endIf the FG enters the system near the patient-end as in an efferent reservoir system, the dead space extends up to the point of FG entry.
FGF
Patient end
In systems where inspiratory and expiratory limbs are separate, it extends up to the point of bifurcation.
Inspiratory limb
Expiratory limbPatient end
Importance of FGFThe dynamic dead space will depend on the FGF and the alveolar ventilation.
The dead space is minimal with optimal FGF.
If the FGF is reduced below the optimal level, the dead space increases .
The whole system will act as dead space if there is no FGF.
Increasing the FGF above the optimum level will only lead to wastage of FG.
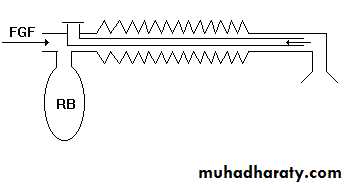
Mapleson A
Corrugated rubber or plastic tubing:110- 130 cm in length
Reservoir bag at machine end
APL valve at the patient end.
Tube Volume > Tidal Volume (550mls)
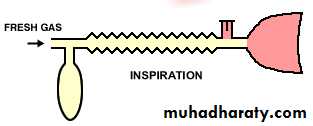
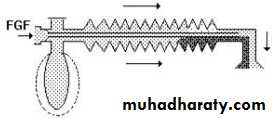
Mapleson ‘A’/Magill’s system:Functional analysis:
Spontaneous breathing:The system is filled with fresh gas before connecting to the patient. When the patient inspires, the fresh gas from the machine and the reservoir bag flows to the patient, and as a result the reservoir bag collapses.
The expired gas, initial part of which is the dead space gas, pushes the FG from the corrugated tube into the reservoir bag and collects inside the corrugated tube .
Expiratory pause –
Fresh gas washes the expired gas out of the reservoir tube, filling it with fresh gas for the next inspiration.Rebreathing of alveolar gas can be prevented if the fresh gas flow = patient's minute ventilation.
Body weight (kg)
Fresh gas flow (l/min)
5
0.6
10
1.1
20
1.9
40
3.3
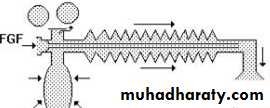
Controlled ventilation:
To facilitate IPPV the expiratory valve has to be partly closed.
During inspiration, the patient gets ventilated with FG and part of the FG is vented through the valve after sufficient pressure has developed to open the valve.
• FGF
• Dead space gas• Alveolar gas
During expiration, the FG from the machine flows into the reservoir bag and all the expired gas (i.e., dead space gas and alveolar gas) flows back into the corrugated tube till the system is full .
• FGF
• Dead space gas• Alveolar gas
During the next inspiration the alveolar gas is pushed back into the alveoli followed by the FG. When sufficient pressure is developed, part of the expired gas and part of the FG escape through the valve .
• FGF
• Dead space gas• Alveolar gas
This leads to considerable rebreathing, as well as excessive waste of fresh gas. Hence these systems are inefficient for controlled ventilation.
A fresh gas flow of >20 L/minute is required to prevent rebreathing during controlled ventilation.
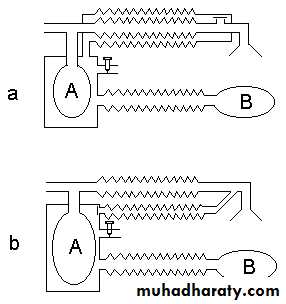
Mapleson A (Magill circuit)
Mapleson A- Lack systemCoaxial modification of Magill Mapleson A
1.5 m length
FGF through outside tube (30mm), exhaled gases through inner tube.
Inner tube wide in diameter (14 mm) to reduce resistance to expiration(1.6cm H2O).
Reservoir bag at machine end
APL valve at machine end.
Better for spontaneous ventilation.
Lack’s system
This system functions like a Mapleson A system both during spontaneous and controlled ventilation.The only difference is that the expired gas instead of getting vented through the valve near the patient, is carried by an efferent tube placed coaxially and vented through the valve placed near the machine end . This facilitates easy scavenging of expired gas.
Lack’s system
The fresh gas inlet near the patient, distal to the expiratory valve.The expiratory valve opens when pressure in the circuit increases, and a mixture of alveolar gas and fresh gas is discharged.
During the next inspiration a mixture of retained fresh gas and alveolar gas is inhaled.
Rebreathing is avoided with fresh gas flow rates of greater than twice the minute ventilation for both spontaneous and controlled ventilation.
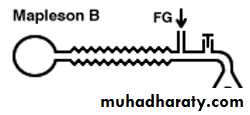
Mapleson B system
This circuit is also known as the Water's circuit.It is similar in construction to the Mapleson B, but the main tubing is shorter.
A fresh gas flow equal to twice the minute ventilation is required to prevent re - breathing. Carbon dioxide builds up slowly with this circuit.
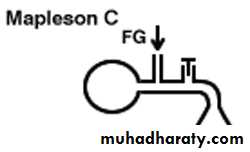
Mapleson C system
Mapleson B & C systems
In order to reduce the re - breathing of alveolar gas and to improve the utilization of FG during controlled ventilation, the FG entry was shifted near the patient.
This allows a complete mixing of FG and expired gas.
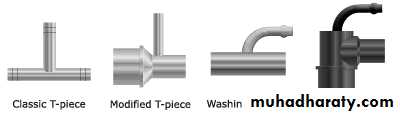
The end result is that these systems are neither efficient during spontaneous nor during controlled ventilation.Ayre’s T - piece
Introduced by Phillips Ayre in 1937.Belongs to Mapleson E .
Available as metallic / plastic .
Length- 2 inches.
Parts – inlet, outlet, side tube.
Inlet size – 10 mm.
Outlet size – 10 mm metalic 15 mm plastic.
Advantages:
Simple to useLightweight
No dead space, no resistance.
For pediatric pts. less than 20Kg.
Expiratory limb is attached to the outlet of T –piece.
- It should accommodate air space equal to 1/3rd of TV.
- If expiratory limb is too long –Rebreathing in spon. breathing pts.
If too short – air dilution in spon. breathing pts & pts becomes light.
1 inch of expiratory tube can accommodate 2-3 ml of gas.
Gas flows – 2-3 times MV
Disadvantes :
High flow rates required.Loss of heat & humidity.
Risk of accidental occlusion of expiratory limb– risk of increased airway pressure & barotrauma to lungs.
Ayre's T-Piece
Efferent reservoir systems
(Mapleson’s D, E and F)Mapleson D
The Mapleson D consists of fresh gas inlet nearer the patient end ,a corrugated rubber tubing one end of which is connected with expiratory valve and then reservoir bag.The system is mainly used with assisted or controlled ventilation.
During assisted or controlled ventilation there is little chance of re - breathing.
The FGF which enters during expiratory pause accumulates in the patient end and is forced during the inflation.
In spontaneous breathing during inspiration the patient will inhale the fresh gas & gas in corrugated tube depending on FGF, TV, length of expiratory pause & volume of corrugated tube.
Re - breathing can be minimized by increasing FGF two to three times the minute volume.
For an adult 15L/min FGF which seems uneconomical is required.
In some cases 250ml/kg/min require to prevent re - breathing.
The system seems to be most efficient for controlled ventilation.
Mapleson D
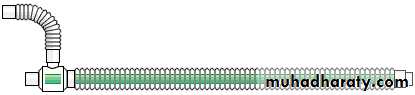
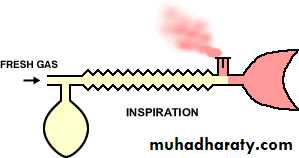
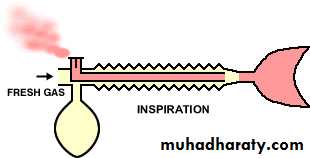
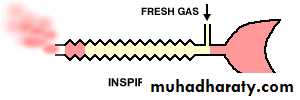
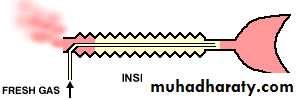
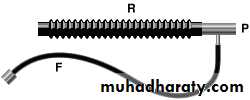
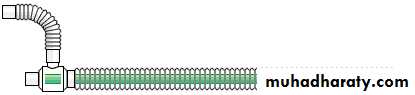
Bain circuitIntroduced by Bain & Spoerel in 1972.
The Bain circuit is a modification of the Mapleson D system.
It is a coaxial system in which the fresh gas flows through a narrow inner tube within the outer corrugated tubing.
Essentially, the Bain circuit functions in the same way as the T-piece, except that the tube supplying fresh gas to the patient is located inside the reservoir tube.
Fresh gases are constantly delivered very close to the patient’s mouth end.
Specifications
Length – 1.8 meters.Diameter of outer tube –22 mm(transparent, carries expiratory gases).
Diameter of inner tube - 7 mm( carries inspiratory gas flows).
Resistance- less than 0.7cm H2O.
Dead space – outer tube up to expiratory valve( around 500ml=TV).
Expiratory valve- called APL valve during controlled ventilation.
Flow rates- 100-150 ml/kg/min for controlled ventilation.
Average 300ml/kg/min for spontaneous ventilation.
Modifications
A bag may be added to the tail of the reservoir tube, as in theT-piece.
Alternatively, the circuit may be attached to a block assembly with a pop-off valve and mounted directly to the common gas outlet of the anaesthesia machine. This arrangement facilitates scavenging and intermittent positive pressure ventilation.
Advantages
Can be used for children and adult-called as Universal circuit.Lightweight,minimal drag on the ETT,helps in various positions & shifting from one position to another with less risk of disconnections,away from the surgical site like head & neck surgeries, in CT scan.
Low dead space.
Low resistance to breathing.
Facilitates scavenging of waste gases.
Automatic warming of fresh gas flow as inner tube is surrounded by expired gases.( providing humidity)
Easily sterilized by Cidex.
Helps controlling pt’s ventilation during transport to RR or ICU.
Disadvantages
High fresh gas flow requirement.As with other co-axial systems, if the inner tube becomes disconnected or breaks, the entire breathing tube becomes dead space, leading to severe alveolar hypoventilation.
Risk of rebreathing mixture of fresh gas & alveolar gas as longer pause is required to drive the alveolar gas out.
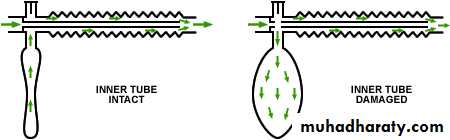
The Pethick Test for the Bain Circuit
A unique hazard of the use of the Bain circuit is occult disconnection or kinking of the inner, fresh gas delivery hose. If this occurs, the entire corrugated limb becomes dead space.
This results in respiratory acidosis which is unresponsive to increased minute ventilation.
To perform the Pethick test, use the following steps:
1. Occlude the patient's end of the circuit (at the elbow).
2. Close the APL valve.3. Fill the circuit, using the oxygen flush valve.
4. Release the occlusion at the elbow and flush.
A Venturi effect flattens the reservoir bag if the inner tube is patent.
Pethick Test
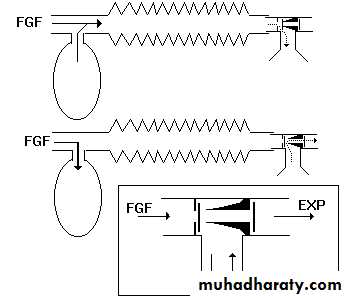
Bain system (Mapleson D)
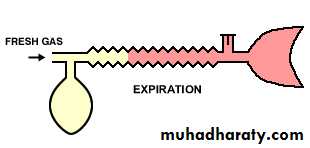
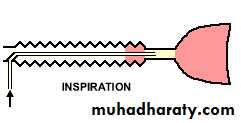
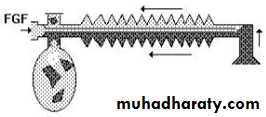
Spontaneous respiration:The breathing system should be filled with FG before connecting to the patient. When the patient takes an inspiration, the FG from the machine, the reservoir bag and the corrugated tube flow to the patient .
During expiration, there is a continuous FGF into the system at the patient end. The expired gas gets continuously mixed with the FG as it flows back into the corrugated tube and the reservoir bag .
FGF
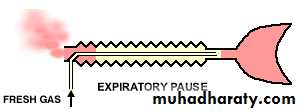
Once the system is full the excess gas is vented to the atmosphere through the valve situated at the end of the corrugated tube near the reservoir bag. During the expiratory pause the FG continues to flow and fill the proximal portion of the corrugated tube while the mixed gas is vented through the valve.
During the next inspiration, the patient breaths FG as well as the mixed gas from the corrugated tube .
Many factors influence the composition of the inspired mixture.
They are FGF, respiratory rate, expiratory pause, tidal volume and CO2 production in the body.Factors other than FGF cannot be manipulated in a spontaneously breathing patient.
It has been mathematically calculated and clinically proved that the FGF should be at least 1.5 to 2 times the patient’s minute ventilation in order to minimize rebreathing .
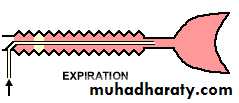
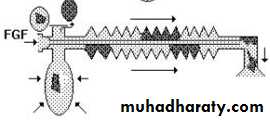
Controlled ventilation
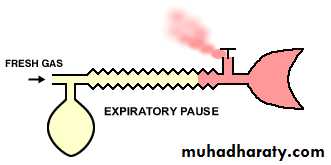
To facilitate intermittent positive pressure ventilation, the expiratory valve has to be partly closed so that it opens only after sufficient pressure has developed in the system. When the system is filled with fresh gas, the patient gets ventilated with the FGF from the machine, the corrugated tube and the reservoir bag .During expiration, the expired gas continuously gets mixed with the fresh gas that is flowing into the system at the patient end. During the expiratory pause the FG continues to enter the system and pushes the mixed gas towards the reservoir .
When the next inspiration is initiated, the patient gets ventilated with the gas in the corrugated tube i.e., a mixture of FG, alveolar gas and dead space gas. As the pressure in the system increases, the expiratory valve opens and the contents of the reservoir bag are discharged into the atmosphere.
Bain ‘s modification of Mapleson D
Mapleson E and F
Valve less breathing system used for children up to 30 kgSuitable for spontaneous and controlled ventilation
Components
T shaped tubing with 3 ports
FGF delivered to one port
2nd port goes to patient
3rd port leads to reservoir tubing
Mapleson F
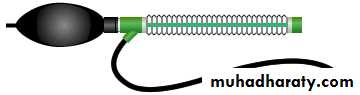
The most commonly used T-piece system is the Jackson-Rees' modification of the Ayre's T-piece (sometimes known as the Mapleson F system). This system connects a two-ended bag to the expiratory limb of the circuit; gas escapes via the `tail' of the bag.It comprise of –
Plastic angle mountPlastic Ayre’s T-piece.
Corrugated rubber hose.
Reservoir bag of 0.5-1L capacity.
Green PVC 1.5 meter long tube with plug that fits into the fresh gas outlet of the Boyle’s apparatus.
Gas flows required – 2-3 times MV.
Dead space – 1ml/lb( 1kg = 2.2lbs.)
Tidal volume – 3 times dead space.
FGF flushes expiratory limb during the pause.
Expiratory limb should be more than TV to prevent air dilution & rebreathing in spon. Breathing child.
This allows respiratory movements to be more easily seen and permits intermittent positive ventilation if necessary. The bag is, however, not essential to the functioning of the circuit.
Intermittent positive pressure ventilation (IPPV) may be performed by occluding the tail of the bag between a finger and thumb and squeezing the bag.
Alternatively, a `bag-tail valve', which employs an adjustable resistance to gas flow, may be attached to the bag tail. This causes the bag to remain partially inflated and so facilitates one-handed performance of IPPV.
Bag-tail valve
Another aid to IPPV is the Kuhn bag, which has the gas outlet on the side of the bag, rather than the tail. This allows the outlet to be occluded with the thumb during IPPV, but leads to difficulties in scavenging the waste gases.Kuhn bag
A number of different designs of T-piece are available, which function in essentially the same way.Modern T-pieces incorporate 15 mm fittings for the reservoir tube and endotracheal adapter.
The volume of the reservoir tubing should approximate the patient's tidal volume. If the volume is too large rebreathing may occur and if too small, ambient air may be entrained.
To prevent rebreathing, the system requires a minimal flow of 4L/min, with a fresh gas flow of 2.5 to 3 times the patient's minute volume.
Advantages
Compact ,lightweight, no drag to ETT.
Inexpensive ,easy to use & sterilize.
No valves
Minimal dead space
Minimal resistance to breathing
Economical for controlled ventilation Disadvantages
The bag may get twisted and impede breathing.
High gas flow requirement .
Lack of humidification.
Uses
Children under 20 kg weight .
Enclosed afferent reservoir system
Mapleson A within a boxEfficient for both SV & IPPV
Complicated
Not often mentioned
Humphrey ADE circuit
Combines the Mapleson A, D & E systems with a switch to select the mode
Efficient in both SV & IPPV
Suitable for both adult & paeds
Increased complexity
The Mapleson A circuit is inefficient for controlled ventilation as is the Mapleson D circuit for spontaneous ventilation.
David Humphrey has designed a single circuit that can be changed from a Mapleson A system to a Mapleson D by moving a lever on the metallic block which connects the circuit to the fresh gas outlet on the anaesthetic machine.
The reservoir bag is situated at the fresh gas inlet end of the circuit, and gas is conducted to and from the patient down the inspiratory and expiratory limbs of the circuit.
BREATHING SYSTEMS WITH CO2 ABSORPTION
Systems so far described have relied on FGF for effective elimination of CO2.Any desire to economize on FGF by allowing a total rebreathing, should be accompanied by removal of the expired CO2 by chemical absorption using soda lime or bara Lyme.
The systems designed for these purpose are again classified as:
Unidirectional flow.
-Circle system.
Bi-directional flow.
-To and fro system.
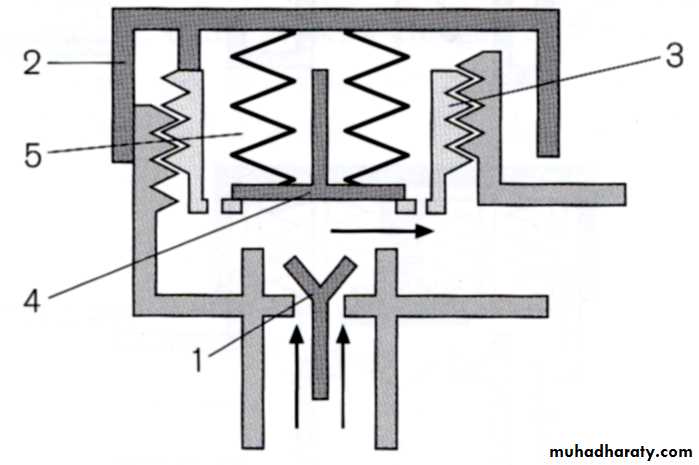
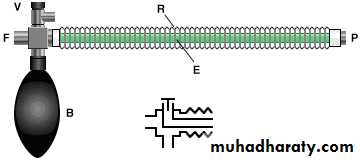
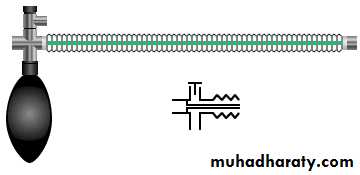
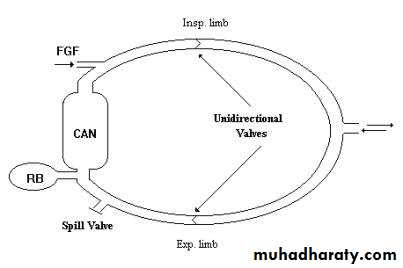
Circle System
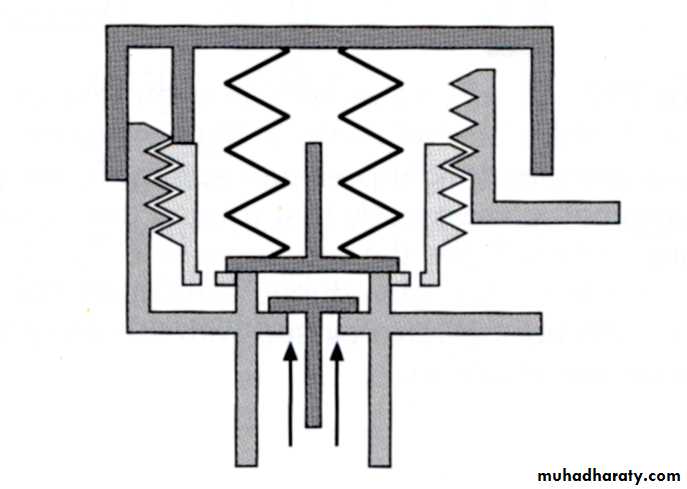
The essential components of the circle system are,
(1) a soda lime canister,
(2) Two unidirectional valves,
(3) Fresh gas entry,
(4) Y-piece to connect to the patient,
(5) Reservoir bag
(6) a relief valve and
(7) low resistance interconnecting tubing.
Components of circle system
For efficient functioning of the system the following criteria should fulfilled.
(1) There should be two unidirectional valves on either side of the reservoir bag,(2) Relief valve should be positioned in the expiratory limb only,
(3) The FGF should enter the system proximal to the inspiratory unidirectional valve.
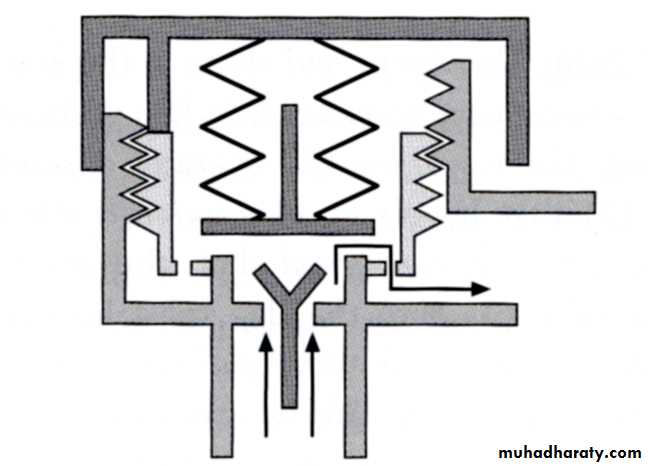
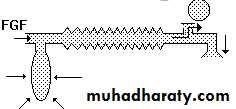
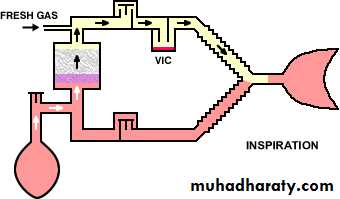
Functional analysis
During inspiration the FG along with the CO2 free gas in the reservoir bag flow through the inspiratory limb and inspiratory unidirectional valve to the patient.No flow takes place in the expiratory limb as the expiratory unidirectional valve is closed by back pressure transmitted to the valve.
During expiration the inspiratory unidirectional valve closes and the expired gas flows through the expiratory unidirectional valve in the expiratory limb to the soda lime canister and to the reservoir bag.
The CO2 is absorbed in the canister. The FGF from the machine continues to fill the reservoir bag. When the reservoir is full the relief valve opens and the excess gas is vented to atmosphere.
By selecting a suitable position for the relief valve, the expired gas can be selectively vented when the FGF is more than the alveolar ventilation.
To facilitate controlled ventilation the relief valve has to be partly closed and the excess gas is vented during inspiration.
Circle System
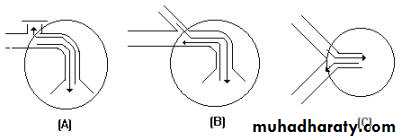
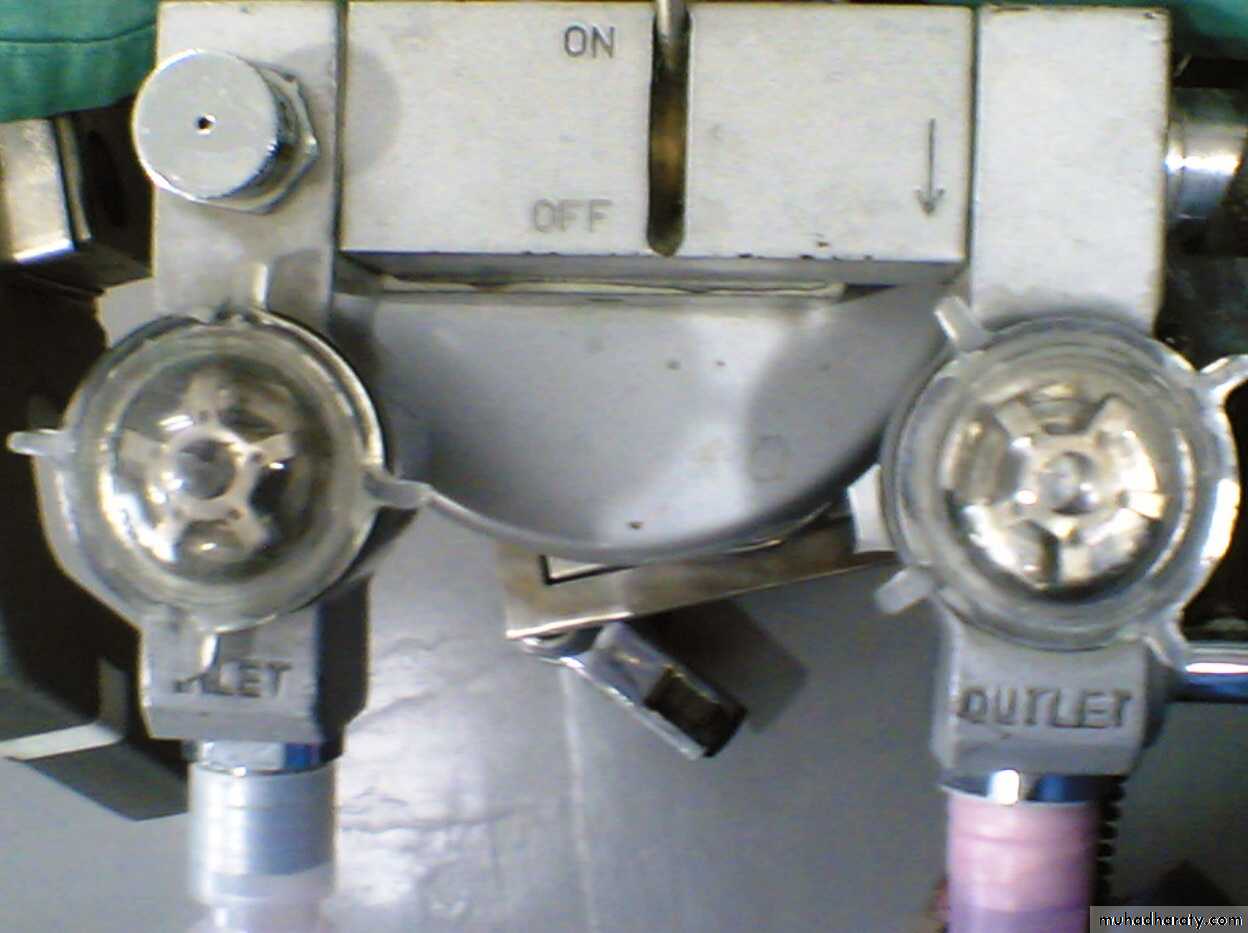
Unidirectional valves
Unidirectional valvesThe unidirectional inspiratory and expiratory valves in most circle absorbers are of the turret type, in which the pressure generated by the patient's breathing causes the disc to rise and allow gas to pass in one direction only. Most have a transparent dome so that the operation of the valve may be observed.
The disc material may be mica, ceramic or plastic. Plastic is less expensive, but tends to warp and allow the valve to become incompetent.
Incompetence may also be caused by the valve sticking in the open position, owing to condensation of water vapour.
Incompetent inspiratory or expiratory valves will reduce the efficiency of gas circulation and result in rebreathing and consequent carbon dioxide retention.
Some machines are equipped with valves made of deformable rubber:
As the rubber ages, these discs tend to harden in a semi-open position, again allowing the valve to become incompetent.Connecting tubing
The body of the absorber is connected to the patient by means of inspiratory and expiratory tubes and a Y-piece. This may be constructed of corrugated black rubber, neoprene or, more recently, plastic.Recently, the so-called Universal F circuit has become popular. This is a co-axial system, the inspiratory tube running inside the expiratory limb:
This arrangement aids warming and humidification of the inspired gases, albeit at the expense of an increase in inspiratory resistance to breathing.
About dead space
Most circle absorbers are satisfactory for use in patients weighing up to around 100 kg.The major problem with using standard circle absorbers in smaller patients is that of dead space.
Patients with very small tidal volumes may not generate enough pressure to open the valves effectively. The effective dead space of the Y-piece is larger than it appears.
Inevitably, some portion of the expired gas is directed down the inspiratory limb of the circuit, and some portion of the inspired gas comes from the expiratory limb, and some mixing of inspired and expired gases occurs.
These difficulties may be reduced by the use of purpose-built infant absorbers, which are smaller than the standard models. Pediatric tubing and Y-pieces, which are simply smaller in diameter than the standard type, may be helpful.
Double-canister absorbers
Many absorbers designed for use employ two canisters placed in series:The top canister is exposed to the expired gases first and removes most of the carbon dioxide.
Any remaining carbon dioxide is then removed by the bottom canister.
When the top canister is exhausted, the absorbent is discarded, the bottom canister is placed in the top position and a canister with fresh absorbent is inserted underneath it.
This arrangement provides optimal efficiency and economy in carbon dioxide absorption. However, these absorbers are bulkier, heavier and more expensive than single-canister models.
Canisters
Sodalime – Brian Sword 1926Barylime.
Sterilization of canister :
Washing with soap water, Immersion in Cidex for 2 hours.
Sodalime
Soda lime is a mixture of chemicals, used in granular form in closed breathing environments, such as general anaesthesia, submarines, rebreathers and recompression chambers, to remove carbon dioxide from breathing gases to prevent CO2 retention and carbon dioxide poisoning.It is made by treating slaked lime with concentrated sodium hydroxide solution.
Sodalime
Chemical componentsThe main components of soda lime are
Calcium hydroxide, Ca(OH)2 (about 75%),
Water, H2O (about 20%),
Sodium hydroxide, NaOH (about 3%), and
Potassium hydroxide, KOH (about 1%).
Chemical composition of absorbents
Sodium/ Potassium:
Small quantities of sodium hydroxide (1.5-5%) are usually added to enhance the reactivity & the hygroscopic property of the mixture. Hence the reason that absorbents are often referred to as ‘soda lime’.
Some manufacturers have added potassium hydroxide for similar reason.
Water content
The optimal moisture content of the absorbent mixture is between 14 – 16 % .This is essential for the chain reactions
Chemical reaction
The overall reaction is:
CO2 + Ca(OH)2 → CaCO3 + H2O + heat (in the presence of water)
The reaction can be considered as a strong base catalyzed, water facilitated reaction.
steps:
1) CO2 + H2O → CO2 (aq) (CO2 dissolves in water - slow and rate determining)2) CO2 (aq) + NaOH → NaHCO3 (bicarbonate formation at high pH)3) NaHCO3 + Ca(OH)2 → CaCO3 + H2O + NaOH (NaOH recycled to step 2) - hence a catalyst)
Each mole of CO2 (44g) reacted produces one mole of water (18g)
The reaction is interesting in that
It produces heat energy ( an exothermic reaction).It changes the pH of the soda lime, which allows the use of indicator dye to show the soda lime is exhausted.
It produces more water than that used up in the reaction.
The exothermic reaction
The heat & water produced by the reaction of soda lime on carbon dioxide is considered beneficial in that they warm & partially humidify the inspiratory gas.
The temperature & humidity of inspired gas is related to a number of factors:
If the FGF is high the dry gas entering the system reduces both the humidity & the temperature.
At low FGFs, the gas circulation time is high, the humidity & the temperature rises.
The longer the system is in use at low FGFs, the greater are the humidity & the temperature of circulating gas.
The heat produced can increase the chemical reaction between volatile anaesthetic agents & absorbents.
Trichloroethylene can be decomposed to dichloroacetylene which is neurotoxic & further to phosgene if temp. exceeds 60°C.
Anaesthetic agents like desflurane, enflurane& isoflurane react with dry, warm soda lime or barium lime to produce carbon monoxide.
Dry barium lime which contains potassium hydroxide has greater tendency to produce CO.
Other constituentsZeolite:
Zeolites are three dimensional, microporous crystalline solids that contains aluminum, silica & oxygen.
They may be added to soda lime to increase:
Porosity of the mixture
Hardness
Water content.
Silica
Small quantities of sodium & potassium hydroxide (1.5-5%) are usually added to enhance the reactivity & the hygroscopic property of the mixture.
However ,they are the main cause of degradation by soda lime of isoflurane, desflurane to CO & sevoflurane to compound A, formaldehyde & methanol.
The granules require the addition of silica ( LoFloSorb) to overcome this.
The new absorbents have been shown to minimize the production of unwanted compounds even when dryCalcium chloride
The addition of 3% calcium chloride (Amsorb Plus) in place of sodium or potassium prevent the formation of CO with isoflurane & desflurane and compound A with sevoflurane.The product also contain 1% calcium sulphate to improve the hardness of the granule.
Indicators for AbsorbentsIndicator Colour when fresh Colour when Exhausted
Phenolphthalein White Pink
Ethyl violet White PurpleClayton yellow Red Yellow
Ethyl orange Orange Yellow
Mimosa Z Red WhiteSo colour change of indicator is one of the sign of exhaustion of sodalime.
Other signs of exhaustion of sodalime,Tachycardia
Hypertension
Increased oozing from wound site
Increased end tidal CO2 on capnography.
Now a days a good quality sodalime with prolonged life ,Durasorb is used which is pink when fresh & white when exhausted.
Hardness of granules should be > 75.
Moisture 14- 19% needed for CO2 absorption.
Size of granules 4 – 8 mesh.
The canister should have 53% of air space.
CO2 absorption is a heat generating process 13,700 calories are produced for 1 mole of CO2 absorbed.
1lb canister lasts for 2 hrs if used continuously.
100 gms of sodalime can absorb 24 to 26 liters of CO2.
Barylime
Composition of Barylime
Ca(OH)2 : 80%
Ba (OH)2 : 20%
It does not require silica.
Barylime is 15% less efficient than sodalime.
Barylime perform well in dry climate.
Indicator – ethyl violet or mimosa Z.
Disadvantage – Chemical skin burn,
- Excessive heat due to exhaustion,
- No regeneration.
Factors affecting CO2 absorption in closed circuit
Freshness of sodalime.Tidal volume of patient.
High flows.
Dead space.
Ill filled sodalime.
Resistance to outflow.
Operational requirements
The volume of the breathing bag must be greater than the patient's inspiratory capacity. This is usually estimated at 30 ml/kg body weight.Since soda lime contains 50% - 70% air around the granules, the volume of the absorber canister should be at least double that of the tidal volume of the patient for optimal efficiency.
Fresh gas flow requirements
Closed systemsIn truly closed systems, the patient consumes oxygen and expires carbon dioxide, which is removed from the system by absorption. The volume of oxygen flowing into the system must, therefore, equal the patient's oxygen consumption.Resting oxygen consumption is approximated by the formula:Oxygen consumption (ml/min) = 10 x BW 0.75.
Body weight (kg) Oxygen consumption (ml /min)
5 3310 56
20 95
40 160
The use of nitrous oxide in closed systems presents the difficulty that, after equilibration, nitrous oxide will accumulate in the circuit and result in a hypoxic breathing mixture. If it is desired to use nitrous oxide in a closed system, it is mandatory to employ an inspired oxygen concentration monitor.
Semi-closed
When using a semi-closed system, the oxygen flow rate must exceed the patient's oxygen consumption. Any excess is simply lost via the pressure relief valve.Initially, it is necessary to use both a high flow rate and high vaporiser setting to raise the concentration of anaesthetic in the circuit. For maintenance, both the vaporizer setting and fresh gas flow rate may be reduced.As a general rule, a flow rate of 2 to 3 liters per minute initially, and 500 ml to 1 liter per minute during maintenance of anaesthesia, will usually prove satisfactory.Advantages of the circle system
Economical.Warming and humidification of the inspired gases.
Reduced atmospheric pollution.
For condition in which there is very high production of CO2 only closed circuit can eliminate such high CO2.(malignant hyperthermia).
Disadvantages
Heavy weight circuits.Chances of accidental exudation & disconnections are high.
If sodalime is exhausted can produce dangerous hypercarbia.
Cross infection from apparatus.
Breathing resistance & dead space high.
Some inhalational agents can produce toxic products when used with sodalime.
Apparatus dead space ( closed Circuit)
3 corrugated tubes – 1000 ml.
Canister (Intergranular space) – 500 ml.
Reservoir bag – 1500 ml.
Anatomical dead space – 150 ml.
LOW FLOW ANESTHESIA
LOW FLOW ANESTHESIALOW FLOW ANESTHESIA
LOW FLOW ANESTHESIALOW FLOW ANESTHESIA
LOW FLOW ANESTHESIALOW FLOW ANESTHESIA
LOW FLOW ANESTHESIALOW FLOW ANESTHESIA
LOW FLOW ANESTHESIA
Why Low Flow ?
Low wasteLow expense
Safe
Effective
Planet-friendly
Warm patient
Moist CO2 absorbent
A FEW DEFINITIONS
Low Flow Anesthesia (LFA) has been variously defined as an inhalation technique in which a circle system with absorbent is used with a fresh gas inflow of :- less than the patient’s alveolar minute volume
- less than 1-1.5 l/min
- 3 l/min or less
- 0.5 – 2 l/min
- less than 4 l/min
- 500 – 1000 ml/min
Closed System Anesthesia is a form of LFA in which the FGF = uptake of anesthetic gases and oxygen by the patient and gas sampling.
No gas is vented by the APL valve.
Dorsch and Dorsch
Understanding Anesthesia EquipmentDefinition of low-flow
Metabolic flow = 250ml/min Minimal flow = 250-500 ml/min Low flow = 500-1000 ml/min Medium flow = 1-2 L/min High flow = 2-4 L/min Super-high flow = >4 L/minLow-flow anesthesia can be defined as a technique which, using a rebreathing system, results in at least 50% of the exhaled air being returned to the lungs after CO2 absorption.
(Low-flow anaesthesia, Anaesthesia, 1995, Volume 50 (supplement), pages 37-44)
THE REBREATHING SYSTEMSREBREATHING describes a technique in which non-consumed gases, contained in the exhaled air are partially or completely re-routed back to the patient during the following inspiration, purified from CO2 AND admixed with a certain amount of fresh gas.
Basic concepts
The recognition of the functional residual capacity as dead space or extension of the circuit.The recognition of the alveolar membrane as a barrier of anesthetic uptake.
Via the observation that anaesthetic vapours are excreted unchanged with the expired air and serial experiments, John Snow concluded In 1850 that:
“ It follows as a necessary consequence of this mode of excretion of a vapour that, if its exhalation by the breath could in any way be stopped, its narcotic effects ought to be much prolonged.”
TECHNICAL ASPECTS
In LFA there are a few technical requirements.
1. Circle rebreathing system with CO2 absorption.
2. Accurate flow meters for adjustments of FGF below 1L/min.3. Gas tight breathing system.
4. Ascending bellows.
5. Continuous gas monitoring MUST be employed. From the clinical standpoint the measurement of expiratory gas concentrations close to the Y-piece is of crucial importance. That information is essential in controlling the patient’s alveolar gas concentrations.
ADVANTAGES OF THE LFA
1. QUALITY OF PATIENT CARE2.2.ECONOMIC BENEFITS
Over 80% of anesthetic gases are wasted when flows of 5L/min are used.
3. ENVIRONMENTAL BENEFITS
THE OTHER SIDE OF THE COIN
Disadvantages of LFA:1.Limitations of currently used vaporizers.
2.Accumulation of unwanted gases into the breathing system:HOW TO ADJUST FGF AT DIFFERENT PHASES OF LFA
Premedication, pre-oxygenation and induction of sleep are performed according to the usual practice. Concerning adjustment of FGF anesthesia can be divided into 3 phases:1. Initial HIGH flow
2. Low flow
3. Recovery
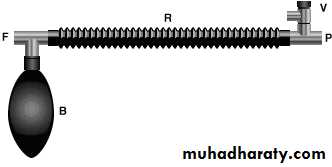
Water’s Canister
To-and-fro system. By Prof. Ralph Water 1922.Since gases travel through canister during controlled ventilation and return through canister to reservoir bag, it is called to & fro canister.
Mapleson C with a soda lime metallic canister between the APL valve and the reservoir.
Cylindrical in shape, handy, can be autoclaved.
Size – 8 by 12cm, holds 1 kg sodalime.Has 2 buffer porous plates to hold sodalime.
Intergranular space = Tidal volume.
Resistance – 2.5 – 3 cm H2O.
Not currently widely used
Advantage:
Efficient for 1-2 hrs for controlled ventilation.
Easy sterilization by autoclaving ; can be used for infected pts like pulm. TB.
Handy , easy to carry.
Disadvantages:
Non transparent(metallic).
Very close to pt’s respiratory tract – Risk of dust reaching the pt. Risk of inhaling soda lime
It becomes warm with heat generated during chemical reaction.
It needs frequent changing.
Channeling , caking of sodalime.
Increasing dead space as granules near the patient are exhausted first
Water’s Canister
Nonrebreathing systemsThey use non rebreathing valves and there is no mixing of fresh gas and the expired gas.
The fresh gas flow (FGF) should be equal to the minute ventilation (MV) of the patient.
These systems satisfy all essential requirements, but are not very popular because of the following reasons:
1) Fresh gas flow has to be constantly adjusted and is not economical.
2) There is no humidification of inspired gas.
3) There is no conservation of heat.
4) They are not convenient as the bulk of the valve has to be positioned near the patient.
5) The valves can malfunction due to condensation of moisture and lead to complications.
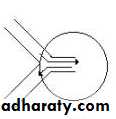
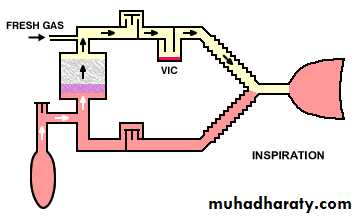
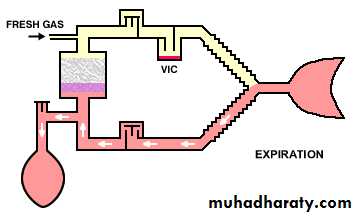
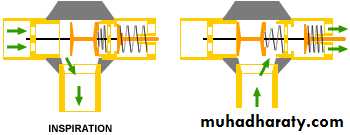
Functional analysis
When the patient takes a breath, or if the reservoir bag is squeezed, the inspiratory unidirectional valve opens and the gases flow into the patient’s lungs .
The expiratory unidirectional valve closes the expiratory port during spontaneous breathing.
The inspiratory unidirectional valve itself closes the expiratory port during controlled ventilation.
At the start of expiration, the inspiratory unidirectional valve returns back to position and expiration takes place through the expiratory port, opening the expiratory valve.
Nonrebreathing system
Non rebreathing valves
Ruben Non-Rebreathing Valve & Ambu E2 Valve
Ruben Non-Rebreathing ValveLight transparent piece .
Has a clear plastic body with metal fitting.
One end to the patient, other end to the gas supply & perforated end to void the exhalations to the atmosphere.
It works on a bobbin which moves against the tension of a light spring.
Dead space- 9ml.
Resistance to gas flow- 0.8cmH2O during inspiration &1 cmH2O during expiration when flow rate is 25 L/min.
Can be used for spontaneous & controlled ventilation.
The valve should not be sterilized by heating as made up of plastic material.
Can be effectively sterilized by soaking with 5% chlorhexidine in water for 5 min.
Ruben Non-Rebreathing Valve
Ambu Non-rebreathing Valve
Has two silicone rubber flaps instead of a bobbin.Can be easily dismantled, cleaned & autoclaved or gas sterilized.
Can be used for spontaneous & controlled ventilation.
Three types – Ambu E
Ambu Hesse
Ambu E2.
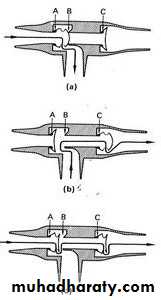
Ambu E
Ambu E valve has got dead space of 10 ml.Resistance to gas flow ranges from 0.6 to 2.1 cm of H2O in inspiration & 0.6 to 2.5 cm of H2O in expiration with a flow rate 5 to 40 L/min.
In Ambu E the fresh gas pass through first nonreturn valve which opens during inspiration.
During expiration first valve closes & second valve opens to allow the expired gases to void in the atmosphere.During inspiration the second valve remains closed so that air from outside cannot enter.
During expiratory pause excess gases pass outside as both valves open partially. This prevents excessive build up of pressure.
During inspiration
During expiration
During expiratory pause
Ambu Hesse
Ambu Hesse was founded in 1937 in Denmark by engineer Dr. Holger Hesse, Ph.D.Ambu Hesse valve is of low resistance to gas flow only 0.4 cm of H2O during inspiration & 0.6 cm of H2O during expiration with flow rate of 25 L/min.
Dead space – 14 ml.
More suitable valve to use with EMO apparatus.
Ambu E2 valve
The Ambu E2 valve differs from the Ambu E valve in having no expiration shutter, thus in spontaneous respiration air is drawn in from the expiratory side.In controlled ventilation only fresh gases are passed to the patient due to closure of exhalation port.