Urticaria
ByDr.Alaa A. Al-sahlany
Dec 23, 2018
Urticaria
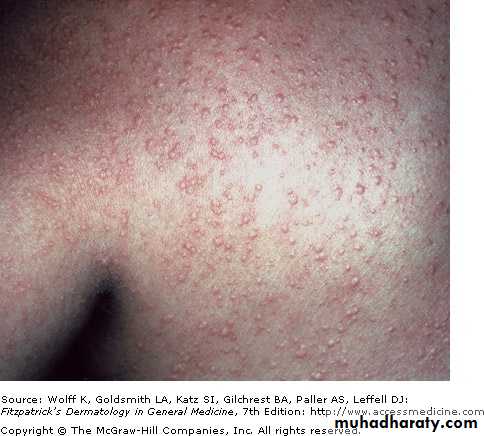
Wheal(lesion): pruritic evenescent pink or pale swelling of superficial dermisAngioedema(lesion): swelling of deep dermis and subcutaneous or submucosal tissue
Urticaria(disease): recurrent wheal or/and angioedema of skin
Urticaria affects 1-5% of population
Overall, urticaria is more common in women than men
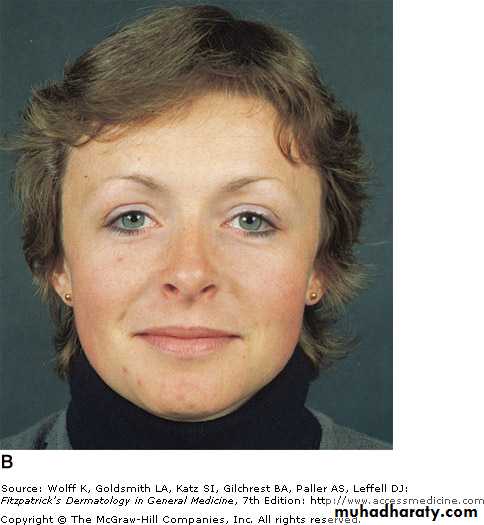
Wheals and Angioedema
AngioedemaWheals
Swelling of deep dermis, subcutaneous tissue
Swelling of upper dermis
Skin-colored, painful and ill-defined
Red and itchy and well-defined
Last more than 24 hours
Last less than 24 hours
Involves skin and mucosae
Involves skin only
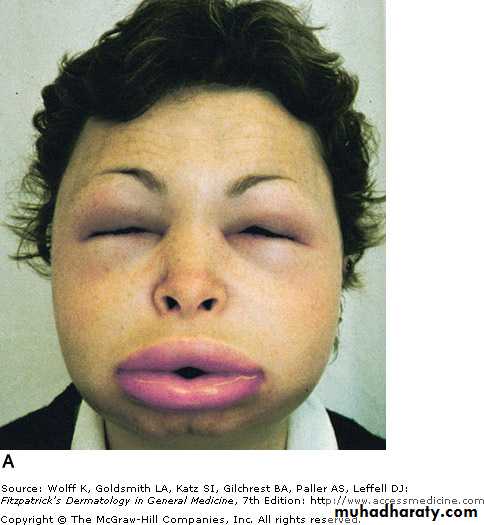
Urticaria Type I hyperensitivity reaction
The allergen bind with the receptor bound IgE leading to cross-linking of two or more IgE receptors on mast cell membrane that result in degranulation
Pathogenesis
. Mast cells are distributed throughout the body
. Mast cells express high affinity IgE receptors.
. Types of degranulating stimuli are (1)immunological i.e. penicillin and (2)non-immunological i.e. opiates, NSAIDS
Degranulators
Autoimmune urticaria
Anti-IgE receptor and to lesser extent anti-IgE antibodies are detected in sera of 25- 50% of patients with a chronic ordinary urticaria and this can be detected by autologous serum skin test(ASST)Autologous serum skin test
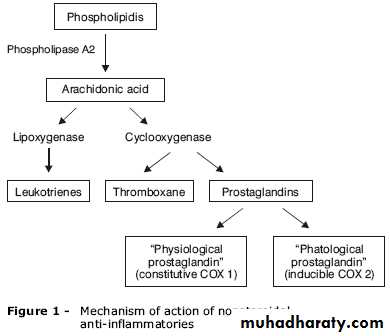
Pathogenesis
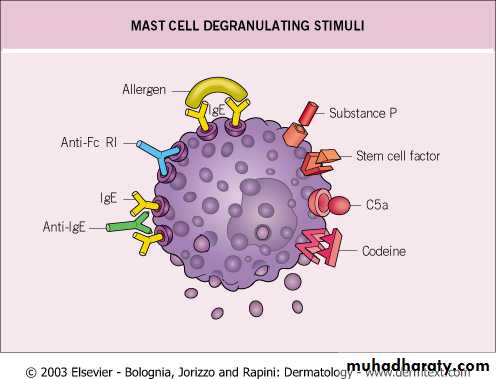
Many proinflammatory mediators are involved; the most important are histamine(produced by mast cells), PGs (has an inhibitory effect on degranulation) and LTs(has a stimulatory effect) and kinins (stimulatory effects)Other WBCs may be involved such as basophils (produce histamine) and eosinophils (produce major basic protein)
Mediatorts of urticaria
Leukotriens
bradykinin
Histamine
The mediator
Aspirin sensitive urticaria
ACE inhibitors
And
C1 estase inhibitor deficiency
Urticaria and angioedema
Example
Treated by lipoxygenase inhibitors i.e. monteleukast
Treated by bradykinin receptor antagonists e.i. icatibant
Treated by antihistamines
Treatment
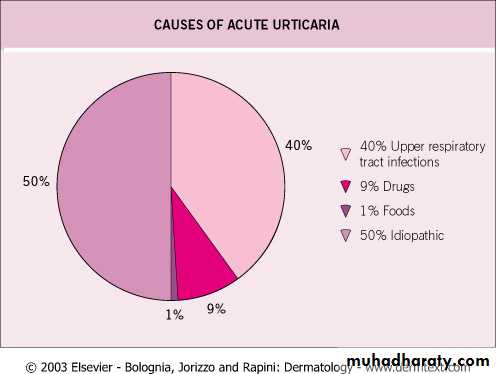
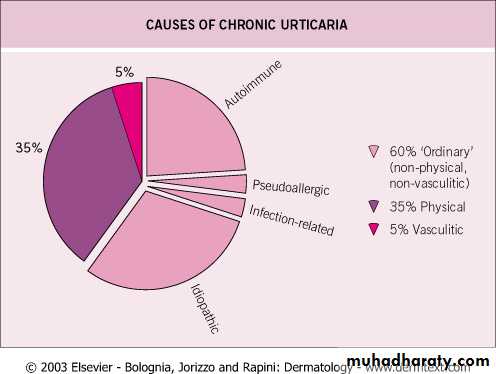
Classification
(I) Acute and chronic (the cut-off is 6 wks)(II) Immunological e.g. penicillins and non-immunological e.g. opiates directly degranulates mast cells
(III) Clinical classification:
1. Ordinary urticaria
2. Physical urticaria
3. Urticarial vasculitis
4. Contact urticaria
5. Angioedema without wheals
6. Urticarial syndromes e.g. Familial meditranean fever
Physical urticaria
Linear wheals at site of scratching and frictionDermographism
Deep swelling after at least 30 min of sustained pressure, may last for few days e.g. Palms after manual work and soles after walk
Delayed pressure urticaria
Pins and needles sensation after sweat-inducing stimuli e.g. exertion, hot bath, stressOccurs usually in young adult with atopic tendency
Cholinergic urticaria
Wheals appears within minutes after cold exposure
• Cold swimming can cause anaphylaxis
Associated with cryoglobulinemia or cryofibrinogenemia
Cold contact urticaria:(1)Primary (idiopathic) 95%
(2)Secondary
Wheals after contact with water of any temperature
Aquagenic urticaria
Wheals appears within minutes of sun exposure
Solar urticaria
• Appears within minutes after contact with heat
• Heat contact urticaria
DermographismCold urticaria(after ice cube test)
Cholinergic urticaria
Angioedema without wheals
C1 estrase inhibitor deiciency( C4)Acquired angioedema
Hereditary angioedema
(Autosomal dominant)
Type 1: lymphoproliferative disease
Type 2: autoAb to C1 estrase inhibitor e.g. SLE
Type 1: low level of C1 estrase inhibitor
Type 2: normal level of dysfunctional
C4: decreased
C1q: decreased
C4 : decreased
C1q: normal
Provocative factors: surgey, trauma and stress
Provocative factors: surgery, stress, trauma
Contact urticaria
Non-immunologicalImmunological (IgE mediated)
Type
Wheals appears within minutes of contact with skin or mucosa
Caused by direct effect on mast cells
Mediated by IgE
Pathogenesis
Nettle sting has histamine
Those who develop hand urticaria after contact with latex in gloves
Example
Respond to NSAIDs
Respond to anti-histamine
Treatment
Contact urticaria
Nettle
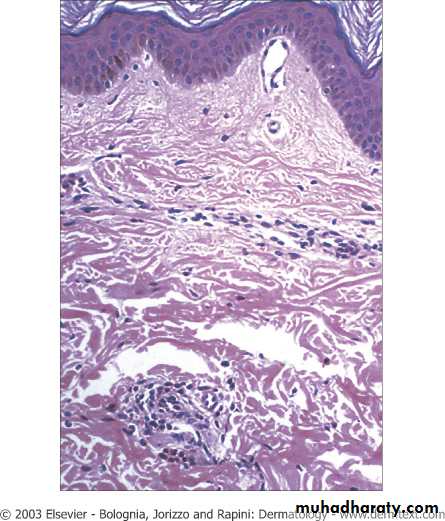
Urticaria and urticarial vasculitis
Urticarial vasculitisOrdinary urticaria
Type
Last longer than 24 hours
Individual lesion Last less than 24 hours
Duration
It leaves pigmentation
Does not leave pigmentation after it disappears
Signs
Burn, pain
Pruritic
Symptoms
Small vessel vasculitis
dermal edema
Pathology
Histopathology
Diagnosis
Detailed history: a Hx of infection, drugs (in acute urticaria), duration, a Hx of exacerbationg factors, family history (hereditary angioedema)Physical exam: circling the wheal e.g. more than 24 hours or pigment left after disappearance of wheal
Investigation:
. Acute urticaria: no need except(1) if not responsive to Rx ,(2) last longer than 24 hrs
. Chronic urticaria: CBC, ESR, WBC differential, C4 and if this is normal ASST
. Urticarial vasculitis biopsy
.
Physical urticaria challenge test
Cold urticaria: ice cube test for cold urticaria and if positive check cryoproteins such as cryoglobulin, cryofibrinogens and cold agglutininsolar uricaria ANA
Delayed pressure urticaria: apply a weight
Cholinergic urticaria: make the patient run
Dermographism: stroke the skin
Treatment
Treatment paradigm
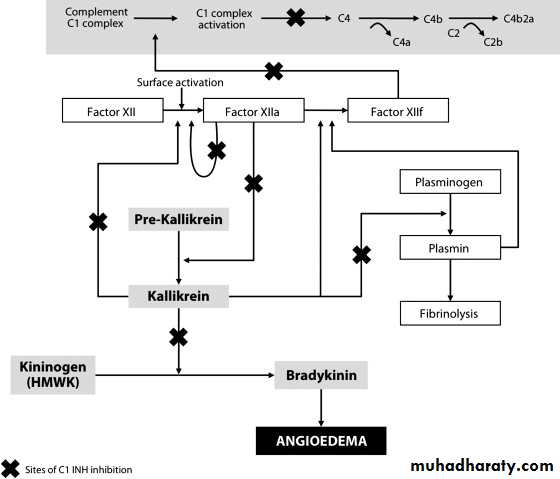
C1 estrase inhibitor is serine protease inhibitor that regulate the (1) Kallikrein-Kinin , (2) fibrinolytic and (3) complement systems
Tranexamic acid may work as C1 INH–sparing agents by freeing up C1 INH from its role within the fibrinolytic pathway, thereby increasing availability to the contact and complement systems