Osteomyelitis & inflammatory bone diseases
1جراحه فم نظري / رابع اسنان كركوك
د.نجاه
24/4/2018
426
Osteomyelitis & inflammatory bone diseases
Osteomyelitis of the jaws: is an infectious disease with complicated course, involving multiple surgical interventions and sometimes leading to facial disfigurement as a result of loss of affected bone and teeth and the accompanying scarring.2
The incidence of osteomyelitis is much higher in the mandible due to the dense poorly vascularized cortical plates and the blood supply primarily from the inferior alveolar neurovacular bundle. It is much less common in the maxilla due to the excellent blood supply from multiple nutrient feeder vessels. In addition the maxillary bone is much less dense than the mandible.
3
Diminished host defenses, both local and systemic, can contribute significantly to the emergence and clinical course of the disease.
Osteomyelitis has been associated with multiple systemic diseases including :
• diabetes,
• autoimmune states,
• malignancies,
• malnutrition,
• and acquired immunodeficiency syndrome.
• The medications linked to osteomyelitis are steroids, chemotherapeutic agents, and bisphosphonates
4
Local conditions that adversely affect the blood supply can also predispose to a bony infection.
• Radiation therapy,
• osteopetrosis,
• and bone pathology can alter the blood supply to the area and cause
5
Pathogenesis :
In the maxillofacial region, osteomyelitis primarily occurs as a result of contiguous spread of odontogenic infections or as a result of trauma. It is initiated by an inoculation of bacteria into the jaw bones. This can occur with the extraction of teeth, root canal therapy, or fractures of the maxilla or mandible. This initial insult results in a bacteria-induced inflammatory process. With inflammation there is hyperemia and increased blood flow to the affected area. Additional leukocytes are present in the area to fight off infection6
Pus is formed , when the pus and subsequent inflammatory response occur in the bone marrow, an elevated intramedullary pressure is created which further decreases the blood supply to this region. The pus can travel via haversian and Volkmann's canals to spread throughout the medullary and cortical bones. Once the pus has perforated the cortical bone and Collects under the periosteum, the periosteal blood supply is compromised and this further aggravates the local condition. The end point occurs when the pus exits the soft tissues either by intraoral or extraoral fistulas.
7
Microbiology
More than 500 bacteria have been identified in the mouth. In the past, staphylococcal species were considered the major pathogen in osteomyelitis of the jaws disease-causing organisms. As with most oral infections the prime pathogenic species are streptococci and anaerobic bacteria. The anaerobes are bacteroides gram -ve or peptostreptococci species(gram +ve anaerobic). Often, the infections are mixed, growing several pathogens on final culture like fusobacterium spp and actinomyces spp. Antibiotic treatment based on the most likely pathogens. This could include penicillin and metronidazole as dual-drug therapy or clindamycin as a single-drug treatment.8
Classification
Osteomyelitis is divided into acute or chronic forms based on the presence of the disease for a one month duration.1. Acute osteomyelitis
a. Contiguous focus
b. Progressive
c. Hematogenous
9
• 2. Chronic osteomyelitis
• a. Recurrent multifocal (moth eaten bone )• b. Garre's
• c . Suppurative or nonsuppurative
• d. Sclerosing
10
Clinical Presentation
the patient with osteomyelitis of the maxillofacial region will present with classic symptoms:• Pain
• Swelling and erythema of overlying tissues
• Adenopathy
• Fever
• Paresthesia of the inferior alveolar nerve
• Trismus
• Malaise
• Fistulas
11
The pain in osteomyelitis is often described as a deep and boring pain, In acute osteomyelitis it is very common to see swelling and erythema of the overlying tissues, which are indicative of the cellulitis phase of the inflammatory process of the underlying bone. Fever often accompanies acute osteomyelitis, where as it is relatively rare in chronic osteomyelitis. Paresthesia of the inferior alveolar nerve is a classic sign of a pressure on the inferior alveolar nerve from the inflammatory process within the medullary bone of the mandible. Trismus may be present if there is inflammatory response in the muscles of mastication of the maxillofacial region.
12
The patient commonly has malaise and fatigue. Lastly both intraoral and extraoral fistulas are generally present with the chronic phase of osteomyelitis of the maxillofacial region. Often these patients will have laboratory work-up as part of their initial examination. In the acute phase of osteomyelitis it is common to see a leukocytosis which is relatively uncommon in the chronic phases of osteomyelitis.
The patient may have an elevated erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP). Both the ESR and CRP are very sensitive but non-specific.
13
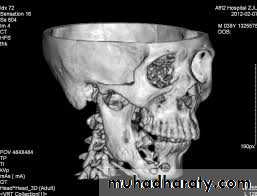
Radiographical appearance ;
It is possible to see a patient with acute osteomyelitis that has a normal-appearing orthopantomogram. However, one can often see the appearance of "moth-eaten" bone or sequestrum of bone, which is the classic appearance of osteomyelitis.14
Computerized tomography (CT) scans have become the standard in evaluating maxillofacial pathology such as osteomyelitis. its sensitive in late stage when 30%-50% of the bone demineralized.
15
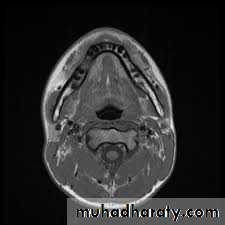
Magnetic resonance imaging (MRI) : is generally considered more valuable in the evaluation of soft tissue lesions of the maxillofacial region. However, MRI can assist in the early diagnosis of osteomyelitis by loss of the marrow signal before cortical erosion or sequestrum of the bone appears. Thus, MRI may benefit in identifying the earlier stages of osteomyelitis.
16
Nuclear medicine has evolved to aid in the diagnosis of osteomyelitis. The technetium 99 is very sensitive in highlighting areas of increased bone turnover.
17
Treatment
The first step in the treatment of osteomyelitis is diagnosing the condition correctly. The diagnosis is made from clinical evaluation, radiographic evaluation, and tissue diagnosis. Tissues from the affected site should be sent for Gram stain, culture, sensitivity, and histopathologic evaluations. The clinical response to the treatment of any patient will be compromised unless altered host factors can be optimized.18
Medical evaluation and management in defining and treating any immunocompromised state is indicated and often helpful. For example, glucose control in a diabetic patient should be stabilized for best response to therapy. Antibiotic therapy used according to the sensitivity
19
Surgical treatment
Classic treatment is:
1. sequestrectomy and saucerization. The aim is to debride the necrotic or poorly vascularized bony sequestra in the infected area and improve blood flow.
2. Saucerization involves the removal of the adjacent bony cortices and open packing to permit healing by secondary intention after the infected bone has been removed.
20
3.Decortication involves removal of the dense, often chronically infected and poorly vascularized bony cortex and placement of the vascular periosteum adjacent to medullary bone to allow increased blood flow and healing in the affected area.
4.Hyperbaric oxygen (HBO) treatment has also been advocated for the treatment osteomyelitis.
21
Osteoradionecrosis
Radiation therapy is a valuable treatment modality in treating cancer of the maxillofacial region. Radiation therapy can be used alone or as adjunctive therapy in combination with surgery and chemotherapy. Radiation therapy like any treatment modality has side effects, including mucositis and xerostomia. One of the most important side effects is osteoradionecrosis (ORN). ORN is generally caused by trauma to the radiated area, usually by dental extraction, but it can also occur spontaneously.22
The clinical picture of ORN is most commonly seen with pain and exposed bone in the maxillofacial region ORN is more common in the mandible than in the maxilla . A dosage of radiation above 5,000 to 6,000 rads is generally felt to make the mandible susceptible to ORN. Radiographically, the appearance on the orthopantomogram or CT scan resembles conventional osteomyelitis with areas of osteolysis and bony sequestrum. Often there is an appearance of moth-eaten bone present on these films: treatment of ORN is aimed at removing the nonviable (necrotic) tissue and allowing the body to heal itself. Minor debridements of exposed bone and Current therapy of HBO consists of 100% oxygen delivered in a pressurized manner.
23
Osteochemonecrosis
In the recent years bisphosphonate therapy has become a widely accepted therapy in various clinical settings such as multiple myeloma, metastatic cancer therapy, and treatment of advanced osteoporosis. With the increased prescription of these drugs, the incidence and prevalence of bisphosphonate-associated complications of the jaw continues to be increased. This seems to be even more the case in patients receiving injectable bisphosphonates, such as pamidronate and zoledronic acid.
24
The pathophysiological mechanisms leading to bisphosphonate-induced osteochemonecrosis of the jaws are differes from osteoradionecrosis ,In bisphosphonate-induced osteochemonecrosis of the jaws osteoclastic action is reduced but osteoblastic production continues leading to an osteopetrosis like condition . These alterations in bone physiology with eventual increase of the medullary bone as the disease progresses and the inability of osteoclasts to remove superinfected "diseased" bone are regarded as causative factors. In contrast to osteoradionecrosis, where a radiation-induced avascular necrosis is the major cause, avascularity does not appear to be a major cofactor .
25