Pediatrics
NEUROLOGY
1
L.4 Dr.Roua Al yaseen
Central Nervous System Infections
Viral infections of the CNS are much more common than bacterial infections,
which, in turn, are more common than fungal and parasitic infections.
Meningitis: means primary involvement of the meninges.
Encephalitis: indicates brain parenchymal involvement.
Meningoencephalitis: involvement of both.
Brain abscess is the best example of a focal infection of the CNS.
Etiology
1- In the neonatal period (0–28 days): Groups B streptococci,E.
coli,Klebsiella, Listeria monocytogenes
2- Infants & children (2 mo to 12 yr of age
N. meningitidis, then S. pneumoniae, and H. influenzae type b
3- Those with underlying immunologic or anatomic (splenic dysfunction,
cochlear defects or implants) disorders increase the risk of meningitis from less
common pathogens such as Pseudomonas aeruginosa, Staphylococcus aureus,
coagulase-negative staphylococci, Salmonella spp., and Listeria
monocytogenes.
Epidemiology
The major risk factors for meningitis include:
1- Young age (neonats & young infants).
2- Recent colonization with pathogenic bacteria paranasal sinusitis, otitis media,
mastoiditis, orbital cellulitis, penetrating cranial trauma, dermal sinus tracts, or
meningomyeloceles..
3- Close contact (household, daycare centers) with individuals having disease
transmission through respiratory tract secretions or droplets.
4- Poverty, and male gender.
5- infants and young children with occult bacteremia.
A Acute Bacterial Meningitis
Pediatrics
NEUROLOGY
2
6- Specific host defense defects like
a) Complement system (C5–C8) defect
recurrent meningococcal infection.
b) Defects of the properdin system
lethal meningococcal disease.
c) Splenic dysfunction (sickle cell anemia) or asplenia
pneumococcal.
8- Those with meningomyelocele
staphylococcal
9- Those with CSF shunt
coagulase-negative staphylococci.
Pathology & pathophysiology :
Damage to the cerebral cortex occurs due to vascular occlusion ,hypoxia,
bacterial invasion , toxic encephalopathy , elevated ICP, ventriculitis, and
subdural effusions.
Vascular and parenchymal cerebral changes will occur result in vasculitis, ,
thrombosis of small cortical veins, occlusion of major venous sinuses,
necrotizing arteritis producing subarachnoid hemorrhage.
Cerebral infarction, resulting from vascular occlusion due to inflammation,
vasospasm, and thrombosis.
Inflammation of spinal nerves and roots produces meningeal signs, and
inflammation of the cranial nerves produces cranial neuropathies of optic,
oculomotor, facial, and auditory nerves
↑ CSF protein may be due to ↑ vascular permeability of blood brain barrier
with loss of albumin-rich fluid; whereas ↓ CSF glucose is due to ↓ glucose
transport by the cerebral tissue.
Increase Intracranial Pressure (ICP) by several
mechanisms include:-
1. Cerebral edema; it is due to cytotoxic, vasogenic or interstitial edema.
2. Hydrocephalus; it is mainly communicating HC due to adhesion of the
arachnoid villi.
3. SIADH (syndrome of inappropriate antidiuretic hormone secretion).
Pediatrics
NEUROLOGY
3
4. Subdural effusion
The onset is either sudden or insidious.
Sudden onset
: is less common manifestation & associated with rapidly
progressive manifestations of shock, purpura, DIC, and ↓ consciousness which
often progress to coma or death within 24 hr.
Insidious onset
: is more common & manifested as nonspecific findings e.g.
fever, headache, anorexia, photophobia, poor feeding, myalgia, arthralgia,
tachycardia, hypotension, & skin rash e.g. petechiae , purpura
Signs of meningeal irritation include nuchal rigidity, back pain, Kernig sign
and Brudzinski sign. In children younger than 12–18 mo, Kernig and
Brudzinski signs are not consistently present.
In infants, there is bulging fontanel & diastasis (widening) of sutures.
Signs of Increased ICP include:
headache, nausea, vomiting, cranial
nerve palsy (especially the abducent & oculomotor); severe cases causing
Cushing triad
which include hypertension, bradycardia, & irregular respiration
(apnea or hyperventilation).
Other signs include: papilledema, decorticate or decerebrate posturing, stupor,
coma, or signs of herniation.
Seizures (focal or generalized) due to cerebritis, infarction, or electrolyte
disturbances occur in 20–30% of patients with meningitis.
Alterations of mental status
Clinical manifestations
Pediatrics
NEUROLOGY
4
Investigations:
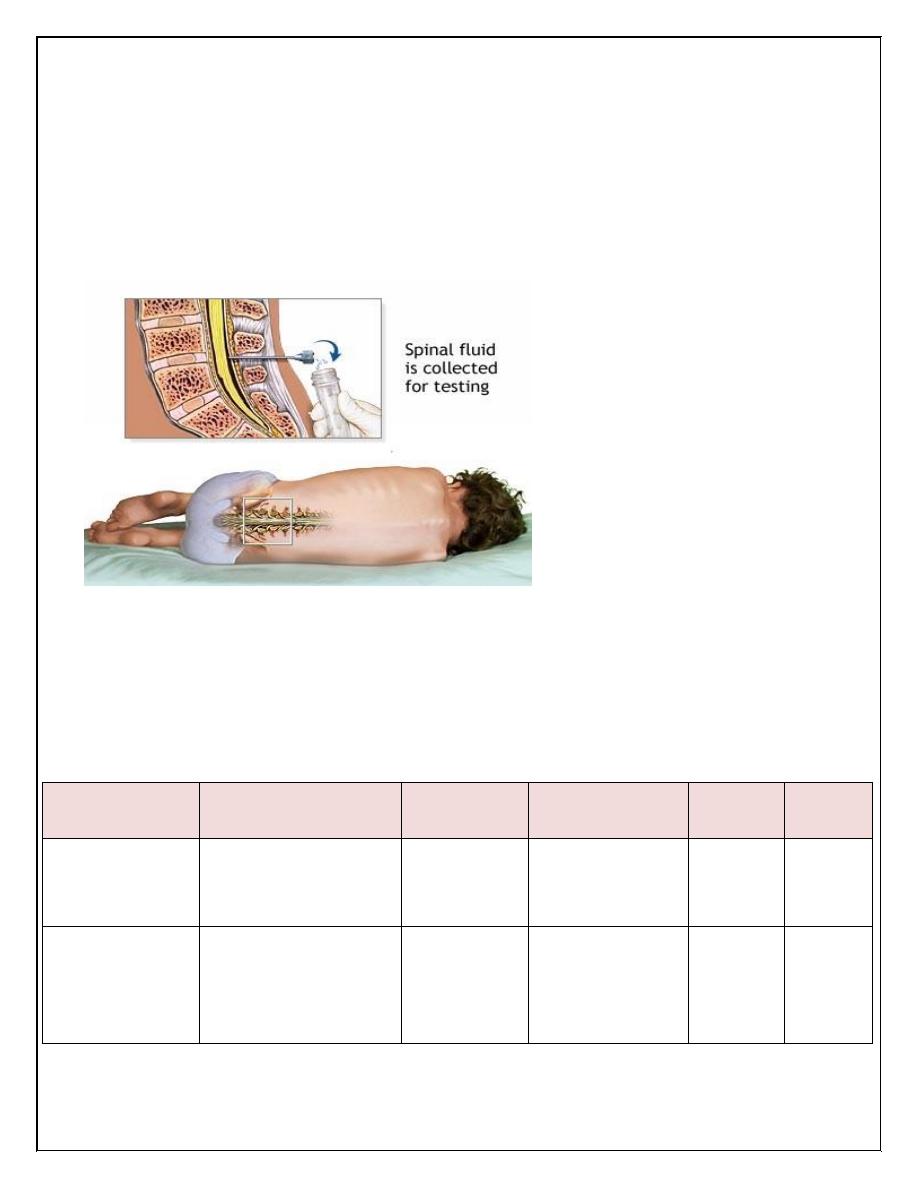
1-Lumbar puncture(LP) & cerebrospinal fluid(CSF) examination :
During LP, the patient is placed in the lateral position, but sick neonates should
be placed in upright position. The ideal interspace for LP is L3-L4 or L4-L5
which determined by drawing horizontal line from one anterior superior iliac
spine to the other.
CSF should be sent for
G-stain, culture, & biochemistry( protein, sugar ,WBC &
differential).
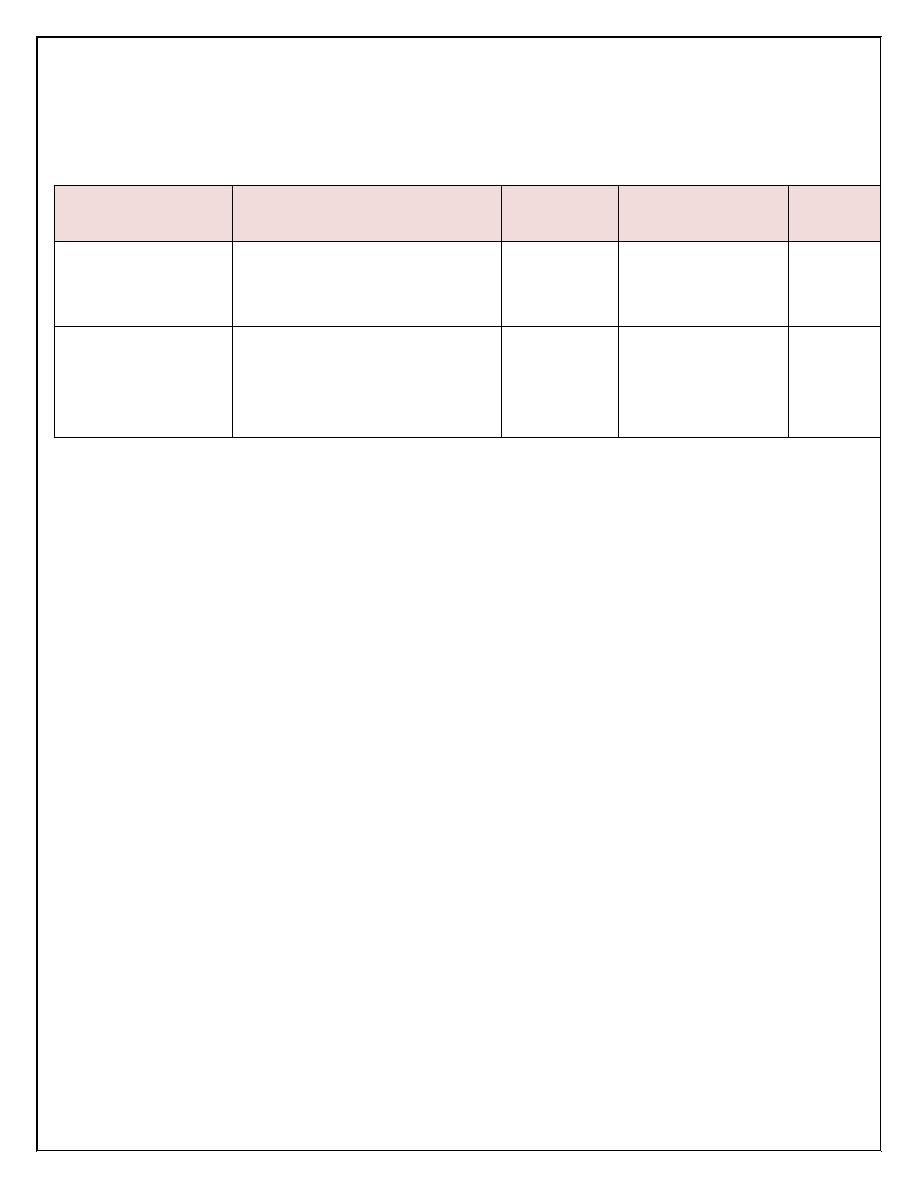
Normal value of CSF analysis:
age
WBC(mm
3
)
Protein
(mg/dl)
Glucose(mg/dl) Pressure
(mmH
2
o)
colour
Infant&
Older children
lymphocytes
5
neutrophiles Nill
20-45
60% of blood
glucose
50-80 clear
Neonates
(0-28days)
15-20,lymphocyte
predominate
120
60% of blood
glucose
Pediatrics
NEUROLOGY
5
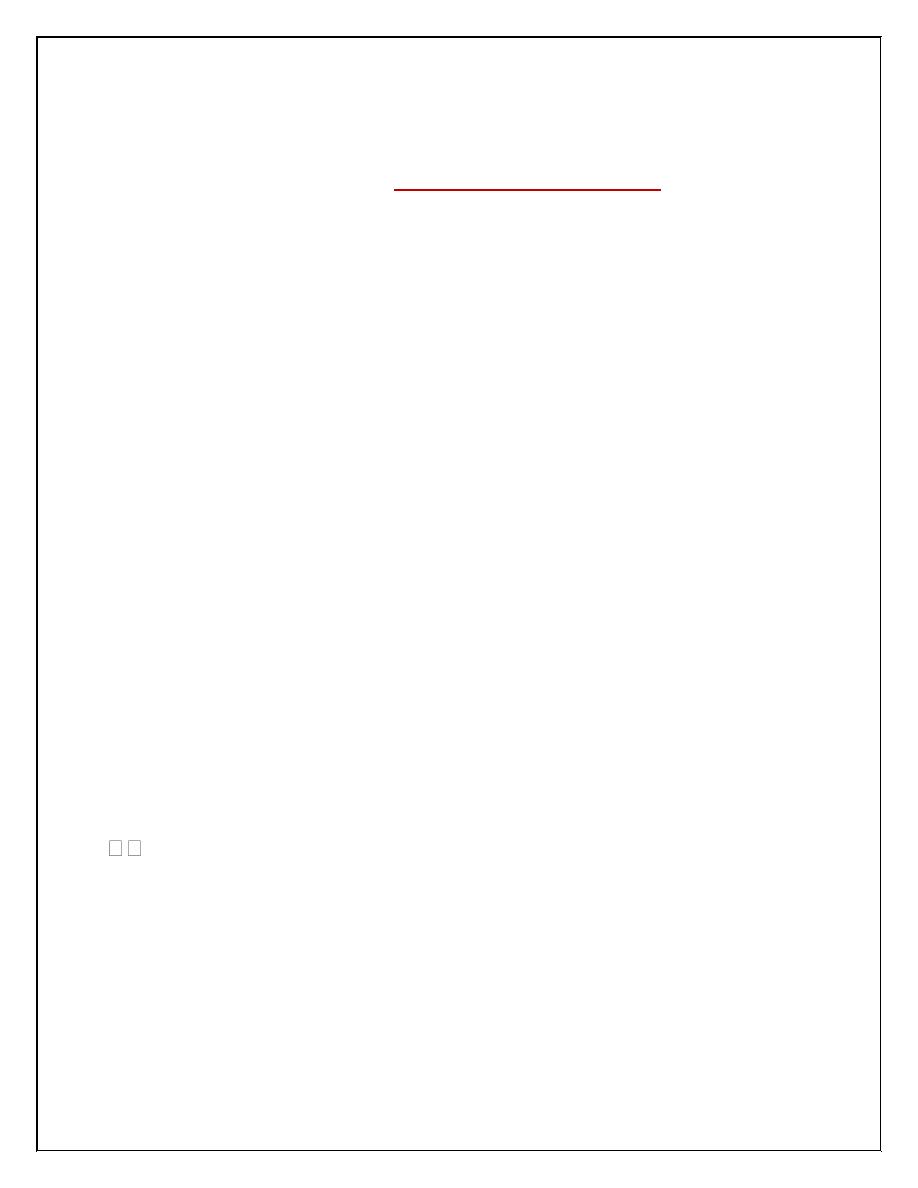
CSF findings in CNS infections
PMN (polymorphonuclear neutrophiles),
-Turbid CSF is present when the CSF leukocyte count exceeds 200–400/mm
3
.
-The Gram stain is positive in 70–90% of patients with untreated bacterial
meningitis.
The analysis of CSF obtained from children already receiving antibiotics
(partially treated meningitis), was negative on Gram stain and culture.
Neutrophilic Pleocytosis, elevated protein level, and a reduced concentration of
CSF glucose usually not affected.
Bacterial antigen may be detected in the CSF by agglutination test.
-Bloody CSF indicated either traumatic LP or subarachenoid hemorrhage& these
differentiated by centrifuged the CSF, if traumatic it become clear, but if
hemorrhage it remain xanthochromic.
Note : In traumatic CSF, WBC count & protein are affected, but G-stain, culture
& glucose level not influenced.
-CSF sent also for
:
Lactate & LDH which may be high in bacterial meningitis while
normal in aseptic meningitis.
WBC(mm
3
)
Protein
(mg/dl)
Glucose(mg/dl) Pressure
(mmH
2
o)
Acute bacterial
meningitis
100-10,000 PMN
Predominate(75-95%)
100-500
Decrease
(
60% of
blood glucose)
Usually
elevated
Viral meningitis
or
encephalitis
Rarely
1000,PMN early
but lymphocyte
predominate later
Normal or
Slightly
elevated
(50-200)
Normal
Normal
Pediatrics
NEUROLOGY
6
LP should be performed whenever bacterial meningitis is
suspected, but there are some
CONTRAINDICATIONS
for (immediate)
LP include:-
1. Evidence of ↑ ICP e.g. ↓ consciousness, cranial nerve palsies, Cushing
triad, papilledema; whereas bulging fontanel alone in infants is not a
contraindication.
2. Severe cardiopulmonary compromise e.g. shock that require prompt
resuscitation.
3. Infection of skin that overlying the site of LP.
4. Thrombocytopenia is a relative contraindication for LP.
2.Blood culture When LP is delayed, Blood culture should be taken (which
is +ve in 80- 90% of cases), then empirical antibiotic therapy can be
initiated.
3.CT scan for evidence of a brain abscess or increased ICP should not delay
therapy. LP may be performed later on after ↑ ICP has been treated.
4.CRP, ESR, and procalcitonin have been used to differentiate bacterial
(usually elevated) from viral causes of meningitis.
Other investigations may include: CBP, blood urea, serum electrolytes, urine
for specific gravity (for SIADH), & tests of coagulation function if there is
evidence of DIC.
Treatment.
It consists of supportive care & antibiotic therapy.
Supportive Care include:-
1. Repeated medical and neurologic assessments especially in the 1st 72
hr e.g. chart for vital signs, fluid input & urine output, pupillary
reflexes, level of consciousness…etc.
2. Patients should initially receive nothing by mouth. Shock should be
treated with fluid resuscitation +/_ inotropic agents; whereas if there is
no hypotension, IV fluid should be restricted to half or two thirds of
Pediatrics
NEUROLOGY
7
maintenance until it can be established that ↑ ICP or SIADH is not
present, then full maintenance can be given.
3. ↑ ICP can be treated by: head elevation, restriction of IV fluid,
furosemide (1 mg/kg) or mannitol , and endotracheal intubation with
hyperventilation. Glycerol has also been used to ↓ cerebral edema by ↑
plasma osmolality & enhance cerebral circulation.
4. Seizures should be treated with IV diazepam (0. 3 mg/kg/dose) or
lorazepam ; for maintenance Treatment of seizures, give phenytoin
which is better than phenobarbital because it produces less CNS
depression
Antibiotic Therapy:-
Empirical antibiotic therapy can be initiated after taken CSF culture as :
Vancomycin vial + Cefotaxime vial or Ceftriaxone + IV
Corticosteroid for 2 days.
until the result of culture appear then change the treatment
accordingly .
-S. pneumonia is sensitive to Vancomycin .
-H. influenza is sensitive to Cefotaxime or Ceftriaxone.
-N. meningitides is sensitive to Penicillin G .
Note: 3rd generation cephalosporins are also effective in N. meningitides
& β-lactam- sensitive S. pneumonia infection.
L. monocytogenes(come in neonate ) is only sensitive to Ampicillin.
Duration of antibiotic Treatment in uncomplicated meningitis as follows:-
N. meningitidis for 5-7 days.
H. influenza for 7-10 days.
S. pneumonia for 10-14 days;
whereas Gram-negative bacilli e.g. E. coli or P. aeruginosa either 3 wk or
at least 2 wk after CSF sterilization.
Pediatrics
NEUROLOGY
8
Corticosteroids use in meningitis:-
IV Dexamethasone use for 2 days to patients >6 wks. of age with
meningitis specifically due to H. influenzae type b had result in shorter
duration of fever, lower CSF protein and lactate levels, and reduction in
sensorineural hearing loss.
The maximum benefits of corticosteroids if given 1–2 hr before antibiotics
are initiated.
Complications.
Acute Complications
include: seizures, increased ICP, cranial nerve
palsies, stroke, cerebral or cerebellar herniation, thrombosis of Dural
venous sinuses, SIADH, & DIC.
Subdural effusions; it occur in the minority of patients but
asymptomatic in the majority; it is more common in infants resulted in
bulging fontanel, diastasis of sutures, enlarging head circumference,
emesis, seizures, & fever; it may be treated by aspiration.
Thrombocytosis, eosinophilia, and anemia may develop during
therapy of meningitis.
Pericarditis or arthritis may occur after Treatment of meningitis,
especially due to N. meningitides.
Late complications(outcome):
35% of patients have late sequelae,
particularly after pneumococcal meningitis include:
1-Sensorineural hearing loss: occurs in 30% of patients with pneumococcal
meningitis, It is due to labyrinthitis or direct auditory nerve inflammation.
2-recurrent seizures.
3-mental retardation.
4-blindness.
5-behavioral problems & learning disabilities.
6-ataxia.

Pediatrics
NEUROLOGY
9
Factor associated with poor prognosis include:-
a. Seizures that persist after the 4th day of illness or seizures that are
difficult to control.
b. Coma or focal neurologic signs on presentation.
c. High concentration of bacteria or low leukocyte count in the CSF.
d. Infants < 6 mo
Prevention
It is either by vaccination or antibiotic prophylaxis.
S. pneumonia; pneumococcal vaccine is recommended for children < 2 yr
of age and those at high risk e.g. asplenia or immunodeficiency.
No antibiotic Prophylaxis is required.
H. influenza type b; Conjugated vaccines for Hib started at 2 mo of age.
Rifampin Prognosis should be given to all house-hold contacts (except
pregnant women) once for 4 days.
N. meningitides; vaccine is recommended for high-risk children > 2 yr,
Rifampin for 2 days; ciprofloxacin or ceftriaxone (single dose) also can be
given. They should be given to all contacts (regardless of immunization
status) e.g. household, daycare center, nursery school contacts, and health
care workers who have direct exposure to oral secretions .
Follow up
1- Daily assessment of:
Vital signs, body weight, urine output, OFC,& neurologic assessment. This
important
to det ect the complications as early as possible & interfere rapidly such as:
blood pr.&
HR
ICP
body wt.& oliguria
SIADH
OFC
subdural effusion or hydrocephalus.
2- Long term follow up include monthly visit to check for OFC, mentality,
vision and hearing.
Pediatrics
NEUROLOGY
10
Viral meningoencephalitis is the most common cause of CNS infection.
Et .
Enteroviruses are the most common cause of viral meningo-
encephalitis. It spread directly from person to person
Herpes simplex virus type 1 (HSV-1) is an important cause of
severe, sporadic encephalitis. Brain involvement usually is focal .
Herpes simplex virus type 2 (HSV-2) may cause severe encephalitis
with diffuse brain involvement in neonates .
Varicella-zoster virus (VZV) may cause CNS infection (especially
cerebellar ataxia) in associated with chickenpox.
CLINICAL MANIFESTATION
The onset is generally acute, CNS signs and symptoms are preceded by a
nonspecific febrile illness of a few days' duration.
In the infant the presenting manifestations are irritability and lethargy.
In older children are headache(frontal or generalized) and hyperesthesia.;
adolescents frequently complain of retrobulbar pain. Fever, nausea and
vomiting, photophobia, and pain in the neck, back, and legs are common.
progressing to stupor with convulsions.
Focal neurologic signs may be present, especially in HSV-1 which cause
sever encephalitis, progression to coma & death occurs in 70% of cases
without antiviral treatment.
Loss of bowel and bladder control may occur. Skin rash may occurs with
enteroviruses & measles infection.
Investigations
CSF exam; see the table above.
Serology of blood may be useful in determining some viral CNS
infection e.g. arbovirus infection
EEG show diffuse slow wave activity.
Viral meningoencephalitis
Pediatrics
NEUROLOGY
11
CT & MRI show swelling of brain parenchyma.
Note:
HSV encephalitis is suggested by focal seizures & focal finding on
EEG, CT, or MRI especially if involve the temporal lobe.
Treatment
HSV encephalitis is treated with IV Acyclovir, for 2-3 wk.
Otherwise, Treatment of viral meningoencephalitis is supportive .
Mild disease may require only symptomatic relief. More severe disease
may require hospitalization and intensive care.
Headache and hyperesthesia are treated with rest, non–aspirin-
containing analgesics & reduction in room light, noise, and
visitors.
Fever; acetaminophen.
Vomiting; phenothiazine.
Poor oral intake; IV fluids ,Total parenteral nutrition may be
required in prolonged coma.
Complications
Guillain-Barre syndrome, Transverse myelitis, Hemiplegia,
and Cerebellar ataxia.
Prognosis
Most children recover completely from viral infections of the CNS,
especially those due to enteroviruses, whereas others have high mortality
rate e.g. HSV, or have severe sequelae e.g. epileptic, visual, or auditory.
Prevention.
Isolation of cases, vaccination is available for some viruses e.g. varicella,
& measles .
