REPRODUCTIVE ENDOCRINOLOGY
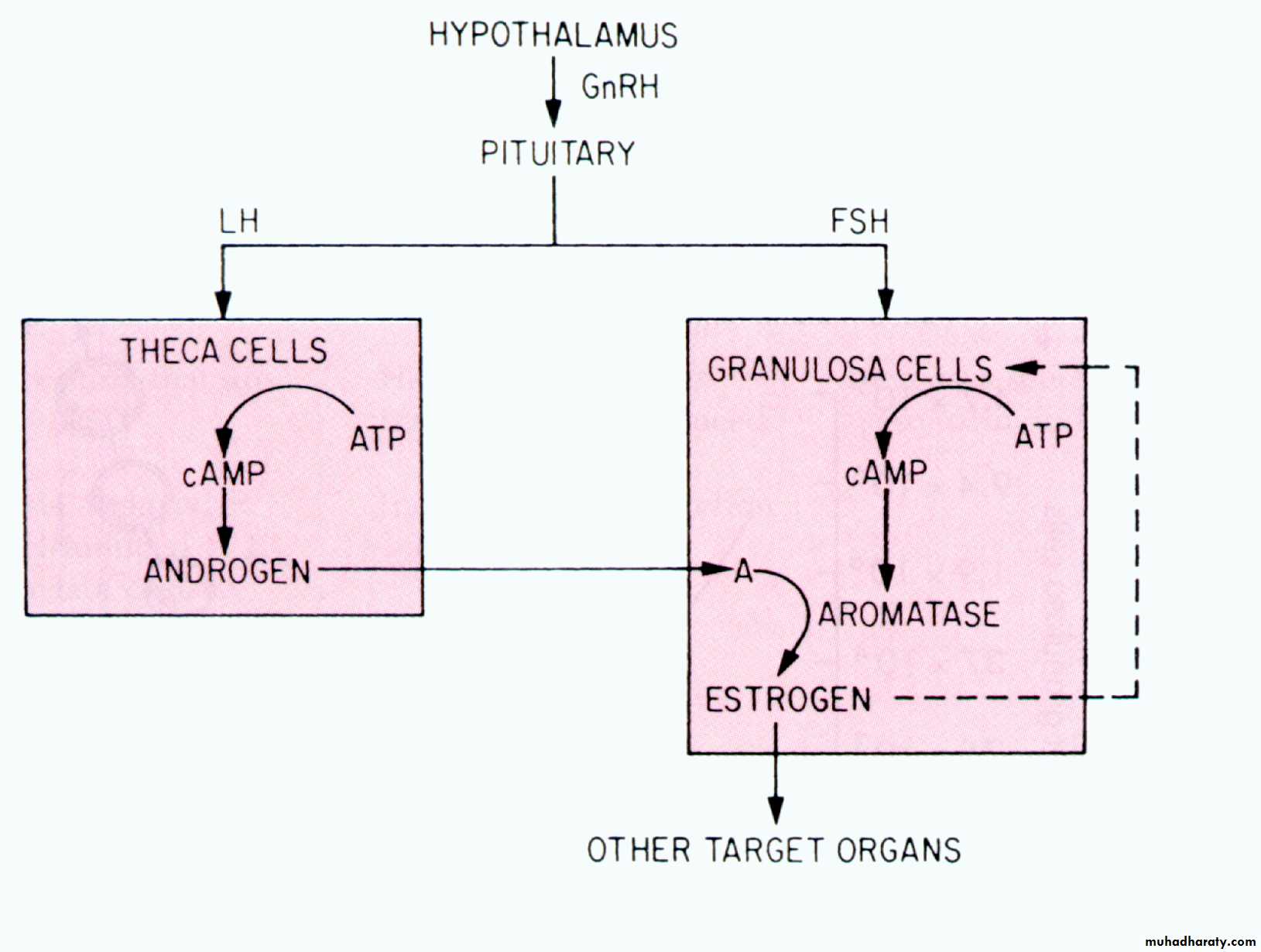
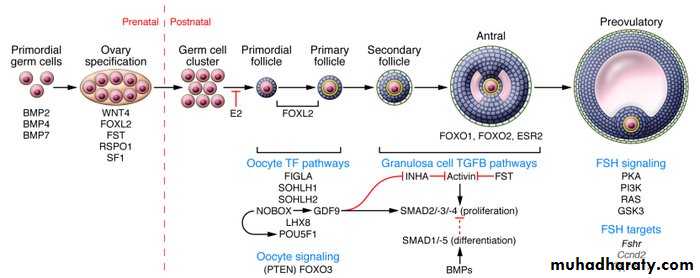
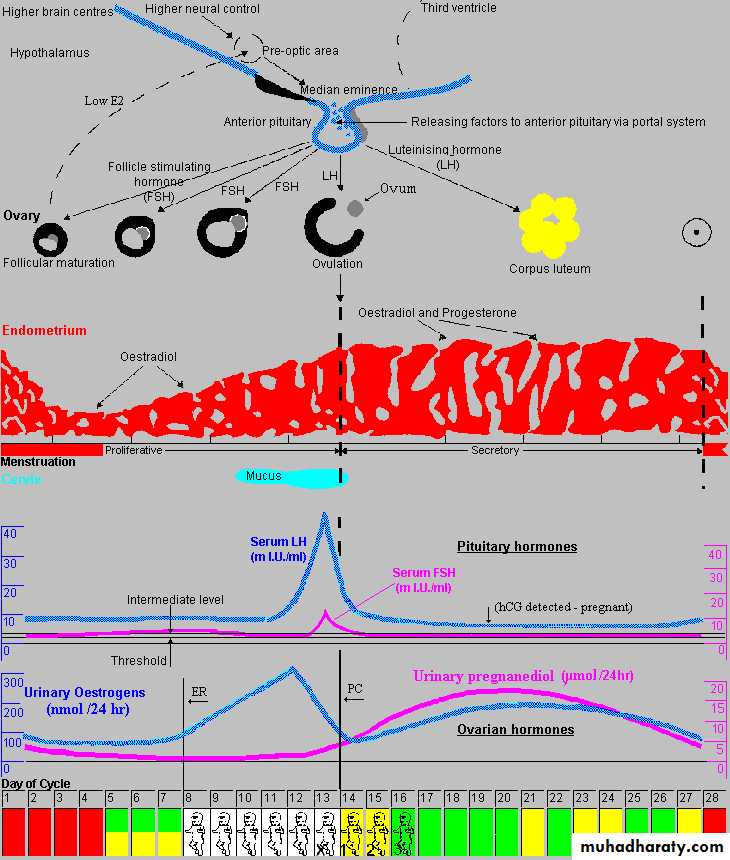
Normal reproductive function requires precise quantitative and temporal regulation of the hypothalamic-pituitary-ovarian axisWithin the hypothalamus, specific nuclei release gonadotropin-releasing hormone (GnRH) in pulses. This decapeptide binds to surface receptors on the gonadotrope of the anterior pituitary gland; which secrete
glycoprotein gonadotropins, that is, luteinizing hormone (LH) and follicle-stimulating hormone (FSH), into the peripheral
circulation.
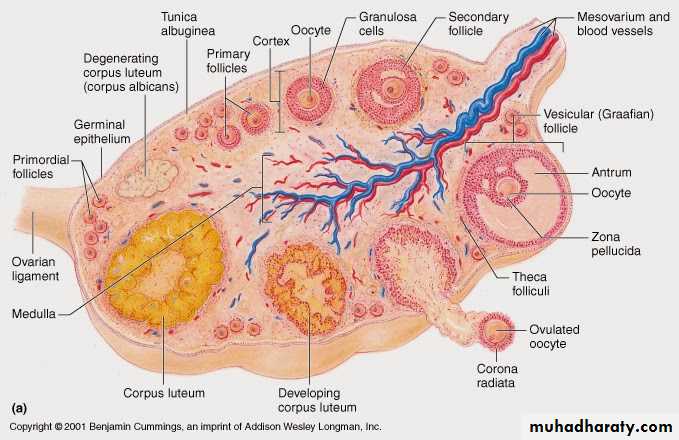
Within the ovary,
LH and FSH bind to theca and granulosa cells to stimulate1-folliculogenesis
2-production of an array of
steroid hormones (estrogens, progesterone, and androgens),
gonadal peptides (activin, inhibin, and follistatin), and
growth factors
Ovarian Hormones
Conclusion
The hypothalamus secretsThe pituitary secrets
The ovary secrets
. Among other functions, these ovarian-derived factors feedback to the hypothalamus and pituitary gland to inhibit or, at the midcycle surge, augment GnRH and gonadotropin secretion.
The ovarian steroids are also critical for preparing the endometrium for implantation of the embryo if pregnancy ensues.
The ‘ two - cell, two gonadotrophin ’hypothesis
specifi es the need for both LH, to stimulate production of precursor androgens, particularly androstenedione, by the theca cell layer,and FSH, to drive aromatizationto oestradiol within the adjacent granulosa cell layer
Folliculogenesis and the ‘follicular phase
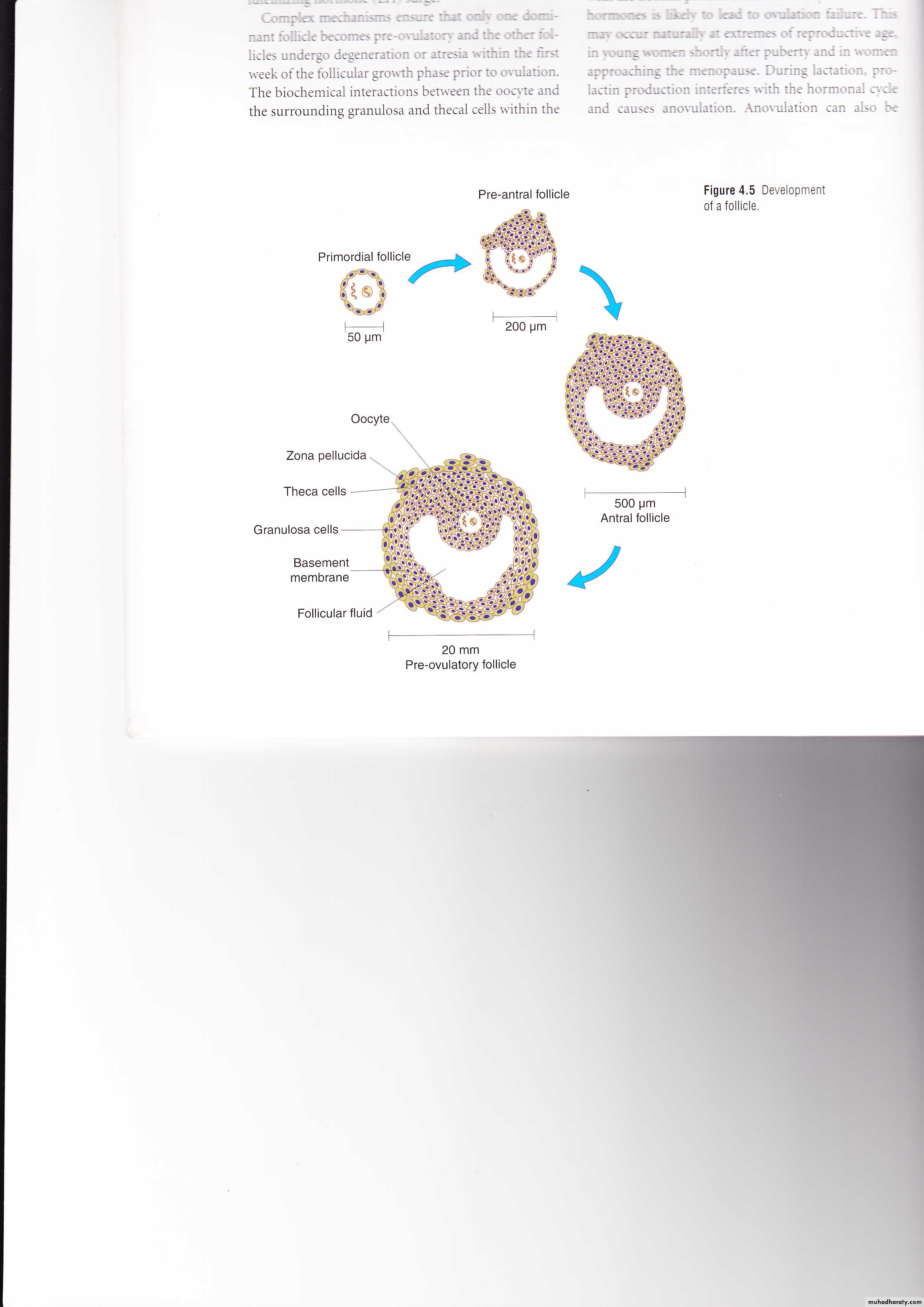
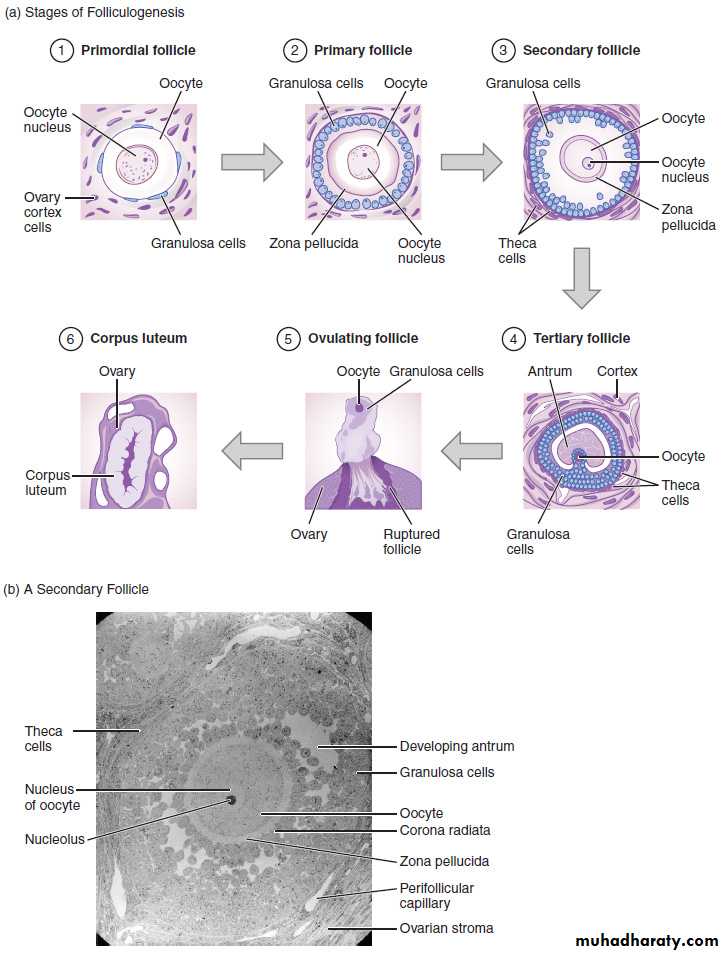
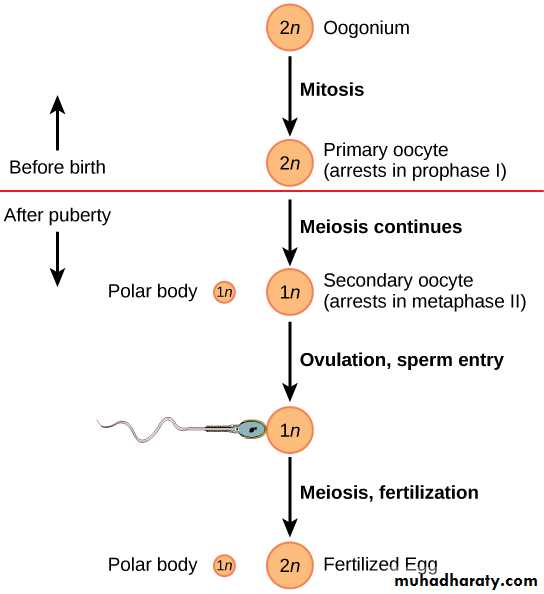
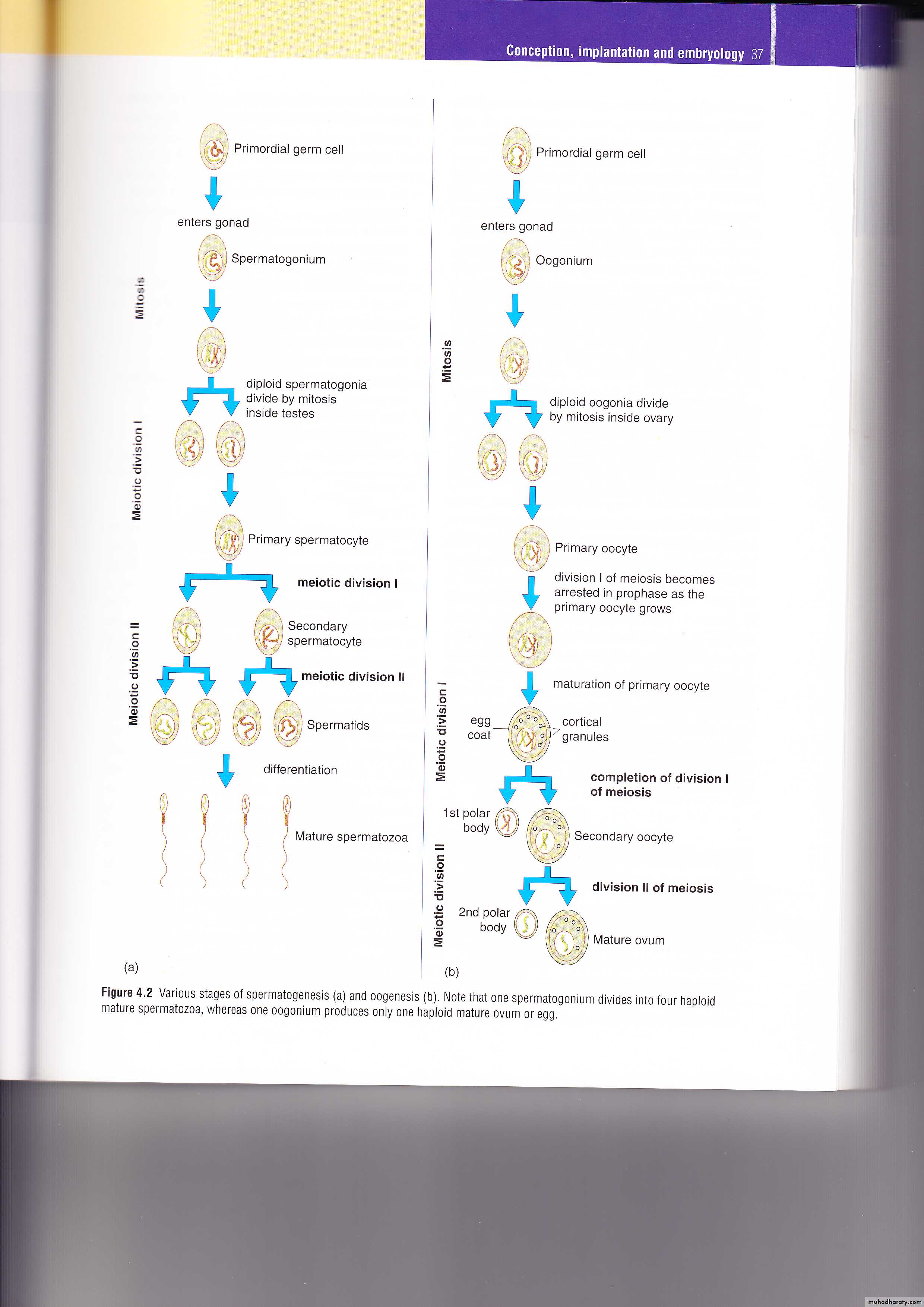
At birth, the human ovaries contain approximately 1million primordial follicles, arrested at prophase of the first meiotic division.Further depletion of the follicle pool will continue throughout reproductive life, with regular escape of follicles from the primordial ‘ resting phase ’ by re - entry into meiosis.
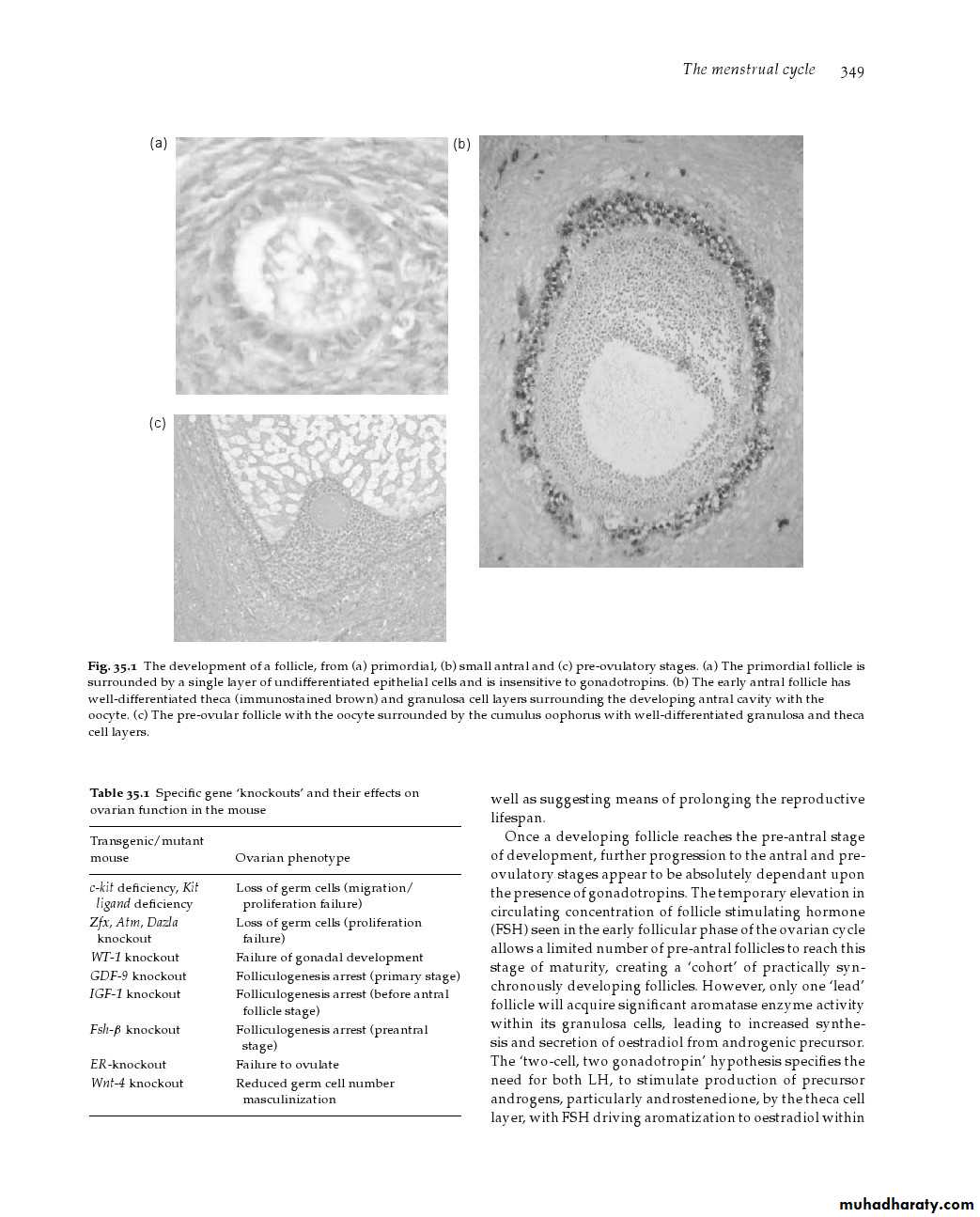
The development of a follicle
primordial follicle is surrounded by a single layer of undifferentiated epithelial cells, and is insensitive to gonadotropins.
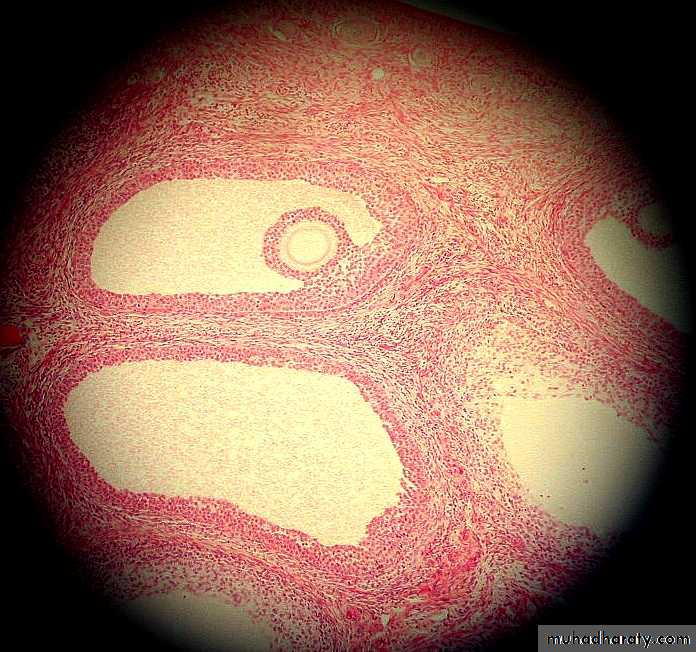
The early antral follicle has well - differentiated theca and granulosa cell layers surrounding the developing antral cavity with the oocyte.
The pre - ovulatory follicle with the oocyte surrounded by the cumulus oophorus with well - differentiated granulosa and theca cell layers.
Once a developing follicle reaches the pre - antral stage of development, further progression to the antral and pre - ovulatory stages appears to be absolutely dependent on the presence of gonadotrophins.
The temporary elevation in circulating concentration of follicle – stimulating hormone (FSH) seen in the early follicular phase of the ovarian cycle allows a limited number of pre - antral follicles to reach this stage of maturity, creating a cohort of practically synchronously developing follicles.
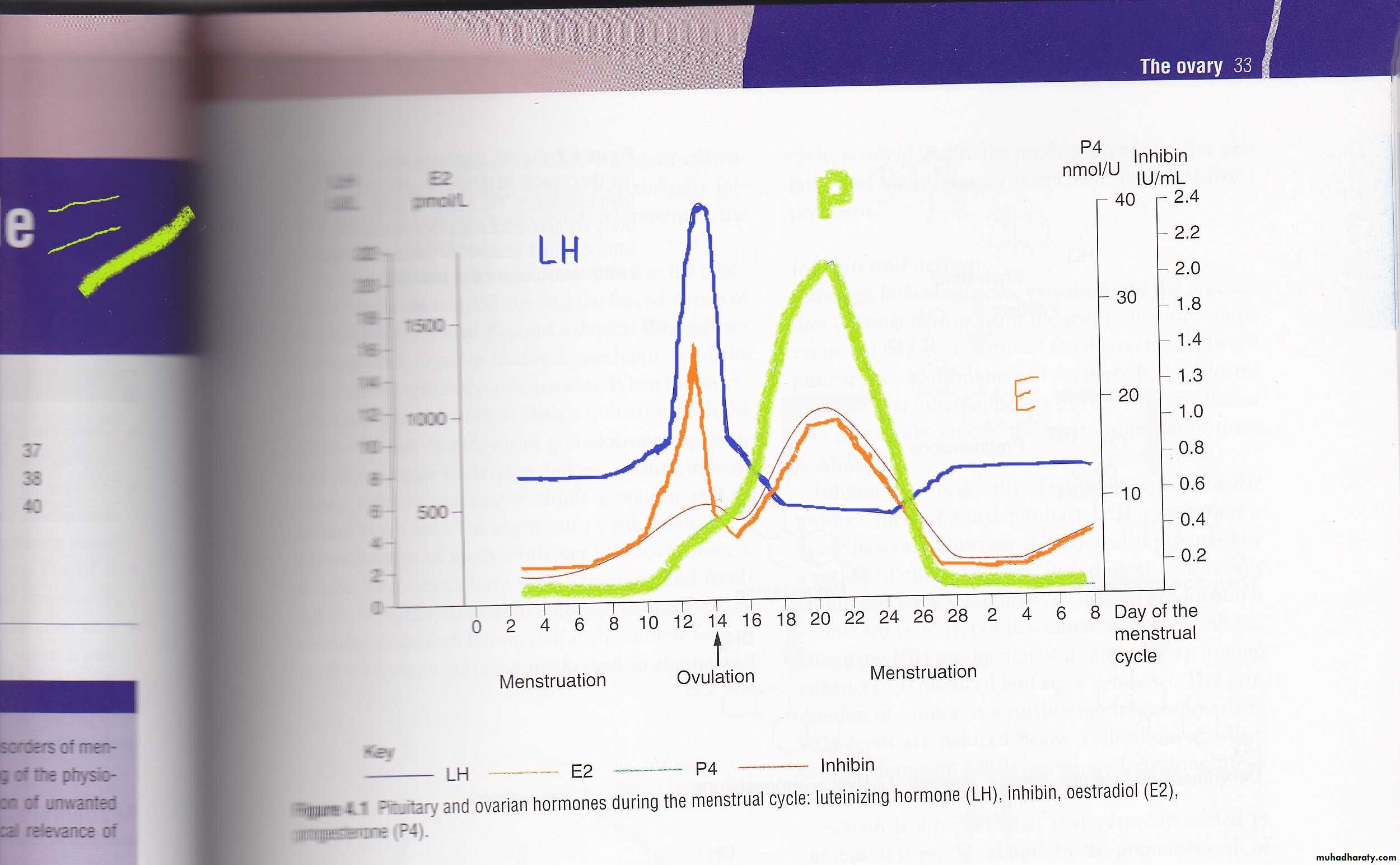
Once the concentration of serum 1)oestradiol begins to rise in the mid - follicular phase, there is rapid suppressionof pituitary FSH production by negative feedback; which is co - mediated by rising serum concentrations of 2) inhibin B,a glycoprotein secreted by the granulosa cells of the developing dominant follicle .
The resulting decrease in [ FSH] withdraws gonadotrophin ‘ drive ’ from the remainder of the growing cohort of follicles.
The result is progression to atresia for all but the dominant follicle, leading to mono - ovulation.
only one ‘ lead ’ follicle will acquire signifi cant aromatase enzyme activity within its granulosa cells, leading to increased synthesis and secretion of oestradiol
The LH surge and ovulation
Final maturation of the oocyte only occurs after initiation of the LH surge. This ensures that the oocyte is mature and ready for fertilization after release from the follicle.. This occurs in response to the rapid rise in
1) oestradiol during the latter days of the follicular phase of the ovarian cycle.Pulses of GnRH from the hypothalamus increase in both magnitude and frequency, triggering the LH surge with a rapid outpouring of LH which is also preceded by a rise in serum concentration of 2) progesterone..
The LH surge
The LH surge initiates final maturation of the oocyte with completion of meiosis and extrusion of the first polar body, which contains one of the two haploid sets of chromosomes from the oocyte.The LH surge also induces an infl ammatory - type reaction at the apex of the follicle adjacent to the outer surface of the ovarian cortex.
A process of new blood vessel formation, with associated release of prostaglandins and cytokines, leads to rupture of the follicle wall and ovulation about 38 hours after the initiation of the LH surge.
A chemotactic effect of ovarian cytokines draws the fimbria of the fallopian tube to within close proximity of the rupturing follicle.
The ‘ empty ’ follicle rapidly fills with blood and the theca and granulosa cell layers of the follicle wall luteinize,with formation of the corpus luteum.
A rapid synthesis of progesterone, along with oestradiol, follows.
[progesterone] in serum rise to This rise still further if pregnancy follows
Endometrial development during themenstrual cycle and early pregnancy
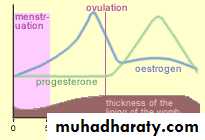
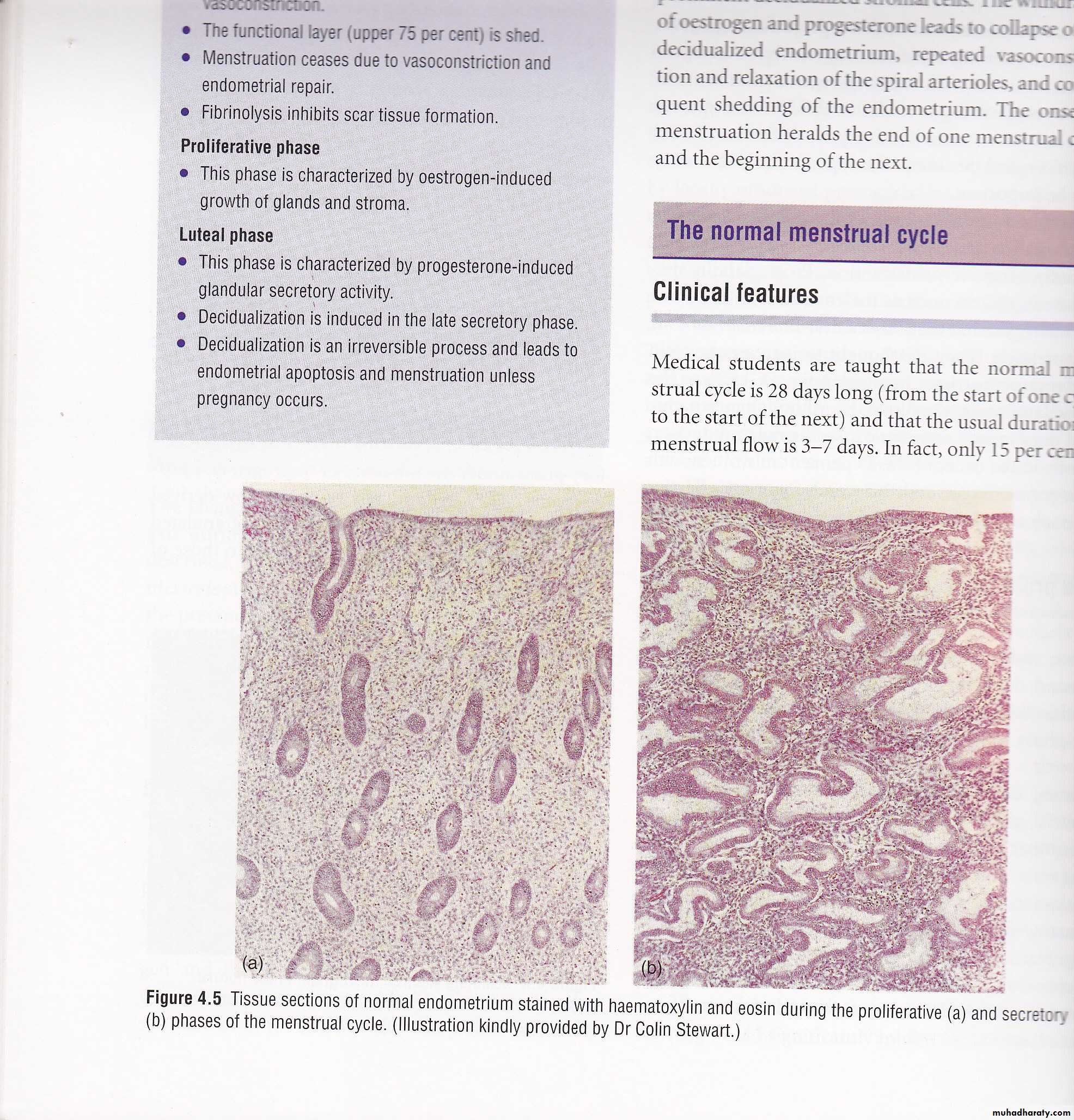
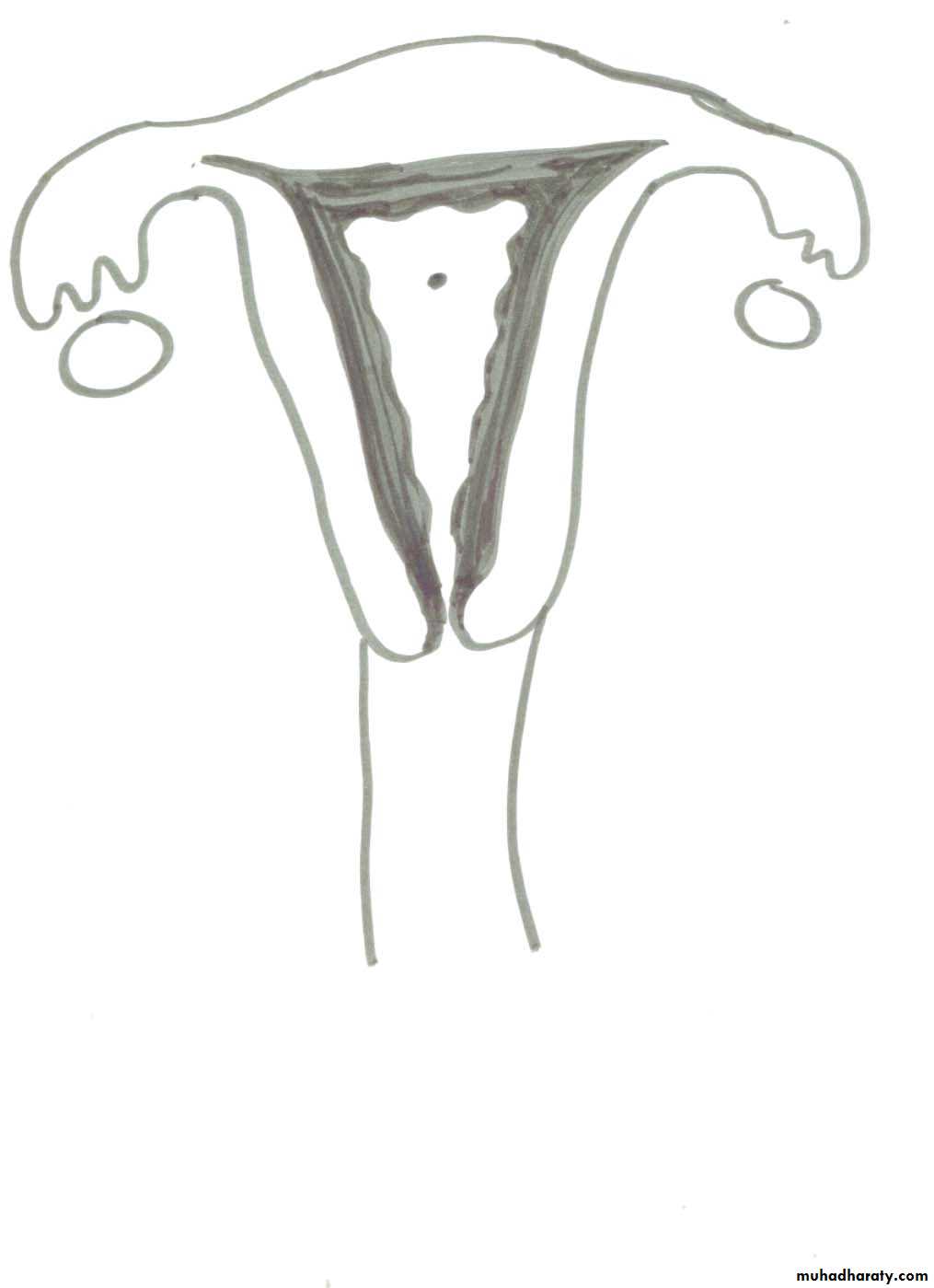
Progression through the follicular phase of the cycle is characterized by the appearance of increasing amounts of oestradiol in the circulation.This acts on the basalis layer of endometrium, which persists from cycle to cycle in contrast to the monthly shedding of the more superfi cial layers of endometrium.
The new, proliferative endometrium grows rapidly under the infl uence of oestradiol, in synchrony with the growth and maturation of the oocyte and its follicle.
An organized architecture appears, with endometrial glands and stromal compartments,
in preparation for the development of secretory endometrium permissive of :-
implantation following theLH surge,
luteinization of the ruptured follicle and
formationof the corpus luteum, with secretion of large amounts of progesterone
A key element in growth of healthy endometrium is
formation of new blood vessels (endometrial angiogenesis),which seems to occur by elongation and expansion
from pre - existing small vessels in the basalis. Endometrial angiogenesis can be divided into three stages:
Firstly,during menstruation, to reform the vascular bed;
second,during the proliferative phase to develop endometrial vascular supply; and,
Changes in the Uterus:
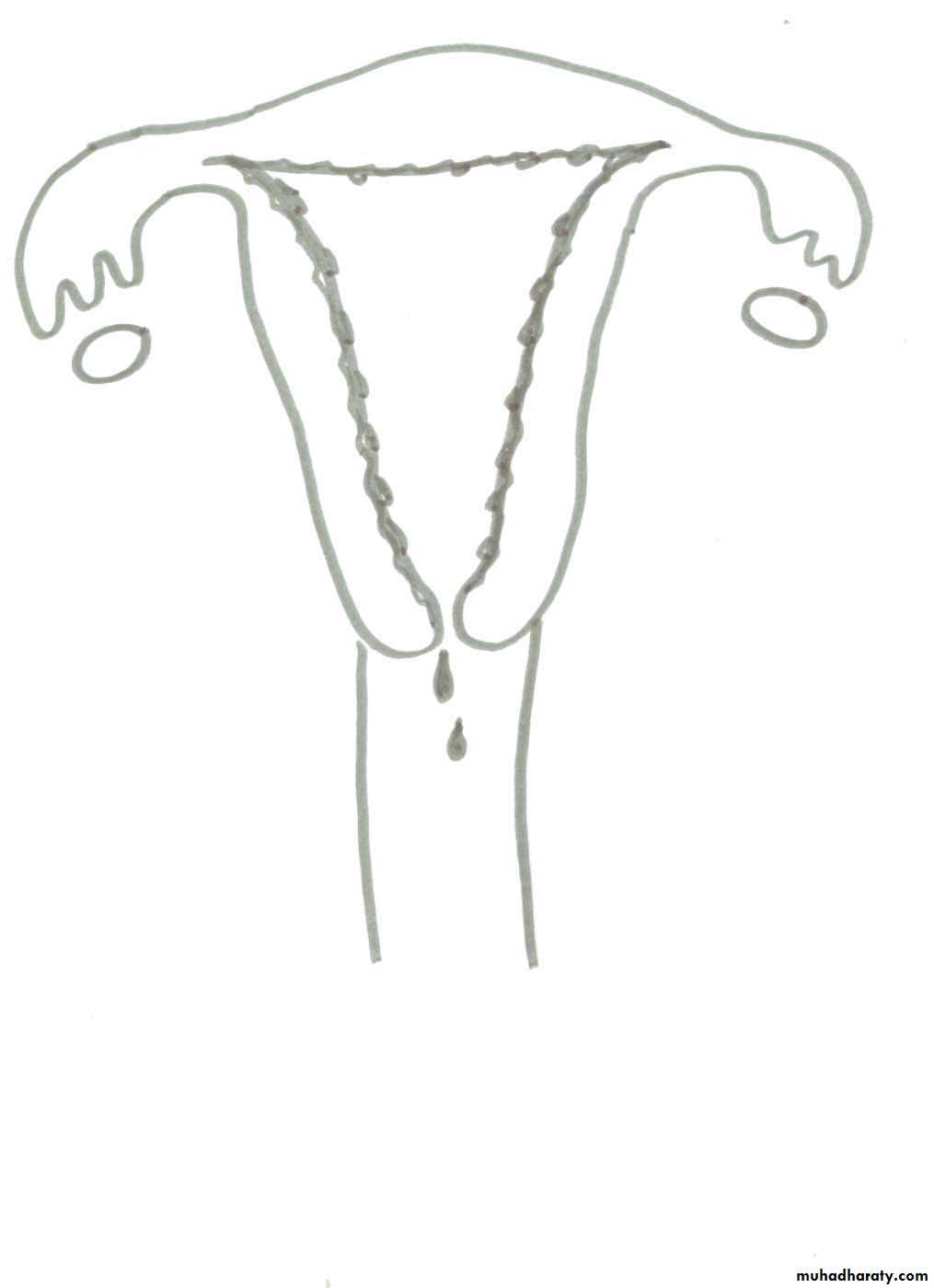
Stage 1- Day 1-5 menstruation
Stage 2 Day 5- 13 pre-ovulatory stageStage 3 Day 14 Ovulation
Stage 4 Day 15-28 post-ovulatory stage
finally, with spiral arteriole growth and coiling during the secretory phase, with the aim of providing an adequately vascularized site for implantation.
The endometrial vascular network grows and regresses during each menstrual cycle.
Secretory phase
The peak secretory activity occurs at time of implantation(7 days after gonadotrophin surge)The progesterone is essential for the secretory endometrial changes & these changes are only seen
after ovulation.
finally the spiral arteriole growth and coiling with the aim of providing an adequately vascularized site for implantation
The Menstruation
menstruationImmediately prior to menstruation, the endometr-
ium regress, endometrial venous drainage is inhibited
then a sequence of intense spiral artery vasoconstriction followed by relaxation is generated.
These event lead to ischemia & tissue damage, shedding of the functional endometrium
(stratum compactum &spongiosum) & bleeding from
fragments of arterioles remaining in the basal endometrium.
. The PGs of the E and F series are present in high concentrations in the endometrium and their synthesis is regulated by the ovarian steroids.
Homeostasis in the endometrium is secured by spiral artery vasoconstriction .
Later, repair of the endometrium & new vessel formation (angiogenesis) lead to complete cessation of bleeding within 5-7 days from the start of the menstrual cycle.normal cycle evry 28days &normal blood loss is 30-80ml