THORAX
Dr.Luma Ibrahim Al-AllafTHORACIC CAVITY
Mediastinum
mediastinum.
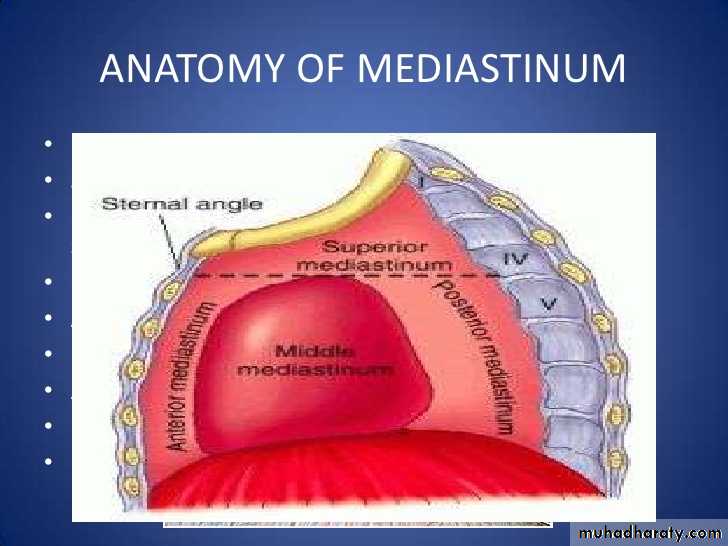
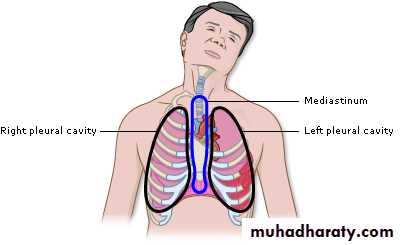
The mediastinum
• lies between the right and left pleuræ in and near the median sagittal plane of the chest.
• It extends from the sternum in front to the vertebral column behind, and contains all the thoracic viscera excepting the lungs.
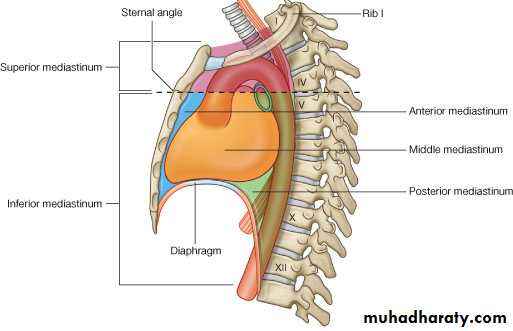
• It may be divided for purposes of description into two parts: an upper portion, above the upper level of the pericardium, which is named the superior mediastinum; and a lower portion, below the upper level of the pericardium.
• This lower portion is again subdivided into three parts, viz., that in front of the pericardium, the anterior mediastinum; that containing the pericardium and its contents, the middle mediastinum; and that behind the pericardium, the posterior mediastinum.
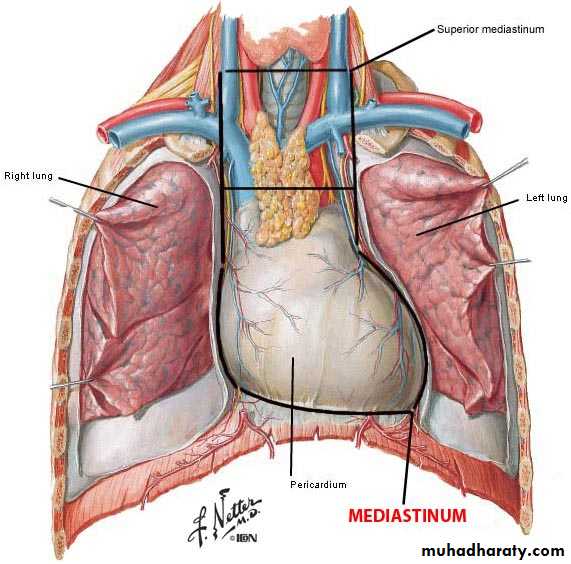
The Superior Mediastinum
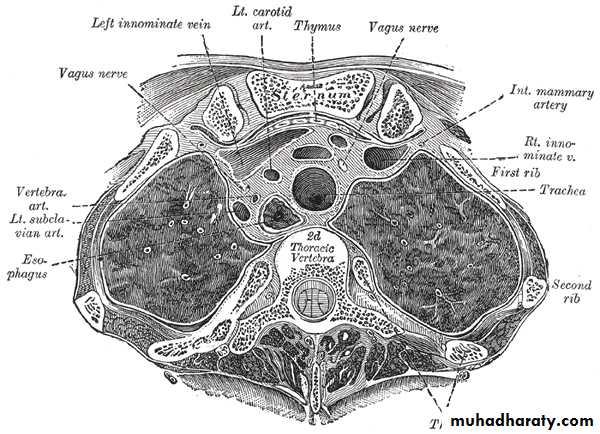
• is that portion of the interpleural space which lies between the manubrium sterni in front, and the upper thoracic vertebræ behind.• It is bounded below by a slightly oblique plane passing backward from the junction of the manubrium and body of the sternum to the lower part of the body of the fourth thoracic vertebra, and laterally by the pleuræ.
mediastinum.
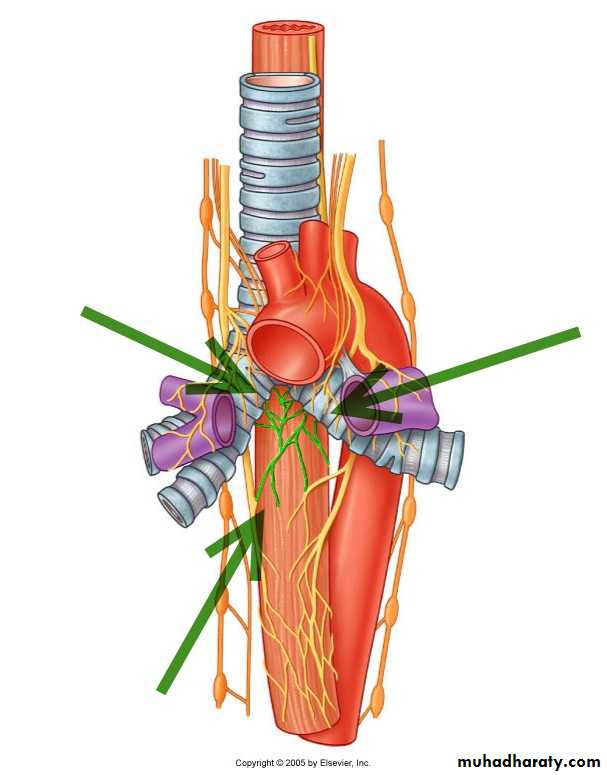
Contents of Superior mediastinum
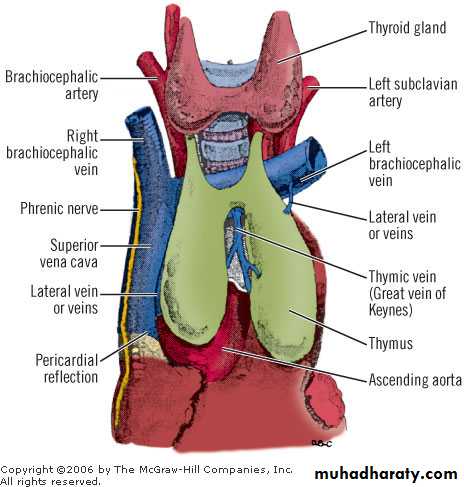
From anterior to posterior:• It contains the origins of the Sternohyoidei and Sternothyr; Thymus.
• Large veins(the brachiocephalic veins and the upper half of the superior vena cava; the left highest intercostal vein).• Large arteries.(the aortic arch; the brachiocephalic artery and the thoracic portions of the left common carotid and the left subclavian arteries)
• Trachea, the vagus, cardiac, phrenic, and left recurrent nerves
• Esophagus and thoracic duct.
• Sympathetic trunks .
• some lymph glands
Superior mediastinum
mediastinum.
Inferior mediastinum
From anterior to posterior:• Thymus.
• Heart within pericardium with phrenic n. on each side.• Esophagus and thoracic duct.
• Descending aorta.
• Sympathetic trunks.
Inferior mediastinum
The Anterior Mediastinum
• exists only on the left side where the left pleura diverges from the mid-sternal line.• It is bounded in front by the sternum, laterally by the pleuræ, and behind by the pericardium.
• It is narrow, above, but widens out a little below.
• Its anterior wall is formed by the left Transversus thoracis and the fifth, sixth, and seventh left costal cartilages. It contains a quantity of loose areolar tissue, some lymphatic vessels which ascend from the convex surface of the liver, two or three anterior mediastinal lymph glands, and the small mediastinal branches of the internal mammary artery(internal thoracic artery).
Anterior mediastinum.
mediastinum.
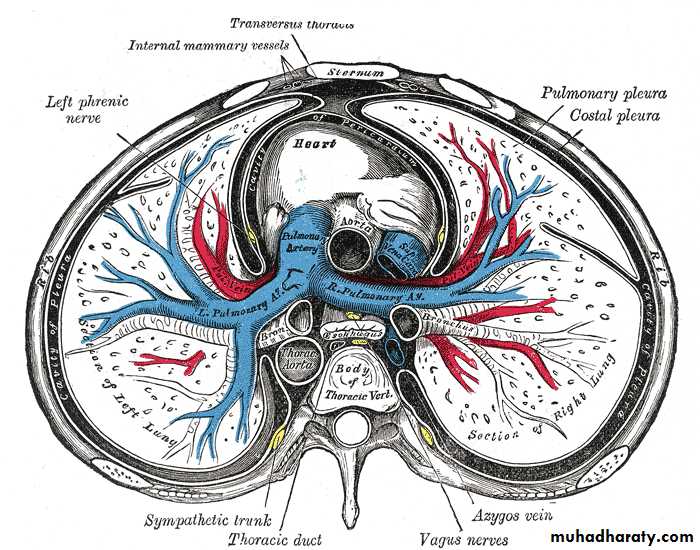
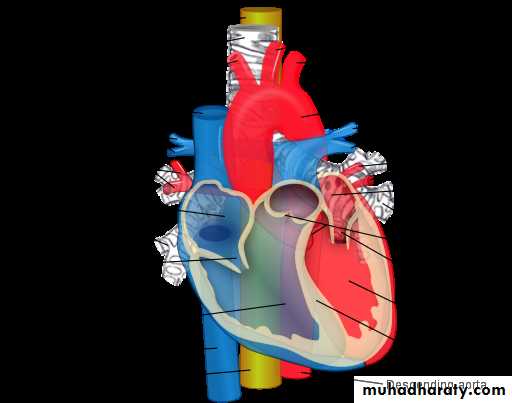
The Middle Mediastinum
• is the broadest part of the interpleural space. It contains :• Heart enclosed in the pericardium,
• Ascending aorta,
• Lower half of the superior vena cava with the azygos vein opening into it,
• Bifurcation of the trachea and the two bronchi,
• Pulmonary artery dividing into its two branches, the right and left pulmonary veins,
• Phrenic nerves,
• and some bronchial lymph glands.
A transverse section of the thorax, showing the contents of the middle and the posterior mediastinum. The pleural and pericardial cavities are exaggerated since normally there is no space between parietal and visceral pleura and between pericardium and heart.
The Posterior Mediastinum
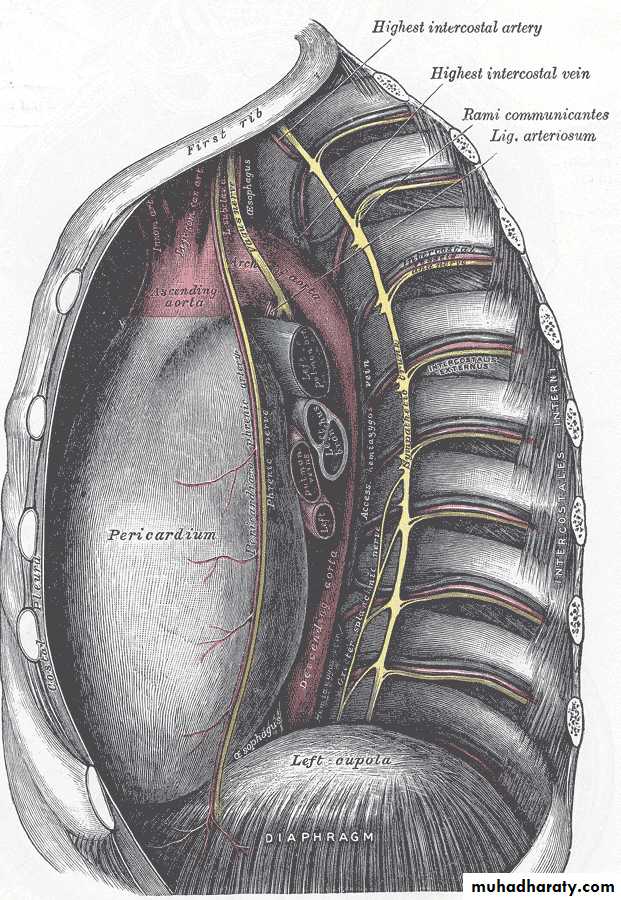
• is an irregular triangular space running parallel with the vertebral column; it is bounded in front by the pericardium above, and by the posterior surface of the diaphragm below, behind by the vertebral column from the lower border of the fourth to the twelfth thoracic vertebra, and on either side by the mediastinal pleura.Contents
• It contains :• the thoracic part of the descending aorta,
• the azygos and the two hemiazygos veins,
• the vagus and splanchnic nerves,
• the esophagus,
• the thoracic duct,
• and some lymph glands.
Thymus
Thymus
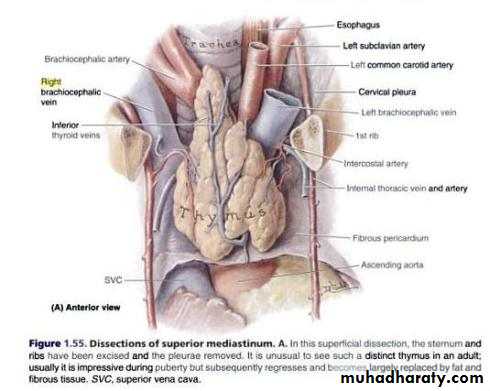
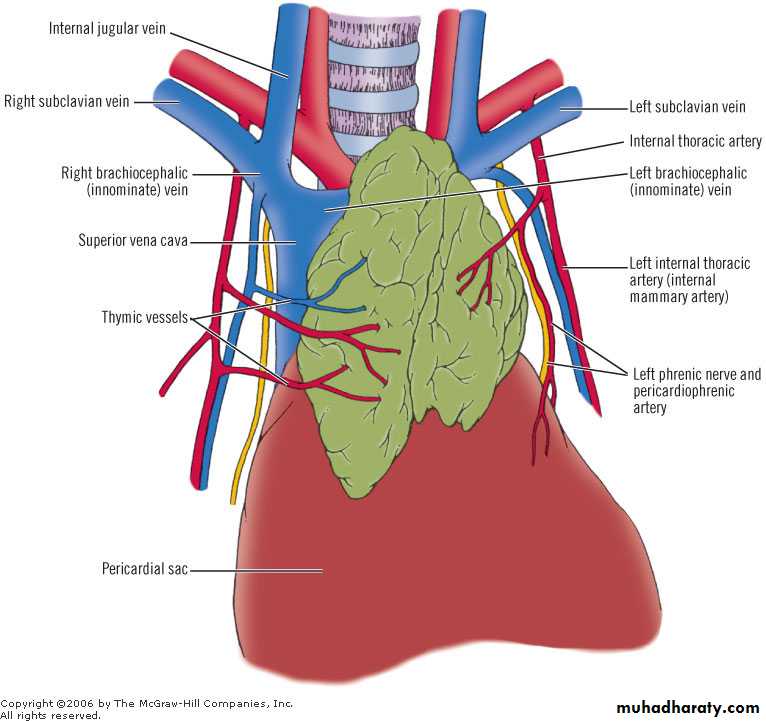
The thymus may appear to be a single organ, but in fact it consists of right and left lobes closely applied to each other for much of their extent.
It is usually most prominent in children, where it may be expected to extend from the level of the fourth costal cartilages to the lower poles of the thyroid gland.
• In front of it lie the pretracheal fascia, the sternohyoid and sternothyroid muscles, the manubrium and upper part of the body of the sternum and their adjacent costal cartilages.
• Behind it are the pericardium, the arch of the aorta with its three large branches (brachiocephalic, left common carotid and left subclavian), the left brachiocephalic vein and the trachea
Blood supply
• Blood supply of thymus:
• Small branches enter the thymus from the inferior thyroid and internal thoracic arteries, and there are corresponding veins.• Frequently a rather large thymic vein formed by tributaries from both lobes enters the left brachiocephalic vein.
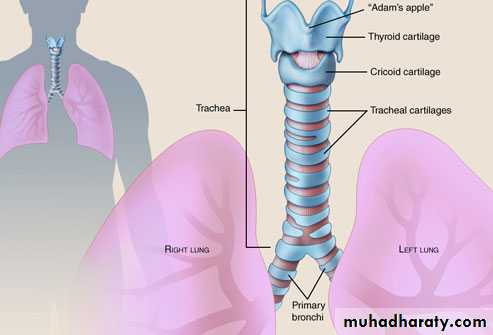
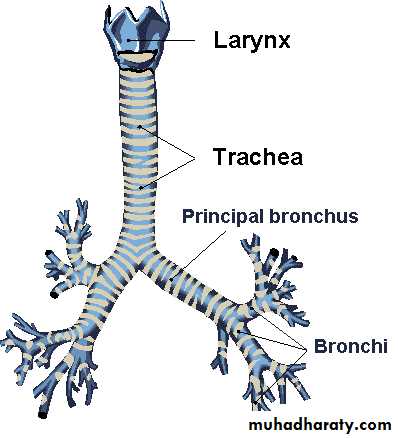
Trachea
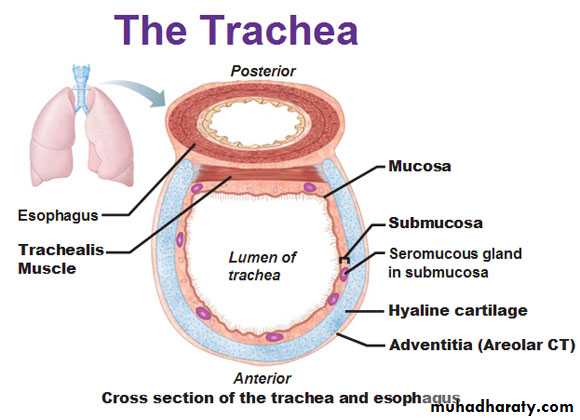
• The trachea is nearly but not quite cylindrical, flattened posteriorly.
• In cross-section, it is D-shaped, with incomplete cartilaginous rings anteriorly and laterally, and a straight membranous wall posteriorly.• The trachea measures about 11 cm in length and is chondromembranous.
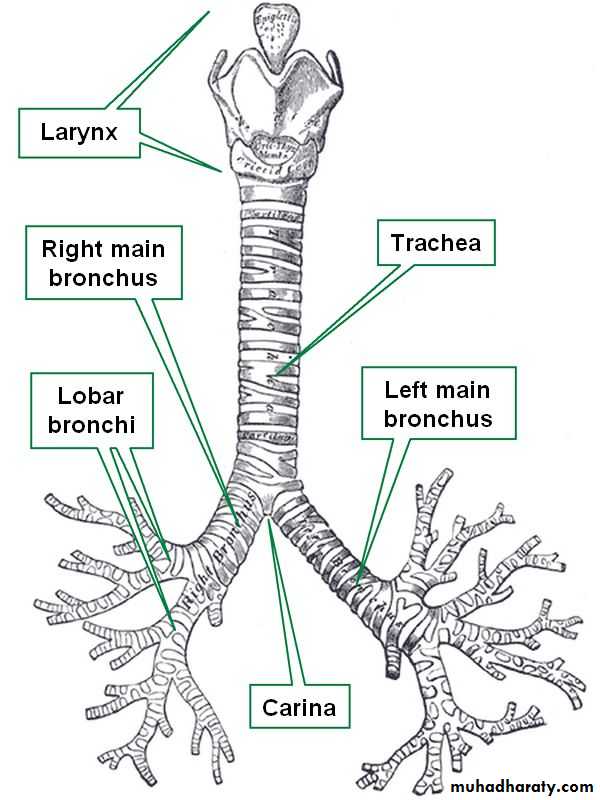
• This structure starts from the inferior part of the larynx (cricoid cartilage) in the neck, opposite the 6th cervical vertebra, to the intervertebral disc between T4-5 vertebrae in the thorax, where it divides at the carina into the right and left bronchi.
Trachealis m.
Carina.
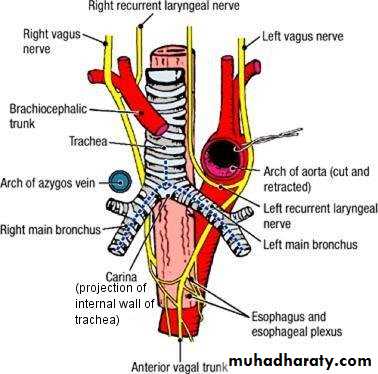
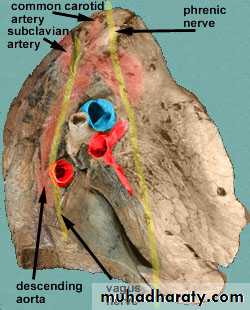
Relations of trachea
Ant.: sternum, thymus, left brachiocephalic v., origins of brachiocephalic & left common carotid arteries, arch of aorta.Pos.: esophagus, left recurrent laryngeal n.
Relations of trachea
Right side: azygos v., right vagus n., pleura.
Left side: arch of aorta, left common carotid & left subclavian arteries, left vagus & left phrenic nerves, pleura.Nerve supply of trachea
Neurovascular supply of the trachea
• Arterial supply• The lateral parts of the trachea and esophagus are supplied via longitudinal vascular anastomoses of interconnected branches along the lateral surface of the trachea from the following arteries :
• Inferior thyroid artery
• Subclavian artery
• Supreme intercostal artery
• Internal thoracic artery
• Brachiocephalic trunk
• Bronchial arteries at the tracheal bifurcation
Venous and lymphatic drainage
• Small tracheal veins join the laryngeal vein or empty directly into the left inferior thyroid vein.
• Left and right descending veins enter the respective brachiocephalic veins.
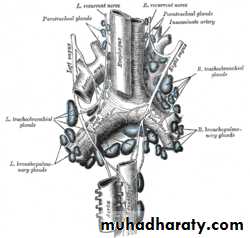
• The tracheal lymphatics drain to the pretracheal, paratracheal, and tracheobronchial groups of lymph nodes.
Nerve supply
• The muscle fibers of the trachea are innervated by the recurrent laryngeal nerve, which also carry sensory fibers from the mucous membrane.• Sympathetic nerve fibers are derived mainly from the middle cervical ganglion and have connections with the recurrent laryngeal nerves.
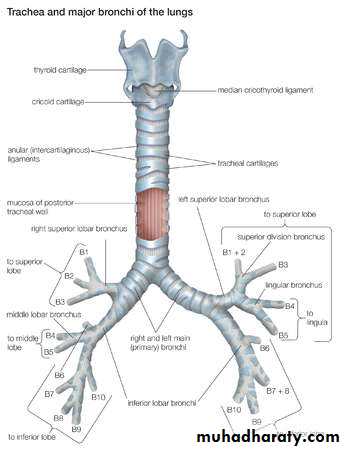
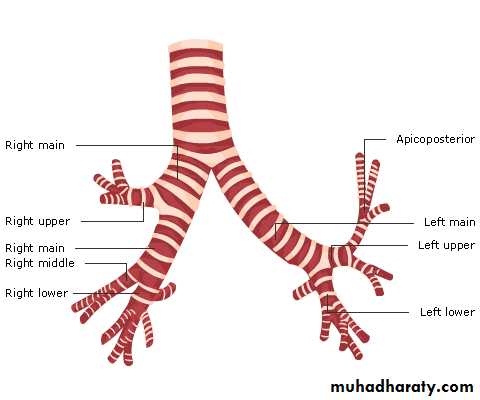
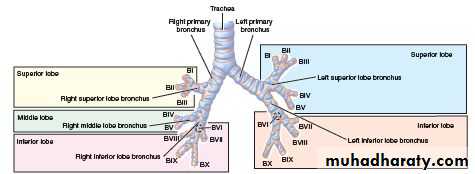
Principal bronchi
The right principal bronchus gives off:
Superior lobar bronchus.Middle lobar bronchus.
Inferior lobar bronchus.The left principal bronchus passes in front of the esophagus.
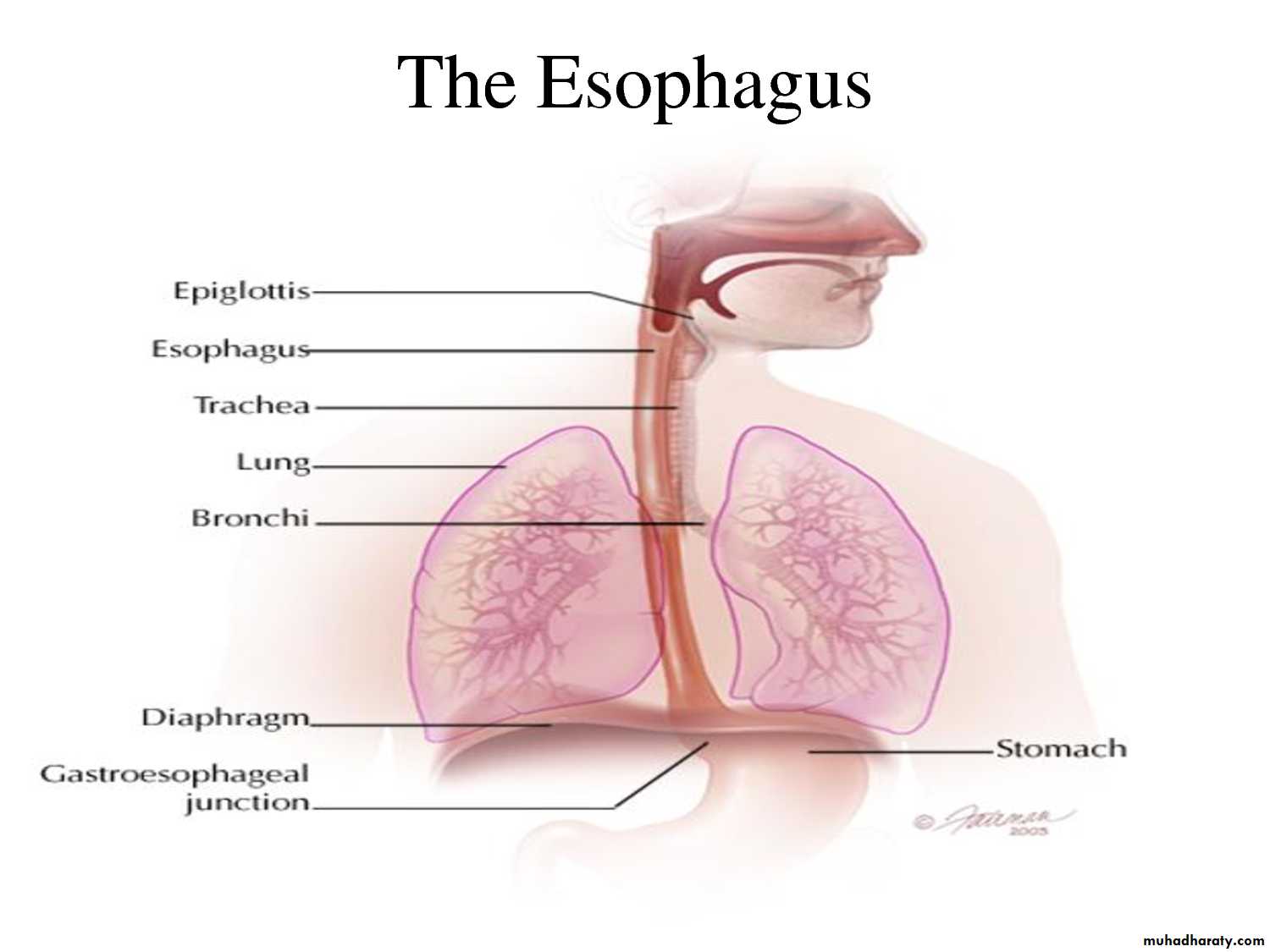
Esophagus
• The esophagus is a 25-cm long muscular tube that connects the pharynx to the stomach.
• The esophagus extends from the lower border of the cricoid cartilage (at the level of the sixth cervical vertebra) to the cardiac orifice of the stomach at the side of the body of the 11th thoracic vertebra• In its vertical course, the esophagus has 2 gentle curves in the coronal plane.
• The first curve begins a little below the commencement of the esophagus and inclines to the left as far as the root of the neck and returns to the midline at the level of fifth thoracic vertebra.
• The second curve to the left is formed as the esophagus bends to cross the descending thoracic aorta, before it pierces the diaphragm.
• The esophagus also has anteroposterior curvatures that correspond to the curvatures of the cervical and thoracic part of the vertebral column.
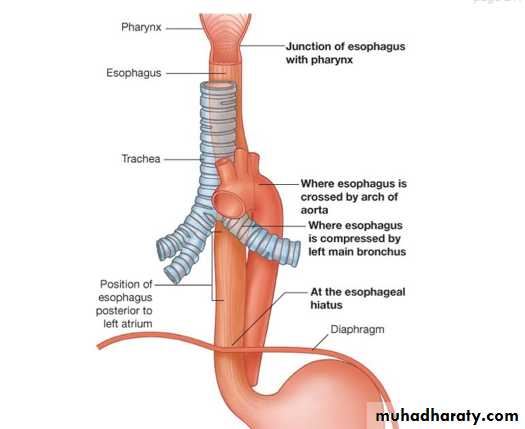
Constrictions
The esophagus is constricted in three places.
The esophagus has four points of constriction. When a corrosive substance, or a solid object is swallowed, it is most likely to lodge and damage one of these four points. These constrictions arise from particular structures that compress the esophagus. These constrictions are:
• At the start of the esophagus, where the laryngopharynx joins the esophagus, behind the cricoid cartilage
• Where it is crossed on the front by the aortic arch in the superior mediastinum
• Where the esophagus is compressed by the left main bronchus in the posterior mediastinum
• The esophageal hiatus where it passes through the diaphragm in the posterior mediastinum
Constrictions
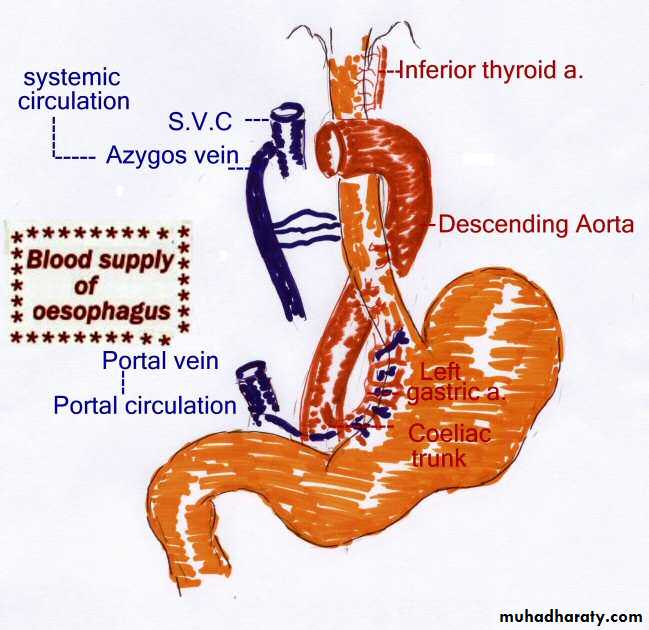
• Blood supply of esophagus:
• Arteries:• The upper third of the esophagus, which lies in the region of the neck, is supplied by the inferior thyroid artery.
• The middle third, which lies in the thorax, is supplies by the branches from the descending thoracic aorta.
•
• And the lower third, which lies in the abdomen, is supplies by the left gastric artery.
• Veins:
• The veins from the upper third portion join the inferior thyroid veins, from the middle third join the azygous vein and from the lower third join the left gastric vein (tributary of the portal vein).
Blood supply of the esophagus
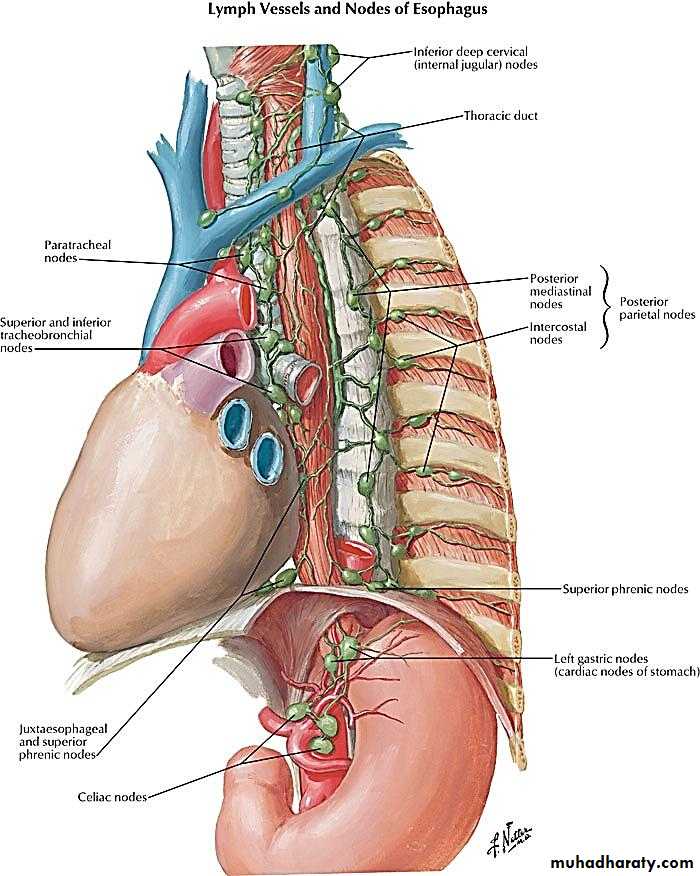
• Lymph drainage of esophagus:
• As is the case with the blood supply, the lymph drainage is also different for the three parts of esophagus.• The lymphatics from the upper third of esophagus drain into the deep cervical nodes.
• Those from the middle third drain into the superior and posterior Mediastinal nodes
• and the lymphatics from the lower third drain into the celiac nodes.
Lymph drainage of the esophagus
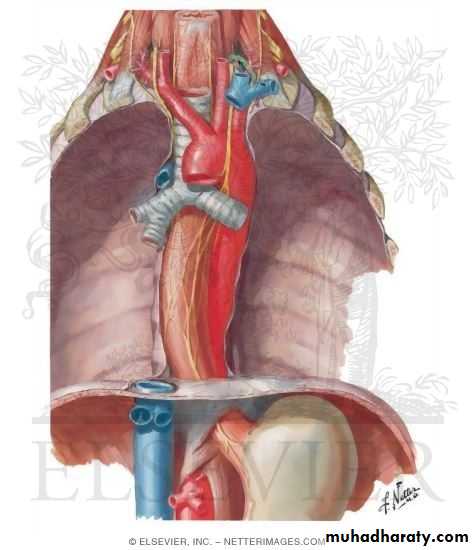
Relations of esophagus
Ant.: trachea, left recurrent laryngeal n., left principal bronchus, pericardium.Pos.: bodies of thoracic vertebrae, thoracic duct, azygos veins, right pos. intercostal arteries, descending thoracic aorta (at its lower end).
Right side: mediastinal pleura, terminal part of azygos v.
Left side: left subclavian a., aortic arch, thoracic duct, mediastinal pleura.
Relations of esophagus
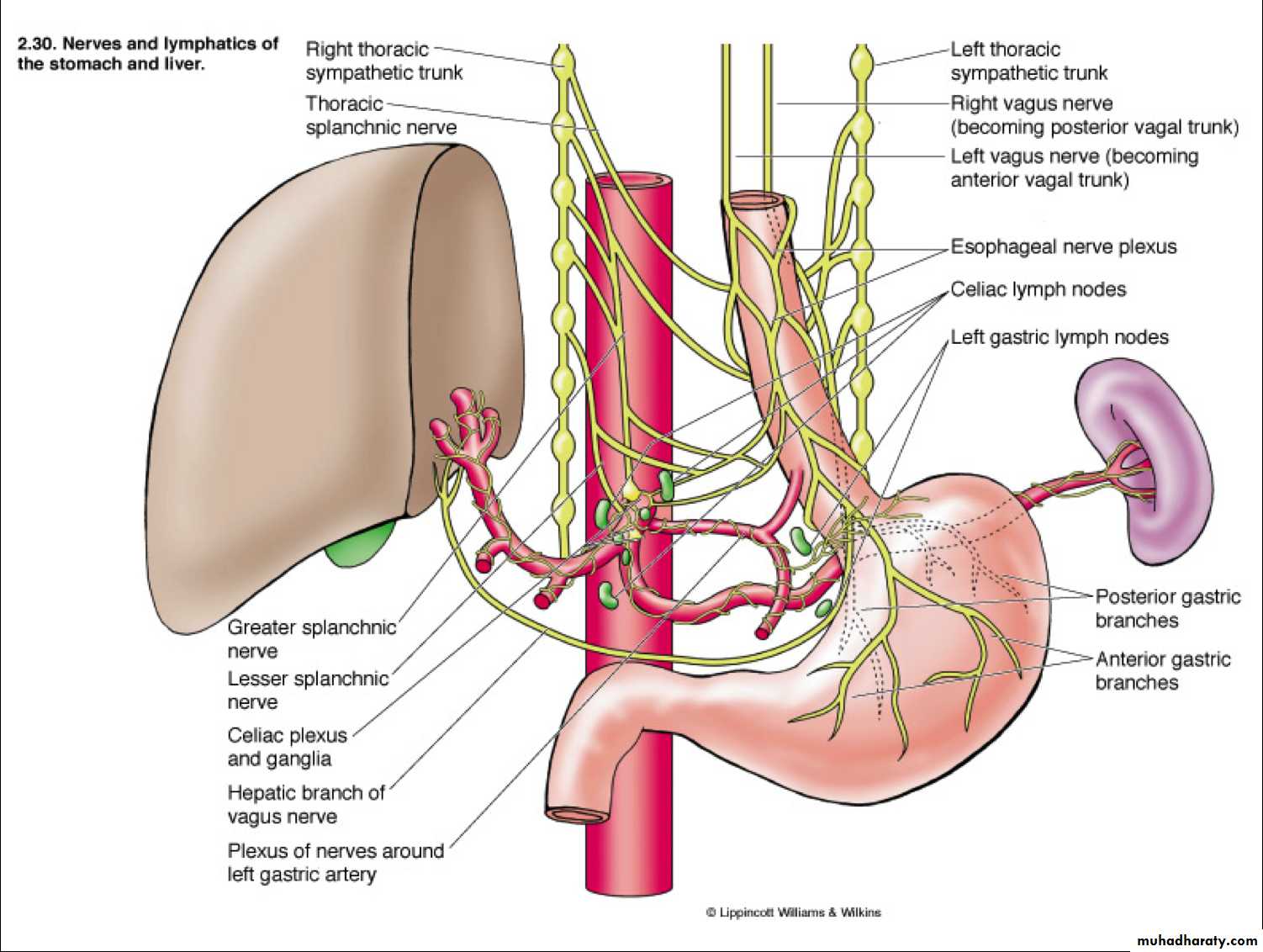
Nerve supply of the esophagus
• The esophagus is innervated by the vagus nerve and the cervical and thoracic sympathetic trunk.
• The vagus nerve has a parasympathetic function, supplying the muscles of the esophagus and stimulating glandular contraction.
• Two sets of nerve fibers travel in the vagus nerve to supply the muscles.
• The upper striated muscle, and upper esophageal sphincter, are supplied by neurons with bodies in the nucleus ambiguus,
• whereas fibers that supply the smooth muscle and lower esophageal sphincter have bodies situated in the dorsal motor nucleus.
• The vagus nerve plays the primary role in initiating peristalsis.
• The sympathetic trunk has a sympathetic function.
• It may enhance the function of the vagus nerve, increasing peristalsis and glandular activity, and causing sphincter contraction.• In addition, sympathetic activation may relax the muscle wall and cause blood vessel constriction.
• Sensation along the esophagus is supplied by both nerves, with gross sensation being passed in the vagus nerve and pain passed up the sympathetic trunk.
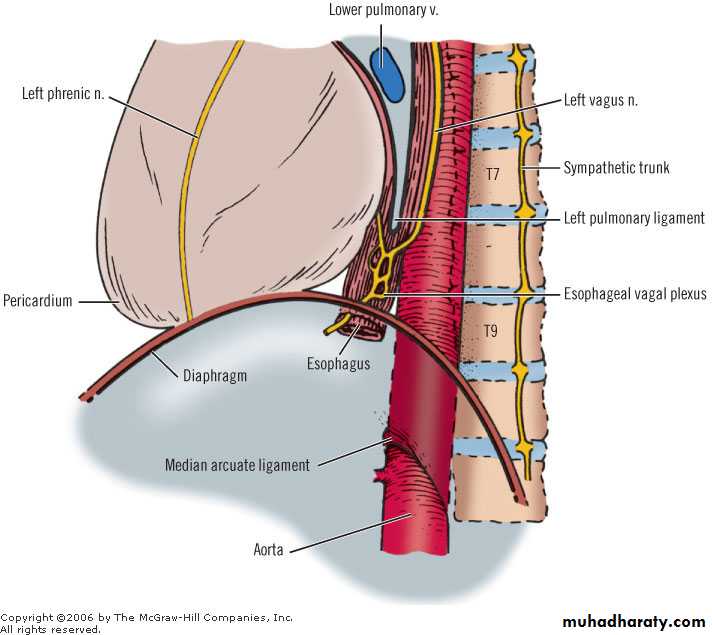
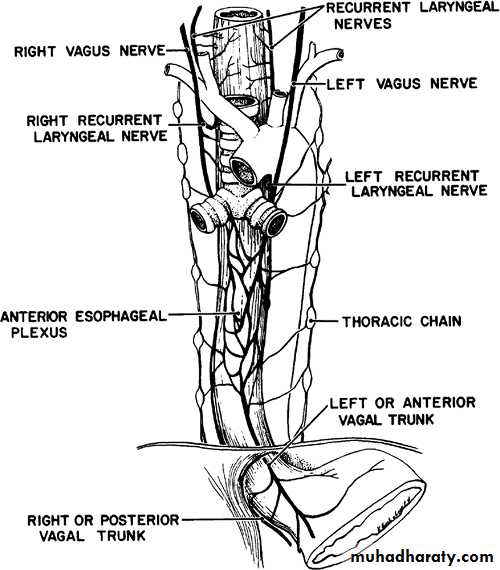
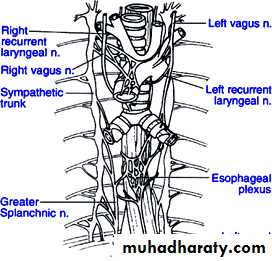
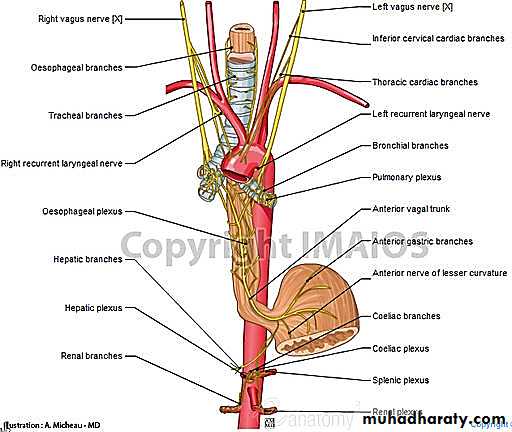
Esophageal plexus.
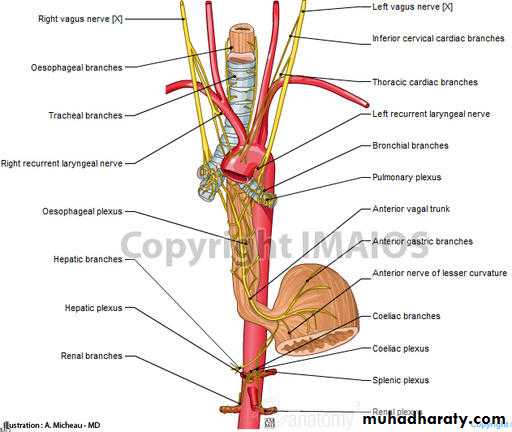
• The esophageal plexus is formed by nerve fibers from two sources, branches of the vagus nerve and visceral branches of the sympathetic trunk.
• Parasympathetic fibers:
• 1. The vagus nerve delivers two fiber types to the esophageal plexus:• A. Preganglionic parasympathetic fibers (Preganglionic fibers) - These fibers have their cell bodies located in the dorsal motor nucleus of the vagus and they will synapse on the terminal ganglia in the walls of the esophagus.
• B. Afferent fibers - These fibers are primarily concerned with autonomic reflexes and they have their cell bodies in the inferior ganglion of the vagus.
• Note: These vagal fibers in the esophageal plexus reform to make the anterior vagal trunk (left vagus) and the posterior vagal trunk(right vagus).
• Anterior and posterior being terms in relation to the esophagus, a mnemonic for which is 'LARP': Left becomes Anterior, Right becomes Posterior.
• Sympathetic fibers
• 2. The visceral branches of the sympathetic trunk also deliver two fiber types to the esophageal plexus• A. sympathetic postganglionic fibers- The cell bodies of these fibers are located in the sympathetic chain ganglia.
• The cell bodies of the preganglionic fibers, the first neuron of this two neuron chain, are located in the intermediolateral cell column (IMLCC) of the thoracic spinal cord.
• B. Afferent fibers- These fibers are primarily concerned with pain and have cell bodies located in the dorsal root ganglion.
Nerves of the thorax
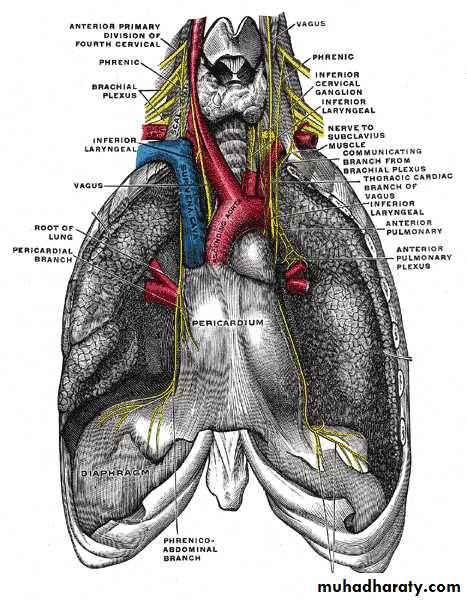
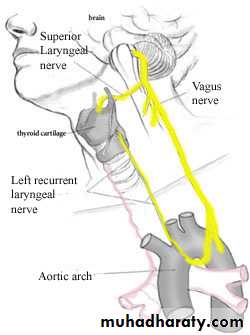
Vagus nerves
Vagus Nerve
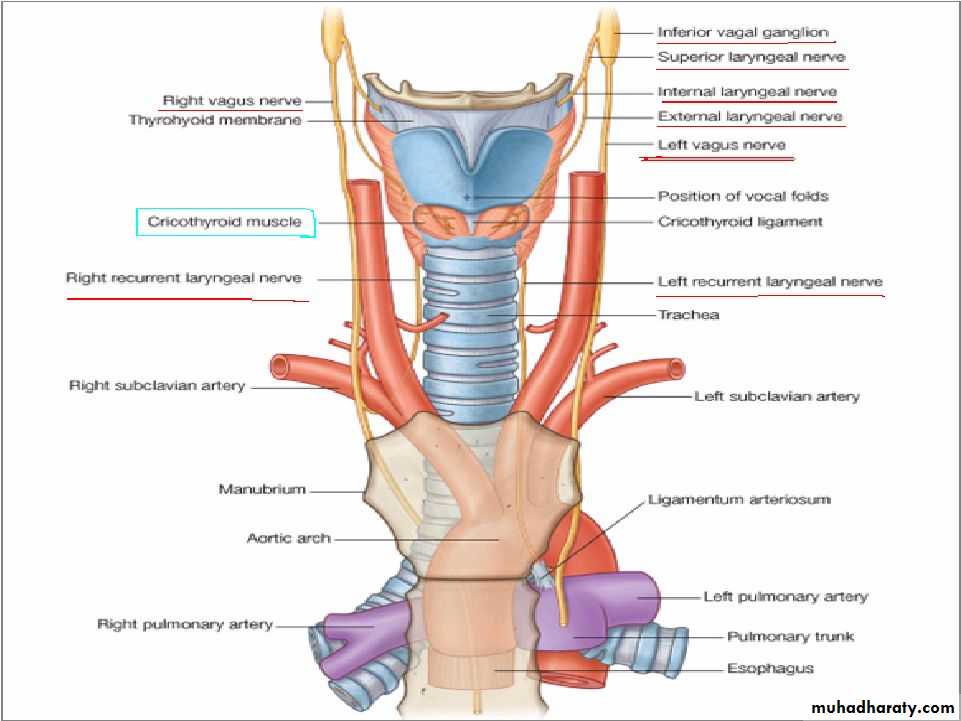
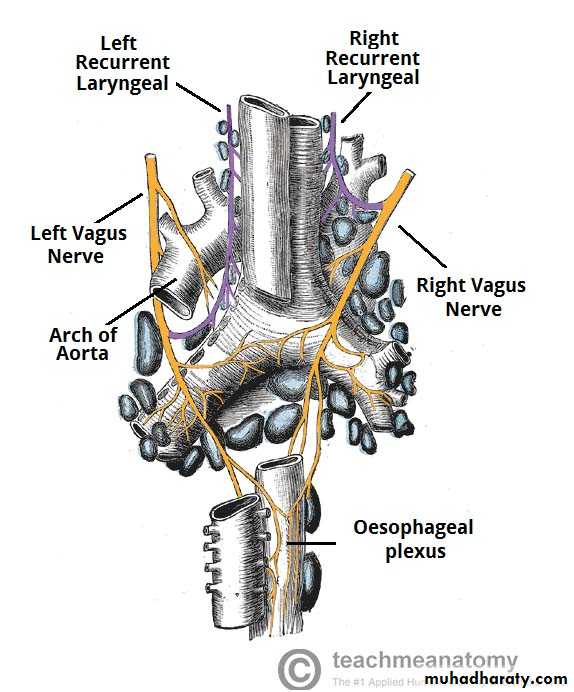
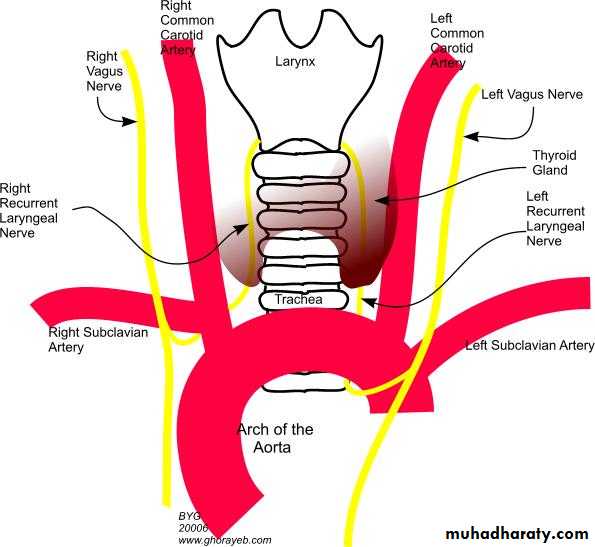
• 1.The right vagus nerve reaches the thorax on the right side of the trachea, which separates it from the right pleura.• 2. gives rise to the right recurrent laryngeal nerve, which hooks around the right subclavian artery and ascends into the neck between the trachea and esophagus.
• 3,The right vagus then crosses anterior to the right subclavian artery,
• 4. runs posterior to the superior vena cava,
• 5.descends posterior to the right main bronchus,
The right vagus nerve
• 6.It then inclines behind the hilum of the right lung and• 7.courses medially toward the esophagus to form the esophageal plexus with the left vagus nerve.
• and contributes to cardiac, pulmonary, and esophageal plexuses.
It forms the posterior vagal trunk at the lower part of the esophagus and enters the diaphragm through the esophageal hiatus.
The left vagus
• 1.crosses in front of the left subclavian artery• 2.to enter the thorax between the left common carotid and subclavian arteries.
• 3. It descends on the left side of the aortic arch, which separates it from the left pleura,
• 4.and travels behind the phrenic nerve.
• 5.It courses behind the root of the left lung
• 6.and then deviates medially and downwards to reach the esophagus and form the esophageal plexus by joining the opposite (right) vagus nerve.
Vagus nerves
The left vagus nerve
• It gives rise to the left recurrent laryngeal nerve, which hooks around the aortic arch to the left of the ligamentum arteriosum and ascends between the trachea and esophagus.• The left vagus further gives off thoracic cardiac branches, breaks up into the pulmonary plexus, continues into the esophageal plexus, and enters the abdomen as the anterior vagal trunk in the esophageal hiatus of the diaphragm.
• The anterior gastric branches of anterior vagal trunk are branches of the anterior vagal trunk which supply the stomach
• The anterior and posterior gastric nerves are then formed from the esophageal plexus.
• The anterior gastric is formed mainly from the left vagus, but it does contain fibers from the right vagus.
• Similarly, the posterior gastric nerve is formed mainly from the right vagus but contains fibers from the left vagus nerve.
• The gastric nerves supply all abdominal organs and the gastrointestinal tract ending just before the left colonic (splenic) flexure .
Vagus nerve branches in the thorax(4)
• 1.Left recurrent laryngeal nerve – it hooks under the arch of the aorta, ascending to innervate the majority of the intrinsic muscles of the larynx.• 2.The inferior cardiac branch
• On the right side, it arises from the trunk of the vagus as it lies beside the trachea. On the left side, it originates from the recurrent laryngeal nerve only. These branches end in the deep part of the cardiac plexus.
• 3.The anterior and posterior bronchial branches are distributed as 2-3 branches on the anterior surface of the root of the lung.
• They form the anterior pulmonary plexus after joining branches from the sympathetic trunk.
• The posterior bronchial branches are larger than the anterior and lie on the posterior surface of the root of the lung to form the posterior pulmonary plexus (with contributory sympathetic fibers) as well.
Vagus nerve branches in the thorax
Pulmonary plexus.Vagus nerve branches in the thorax
• 4.The esophageal branches are anterior and posterior branches. Together they form the esophageal plexus.
• The posterior surface of the pericardium is supplied by filaments from this plexus.
Right vagus n.
It passes behind the root of the right lung.
Esophageal plexus.
Left vagus n.
It turns backward behind the root of the left lung.
Esophageal plexus.
Branches
Left recurrent laryngeal n.
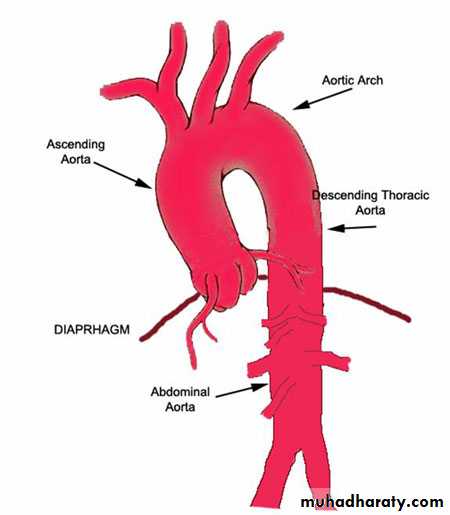
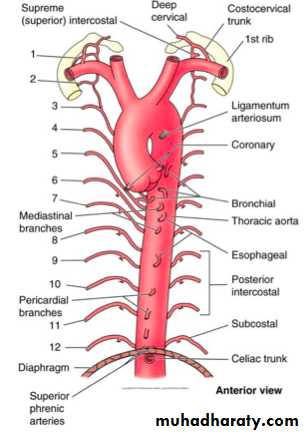
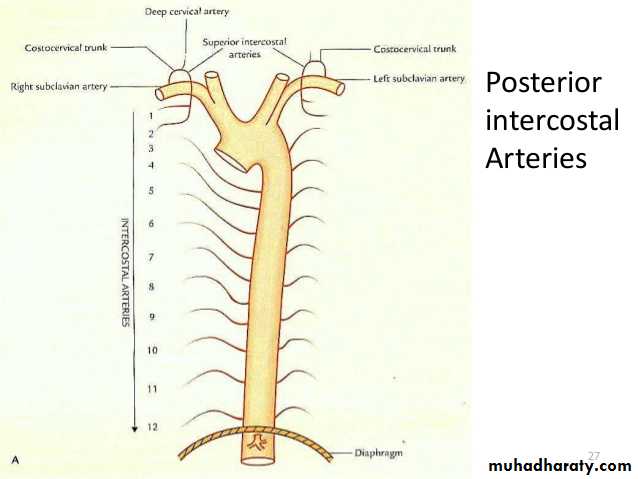
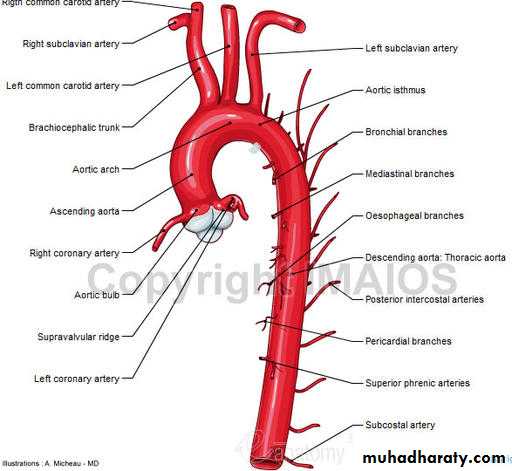
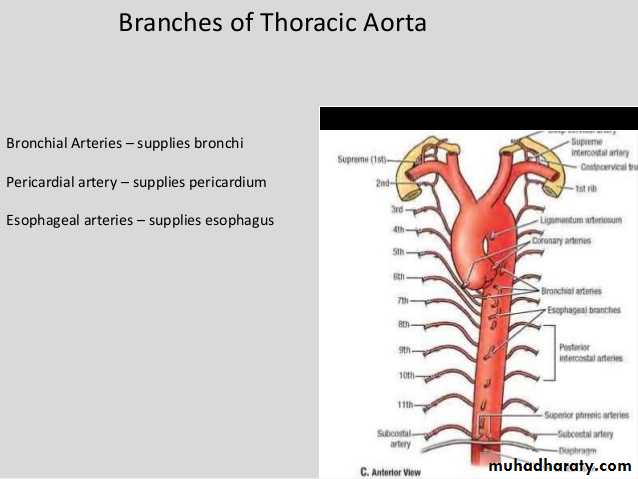
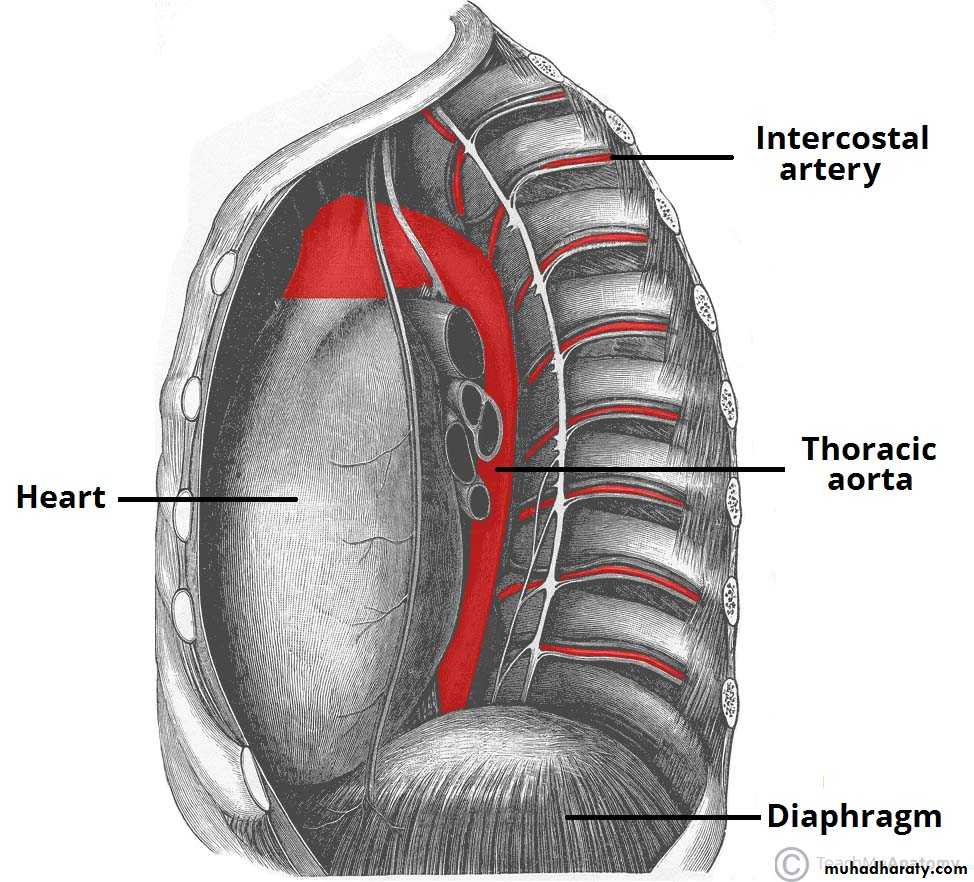
Descending thoracic aorta
descending aorta (thoracic aorta)
• The aorta originates from the left ventricle of the heart. It ends in the abdomen where it branches into the two common iliac arteries. The aorta has five separate segments.• The descending aorta begins at the arch of the aorta (where it loops over the heart to begin its descent). It is divided into two segments, the thoracic and the abdominal.
• The descending aorta (thoracic aorta) is between the arch of the aorta and the diaphragm muscle below the ribs.
• At the origination point, it is on the left side of the vertebrae. As it descends, it winds around the vertebrae and ends in front. The diameter of the artery is 2.32 centimeters.
• It has six paired branches: bronchial arteries, mediastinal arteries, esophageal arteries, pericardial arteries, superior phrenic artery, and intercostal arteries and subcostal A.
• BMEPPP
Branches
Posterior intercostal arteries.
Subcostal arteries.
Pericardial, esophageal, and bronchial arteries.
• There are nine pairs of the intercostal arteries. The right branches are longer than the left, because the descending aorta (thoracic aorta) is on the left side of the vertebrae.
• Through its various branches, it supplies blood to the esophagus, lungs, and the chest area, including the ribs and mammary glands.
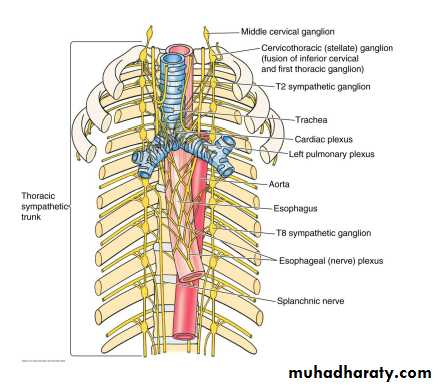
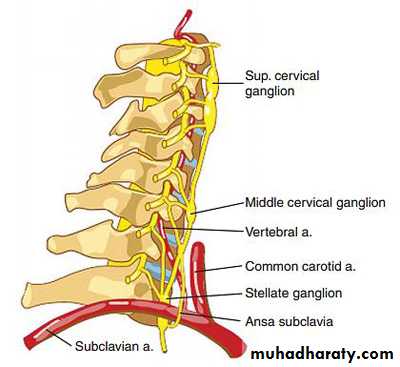
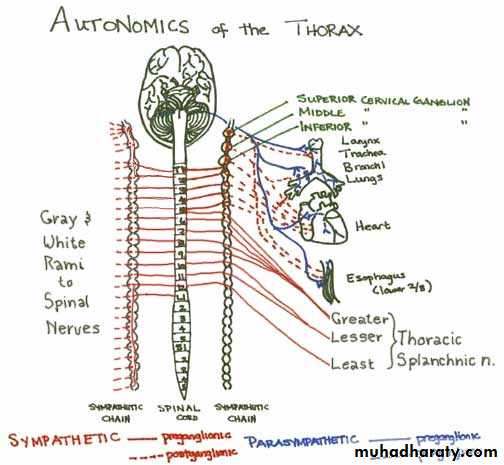
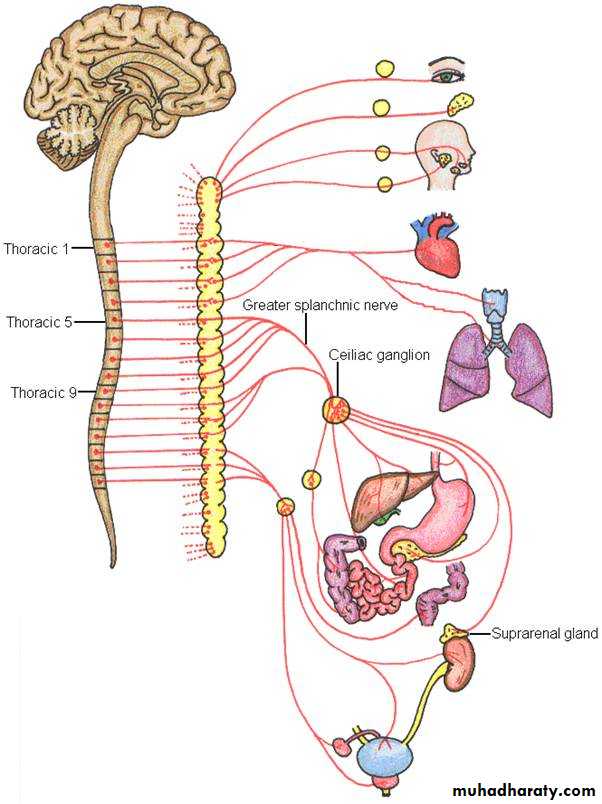
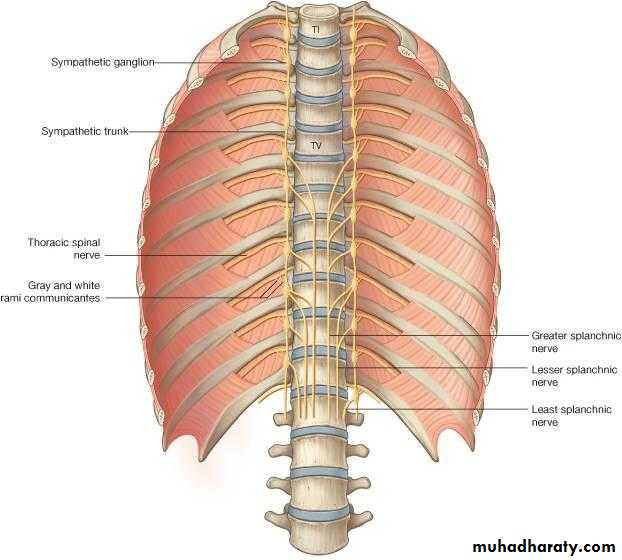
Thoracic part of the sympathetic trunk
The sympathetic trunk
• Lying on the necks of the ribs, just lateral to their heads, and anterior to the intercostal vessels and nerves, is the thoracic part of the sympathetic trunk. It is described as possessing 12 ganglia, one for each intercostal nerve, but characteristically there are fewer, the result of fusion of adjacent ganglia.
• Thus the first ganglion is commonly fused with the inferior cervical ganglion to form the cervicothoracic (stellate) ganglion.
• Each receives a white ramus from its corresponding spinal nerve, and this emerges from the anterior ramus of the nerve. After relay in the ganglion a postganglionic gray ramus is given to each thoracic nerve, and this usually lies medial to the white ramus.
• It lies just lateral to the vertebral bodies for the entire length of the vertebral column. It interacts with the anterior rami of spinal nerves by way of rami communicantes.
• The sympathetic trunk permits preganglionic fibers of the sympathetic nervous system to ascend to spinal levels superior to T1 and descend to spinal levels inferior to L2/3.
• The superior end of it is continued upward through the carotid canal into the skull, and forms a plexus on the internal carotid artery; the inferior part travels in front of the coccyx, where it converges with the other trunk at a structure known as the ganglion impar.
• Along the length of the sympathetic trunk are sympathetic ganglia known as paravertebral ganglia.
• In general, there are two kinds of neurons involved in the transmission of any signal through the sympathetic system: pre-ganglionic and post-ganglionic.
• The shorter preganglionic neurons originate from the thoracolumbar region of the spinal cord specifically at T1 to L2~L3, and travel to a ganglion, often one of the paravertebral ganglia, where they synapse with a postganglionic neuron. From there, the long postganglionic neurons extend across most of the body.
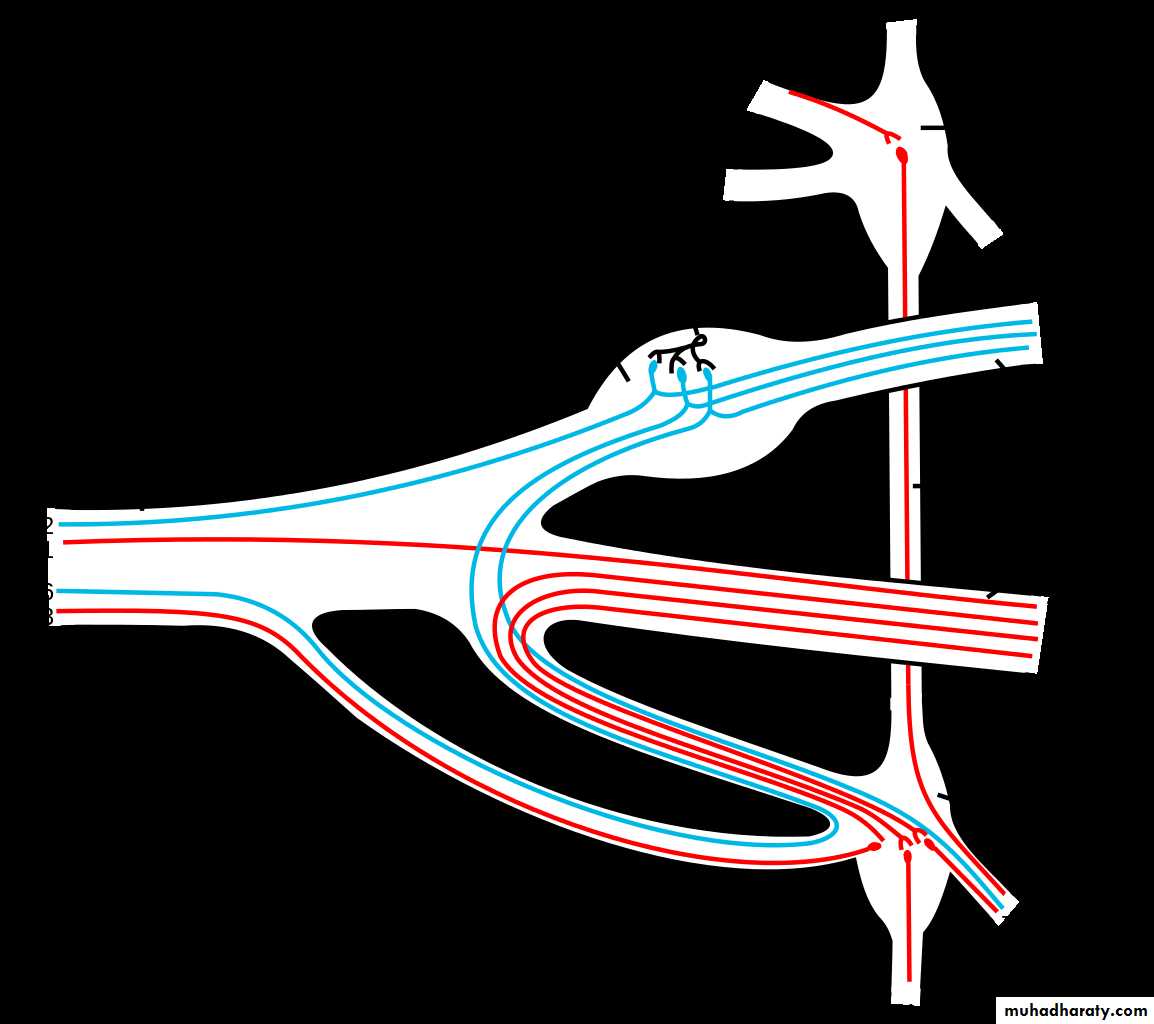
• Gray ramus communicans
• The grey rami communicantes exist at every level of the spinal cord and are responsible for carrying postganglionic nerve fibres from the paravertebral ganglia to their destination, and for carrying those preganglionic nerve fibres which enter the paravertebral ganglia but do not synapse.
• White ramus communicans
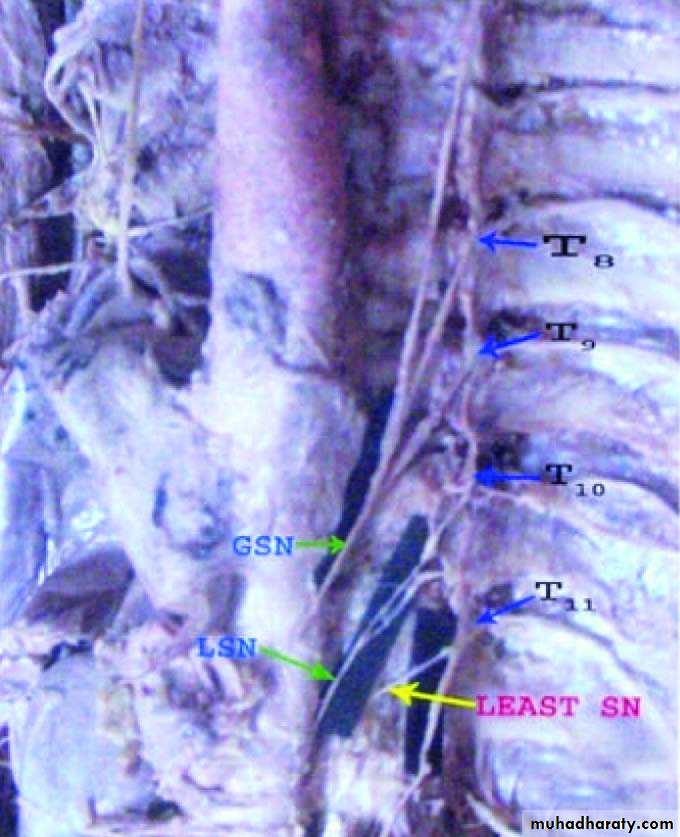
• The white rami communicantes exist only at the levels of the spinal cord where the intermediolateral cell column is present (T1-L2) and are responsible for carrying preganglionic nerve fibres from the spinal cord to the paravertebral ganglia.• Thoracic splanchnic nerves
•
• Thoracic splanchnic nerves are splanchnic nerves that arise from the sympathetic trunk in the thorax and travel inferiorly to provide sympathetic innervation to the abdomen. The nerves contain preganglionic sympathetic and general visceral afferent fibers.
• There are three main thoracic splanchnic nerves:
•
White and gray ramus communicans.
Scheme showing pathways (white/grey rami are spatially reversed, possibly for clarity?) of a typical spinal nerve.1. Somatic efferent.2. Somatic afferent.3,4,5. Sympathetic efferent.6,7. Parasympathetic afferent.
Stellate ganglion.
Branches
• Gray rami communicantes.• Postganglionic fibers to the heart, aorta, lungs, and esophagus.
• Splanchnic nerves.
Branches
Greater splanchnic n.
Lesser splanchnic n.
Lowest splanchnic n.
Thoracic duct
1.In human anatomy, the thoracic duct is the largest of the two lymph ducts of the lymphatic system.
2.The other duct is the right lymphatic duct.
3.It carries chyle, a liquid containing both lymph and emulsified fats, rather than pure lymph.
4.In adults, the thoracic duct is typically 38–45 cm in length and has an average diameter of about 5 mm.
5.The vessel usually starts from the level of the T12 and extends to the root of the neck.
6.It drains into the systemic (blood) circulation at the angle of the left subclavian and internal jugular veins as a single trunk, at the commencement of the brachiocephalic vein.
7. It also collects most of the lymph in the body other than from the right thorax, arm, head, and neck which are drained by the right lymphatic duct.
8.The thoracic duct originates in the abdomen from the confluence of the right and left lumbar trunks and the intestinal trunk, forming a significant pathway upward called the cisterna chyli.
9. It traverses the diaphragm at the aortic aperture and ascends the superior and posterior mediastinum between the descending thoracic aorta (to its left) and the azygos vein (to its right). The duct extends vertically in the chest and curves posteriorly to the left carotid artery and left internal jugular vein at the T5 vertebral level it drains into the systemic (blood) circulation at the venous angle of the left subclavian and internal jugular veins as a single trunk, at the commencement of the brachiocephalic vein, below the clavicle.
The azygos vein
1.The azygos vein is a vein running up the side of the thoracic vertebral column draining itself towards the superior vena cava.2.It connects the systems of superior vena cava and inferior vena cava and can provide an alternative path for blood to the right atrium when either of the venae cavae is blocked.
3. The azygos vein transports deoxygenated blood from the posterior walls of the thorax and abdomen into the superior vena cava vein.
4. The anatomy of this blood vessel can be quite variable. In some rare variations for example, it also drains thoracic veins, bronchial veins and even gonadal veins. The vein is so named because it has no symmetrically equivalent vein on the left side of the body.
5.It is formed by the union of the ascending lumbar veins with the right subcostal veins at the level of the 12th thoracic vertebra, ascending in the posterior mediastinum, and arching over the right main bronchus posteriorly at the root of the right lung to join the superior vena cava.
6. This "arch of the azygos vein" is an important anatomic landmark. As an anatomical variation in 1-2% of the population, the arch can be displaced laterally, thereby creating a pleural septum separating an azygos lobe from the upper lobe of the right lung.
7.A major tributary is the hemiazygos vein, a similar structure on the opposite side of the vertebral column. Other tributaries include the bronchial veins, pericardial veins, and posterior right intercostal veins. It communicates with the vertebrael venous plexuses
The hemiazygos vein
1.is a vein running superiorly in the lower thoracic region, just to the left side of the vertebral column
2.The hemiazygos vein and the accessory hemiazygos vein, when taken together, essentially serve as the left-sided equivalent of the azygos vein.
3. That is, the azygos vein serves to drain most of the posterior intercostal veins on the right side of the body, and the hemiazygos vein and the accessory hemiazygos vein drain most of the posterior intercostal veins on the left side of the body. Specifically, the hemiazygos vein mirrors the bottom part of the azygos vein.
4.The structure of the hemiazygos vein is often variable. It usually begins in the left ascending lumbar vein or renal vein, and passes upward through the left crus of the diaphragm to enter the thorax. It continues ascending on the left side of the vertebral column, and around the level of the ninth thoracic vertebra, it passes rightward across the column, behind the aorta, esophagus, and thoracic duct, to end in the azygos vein.
5.The hemiazygos may or may not be continuous superiorly with the accessory hemiazygos vein.
6.It receives the 9th, 10th, and 11th posterior intercostal veins and the subcostal vein of the left side, and some esophageal and mediastinal veins.
.