Multiple pregnancy
DefinitionsIn general terms, multiple pregnancies consist of two or more fetuses.
There are rare exceptions to this,such as twin gestations made up of a singleton viable fetus and a complete mole.
Twins
‘higher multiples
Prevalence
Risk factors for multiple gestations include assisted reproduction techniques (both ovulation induction and in vitro fertilization (IVF)), increasing maternal age,high parity,
black race and
maternal family
Traditionally, the expected incidence was
calculated using Hellin’s rule. Using this rule, twins were expected in 1 in 80 pregnancies, triplets in 1 in 802 and so on..
Classification
based on:• number of fetuses: twins, triplets,
quadruplets, etc.
• number of fertilized eggs: zygosity
• number of placentae: chorionicity
• number of amniotic cavities: amnionicity.
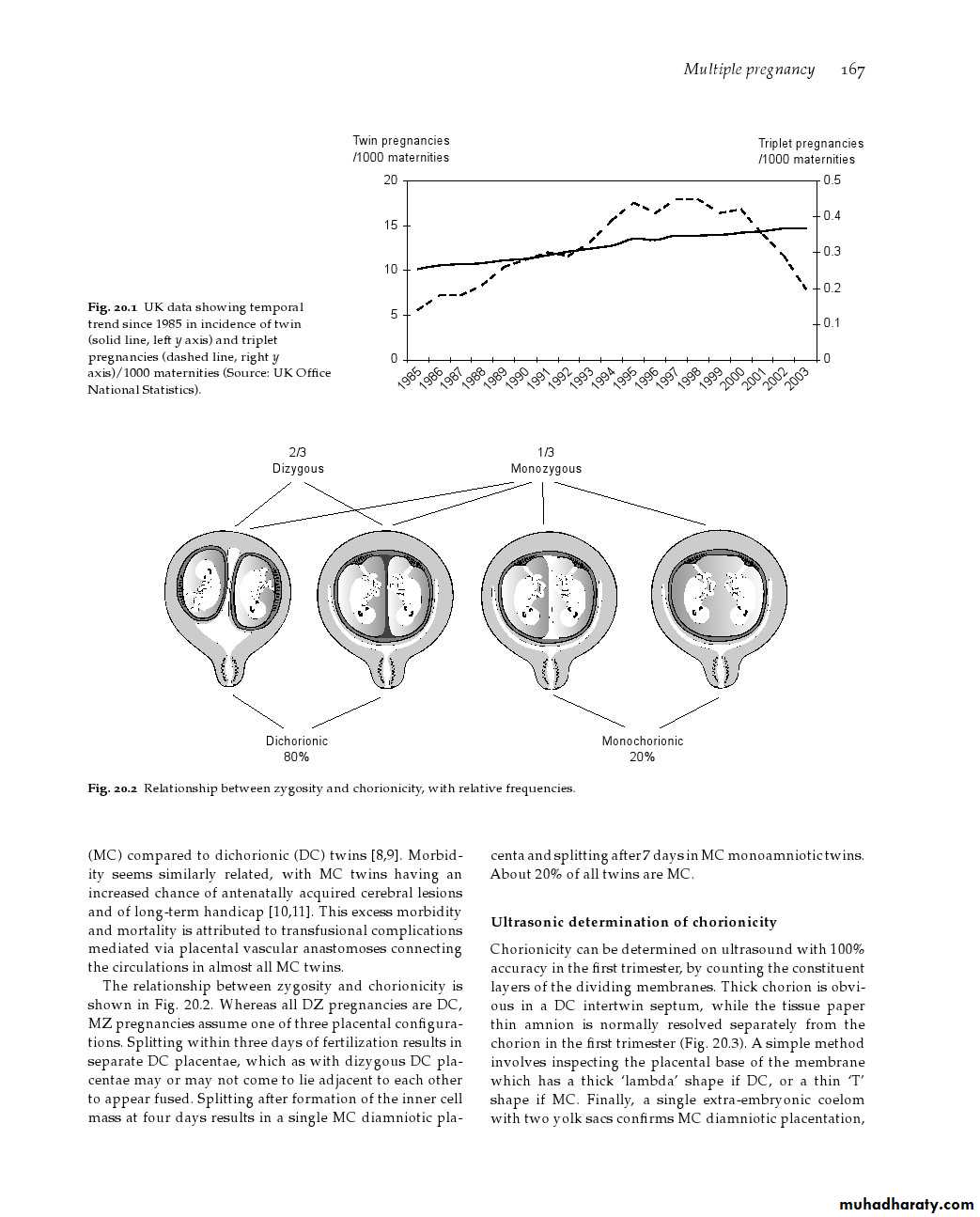
Monozygotic twins arise from a single fertilized
ovum that splits into two identical structures. The
type of monozygotic twin depends on how long
after conception the split occurs. When the split
occurs within 3 days of conception, two placentae
and two amniotic cavities result, giving rise to a
dichorionic diamniotic (DCDA) pregnancy. When
splitting occurs between days 4 and 8, only the
chorion has differentiated and a monochorionic
diamniotic (MCDA) pregnancy results.
Later splitting after the amnion has differentiated leads to both twins developing in a single amniotic cavity, a monochromic monoamniotic (MCMA) pregnancy.
If splitting is delayed beyond day 12, the embryonic disc has also formed, and conjoined, or ‘Siamese’twins will result.
The incidence of monozygotic or identical twins
is generally accepted to be constant at 1 in 250. It is not influenced by race, family history or parity.
What is the type of multiple gestation in following
1- twin one is boy the other is girl2-tiwn of different sex with 2 placentae
3-tiwn of different sex with 2 placentae and 2 amniotic membranes
4-indentical twins with 2amniotic membrnes 1 placenta
5-2 female fetuses with 1 placenta and 1amniotic membrane
Complications relevant to twinpregnancy
1)Miscarriage and severe preterm deliveryHalf of all twins deliver preterm
2)Perinatal mortality in twins
The overall infant mortality rate for twins is around 5.5 times higher than for singletons.
Complication
Singleton (%) Dichorionic (%) Monochorionic (%)Miscarriage at 12–23 weeks 1 2 12
Delivery at 24–32 weeks 15 25
Small for gestation 10 25 50
Fetal defects 1 2 4
Increased perinatal mortalityIt may be due to
preterm delivery IUGR
operative manipulation: Birth trauma
congenital malformation.
4.Increased low body weight:
5.monochorionic complication6.monoamniotic complication
4)-Death of one fetus in a twin pregnancy
early demise and subsequently ‘vanish’After the first trimester, the intrauterine death of one fetus in a twin pregnancy may be associated with a poor outcome for the remaining co-twin. Maternal complications such as disseminated intravascular coagulation have been reported, but the incidence is very low
5)Fetal abnormalities
Compared to singletons, twin pregnancies carry at least twice the risk of the birth of a baby with an anomaly.Complications unique to monochorionic twinning
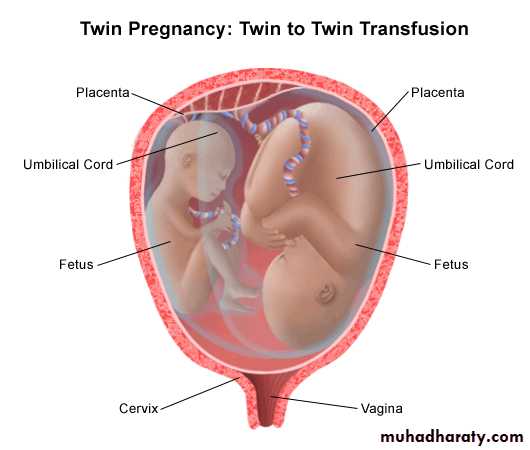
In all monochorionic twin pregnancies there are
placental vascular
In approximately 15 per cent of , imbalance
in the flow of blood across these arteriovenous
communications results in twin-to-twin transfusion
syndrome (TTTS). One fetus becomes overperfused
and the other underperfused. The development of
mild, moderate or severe TTTS depends on the degree
of imbalance. The growth-restricted donor fetus
suffers from hypovolaemia and becomes oliguric. As
fetal urine is the major component of amniotic fl uid,
this fetus develops oligohydramnios
. The recipient fetus becomes hypervolaemic, leading to polyuria and polyhydramnios. There is also a risk of myocardialdamage and high output cardiac failure. Severe disease may become apparent in the second trimester.
The mother often complains of a sudden increase in abdominal girth associated with extreme discomfort.
Twin to Twin transfusion
treatment
The long-standing method of treatment has been
amniocentesis every 1–2 weeks.
fetoscopically guided laser
coagulation to disrupt the placental blood vessels
that connect the circulations of the two fetuses
Complications unique to monoamniotic twinning
increased risk of cord accidents and cord entanglement. Many clinicians advocate electivedelivery by Caesarean section at 32–34 weeks
gestation, as this complication is usually acute, fatal and unpredictable.
Maternal Response/Complications
1-Increased maternal mortality.2-Increased pregnancy risks:
1Anemia (15%): due to iron deficiency or folic acid deficiency
2Preeclampsia- eclampsia:
3Glucose intolerance.
4Threatened or actual abortion.
5Polyhydramnios (12%): acute: more in monozygotic than dizygotic twins. or chronic: not related to type
6Mechanical effects:.
7Rupture of membranes
8Antepartum hemorrhage.
9P0st partum hemorrhage.
10Psychological:
3-Increased labor risks
Preterm labor (50%): which may be spontaneous or inducedAbnormal fetal presentation.
Twins entanglement and locked twins
Cord prolapse
Postpartum Hemorrhage
Puerperal Sepsis
Antenatal management
1Determination of chorionicity2Dtection of chromosomal abnormalities
Both amniocentesis and chorion villus sampling
(CVS) can be performed in twin regnancies, but in dichorionic pregnancies, it is essential that both fetuses are sampled.
3 monitoring for fetal growth
It is reasonable to plan 4- to 6-weekly ultrasound scans in uncomplicated dichorionic twins.Fortnightly ultrasound is appropriate in monochorionic pregnancies.
4-Threatened preterm labour
As in singleton pregnancies, neither bed rest norprophylactic administration of tocolytics is useful in
preventing preterm delivery. Despite this, screening
for preterm birth may be worthwhile.
maternal steroid therapy to enhance fetal lung
maturation,
supplementary education as to the signs
and symptoms of preterm labour, advance planning
regarding intrapartum care,
screening for group Bstreptococcus (GBS) (intrapartum antibiotics reduce neonatal infection)
transvaginal cervical ultrasound shows
the most promise as a predictor of very preterm
delivery
Intrapartum management
Complications in labour are more common with twin gestations.
These include premature birth,abnormal presentations,
prolapsed cord,
premature separation of the placenta and postpartum haemorrhage.
It may require considerable expertise and is
the only situation in which internal podalic version is still practised in obstetrics.Preparation
This should begin long before labour, with antenatal education . A twin CTGmachine should be used for fetal monitoring and aportable ultrasound machine should be available. A standard oxytocin solution
for augmentation should be prepared, run through an intravenous giving-set and clearly labelled ‘for augmentation’, for use for delivery of the second twin,if required. postpartum haemorrhage.
A second high-dose oxytocin infusion should also be available for the management ofpostpartum hemorrhage keep this separate, not run through a giving-set until
needed and clearly labelled ‘for postpartum use only’.It is essential that two neonatal resuscitation trolleys,two obstetricians and two paediatricians are available and that the special care baby unit and anaesthetist are
informed well in advance of the delivery.
Analgesia during labour
Epidural analgesia is recommended. Indeed, if the presentation of twins is anything other than vertex–vertex, the use of an epidural can be justifi ed in terms of analgesia for possible intrauterine manipulationsrequired in the second stage for delivery of the second twin.
Fetal well-being in labour
Fetal heart rate monitoring should be continuous throughout labour, ideally using a specialized twin monitor.
The condition of the second twin must be carefully monitored after the delivery of the first twin, as acute complications suchas
cord prolapse and
placental separation
Vaginal delivery of vertex–vertex
Although this combination is considered low risk,an obstetrician should be present. Deliveryof the first twin is undertaken in the usual manner and thereafter the majority of second twins will be
delivered within 15 minutes. After the delivery of the first twin, abdominal palpation should be performed to assess the lie of the second twin.
If contractions do not ensue within 5–10 minutes after delivery of the first twin, an oxytocin infusion should be started
Delivery of vertex–non-vertex
If the second twin is a breech, the membranes canbe ruptured once the breech is fixed in the birth canal.
A total breech extraction may be performed if fetal
distress occurs or if a footling breech is encountered,
but this requires considerable expertise.
Non-vertex first twin
When the first twin presents as a breech, cliniciansusually recommend delivery by elective Caesarean
section. This is largely because of the increased risks
associated with singleton breech vaginal delivery. Other factors include decreased experience of breech delivery
and the rarely seen phenomenon of ‘locked twins’.
Higher multiples
A consequence of the widespread introduction of assisted reproductive techniques has been an l increase in the incidence of higher multiple gestations mostly triplets.At least 75 per cent of triplet pregnancies are secondary to assisted conception. They are associated with increased risks of miscarriage, perinatal death and handicap. The median gestational age at birth is 33 weeks
In an attempt to reduce the morbidity and mortality associated with extremely preterm delivery, the procedure of multi-fetal reduction was
introduced. Iatrogenic fetal death is achieved by
the ultrasound-guided puncture of the fetal heart
and injection of potassium chloride. Although it
is technically feasible to perform reduction from
as early as 7 weeks gestation, it is usually delayed
until around 11–12 weeks
Higher multiple
25 per cent risk of extremely preterm deliverybetween 24 and 32 weeks. After multi-fetal reduction,usually to twins, the risk of loss before viability is increased to 8 per cent. However, the chance of a very preterm birth drops to 10 per cent.
Key points
• Twins account for about 1.5 per cent of pregnancies but
up to 25 per cent of special care baby unit admissions.
• Perinatal mortality rate in twins is nearly six times
higher than in singletons, primarily due to spontaneous
preterm births.
• Both serious maternal complications and minor
discomforts are increased in multiple gestation.
• The determination of chorionicity is very important – the
highest risks are seen in monochorionic twins