Eczema (dermatitis) and Lichenification
Ecema1
2
The word 'eczema' comes from the Greek for 'boiling' that are often seen in the early acute stages of the disorder, but less often in its later chronic stages.
Although the terms dermatitis and eczema are nowadays generally regarded as synonymous , so that all eczema is regarded as dermatitis but not all dermatitis is eczema . The most common skin conditions (20% of all new patients).
Definition
Stages of eczema:There are three stages1)Acute eczema: (primary lesions are vesicles, blisters).
HP: oedema in the epidermis (spongiosis) progress to intraepidermal vesicles, which may form larger blisters.
3
4
2)Subacute eczema: (less edema; few vesicles) erythema and scale are present in various patterns, usually with indistinct borders.
HP: spongiosis diminished , thickening of the prickle cell layer (acanthosis ), with formation of a parakeratotic (retention of nuclei in the horny layer)
5
3)Chronic eczema: less vesicular and exudative; more scaly and thickened; more likely to show lichenification; and more likely fissure.
HP:less spongiosis and vesication more thickening of the prickle cell layer (acanthosis) and horny layer (hyperkeratosis) and retention of nuclei in the horny layer(parakeratosis).
6
It involves the interaction between three things :
a. Triggering factor ,
b. Keratinocytes ,
c. T-lymphocytes , which seems particularly important in most eczema types
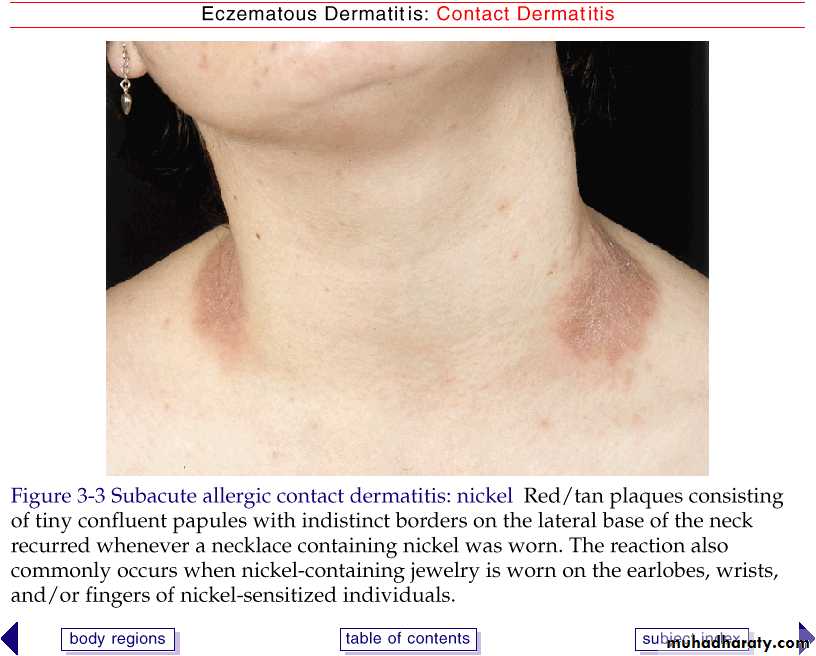
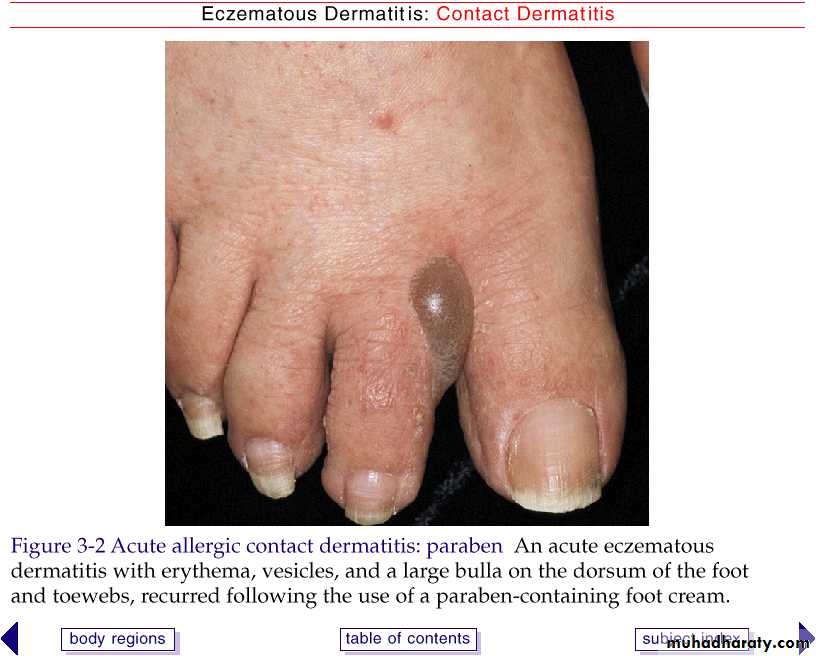
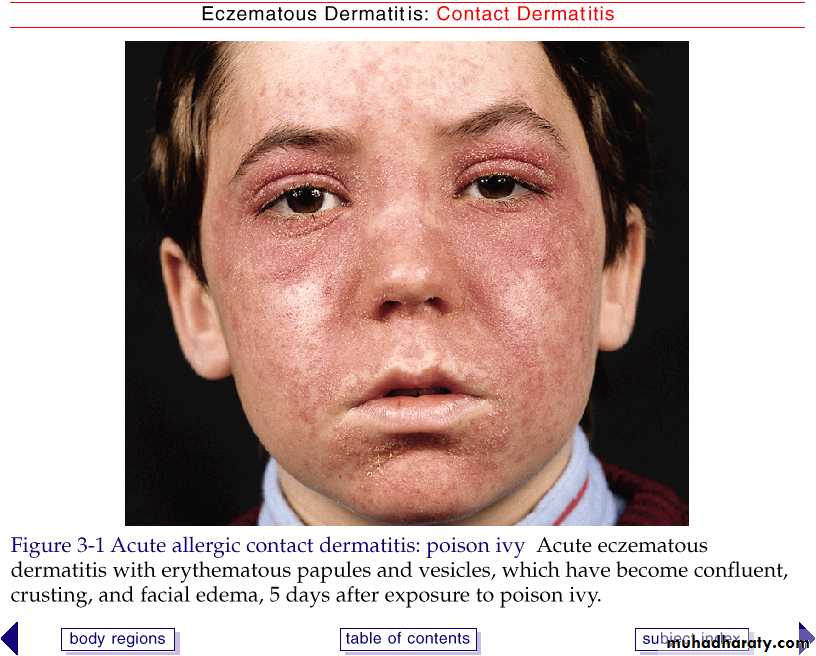
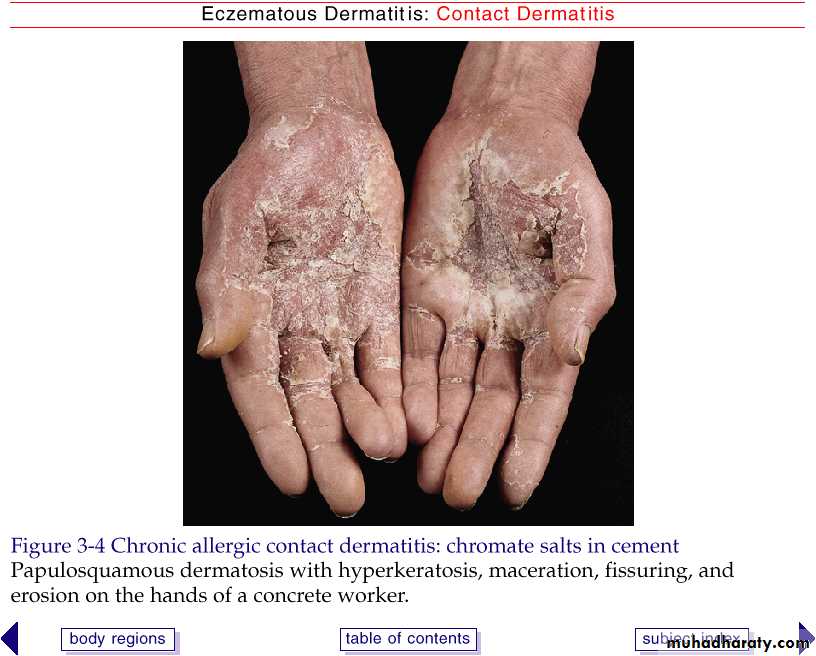
Allergic contact dermatitis is the consequence of an immune reaction mediated by T cells against low molecular weight chemicals known as haptens.
in allergic contact dermatitis arises as a result of two essential stages: an induction phase, which primes and sensitizes the immune system for an allergic response, and an elicitation phase, in which this response is triggered. As it involves a cell-mediated allergic response, ACD is termed a type 1V delayed type hypersensitivity which is mediated by hapten-specific T cells.
Pathogenesis
7Irritant contact dermatitis is a nonspecific response of the skin to direct chemical damage that releases mediators of inflammation predominantely from epidermal cells.
In irritant contact dermatitis , the three predominant processes are : *disturbed barrier function , *epidermal cell damage and *release of inflammatory mediators and cytokines , which induce morphological changes apparent histologically and clinically as eczema
It is not immune mediated
Pathogenesis
8
Pathogenesis
Secondary dissemination :
A very characteristic feature of eczema is it's tendency to spread far from it's point of origin . There are four main mechanisms of dissemination :
• Spread by contact with external allergen: e.g. a contact dermatitis of the lower leg induced by lanolin ointment , may spread to the hand and the face as a result of casual contact during application of the ointment .
2. Spread by ingestion or injection of an allergen: an eruption originally induced by sensitivity to topical allergen (e.g. allergic contact dermatitis) may relapse after ingestion or injection of the same chemical , e.g. medication that can be used topically or systemically .
9
Pathogenesis
Secondary dissemination :
3. Conditional hyperirritability ('angry back' syndrome) : this term refers to the phenomenon where by an area of inflamed skin on one part of the body results in generalized hyperirritability of the skin sites , that are distant from the primary site of inflammation .
4. Bacterial hypersensitivity : heavily infected eczema will some times disseminate in the absence of demonstrable allergic sensitivity to topical medication , it is probably that allergy to bacteria or their products is some times a factor in the dissemination .
Classification:
10Exogenous eczema
Irritant eczema
Allergic contact eczema
Photoallergic contact eczema
Eczematous polymorphic light eruption
Infective eczema
Dermatophytide
Post-traumatic eczema
11
Endogenous eczema
Atopic eczema
Seborrhoeic eczema
Asteatotic eczema
Discoid eczema
Eyelid eczema
Exudative discoid and lichenoid chronic dermatosis
Chronic superficial scaly dermatitis
Pityriasis alba
Hand eczema
Venous eczema
Juvenile plantar dermatosis
Metabolic eczema or eczema associated with systemic disease
Eczematous drug eruptions
12
Exogenous eczema
Irritant and allergic contact eczema.
Irritant
Allergic
Incidence
everyone
Only in the sensitized
Sensitization
No previous sensitization
Two phases: sensitization phase and elicitation phase
Mechanism
Nonimmunologic; a physical and chemical alteration of epidermis.
Delayed hypersensitivity reaction.
Number of exposure
Few to many
One or several to cause sensitization.
Nature of substance
Organic solvent, soap
Low-molecular-weight hapten (metals, formalin)
13
14
Concentration of substance required
Usually high
May be very low
Mode of onset
Usually gradual as epidermal barrier becomes compromised
Once sensitized, usually rapid; 12-48h after exposure.
Distribution
Borders usually indistinct
May correspond exactly to contactant (watchband)
Investigative procedure
Trial avoidance
Trial avoidance, patch testing, or both
Management
Protection and reduced incidence of exposure
Complete avoidance
dermatitis
Napkin dermatitis; housewife dermatitis
Lip-stick dermatitis; nylon; dyes (hair dermatitis); shoes dermatitis; metal
15
• Napkin (diaper) dermatitis:
• the most common type is irritant in origin, and is aggravated by the use of waterproof plastic pants. The mixture of faecal enzymes and ammonia produced by urea-splitting bacteria, if allowed to remain in prolonged contact with the skin, leads to a severe reaction. The fold remain unaffected in contrast to intertrigo, inverse psoriasis, and candidiasis.
16
Infective dermatitis (microbial eczema):
eczema that is caused by microorganisms or their products , which clears when the organisms are eradicated . This should be distinguished from infected eczema , in which eczema is complicated by secondary infection (bacterial or viral) .
17
Dermatophytid:
A reaction, at a remote site, to a dermatophyte infection. This diagnosis should be suspected when the presence of a dermatophyte infection has been established and no fungus can be demonstrated in the dermatophytid lesions.
The diagnosis is supported further by clearing of the dermatophytid after the dermatophyte has been eradicated.
Eczematous vesicles on the hands or feet are the commonest pattern
18
Endogenous eczema:
Atopic dermatitis
The word ‘atopy’ comes from the Greek ‘without a place’. It was introduced years ago to designate a group of patients who had a personal or family history of one or more of the following diseases: high fever, asthma, very dry skin, and eczema.19
Stages of AD:three stages:
1-Infantile AD: Occurring from 2 months to 2 years of age.2-childhood AD: From 2-10 years.
3-Adults AD.
In all stages, pruritus is present. Itching often precede the appearance of lesions, hence the concept that AD is “the itch that rashes”.
20
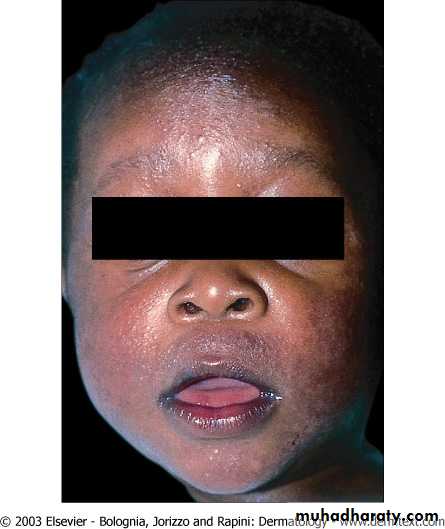
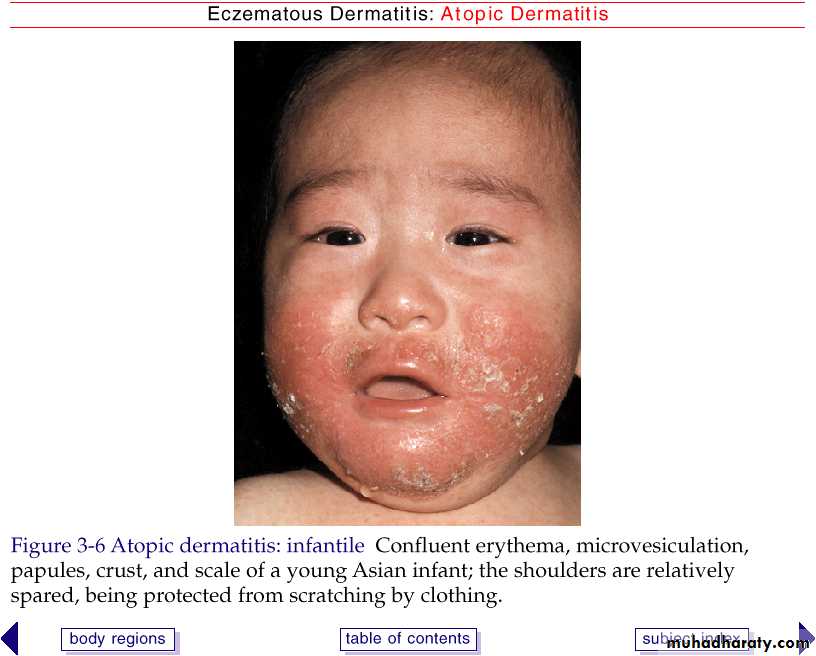
Infantile Atopic Dermatitis
60% of case AD present in the first year of life, after 2 months of age
Begin as itchy erythema and scaling of the cheeks
Distribution include scalp, neck, forehead, wrist, and extensors
May become desquamate leading to erythroderma.
Most cases the symptoms will disappear toward the end of the second year.
Egg, peanut, milk, wheat, fish, soy, and chicken may exacerbate infantile AD
Involvement of the cheeks is characteristic of the infantile pattern of AD.
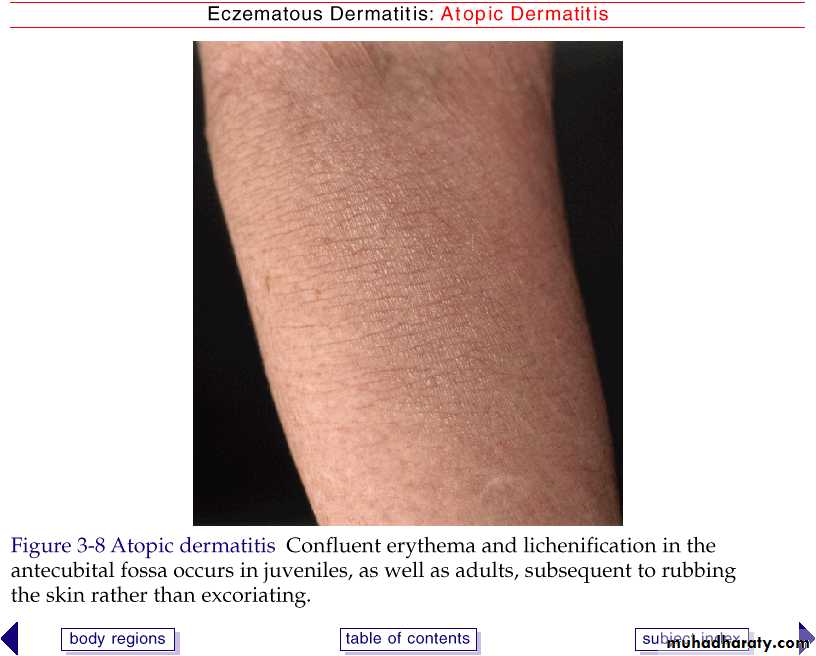
Childhood Atopic DermatitisCharacterized by less exudative lesions.
Distribution: antecubital and popliteal fossae, flexor wrist, eyelids, and face.
A vicious cycle may be established (the itch-scratch cycle), as pruritus leads to scratching, and scratching causes secondary changes that themselves cause itching.
Severe atopic dermatitis involving more than 50% of body surface area is associated with growth retardation.
24
Childhood Atopic Dermatitis
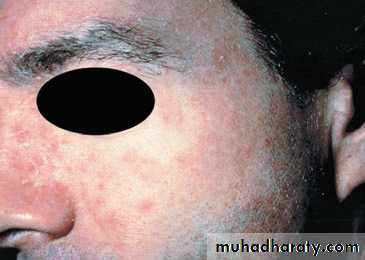
Adult Atopic Dermatitis
Distribution: antecubital and popliteal fossae, the front side of the neck, the forehead, and area around the eyes.Atopic individuals are at greater risk of developing hand dermatitis than are the rest of the population
Lichenification and prurigo-like papules are common.
70% develop hand dermatitis some times in their lives
Adult Atopic Dermatitis
Associated features and complications:Cutaneous stigmata:
Dennie-Morgan fold: a linear transverse fold just below the edge of the lower eyelids.
Pityriasis alba: poorly marginated hypopigmented, slightly scaly patches on the cheeks, upper arms, trunk, in young children.
Keratosis pilaris: horny follicular lesionsof arms, legs, cheeks, and buttocks.
Hertoghe’s sign – thinning of the lateral eyebrows
Hyperkeratosis and hyperpigmentation of the neck “dirty neck”
27
Vascular Stigmata
Headlight sign – perioral, perinasal and periorbital pallorWhite dermographism – blanching of the skin at the site of stroking .
Low finger temperature.
Pronounced vasoconstriction on exposure to cold.
Ophthalmologic abnormalities:
cataracts.
Infection
More than 90% of chronic lesions contain Staph aureus.Eczema herpeticum – generalized herpes simplex infection.
Vaccination against smallpox is contraindicated in person with atopic dermatitis. Even when condition is in remission, widespread and even fatal vaccinia can occur. Complicated varicella.
Warts; molluscum contagiosum.
Triggering factors
Temperature change and sweatingDecreased humidity
Excessive washing
Contact with irritant substances
Contact allergy
Aeroallergens
Microbic agents
Food (eggs, milk, fish)
Emotional stress
30
Pathogenesis and immunology
The pathogenesis of atopic dermatitis is unknown, but the disease seems to be the result of genetic susceptibility, immune dysfunction and epidermal barrier dysfunction
Genetic:
The concordance rate for AD is higher among monozygotic twins (77%) than among dizygotic twins (15%).
31
32
Pathogenesis and immunology
Elevated IgE and the inflammatory response:
The IgE level is increased in the serum of many patients with AD, but 20% of AD have normal serum IgE.
The level of IgE do not correlate with the activity of the disease; therefore elevated serum IgE levels can only be considered supporting evidence for the disease.
33
Blood eosinophilia:
Blood eosinophil counts correlate with disease severity; especially with severe AD and concomitant respiratory allergies.
Degranulation of eosinophils in the dermis may induce histamine release from basophils and mast cells and stimulate itching, irritaion.
Pathogenesis and immunology Immunology
Activation T helper cell type 2 (Th2).Th2 produces IL-4, 5, 10, and IL-13, and inhibition of the Th1 response.
IL-4 and IL-5 produce elevated IgE and eosinophilia in tissue and peripheral blood.
IL-10 inhibits delayed type hypersensitivity
Th2 maybe sensitive to house mites or grass pollen.
Immunology
Monocytes produces elevated amount of prostaglandin E2 (PGE2)
PGE2 reduces gamma-interferon production
PGE2 also directly enhances IgE production from B cells
Immunology
Langerhans cells of AD patient stimulate helper T cells into Th2 phenotype without the presence of antigenLangerhans cells have IgE bound to their surface receptors. These IgE are associated with atopic antigens, such as house dust mites
Criteria for diagnosis of AD
Major criteria: (must have three of the following)• Pruritus
• Typical morphology and distribution:
• flexural lichenification in adults;
• facial and extensor involvement in infancy.
• 3) Chronic or chronically relapsing dermatitis
• 4) Personal or family history of atopic disease (asthma, allergic rhinitis, AD)
37
38
Minor criteria:(must also have three of the following)
• Xerosis (dry skin)
• Ichthyosis\hyperlinear palms\keratosis pilaris
• IgE reactivity (immediate skin test reactivity, radioallergosorbent test positive)
• Elevated serum IgE
• Early age of onset
• Tendency for cutaneous infections ( S. aureus and herpes simplex virus)
• Tendency to nonspecific hand\foot dermatitis
• Nipple eczema
• Cheilitis(inflammation of the lips)
• Recurrent conjunctivitis
• Dennie-Morgan infraorbital fold
39
Minor criteria:(must also have three of the following)
12) Keratoconus (bilateral protrusion of the cornea)
13) Anterior subcapsular cataracts
14) Orbital darkening
15) Facial pallor\facial erythema
16) Pityriasis alba
17) Itch when sweating
18) Intolerance to wool and lipid solvents
19) Perifollicular accentuation
20) Food hypersensitivity
21) Course influenced by environmental and\or emotional factors
22) White dermographism or delayed blanch to cholinergic agents
40
• Treatment:
• 1-explanation, reassurance and encouragement.
• 2-the avoidance of exacerbating factors.
• 3-topical steroids. Principles are use weaker steroid that controls the eczema effectively; review their use regularly (check for local and systemic side-effects); avoid using potent and very potent steroids for children.
• 4-the regular use of bland emollients, either directly to the skin or in the form of oils to be used in the bath.
• 5-those with Ichthyosis should use ointments rather than creams.
41
• 6-the scratch-itch cycle can often be interrupted by occlusive bandaging, and nails should be kept short.
• 7-sedative antihistamines, e.g. trimeprazine or hydroxyzine.
• 8-systemic antibiotics, e.g. erythromycin.
• 9-systemic steroids for generalized and severe cases.
• 10- UVB, UVA or even PUVA therapy may be useful for severe cases.
Treatment:
Note the Dennie–Morgan lines and central facial pallor.
Keratosis pilaris
4445
46
47
48
49
Seborrhoeic dermatitis
It is chronic, characterized by redness, and scaling in the area with a rich supply of sebaceous glands, namely the scalp, face, upper trunk, and in the body folds.
Affects infancy (within the first months), and adults, most between 20-50 years old.
It is common occurring in 2-5% of the population.
50
Etiology
May be related to increased sebum secretion, abnormal sebum composition, certain drugs (arsenic, gold methyl-dopa, cimetidine, neuroleptics)May be related to the presence of the lipophilic yeast Malassezia furfur ( also known as Pityrosporum ovale).
The density of yeast has been correlated with the severity of the disease. P. ovale may also be abundant on the scalp of patients who have no clinical signs of the disease, and the yeast may only be pathogenic in predisposed individuals.
May be cutaneous marker of HIV infection and AIDS, especially when severe, atypical, and therapy resistant
51
Clinical features
• Infants (cradle cap): infants commonly develop a greasy adherent scale on the vertex of the scalp.• Young children (tinea amiantacea and blepharitis): one patch or several patches, range from 2-10 cm of dense scale appear anywhere on the scalp. The scale suggests fungal scalp disease, which explains the designation tinea. Amiantacea, meaning asbestos, refers to the platelike quality of the scale, which resembles genuine asbestos.
52
Clinical features
• 3) Adolescents and adults (classic seborrheic dermatitis):Dandruff (Pityriasis sicca): represents a mild form of seborrhoeic dermatitis: fine, dry, white scalp scaling with minor itching. The distribution of scaling and inflammation may become more diffuse and occur in the seborrheic area.
Scaling of the ears may be misjudged as eczema or fungus infection.
Older patients especially with neurologic problems tend to have more chronic and extensive disease.
53
Treatment
Topical steroids tend to produce a rapid effect, but on the face can produce steroid rosacea.Antiyeast medications: ketoconazole.
Oral antifungals. Oral itraconazole; 200mg\day.
54
55
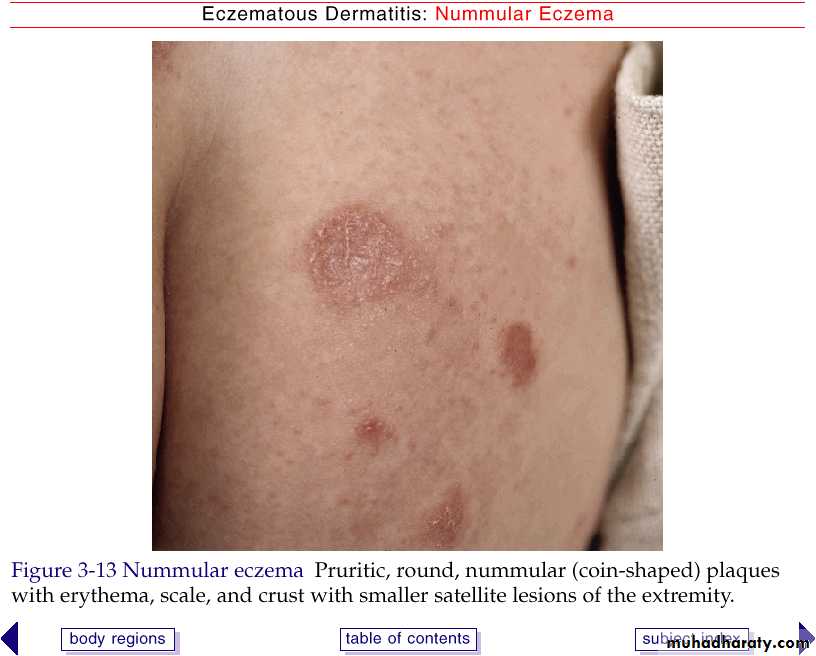
Discoid eczema(nummular eczema)
It is a chronic, pruritic, inflammatory dermatitis occurring in the form of coin-shaped plaques composed of grouped small papules and vesicles on an erythematous base. It is especially common on the extremities during winter months; often seen in atopic individuals.Usually begins on the lower legs, dorsa of the hands, or extensor surfaces of the arms.
Treatment: topical steroids; intralesional steroids
Systemis: AB if secondary infection present; antihistamines; corticosteroids.
56
57
Asteatotic eczema
Also known as xerotic eczema; winter itch; eczema craquelé; and asteatotic eczema. These terms are all applied to dehydrated skin showing redness, dry scaling, and fine crackling that may resemble crackled porcelain or the fissures in the bed of a dried lake or pond.favored sites are the anterior shins, extensor arms, and flank. Elderly persons are particularly predisposed, and xerosis appears to be the most common cause of pruritus.
seen most frequent during the winter, when there is low humidity. Bathing with hot water and harsh soaps contribute.
limitation of the use of soap, and prompt application of an emollient are usually effective.
58
59
Pityriasis alba
It is a form of subclinical dermatitis, frequently atopic in origin. It presents as poorly marginated, hypopigmented, slightly scaly patches on the cheeks, upper arms, and trunk, typically in young children. Exposure to the sun makes the patches more obvious. It usually responds to emollients and mild topical steroids.60
61
Acute vesiculobullous hand eczema (pompholyx, dyshidrosis)
Idiopathic acute vesicular hand dermatitis is not related to blockage of sweat duct.Primary lesions are macroscopic, deep-seated multilocular vesicles resembling tapioca on the sides of the fingers, palms, and soles.
The eruption is symmetrical and pruritic, with pruritus often preceding the eruption.
62
63
Venous eczema
Also known as gravitational eczema (stasis eczema).It is a cutaneous marker for venous insufficiency.
Presents as erythema and a yellowish or light-brown pigmentation of the lower third of the lower legs.
Varicose veins are usually present .
64
65
Juvenile plantar dermatosis
It is eczematous disorder of children.The disease is caused by the repeated maceration of the feet by occlusive shoes, especially athletic shoes.
It usually begins as a patchy, symmetrical, smooth, red glazed macules on the base or medial surface of the great toes, sometimes with fissuring and desquamation.
66
67
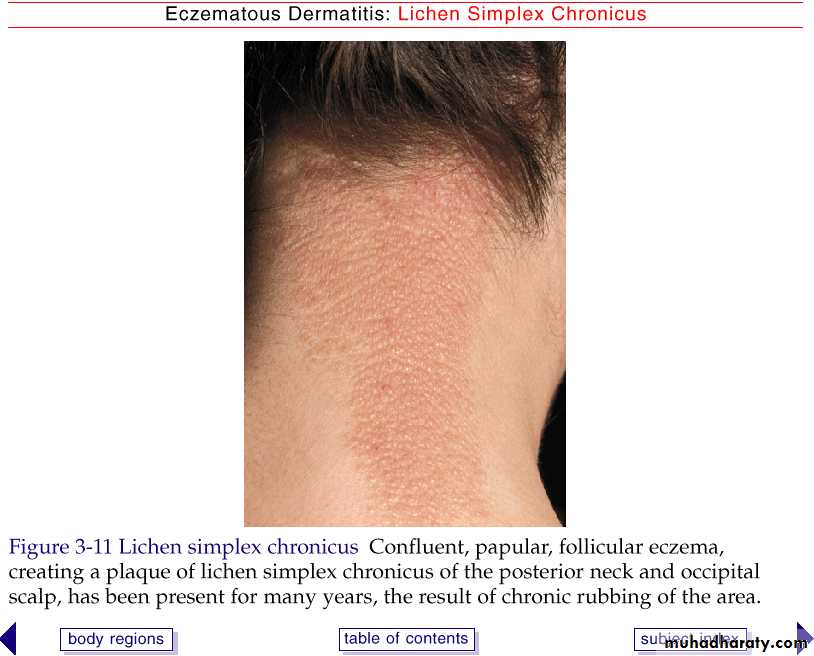
Lichenification: lichen simplex (localized neurodermatitis)
As a result of long continued rubbing and scratching, the skin becomes thickened and leathery. The normal markings of the skin become exaggerated. This change, known as lichenification. Ex. lichen simplex .lichen simplex: it is an eczematous eruption that is created by habitual scratching of a single localized area.
The disease has a predilection for the back and sides of the neck, and the extremities-especially the wrists and ankles.
68
69