OBESITY
TUCOM
Internal Medicine
3rd class
Dr. Hasan. I. Sultan
OBESITY
Learning objectives;
1. Make the definition and classification of obesity
according to body mass index(BMI) formula.
2. Recognize the types of obesity according to
various body fat distribution patterns.
3. Review the pathogenesis of obesity.
4. Understand the causes of obesity.
5. Clarify the complications of obesity.
6. Explain the clinical assessment of obese
patient.
7. List the important investigations of obesity.
8. Explain the management of obesity.

Obesity
Define as
;
A nutritional disorder
in which excess body fat has
been accumulated to the extent
that it may have an adverse
effect on health.
Body Mass Index (BMI) is ≥ 30
kg/m2 .
body mass index (BMI) =
weight/height2 (in kg/m2)

Obesity Classification Based on Body
Mass Index (BMI)
Classification BMI
(kg/m2)
Underweight
<20
Ideal
20-24.9
Overweight
25-29.9
Obese
30-40
Severely obese
>40

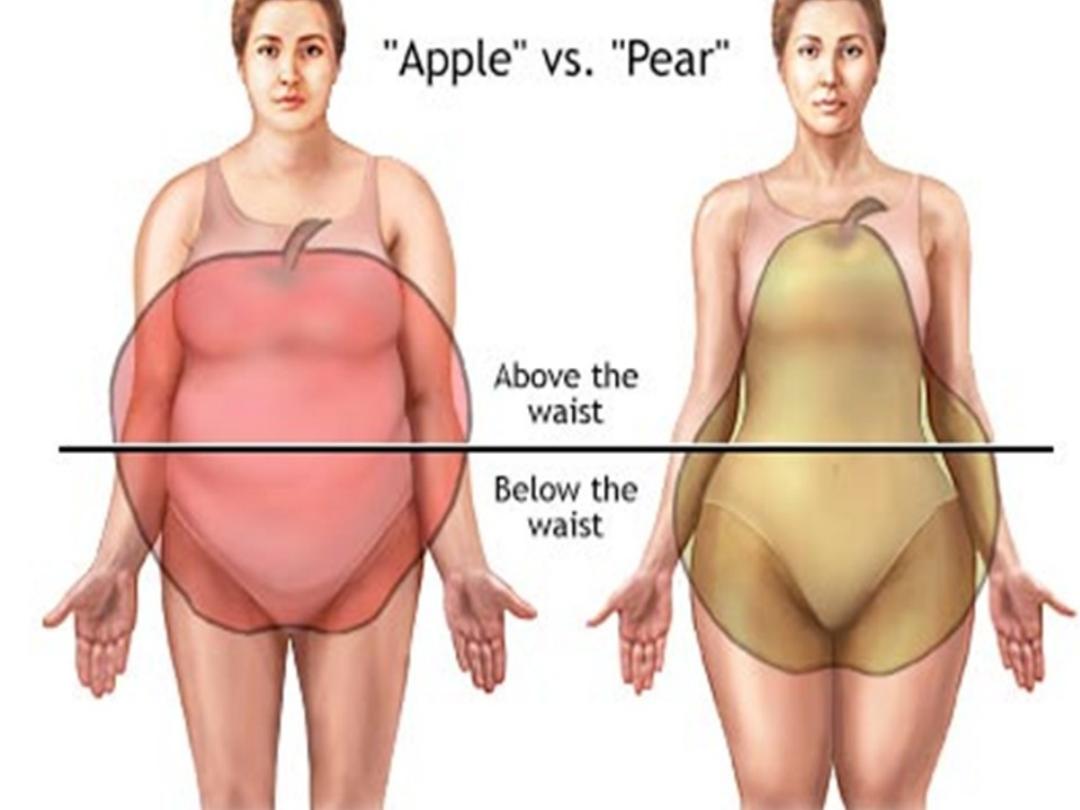
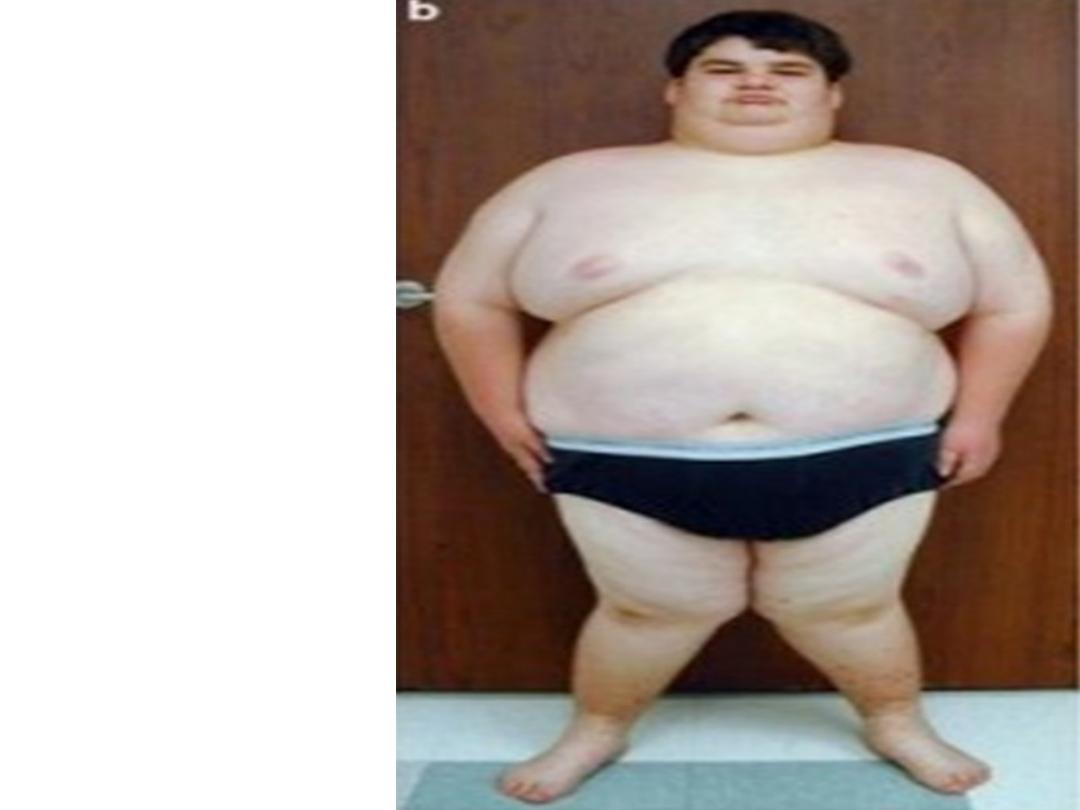
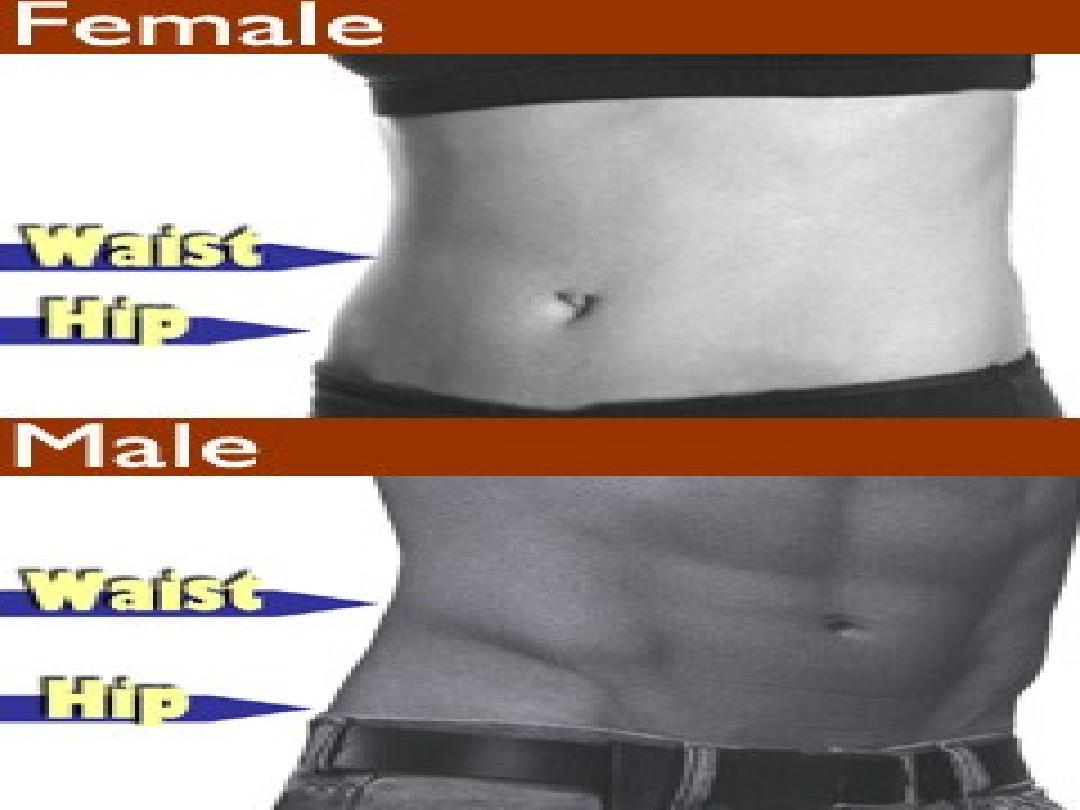
The types of obesity according to body
fat distribution;
1. Intra-abdominal fat accumulation
causes 'central' ('abdominal',
'visceral', 'android' or
'apple-shaped') obesity.
This form
is more common in men and is
more closely associated with type
2 diabetes, the metabolic
syndrome and cardiovascular
disease.
2. Generalised fat accumulation
('gynoid' or 'pear-shaped') obesity

The prevalence of obesity has
increased
∼threefold
within the
last
20 years
and continues to rise.
Obesity has reached epidemic
proportions throughout the world, and
this has also affected people of Arabic
countries, especially those in
higher-income and oil-producing
countries, due to rapid urbanization
and improved living conditions
(changes in food consumption,
socioeconomic status and physical
activity).
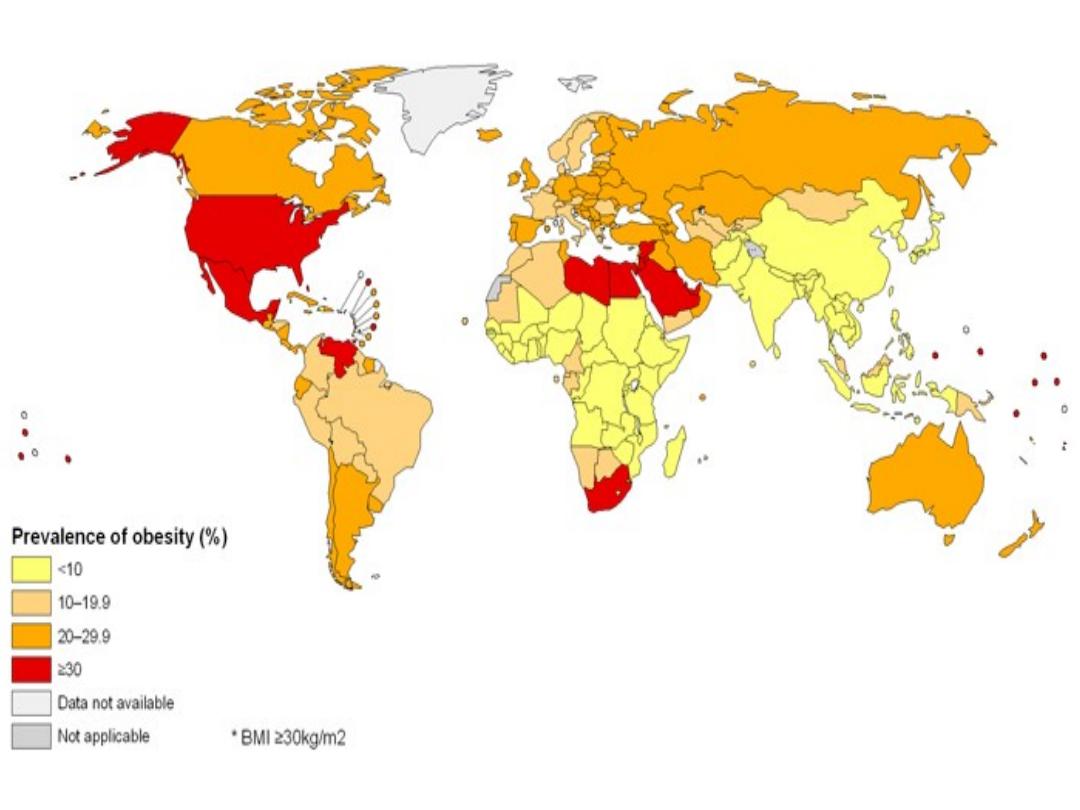
World Health Organization, prevalence of adult
obesity in 2008.
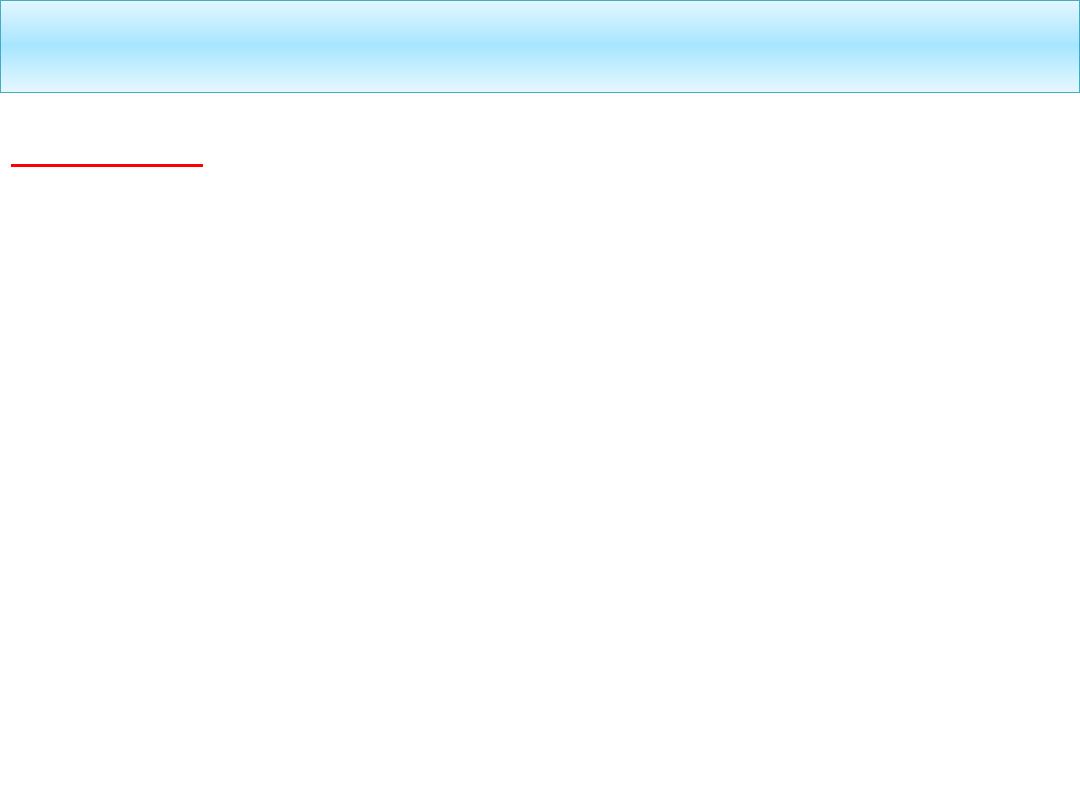
Pathogenesis of obesity
Leptin;
A hormone produced
primarily by fat cells.
The
overfed adipocyte
secretes
leptin,
which circulates and binds to
receptors in the
hypothalamus
,
causing;
1. Release
of
glucagon-like peptide-1
(GLP-1)
(appetite suppresser).
2. Inhibiting
neuropeptide Y (NPY)
(stimulator of appetite).
GLP-1
NPY
• Low leptin level
signal starvation
and stimulate feeding.
• Congenital leptin deficiency
lead to
hyperphagia and severe obesity.
Insulin;
Stimulates
lipoprotein lipase
permitting uptake of dietary fat by
the adipocyte.
• Leptin suppresses insulin
production.
• Thus common forms of human
obesity actually appear to be
leptin
resistant
.
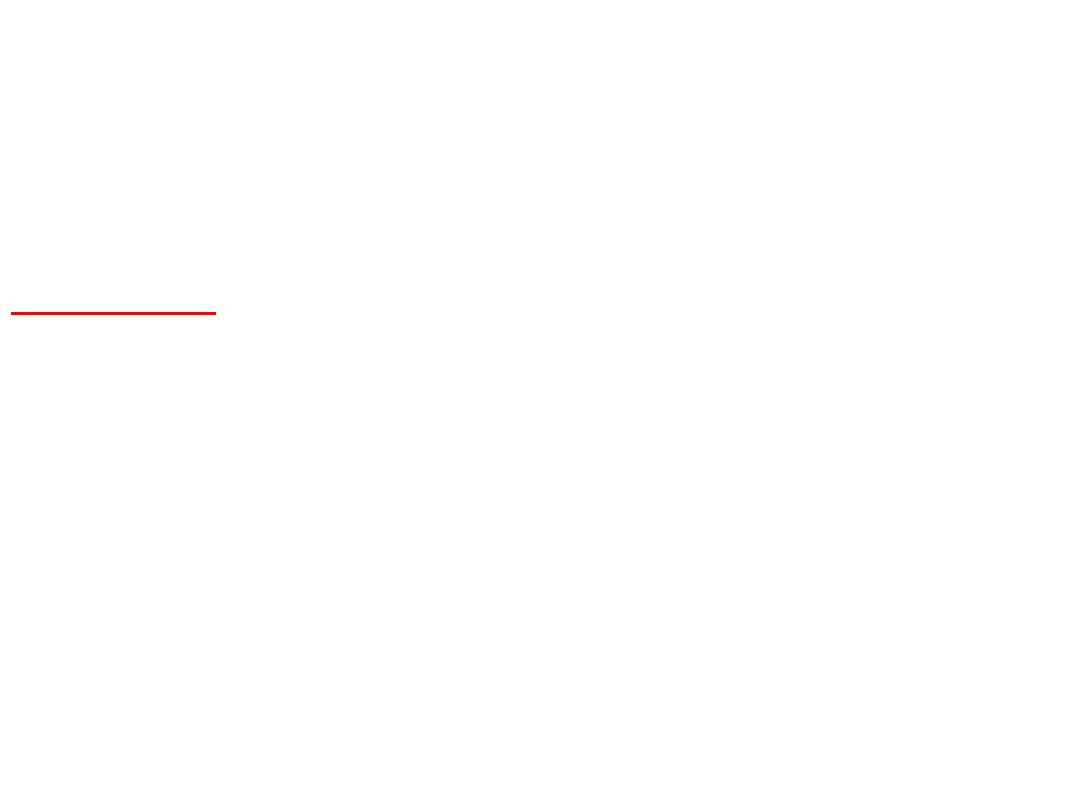
Aetiology
Obesity result from discrepancy between energy
consumption and expenditure. It is caused by long
term positive energy balance.
Aetiology
1-Role of genetic and
environment;
Obesity= Gene + availability of
palatable food + sedentary lifestyle.
Majority of human obesity is related
to the combination of
polygenic
susceptibility traits and
environmental conditions.
a- Polygenic disorder;
b- Single gene disorders; cause
severe childhood obesity;
Prader-Willi and
Lawrence-Moon-Biedl syndromes.
Prader- Willi
Syndrome:
short stature,
poor motor
skills, weight
gain and
underdeveloped
sex organs.

Lawrence-Moon-Biedl syndromes: Short stature, obesity,
polydactyly, retinal disorders, and hypogonadism.

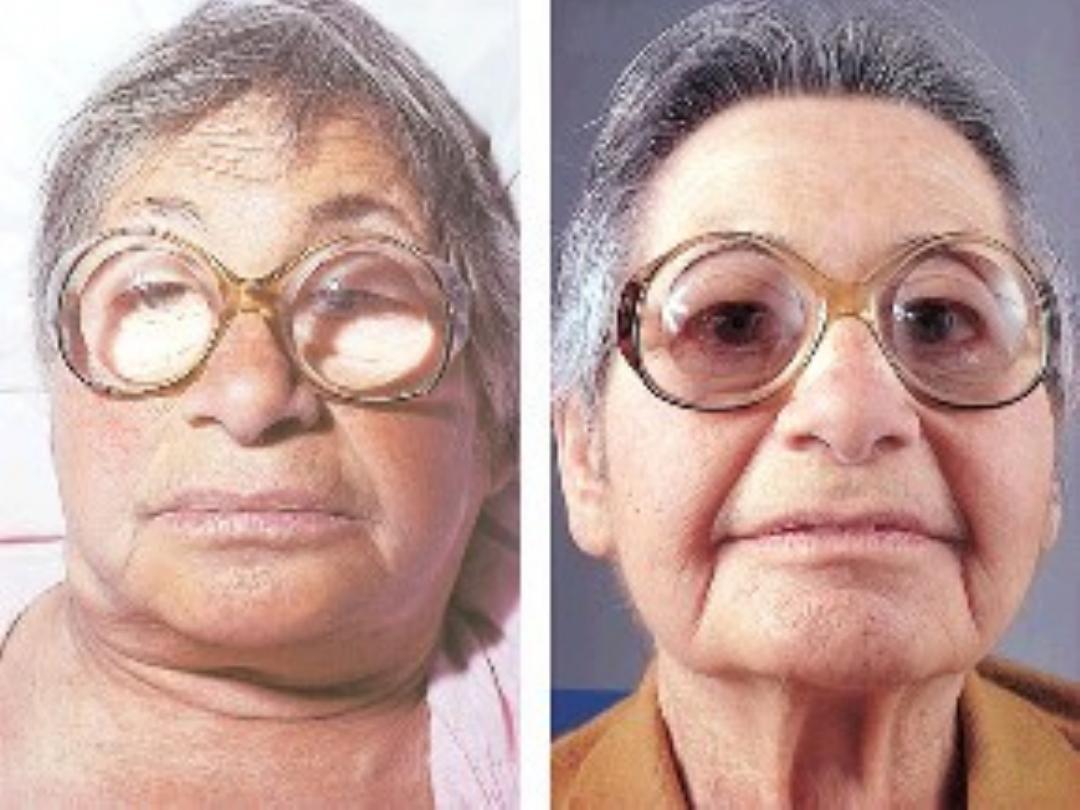
2- Reversible causes of obesity;
A- Endocrine factors
• Hypothyroidism
• Hypothalamic tumours or injury
• Cushing's syndrome
• Insulinoma
B- Drug treatments
• Tricyclic antidepressants
• Corticosteroids
• Sulphonylureas
• Sodium valproate
• Oestrogen-containing contraceptive pill
• β-blockers

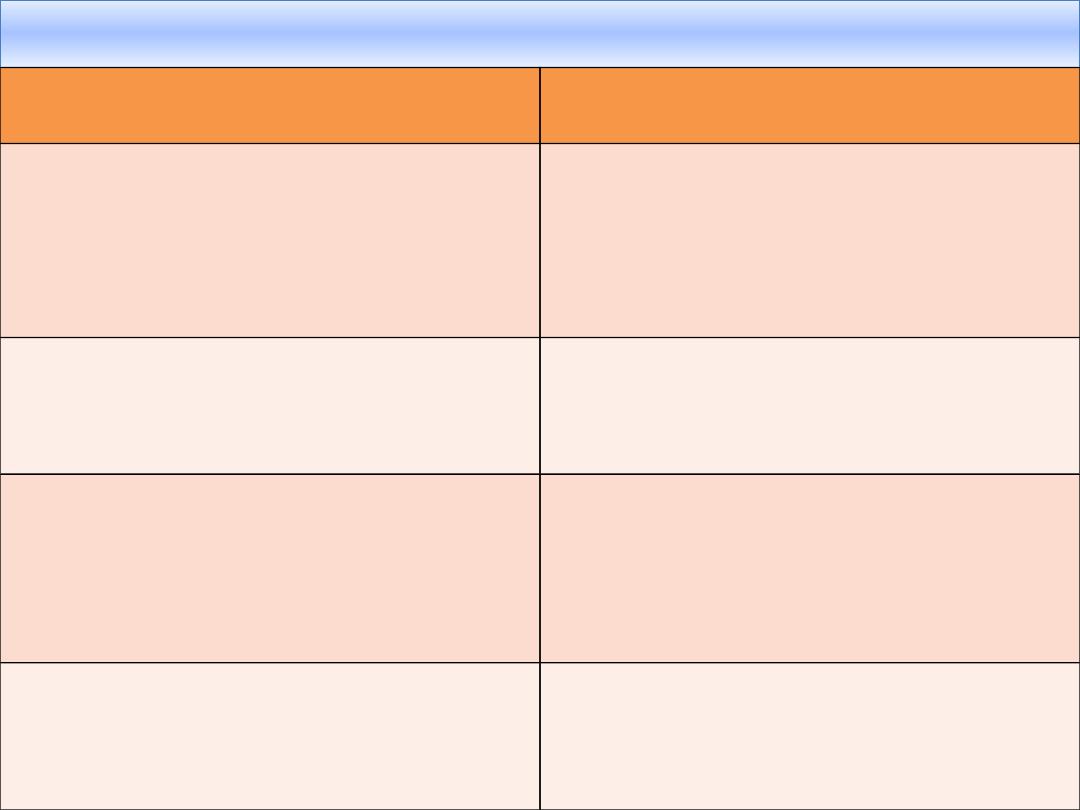
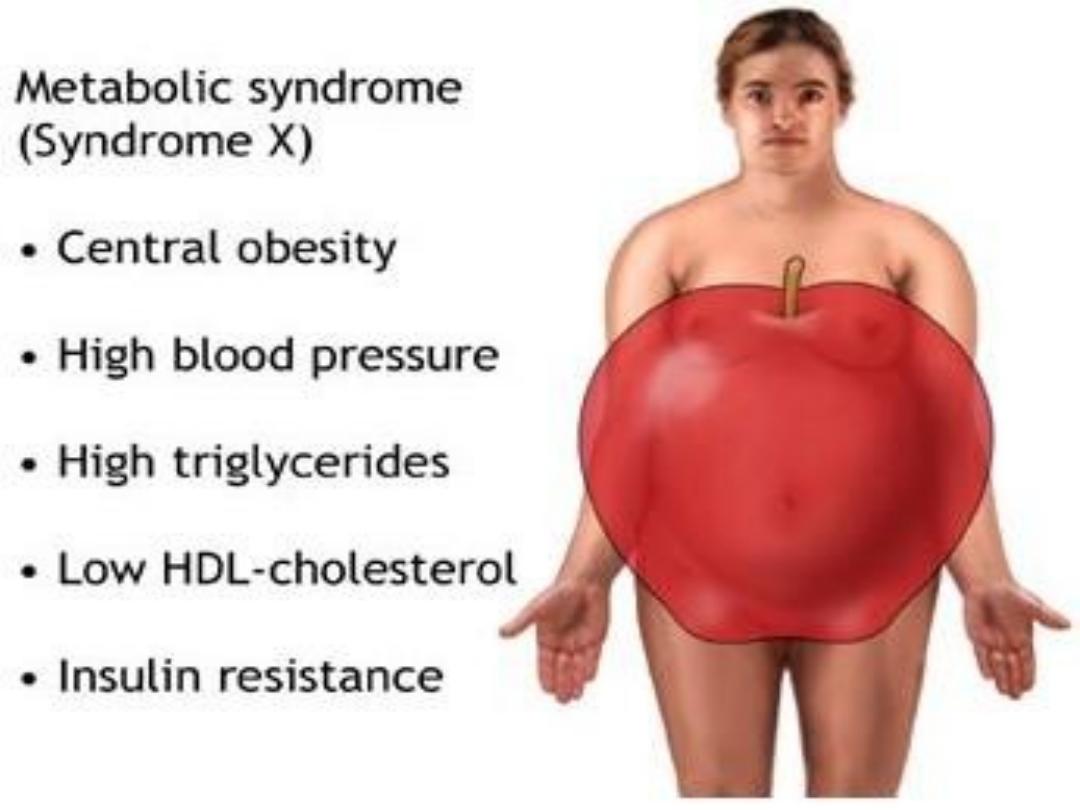
Complications
of obesity
Risk factors
Outcomes
'Metabolic syndrome'
Type 2 diabetes
Hypertension
Hyperlipidaemia
Coronary heart disease
Stroke
Diabetes complications
Liver fat
accumulation
Non-alcoholic
steatohepatitis
Cirrhosis
Restricted ventilation
Exertional dyspnoea
Sleep apnoea
Respiratory failure
(Pickwickian syndrome)
Mechanical effects of
weight
Urinary incontinence
Osteoarthritis
Varicose veins
Increased
peripheral steroid
interconversion in
adipose tissue
Hormone-dependent
cancers (breast,
uterus)
Polycystic ovary
syndrome (infertility,
hirsutism)
Others
Psychological morbidity
(low self-esteem,
depression)
Socioeconomic
disadvantage (lower
income)
Gallstones
Colorectal cancer
Skin infections (groin
and submammary
candidiasis;
hidradenitis)


Clinical assessment
1- History;
dietary history:
food consumption, binge
eating, nocturnal eating, alcohol consumption. Any
symptoms related to weight gain e.g. poor sleep or
snoring or dyspepsia. Taking relevant
drugs
•
Underlying disorder
such as hypothyroidism or Cushing's
syndrome.
•
Complications
of obesity
•
Family history
of obesity, DM, HT, or ischemic heart
disease.
•
Impact of obesity on the patient's life and work
. Is his
work active or sedentary. Is there regular exercise? Are
there any psychological problems as depression?

2- Examination and
measurements;
•
BMI =kg/m2
Example: adult Wt 70 kg and Ht 1.75
m the BMI is =70/1.752 = 22.9 .
•
Waist circumference
of
> 102 cm in men = obesity
> 88 cm in women = obesity
•
Waist-to-hip circumference ratio
> 1 in men = android
obesity
> 0.9 in women = android obesity



• Anthropometry;
skin fold thickness.
By using calipers, typically at the
forearm.
• Densitometry;
under water
weighting.
• B.P;
with large cuff.
• Search of
complications.
• Look for signs of hypothyroidism or
Cushing's syndrome.
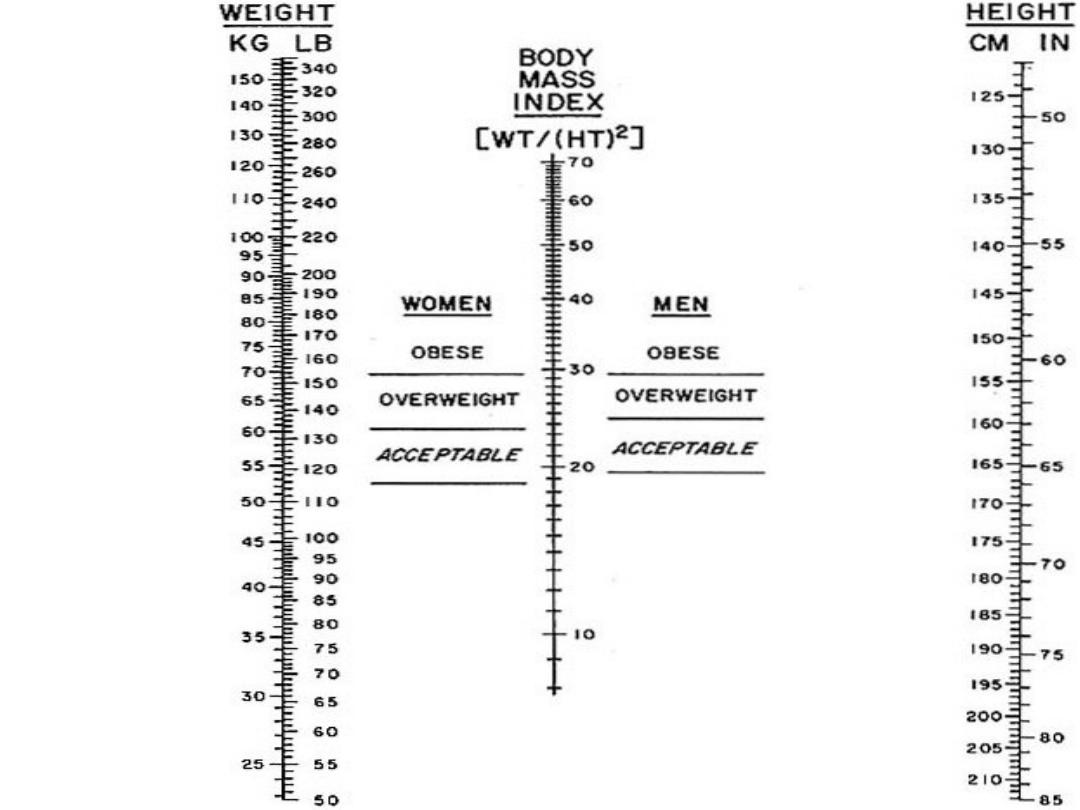
Nomogram
for
determining
body mass
index. To
use this
nomogram,
place a ruler
or other
straight
edge
between the
body weight
(without
clothes) in
kilograms or
pounds
located on
the
left-hand
line and the
height
(without
shoes) in
centimeters
or inches
located on
the
right-hand
line.

Investigations
• Blood glucose and a serum lipid
profile
• Serum transaminases
• Thyroid function tests
• Overnight dexamethasone
suppression test or 24-hour urine
free cortisol
• ECG

Management
1-Lifestyle advice;
A-avoid of the 'obesogenic'
environment
.
2-Decreasing energy
expenditure
↑ Car ownership
↓ Walking to school/work
↑ Automation; ↓ manual
activities
↓ Sports in schools
↑ Time spent on video
games and watching TV
↑ Central heating
Obesogenic
environment
1-Increasing
energy intake
↑ Portion sizes
↑ Snacking and loss
of regular meals
↑ Energy-dense food
(mainly fat)




B- Changes in eating behavior;
avoidance of snacking, and take
regular meals to encourage satiety.
Adequate hydration with meals helps
to limit calorie intake by causing
gastric distension.
C- Maximize their physical activity;
e.g. walking rather than driving.
2- Weight loss diets;
To maintains balance of nutrients and
suppress hunger
Low-calorie diet therapy for
obesity
Diet
%
carbohydr. % fat
% protein
Normal
50
30
15
Moderate
fat
60
25
15
Low
carbohydr
ate
10
60
30
High
protein
43
30
27
Low fat
70
13
17

Note;
•
The goal is to lose ∼0.5 kg/week.
•
There is no role for starvation diets
--a risk of sudden death.
3- Drugs;
No role for diuretics, or
thyroxine
A- Orlistat;
Inhibits pancreatic lipases
-- decreases hydrolysis of ingested
dietary fat and absorption by ∼30%.
Side-effects include malabsorption of
fat and fat soluble vitamins.

B- Sibutramine;
Reduces food intake
through β1-adrenoceptor and
serotonin receptor agonist activity in
the central nervous system.
Side-effects include dry mouth,
constipation, insomnia and increase
blood pressure.
Drug therapy is usually reserved
for patients with high risk of
complications from obesity.


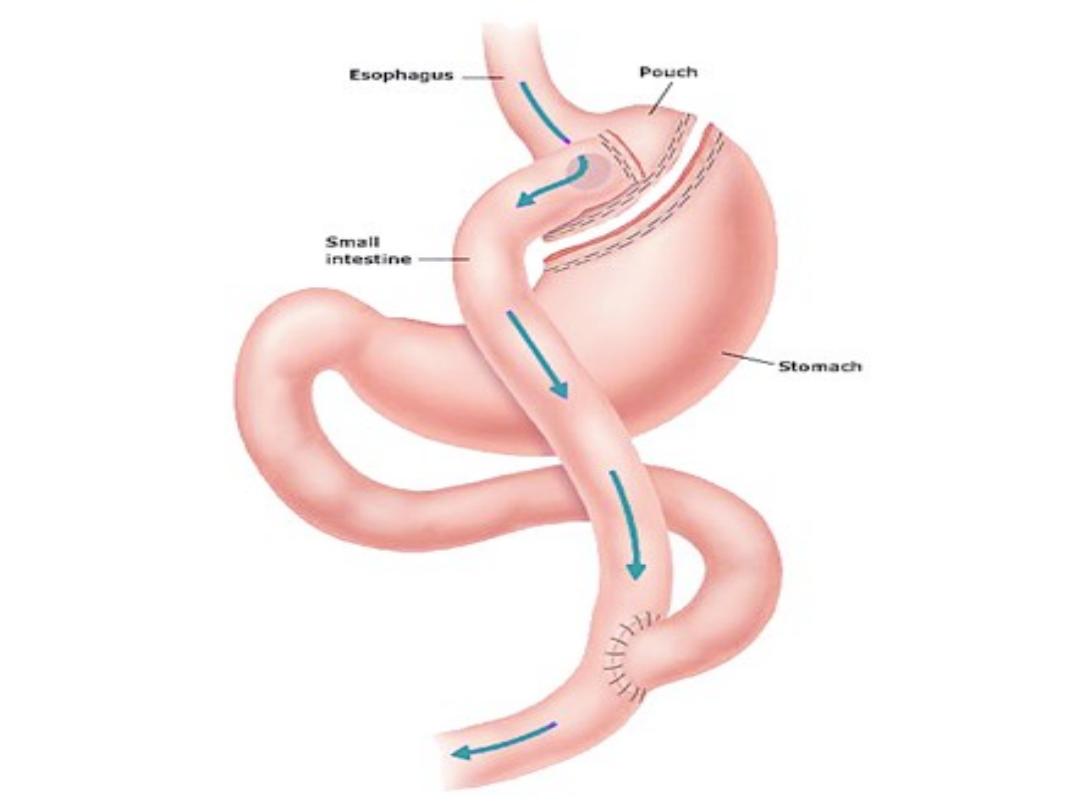
4-Surgery ;
'Bariatric' surgery to
reduce the size of the stomach is by
far the most effective long-term
treatment for obesity.
In whom have very high risks of
complications of obesity and drug
therapy has been ineffective.
5-Treatment of additional risk
factors;
Smoking, excess alcohol consumption,
diabetes mellitus, hyperlipidemia and
hypertension.

Quiz
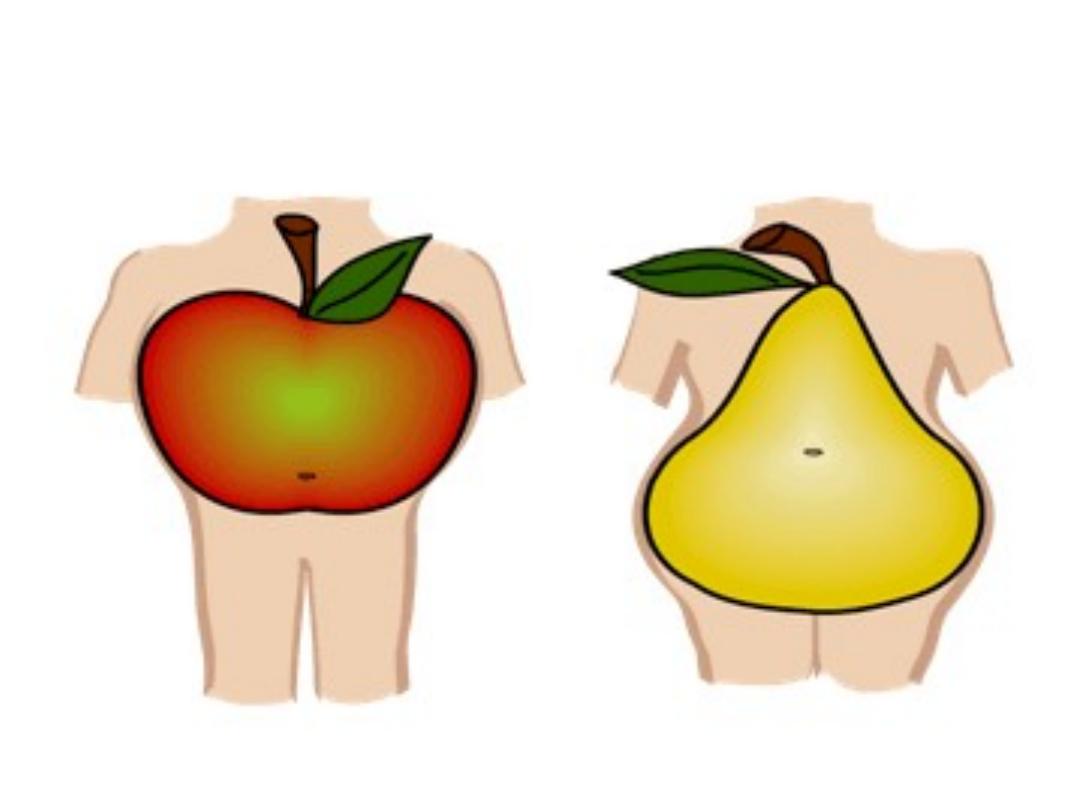
What are the difference between
figure A and B regarding obesity
Figure A
Figure B
THANKS
