د. خالد امراض 29\3\2018
عدد الاوراق ( 6 ) م\3\موصل lec:1THE LIVER
General features.liver weighs 1500g, functions as station between splanchnic & systemic circulations to maintain body’s metabolic homeostasis through -processing dietary carbohydrates, amino acids, lipids, & vitamins -removal of microbes & toxins in splanchnic to systemic circulation -synthesis of plasma proteins -detoxification & excretion of waste products & pollutant xenobiotics
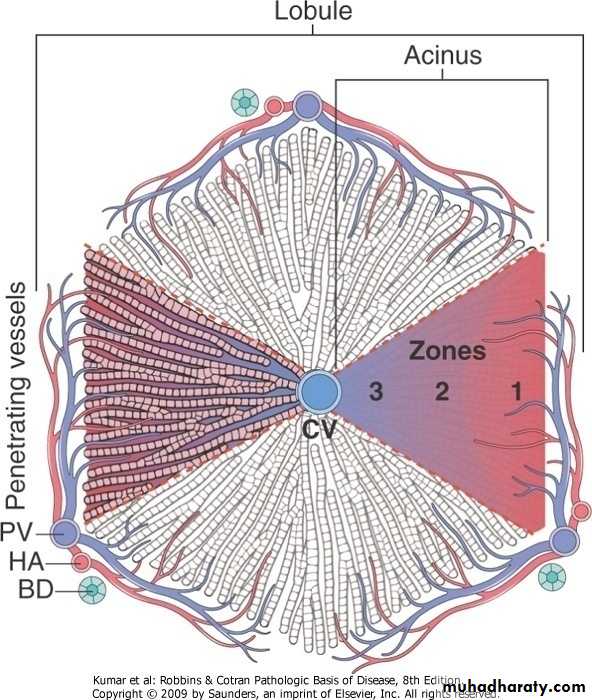
Liver, microarchitecture
General Features of Hepatic DiseaseLABORATORY EVALUATION OF LIVER DISEASEmost common.hepatocyte integrity. -(AST, ALT) .biliary excretory function. -substances secreted in bile .(serum bilirubin) -plasma membrane enzymes .(serum alkaline phosphatase).hepatocyte function -(serum albumin, prothrombin time)
TYPES OF LIVER DISEASES.metabolic.toxic.microbial.circulatory.neoplastic PATTERNS OF HEPATIC INJURY
.degeneration & intracellular accumulations
.cell death
.inflammation
.regeneration
.fibrosis
HEPATIC FAILURE.results from -acute liver injury (massive hepatic necrosis) .drugs (acetaminophen) .toxins (carbon tetrachloride, mushroom) .hepatitis (infection, autoimmune) mechanisms of injury -direct toxic damage -combined toxicity & immune mediated -chronic liver disease (chronic hepatitis> cirrhosis) -hepatic dysfunction without overt necrosis (tetracycline,Reye syndrome,fatty liver in pregnancy)
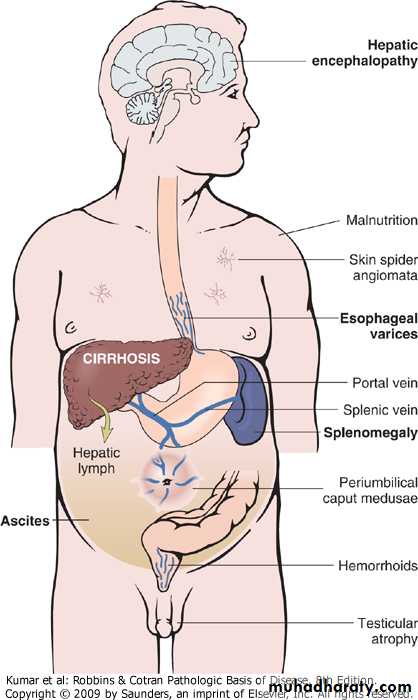
.clinical features -jaundice -coagulopathy -hypoalbuminemia>edema -hyperestrogenemia>palmar erythema, hypogonadism, gynecomastia -failure of multiple organ systems -hyperammonemia>encephalopathy .complications -hepatic encephalopathy -hepatorenal syndrome (renal failure) -hepatopulmonary syndrome
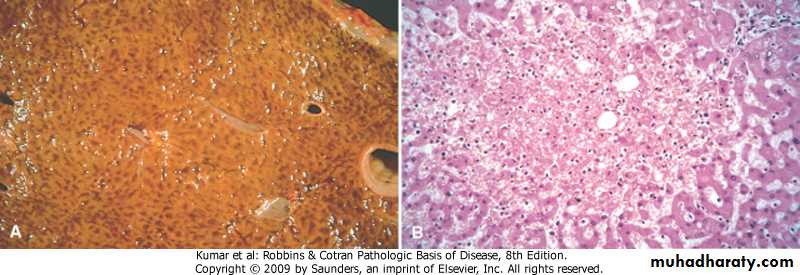
CIRRHOSIS
defined by 3 characteristics
-bridging fibrous septae
-parenchymal nodules
-diffuse disruption of architecture
Cirrhosis is among the top 10 causes of death in the Western world.
Liver failure in chronic liver disease is most often associated with cirrhosis.
However, not all cirrhosis leads inexorably to chronic liver failure and not all end-stage chronic liver disease is cirrhotic.
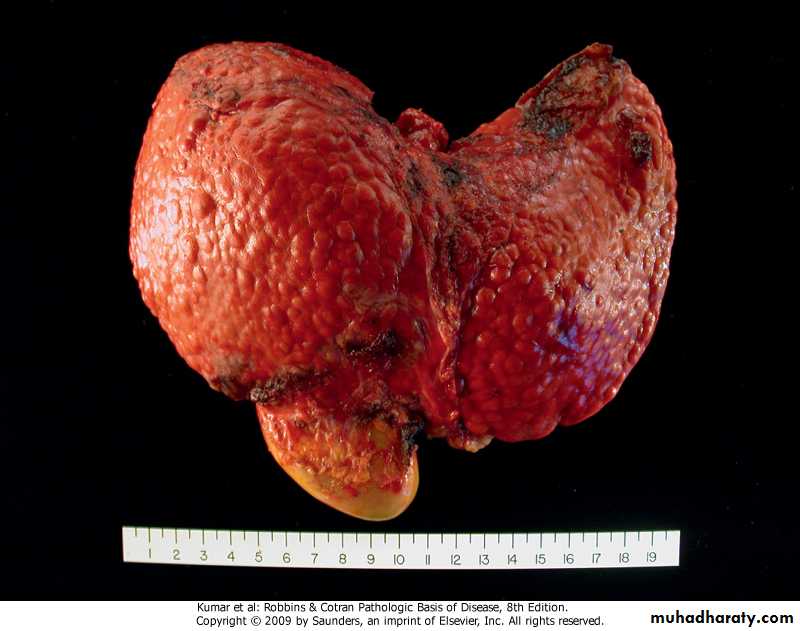
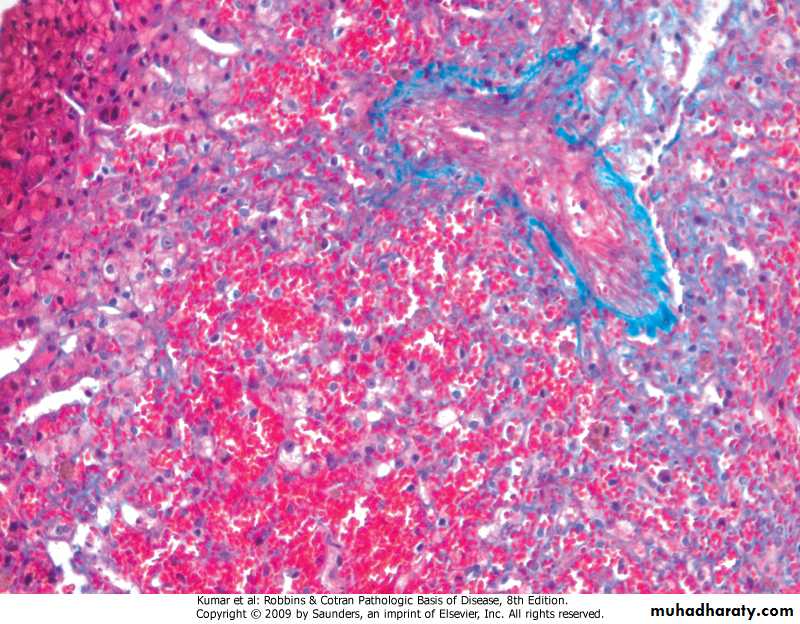
Cirrhosis
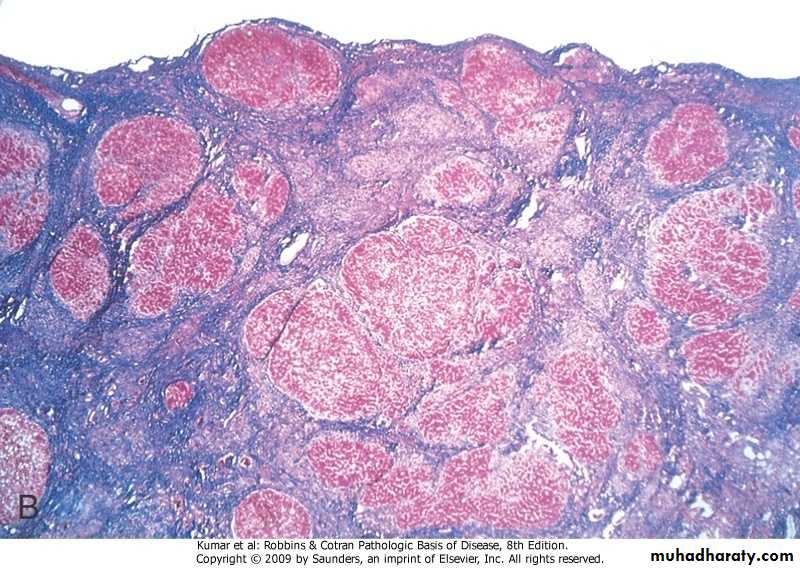
Cirrhosis, Masson trichrome
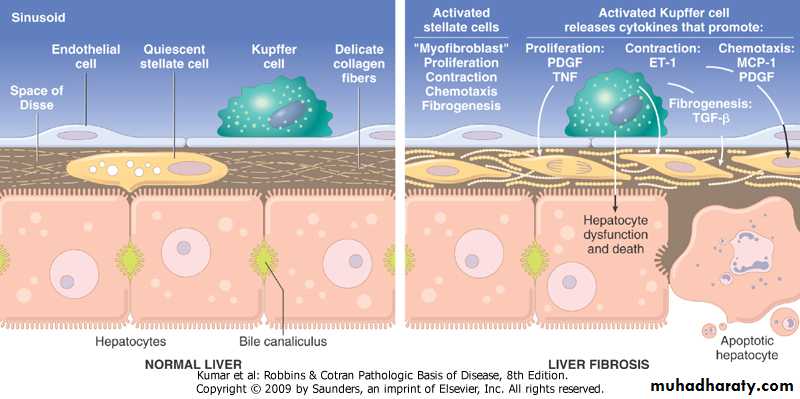
.classification -the best is based on presumed etiology .excessive alcoholic consumption .nonalcoholic steatohepatitis (NASH), .autoimmune diseases. . Chronic viral hepatitis .biliary diseases .primary hemochromatosis .Wilson disease .α-1 antitrypsin deficiency .cryptogenic .pathogenesis -death of hepatocytes -extracellular matrix (ECM) deposition (fibrosis) mediated mainly by stellate cells and Kuppfer cells -nodular regeneration of surviving hepatocytes -vascular reorganizationCirrhosis, pathogenesis
.clinical features-asymptomatic
-non-specific (anorexia, weight loss, weakness)
-hepatic failure
-ultimate cause of death
.progressive liver failure
.portal hypertension
.hepatocellular carcinoma
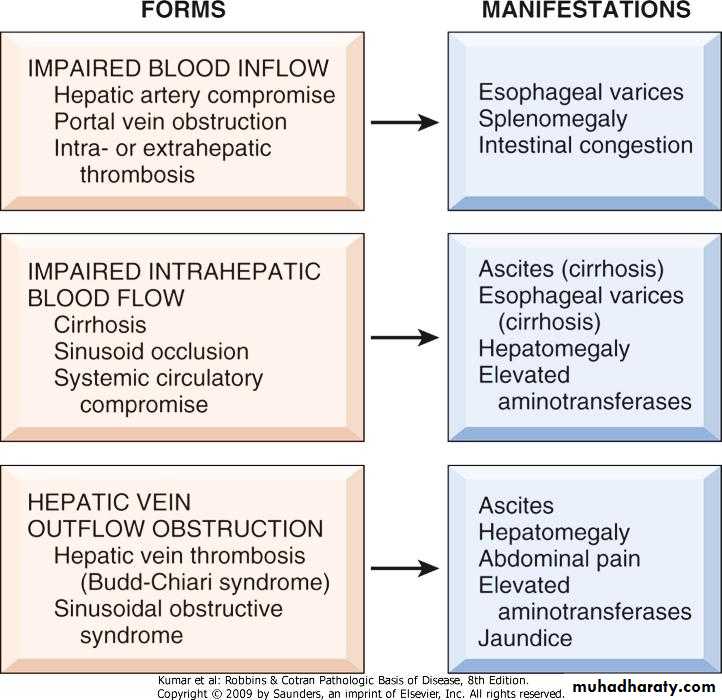
PORTAL HYPERTENSIION
Increased resistance to portal blood flow may develop from prehepatic, intrahepatic, and posthepatic causes.pre-hepatic, (thrombosis, portal vein narrowing, massive splenomegaly)
.intra-hepatic, (cirrhosis, schistosomiasis,
sarcoidosis, massive fatty change, diseases of portal microcircultion)
.post-hepatic, (severe right-sided heart failure, constrictive pericarditis, hepatic vein outflow obstruction)
.pathophysiology -increased resistance to portal flow at level of sinusoids .contraction of vascular smooth muscle cells & myofibroblasts .disruption of blood flow by scarring & parenchymal nodules -increase in portal venous blood flow .arterial vasodilation in the splanchnic circulation
Clinical consequences of portal hypertension
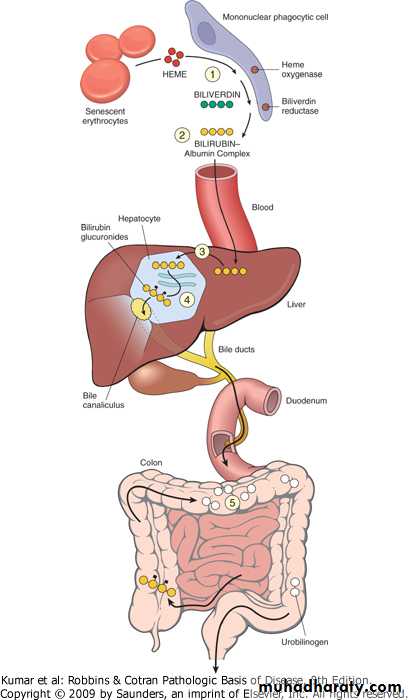
JAUNDICE Jaundice .yellow discoloration of skinIcterus.yellow discoloration of scleraJaundice and Icterus occur when systemic retention of bilirubin produces serum levels above 2.0 mg/dL (the normal level in adults is below 1.2 mg/dL)..pathophysiology of jaundice -disequilibrium between bilirubin production & clearance due to: .excessive production of bilirubin (hemolytic anemias, ineffective erythro- poiesis, resorption of blood from internal hemorrhage) .reduced hepatocytes uptake (drugs, genetic) .impaired bilirubin conjugation (genetic, physiologic, diffuse liver disease) .decreased hepatocellular excretion (genetic) .impaired bile flow (obstruction)
Neonatal Jaundice (physiologic jaundice of the newborn) .almost every newborn has transient & mild unconjugated hyperbilirubinemia.exacerbated by breastfeeding, due to presence of bilirubin-deconjugating enzymes in breast milk Hereditary Hyperbilirubinemias.uncojugated hyperbilirubinemia -Crigler-Najjar syndrome type I (UGT1A1 is completely absent) -Crigler-Najjar syndrome type II (UGT1A1 is greatly reduced) -Gilbert syndrome (UGT1A1 is 30%).conjugated hyperbilirubinemia -Dubin-Johnson syndrome (defect in excretion of bilirubin glucuronides) -Rotor syndrome (defects in uptake & excretion of bilirubin pigments)
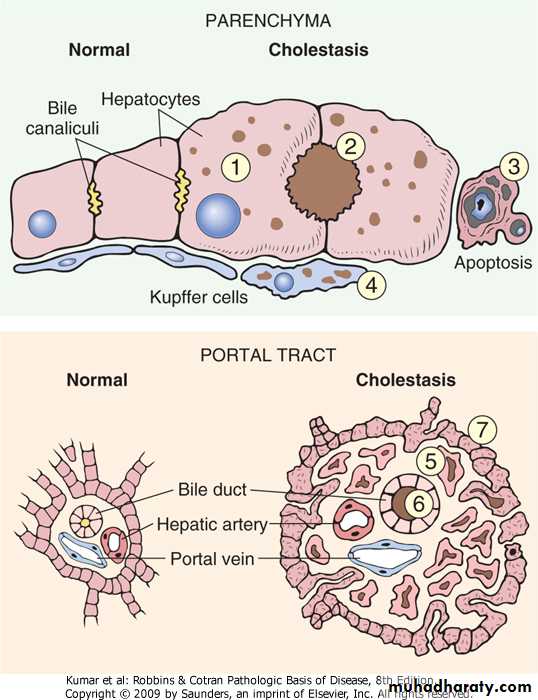
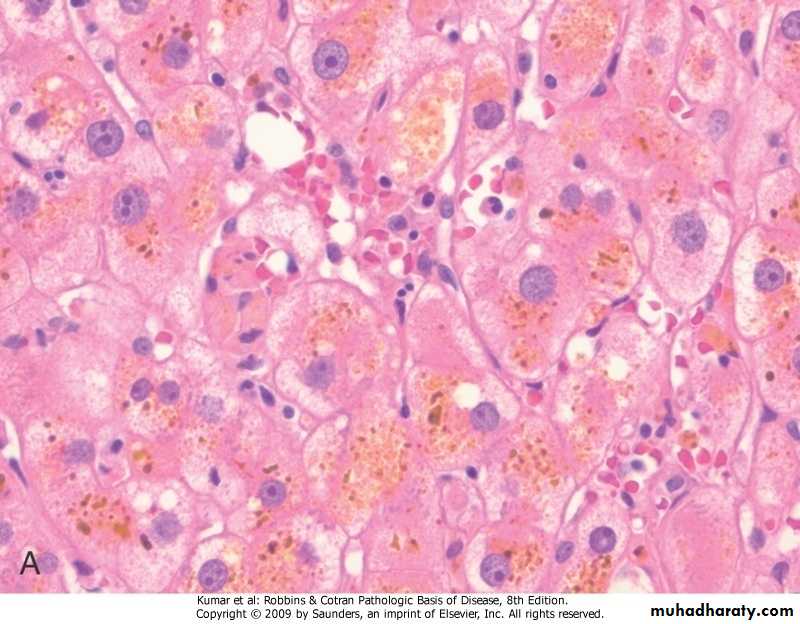
CHOLESTASIS.systemic retention of bilirubin & other solutes eliminated in bile .clinical features (jaundice, pruritis, skin xanthomas, malabsorption syndrome).results from impaired bile flow dueto -defects in hepatocyte bile secretion -biliary obstruction .characteristic laboratory finding is elevated serum alkaline phosphatase
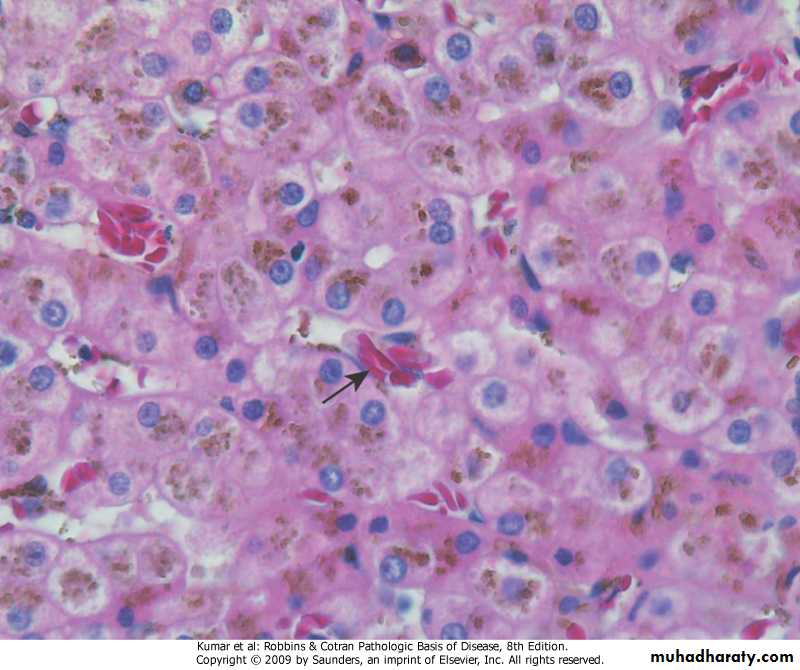
Morphologic features of cholestasis
Liver, intracellular cholestasis
Bile caniliculi cholestasis, bile plug
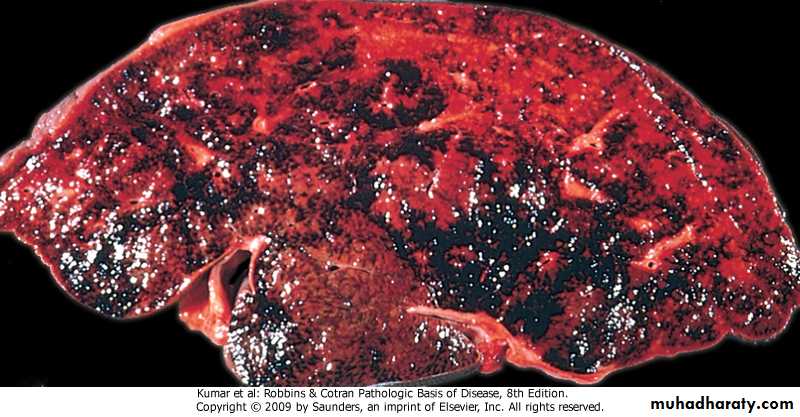
Hepatic Circulatory DisordersLiver infarcts, impaired blood inflow
Sickle cell anemia, impaired intrahepatic blood flow
System circulatory compromise, impaired intrahepatic blood flow
Budd-chiari syndrome, hepatic vein outflow obstruction
Sinusoidal obstructive syndrome, hepatic vein outflow obstruction
Drug And Toxin-Induced Liver Disease
.general features -genetic variability is a critical factor -injury of hepatocytes or biliary epithelium causing cell death or disruption of cellular function may result -from direct toxicity -through hepatic conversion of a xenobiotic to an active toxin -through immune mechanisms, usually by a drug or a metabolite acting as a hapten
.mechanisms
-predictable, occurs in anyone who receives sufficient dose of an agent
-unpredictable (idiosyncratic), depends on .rate of metabolism of the agent
.intensity of immune response
.morphology -hepatocyte necrosis -cholestasis -chronic hepatitis -micro & macrovesicular steatosis
.clinically & histologically is similar to chronic viral hepatitis, distinction is made by serology.recovery upon removal of the drug LIVER TRANSPLANTION
.liver transplantation is aiming -to restore health -to improve survival .Posttransplantation survival at 5 years is 65%-78% -immunosuppressive therapy -surgical techniquesTypes of donors
.non-heart beating donor (majority)
-full size liver (adult)
-split liver
.left lateral segment (child)
.rest of liver (adult)
.living donor
-partial hepatectomy
.left lateral segment (child)
.right lobe (adult)
Who needs a liver transplant?
.acute/subacute liver failure
.chronic liver failure
.hepatocellular carcinoma
.surgical gene therapy
Complications .immunosuppression -infection (local and systemic) -direct side effects on body organs -malignancy (late) .liver parenchyma -non-functioning liver -rejection -ischemic-reperfusion injury -anastomotic complications -bile leak -recurrence of disease (late)