DR.MAHA TALAL
LOCAL ANESTHETICSFunctional consequences of Na+ channel blockade by local anesthetics:
nerves: decrease or abolition of conductionvascular smooth muscle: vasodilatation
heart: decreased excitability (reduced pacemaker activity, prolongation of effective refractory period)central nervous system: increased excitability, followed by generalized depression
Pharmacological effects and toxicities• Effects of local anesthetics on nerve conduction
• Na+ channels are present in all nerves and local anesthetics, at sufficient concentrations, can completely block action potential generation and conduction
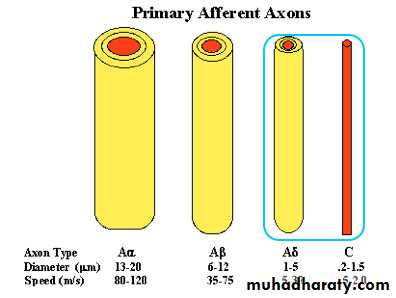
• “differential nerve blockade” – nerve fibres differ markedly in their susceptiblity to conduction blockage by local anesthetics (this is the basis of their clinical use)
• e.g., small, non-myelinated neurons mediating pain are much more susceptible that large, myelinated fibres mediating motor functions
Pharmacological effects and toxicities
Relative size and myelination and susceptibility to blockage by local anesthetics
Fibre type
functiondiameter (µm)
myelination
susceptiblity to LA block
Type A
alpha
proprioception, motor
12-20
heavy
+
beta
touch, pressure
5-12
heavy
++
gamma
muscle spindles
3-6
heavy
++
delta
pain, temperature
2-5
heavy
+++
Type B
preganglionic
<3
light
++++
Type C
dorsal root
pain
0.4-1.2
none++++
Sympathetic block (vasodilatation)
Loss of pain and temperature sensationLoss of proprioception
Loss of touch and pressure sensation
Loss of motor function
Sequence of clinical anesthesia
Pharmacological effects and toxicities• Differential susceptibility of nerves to local anesthetics
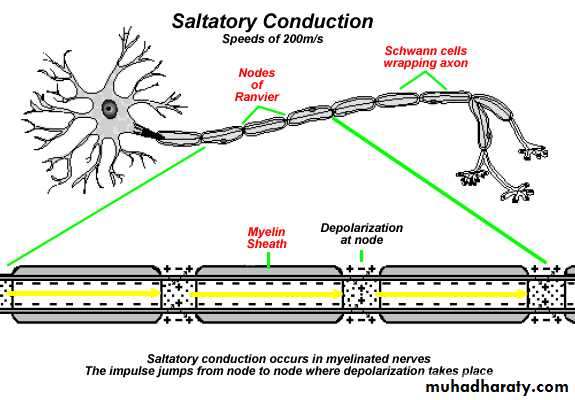
• In neuronal conduction, depolarizing current moves along nodes of Ranvier – 2-3 successive nodes must be blocked to completely impair neuronal conduction
•
•
•
• small fibres have smaller internodal distances - ∴ a shorter length of nerve fibre needs to be blocked to impair conduction as compared to larger nerve fibres
Pharmacological effects and toxicities
•• Illustration of use-dependent local anesthetic neuronal blockade – as stimulation frequency increases from 1 to 25, the downward Na+ current spike is progressively reduced.
• Differential susceptibility of nerves to local anesthetics (cont’d)
• 2. Anesthetic blockade of Na+ channels exhibits “use-dependence” - increased frequency of stimulation increased level of blockade
•
• high stimulation frequency increases # of Na+ channels in the “open” form that preferentially binds anesthetic
• ∴ neurons with high rates of firing (e.g., pain fibres) or ectopic pacemakers in the myocardium will be highly susceptible to blockade by local anesthetics
Pharmacological effects and toxicities Differential susceptibility of nerves to local anesthetics (cont’d)
• In excitable tissues with long action potentials, probability of Na+ channels being in (susceptible) “open” form is increased enhanced susceptibility to blockade by local anesthetics
• e.g., pain fibres have long action potentials (3 millisec) versus motor fibres (0.5 millisec)
• cardiac muscle has prolonged action potentials relative to other excitable tissues - ∴ myocardium highly susceptible to local anesthetics (clinically important)
Pharmacological effects and toxicities
Effects of local anesthetics on vascular smooth muscleBlockade of Na+ channels in vascular smooth muscle by local anesthetics vasodilatation
consequences of vasodilatation:
enhanced rate of removal of anesthetic from site of administration (decreased duration of anesthetic action and increased risk of toxicity)
hypotension (may be intensified by anesthetic-induced cardiodepression)
Pharmacological effects and toxicities
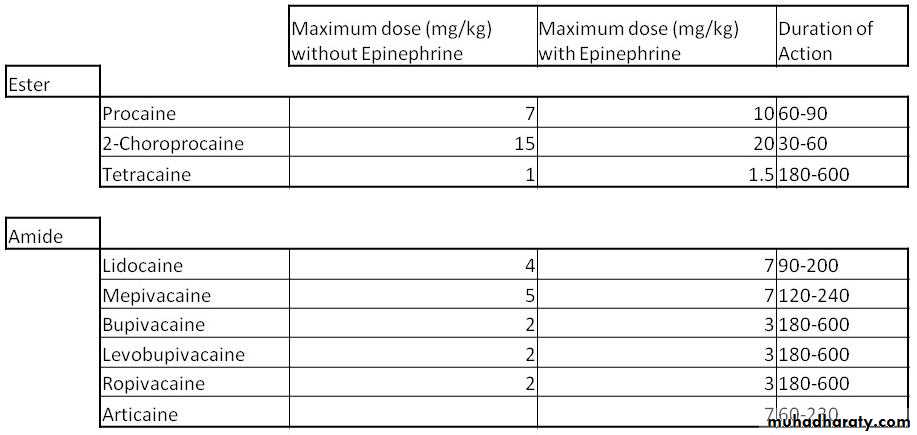
• Effects of local anesthetics on vascular smooth muscle• Anesthetic-induced vasodilatation can be counteracted by the concomitant administration of a vasoconstrictor
• consequences of including vasoconstrictor:
• prolongation of anesthetic action
•
• decreased risk of toxicity
• decrease in bleeding from surgical manipulations
•
•
•
Pharmacological effects and toxicities
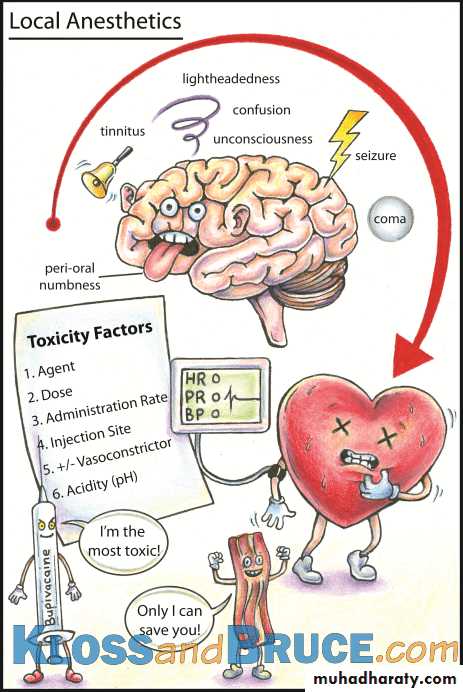
Effects of local anesthetics on heartLocal anesthetics can reduce myocardial excitability and pacemaker activity and also prolong the refractory period of myocardial tissue – this is the basis of the antiarrhythmic effects of local anesthetics
Local anesthetic-induced myocardial depression (compounded by anesthetic-induced hypotension) can also be a manifestation of toxicity and can lead to cardiovascular collapse and even death!
Pharmacological effects and toxicities
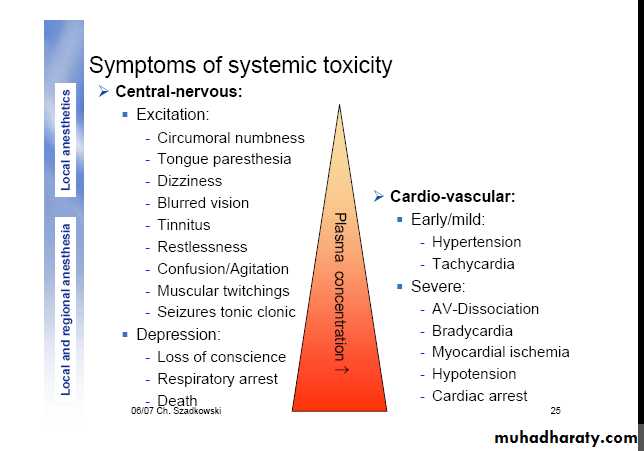
Effects of local anesthetics on CNSAs is the case with CNS depressants generally (e.g., alcohol) local anesthetics (at toxic doses) produce a biphasic pattern of excitation followed by depression
The excitatory phase likely reflects the preferential blockade of inhibitory neurons and effects can range from mild hyperactivity to convulsions)
The subsequent depressive phase can progress to cardiovascular collapse and even death if unmanaged.
COMERCIALLY PREPAREDLOCAL ANESTHESIACONSISTS OF
:Local anesthetic agent (xylocaine, lignocaine 2%)
Vasoconstrictor (adrenaline
Reducing agent (sodium metabisulphite)
Preservative (methylparaben,capryl hydrocuprienotoxin)
Fungicide (thymol)
Vehicle (distillde water,NaCl)
Vasoconstrictors
Two types:Sympathomimetic naturally occurring.
Synthetic polypeptides, Felypressin
Pharmacological effects and toxicities
• Effects of vasoconstrictors on local anesthetic duration
• Adrenaline is the conventional vasoconstrictor included in commercial local anesthetic preparations
• The concentration of adrenaline in these preparations can vary and is expressed as grams/ml (e.g. 1:100,000 = 1 gram/100,000 ml)
•
•
•
•
local anesthetic
adrenaline
duration of anesthesia (min)
lidocaine (2%)
-
5-10
• lidocaine (2%)
1:100,000
60
• lidocaine (2%)
1:50,000
60Vasoconstrictors
Epinephrine: (Adrenaline)
Uses in dentistry:
Local anaesthetic solution.
Gingival retraction cords.
In the ER as life-saving drug in anaphylaxis.
Mechanism of action:
Interact with adrenergic receptors in the vesselsα1 & α2 producing vasoconstriction in skin & MM
β2 stimulation causing vasodilatation in skeletal muscles.
Vasoconstrictors Epinephrine
Blood vessels:Contain α1, α2 and β2 adrenoreceptors in the vessels of the skin, mucous membrane and skeletal muscles.
α1 receptors causes vasoconstriction since they are susceptible to endogenous nor-epinephrine and exogenous epinephrine. Reduce operative bleeding
Vasoconstrictors Epinephrine
α2 receptors are only susceptible to circulating epinephrine.β2 found in the skeletal muscles, and very uncommon in the skin and mucous membrane. β2 stimulation result in vasodilatation, lowering peripheral resistance and a fall in the diastolic blood pressure. (with dental dose)
Vasoconstrictors Epinephrine
Haemostasis:The vasoconstricting effect.
Adrenaline promote platelets aggregation in the early stages.
Fibrinolytic activity compromise clot stability.
Lungs:
Stimulation of β2 receptors in the lung lead to bronchial muscle relaxation, life-saving in bronchial (spasm) constriction during anaphylactic reaction.
Wound healing:
Reduced local tissue oxygen tension.
Epinephrine-induced fibrinolysis.
Vasoconstrictors
Felypressin:It is an analogue of the naturally occurring Vasopressin.
Bind to vasopressin V1 receptor in the vascular smooth muscle producing vaso-constriction and reduce local blood flow.
Less potent than the catecholamines &poorer control of bleeding during operative procedures.
Acts on the venous side rather than the arterial side.
Dose:
0.03 IU/ml (0.54 µg/ml)Benefits of Decreased Absorption
Increased neuronal uptake
Enhances quality of analgesia
Prolongs duration of action
Limits toxic side effects
Produce less blood field operation
Max dose of vasoconstrictors
- Healthy patient approximately0.2mg
- Patient with significant cardiovascular history: 0.04mg
• Max Dose for Vasoconstrictors (CV
patient) =2.22 carpules
• In a healthy adult patient
0.2/0.018=11.1 carpules
Review of literature
24Toxicity Maximum Dosage (mg/lbs) X weight (lbs) = Maximum Total Dosage (mg) Maximum Total Dosage (mg) ÷ mg/carpule = Maximum Number carpules
Example calculations of maximumlocal anesthetic doses for a15-kg (33-lb) child
LidocaineTherefore 2.9 cartridges is the maximum
Pharmacology of Local Anesthetics• Outline
• History
• Chemistry and Structure-Activity Relationships
• Mechanism of Action
• Pharmacological effects and toxicities
• Clinical aspects
Clinical aspects
• Applications of local anesthesia:• nerve block: injected locally to produce regional anesthesia (e.g., dental and other minor surgical procedures)
• topical application: to skin for analgesia (e.g., benzocaine) or mucous membranes (for diagnostic procedures)
• spinal anesthesia: injection into CSF to produce anesthesia for major surgery (e.g., abdomen) or childbirth
• local injection: at end of surgery to produce long-lasting post-surgical analgesia (reduces need for narcotics)
• i.v. infusion: for control of cardiac arrhythmias (e.g., lidocaine for ventricular arrhythmias)
Pharmacology of Local Anesthetics
• Outline
• History
• Chemistry and Structure-Activity Relationships
• Mechanism of Action
• Pharmacological effects and toxicities
• Clinical aspects
Clinical aspects
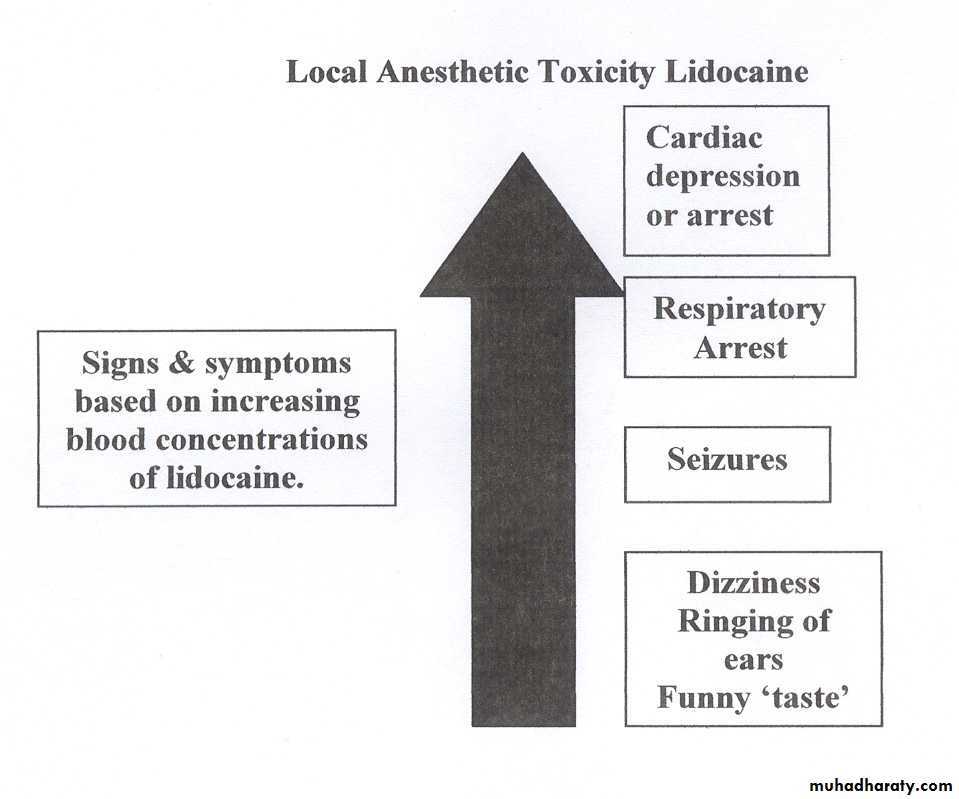
local anesthetic toxicitymost common causes:
inadvertent intravascular injection while inducing nerve block (important to always aspirate before injecting!)rapid absorption following spraying of mucous membranes (e.g., respiratory tract) with local anesthetic prior to diagnostic or clinical procedures
manifestations of local anesthetic toxicity: allergic reactions, cardiovascular and CNS effects
Clinical aspects
local anesthetic toxicity (cont’d)allergic reactions: restricted to esters – metabolized to allergenic p-amino benzoic acid (PABA) (∴ amides usually preferred for nerve block)
cardiovascular: may be due to anesthetic (cardiodepression, hypotension) or vasoconstrictor (hypertension, tachycardia) ∴ monitor pulse/blood pressure
CNS: excitability (agitation, increased talkativeness – may → convulsions) followed by CNS depression (∴ care in use of CNS depressants to treat convulsions - may worsen depressive phase – convulsions usually well tolerated if brain oxygenation maintained between seizures)