Introduction to Cardiovascular disease dr.Faris alhialy lect. 1
Cardiovascular disease is the most frequent cause of adult death in the Western world; for example in the UK one-third of men and one-quarter of women died as a result of ischaemic heart disease. In many developed countries, the incidence of ischaemic heart disease has been falling for the last two or three decades, but it is rising in Eastern Europe and Asia.
SYMPTOMS OF HEART DISEASE
The following symptoms occur with heart disease:
Chest pain
Breathlessness
Palpitations
Syncope
Fatigue
Peripheral oedema.
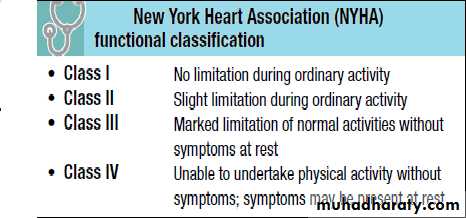
The severity of cardiac symptoms or fatigue is classified according to the New York Heart Association (NYHA) grading of cardiac status (see Table below).
Chest pain
Chest pain is a common presentation of cardiac disease but can also be a manifestation of anxiety or disease of the lungs or musculoskeletal or gastrointestinal systems . Some patients deny ‘pain’ in favour of ‘discomfort’ but the significance remains the same.Central chest pain
This is the most common symptom associated with heart disease. The pain of angina pectoris and myocardial infarction is due to myocardial hypoxia. Types of pain include:
Retrosternal heavy or gripping sensation with radiation to the left arm or neck that is provoked by exertion and eased with rest or nitrates this is (angina pectoris)
Similar pain at rest (acute coronary syndrome)
Severe tearing chest pain radiating through to the back (aortic dissection)
Sharp central chest pain that is worse with movement or respiration but relieved with sitting forward (pericarditis pain)
Sharp stabbing left submammary pain associated with anxiety (Da Costa’s syndrome)
Dyspnoea
Left ventricular failure causes dyspnoea due to oedema of the pulmonary interstitium and alveoli. This makes the lungs stiff (less compliant), thus increasing the respiratory effort required to ventilate the lungs. Tachypnoea (increased respiratory rate) is often present owing to stimulation of pulmonary stretch receptors.Orthopnoea refers to breathlessness on lying flat. Blood is redistributed from the legs to the torso, leading to an increase in central and pulmonary blood volume. The patient uses an increasing number of pillows to sleep.
Paroxysmal nocturnal dyspnoea (PND) is when a patient is woken from sleep fighting for breath. It is due to the same mechanisms as orthopnoea. However, as sensory awareness is reduced whilst asleep, the pulmonary oedema can become quite severe before the patient is awoken.
Hyperventilation with alternating episodes of apnoea (Cheyne–Stokes respiration) occurs in severe heart failure.
Palpitations
These represent an increased awareness of the normal heart beat or the sensation of slow, rapid or irregular heart rhythms.
The most common arrhythmias felt as palpitations are premature ectopic beats and paroxysmal tachycardias.
Premature beats (ectopics) are felt by the patient as a pause followed by a forceful beat. This is because premature beats are usually followed by a pause before the next normal beat, as the heart resets itself. The next
beat is more forceful as the heart has had a longer diastolic period and therefore is filled with more blood before this beat.
Paroxysmal tachycardias are felt as a sudden racing heart beat.
Bradycardias may be appreciated as slow, regular, heavy or forceful beats. Most often, however they are simply not sensed.
Syncope
Syncope is a transient loss of consciousness due to inadequate cerebral blood flow. The cardiovascular causes are
Vascular:
A vasovagal attack is a simple faint and is the most common cause of syncope. The mechanism begins with peripheral vasodilatation and venous pooling of blood, leading to a reduction in the amount of blood returned to the heart. The near-empty heart responds by contracting vigorously, which in turn stimulates mechanoreceptors (stretch receptors) in the inferoposterior wall of the left ventricle. These in turn trigger reflexes via the central nervous system, which act to reduce ventricular stretch (i.e. further vasodilatation and sometimes profound bradycardia),
but this causes a drop in blood pressure and therefore syncope. These episodes are usually associated with a prodrome of dizziness, nausea, sweating, tinnitus, yawning and a sinking feeling. Recovery occurs within a few seconds, especially if the patient lies down.
Postural (orthostatic) hypotension is a drop in systolic blood pressure of 20 mmHg or more on standing from a sitting or lying position. Usually, reflex vasoconstriction prevents a drop in pressure but if this is absent or the patient is fluid depleted or on vasodilating or diuretic drugs, hypotension occurs.
Postprandial hypotension is a drop in systolic blood pressure of ≥20 mmHg or the systolic blood pressure drops from above 100 mmHg to under 90 mmHg within 2 hours of eating. The mechanism is unknown but may be due to pooling of blood in the splanchnic vessels. In normal subjects, this elicits a homeostatic response via activation of baroreceptors and the sympathetic system,peripheral vasoconstriction and an increase in cardiac output.
Micturition syncope refers to loss of consciousness whilst passing urine.
Carotid sinus syncope occurs when there is an exaggerated vagal response to carotid sinus stimulation provoked by wearing a tight collar, looking upwards or turning the head.
Obstructive. The obstructive cardiac causes lead to syncope due to restriction of blood flow from the heart into the rest of the circulation, or between the different chambers of the heart.
Arrhythmias. Stokes–Adams attacks are a sudden loss of consciousness unrelated to posture and due to intermittent high-grade AV block, profound bradycardia or ventricular standstill. The patient falls to the ground without warning, is pale and deeply unconscious. The pulse is usually very slow or absent. After a few seconds the patient flushes
brightly and recovers consciousness as the pulse quickens.
Often there are no sequelae, but patients may injure themselves during falls. Occasionally a generalized convulsion may occur if the period of cerebral hypoxia is prolonged, leading to a misdiagnosis of epilepsy.
Fatigue
Fatigue may be a symptom of inadequate systemic perfusion in heart failure. It is due to poor sleep, a direct side-effect of medication, particularly beta-blockers, electrolyte imbalance due to diuretic therapy and as a systemic manifestation of infection such as endocarditis.
Peripheral oedema
Heart failure results in salt and water retention due to renal underperfusion and consequent activation of the reninangiotensin-aldosterone system . This leads to dependent pitting oedema.
General features of the patient’s wellbeing should be noted
as well as the presence of conjunctival pallor, obesity, jaundiceand cachexia.
Clubbing is seen in congenital cyanotic heart disease, particularly Fallot’s tetralogy and also in 10% of patients with subacute infective endocarditis.
Splinter haemorrhages. These small, subungual linear haemorrhages are frequently due to trauma, but are also seen in infective endocarditis.
Cyanosis is a dusky blue discoloration of the skin (particularly at the extremities) or of the mucous membranes when the capillary oxygen saturation is less than 85%. Central cyanosis is seen with
shunting of deoxygenated venous blood into the systemic circulation, as in the presence of a right-to-left heart shunt.
Peripheral cyanosis is seen in the hands and feet, which are cold. It occurs in conditions associated with peripheral vasoconstriction and stasis of blood in the extremities leading to increased peripheral oxygen extraction. Such conditions include congestive heart failure, circulatory shock, exposure to cold temperatures and abnormalities of the peripheral
circulation, e.g. Raynaud’s phenomena
INTRODUCTION TO MEDICINE AND ART OF HISTORY TAKING
The principles of medicine are difficult to define they represent the interaction of clinical experience with knowledge acquired by study and researches and Good medical practice and the art of medicine, hinges on recognizing and respecting the breadth of physical, cultural, spiritual, experiential and psychosocial characteristics of each patient, and understanding their impact on the patient's beliefs, attitudes and expectations. Doctors must deliver appropriate care which considers the technical complexities of modern treatment, and at the same time deals with the communication and interpersonal needs of the patient, at a time when he or she may feel most vulnerable. In addition to the diagnosis and treatment of illness, the scope of medicine has expanded to preventing disease through measures such as screening, vaccination and health promotion.
write management of the patient need proper diagnosis which require
2-history taking 2-physical examination 3-investigations and 4-interpretation of these data, keeping in mind that diagnosis should precede treatment whenever possible
ART OF HISTORY TAKING.
History taking is a special form of communication and you should put the patient at ease and encourage him or her to talk freely and to tell their story in their own way and own words and experienced doctor can diagnose the problem from the moment the patient walks or general appearance or attitude and personalityIn spite of the proliferation of modern diagnostic tests and sometimes freely available, history taking and physical examination remain essential
The history is vary according to whether it is being taken in the wards, out patient clinic , emergency unite or in the home and according to the availability of time and status of the patient and try to be gentle and always tell the patient what you are doing and try never to cause pain.
Heading to be used in history taking
Name
Age
Address
occupation
marital status
you may ask about religion, nationality, blood group and next of kin.
Date of admission(DOA(
chief complaint and duration
history of present illness
review of systems (CVS, RS, GIT, US, NS & LS(
Past Medical history.
past surgical history.
family history.
personal and social history.
drug history & allergy
menstrual history in female.
Regarding chief complaint some patients have more than one complaint and you can mentioned two or three complaint but keeping in mind that some neurotic and anxious patient have so many complaint that is impossible to identify a single presenting complaint, the timing and duration of symptoms is important and some patients with long standing symptom tend to date them by events rather than by date and you should avoid as far as possible leading questions witch themselves suggest an answer and usually ask the patient to tell you the story of the illness from the beginning .
Pain is the commonest complain among patient e.g. chest pain, back pain ,loin pain, headache and extra and once pain is present you have to ask the following questions
Analysis of pain:-
1-Site of the pain e.g. retrosternal chest pain
2-Severity e.g. does it interfere with daily activity but some patient exaggerated their symptoms and seeking sympathy by increase severity of pain.
3-Radiation dose it spread and move may gradually or shooting acute like disc prolapsed
4-Timing and duration
5-Character of the pain like stabbing, pricking, burning, colicky or continuous steady pain.
6- Aggravating and reliving factors.
Negative Data is important to be mentioned the absence of important symptoms is significant as the presence of symptoms like haemoptesis in cough or SOB.
History does not end when the patient as first seen and continuation notes should record the disappearance of symptoms or the appearance of new ones or any other thing appear while the patient is under observation