NAUSEA
VOMITING
JAUNDICE
TUCOM
Internal Medicine
3rd year
Dr. Hasan.I.Sultan
NAUSEA & VOMITING
1. Make a definition of vomiting,
nausea and regurgitation.
2. Clarify the mechanism of vomiting.
3. List the causes of vomiting.
4. Understand the examination points
in patient with vomiting.
5. List the complications of vomiting
6. Outline the treatment of nausea
and vomiting.
Learning objectives;

VOMITING
• Vomiting;
Is a forcible ejection of gastric contents, due to
synchronous contraction of the diaphragm, intercostal muscles
and abdominal muscles, raises intra-abdominal pressure with
relaxation of the lower oesophageal sphincter.
Is a highly
integrated and complex reflex involving both autonomic and
somatic neural pathways.
• Nausea;
Is the subjective feeling of a need to vomit.
• Regurgitation;
the effortless passage of gastric contents into
the mouth.
• Projectile vomiting;
refers to vomiting that is sudden, usually
without nausea, and so vigorous that the vomit is forcefully
projected to a distance. Projectile vomiting is associated with
increased intracranial pressure or pyloric obstruction.
Mechanisms;
Vomiting is coordinated by the brain stem and is effected by
neuromuscular responses in the gut, pharynx, and thoracoabdominal wall
Activators of Emesis;
act at several sites.
1. Cerebral cortex;
by unpleasant thoughts or smells
2. Cranial nerves;
after gag reflex activation
3. Postrema;
a medullary nucleus, responds to blood borne emetic stimuli
and is termed the
chemoreceptor trigger zone
. Many emetogenic drugs act
on the area postrema, as do bacterial toxins and metabolic factors
produced during uremia, hypoxia, and ketoacidosis,
by activation of 5-HT3,
M1, H1, and dopamine D2 receptor subtypes
4. Labyrinthine apparatus;
motion sickness and inner ear disorders,
by
activation of cholinergic muscarinic M1 and histaminergic H1 receptors.
5. Gastric irritants;
such as cytotoxic agents stimulate gastroduodenal vagal
afferent nerves
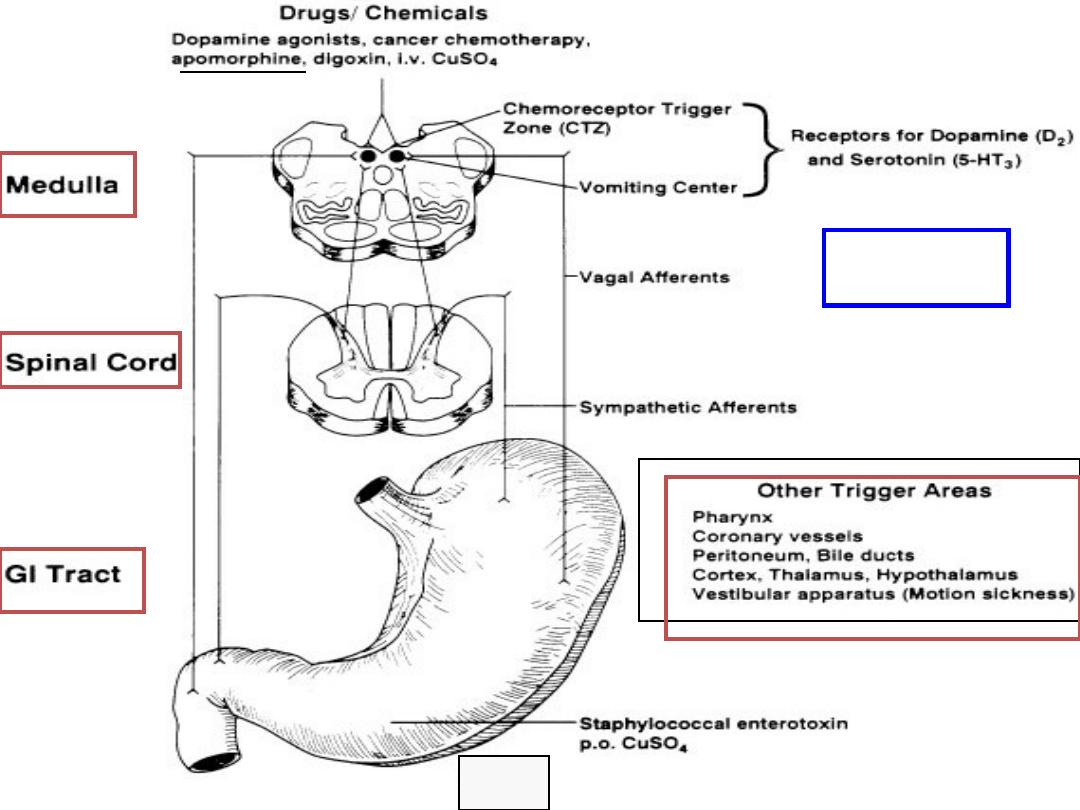
VOMITING
PATHWAYS
Ipecac syrup
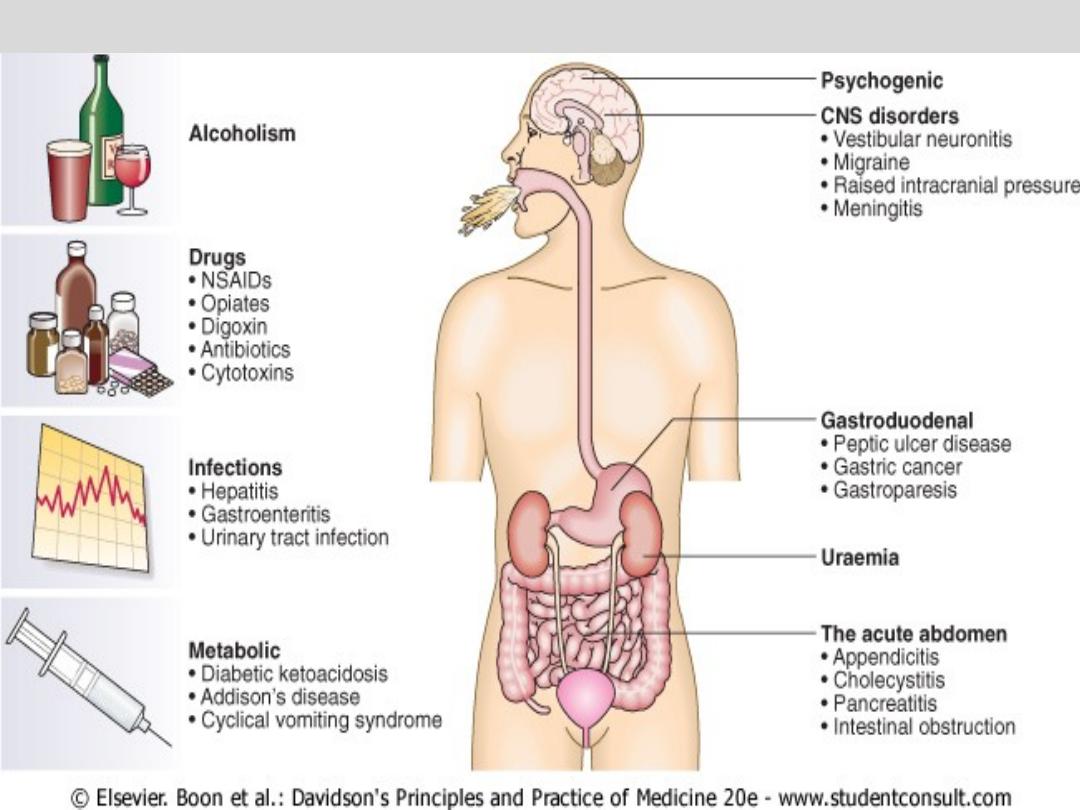
The major causes of vomiting

Examination;
• May reveal signs of dehydration, fever
and infection.
• Evidence of abdominal masses, peritonitis
or intestinal obstruction must be sought.
• Neurological signs including
papilloedema, nystagmus, photophobia
and neck stiffness.
• Other findings may suggest alcoholism,
pregnancy or bulimia as the underlying
diagnosis.
• The diagnostic approach will be dictated
by the history and examination
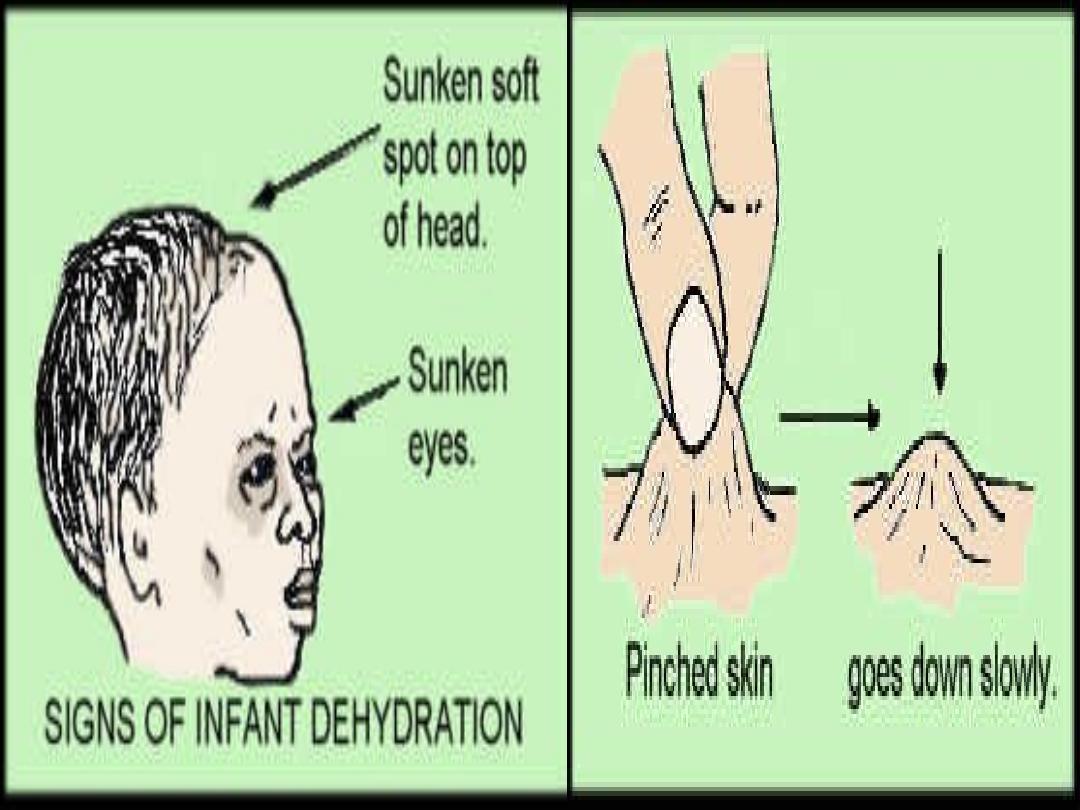
Complications of vomiting
1. Fluid and electrolyte imbalances;
Dehydration, metabolic alkalosis,
hypokalemia and prerenal
azotemia.
2. Nutritional deficiencies
3. Aspiration pneumonia
4. Mallory-Weiss tears
5. Esophageal rupture
Treatment of nausea and vomiting
1. Treat complications regardless of
cause e.g., replace salt, water,
potassium losses.
2. Identify and treat underlying cause,
whenever possible.
3. Relief the symptoms (nausea and
vomiting).
4. Use preventive measures when
vomiting is likely to occur (e.g.,
cancer chemotherapy, parenteral
opiate administration).
Drugs for treatment of nausea
and vomiting
A- Antiemetic agents;
1. Antihistaminergic; Dimenhydrinate, meclizine ---
esp. for
motion sickness, inner ear disease.
2. Anticholinergic; Scopolamine ---
esp. for motion sickness,
inner ear disease.
3. Antidopaminergic; Prochlorperazine ---
esp. for
medication-, toxin-, or metabolic-induced emesis.
4. 5-HT3 antagonist; Ondansetron, granisetron ----
esp. for
chemotherapy- and radiation-induced emesis,
postoperative emesis
5. Tricyclic antidepressant; Amitriptyline, nortriptyline ---
esp. for chronic idiopathic nausea, functional vomiting.
B- Prokinetic agents;
1. Antidopaminergic;
Metoclopramide, Domperidone ---
for gastroparesis.
2. Motilin agonist; Erythromycin ---
for gastroparesis.
C- Special settings;
1- Benzodiazepines; Lorazepam ---
Anticipatory nausea and vomiting
with chemotherapy.
2-
Glucocorticoids;
Methylprednisolone, dexamethasone
---
for chemotherapy-induced emesis
JAUNDICE
1. Define jaundice.
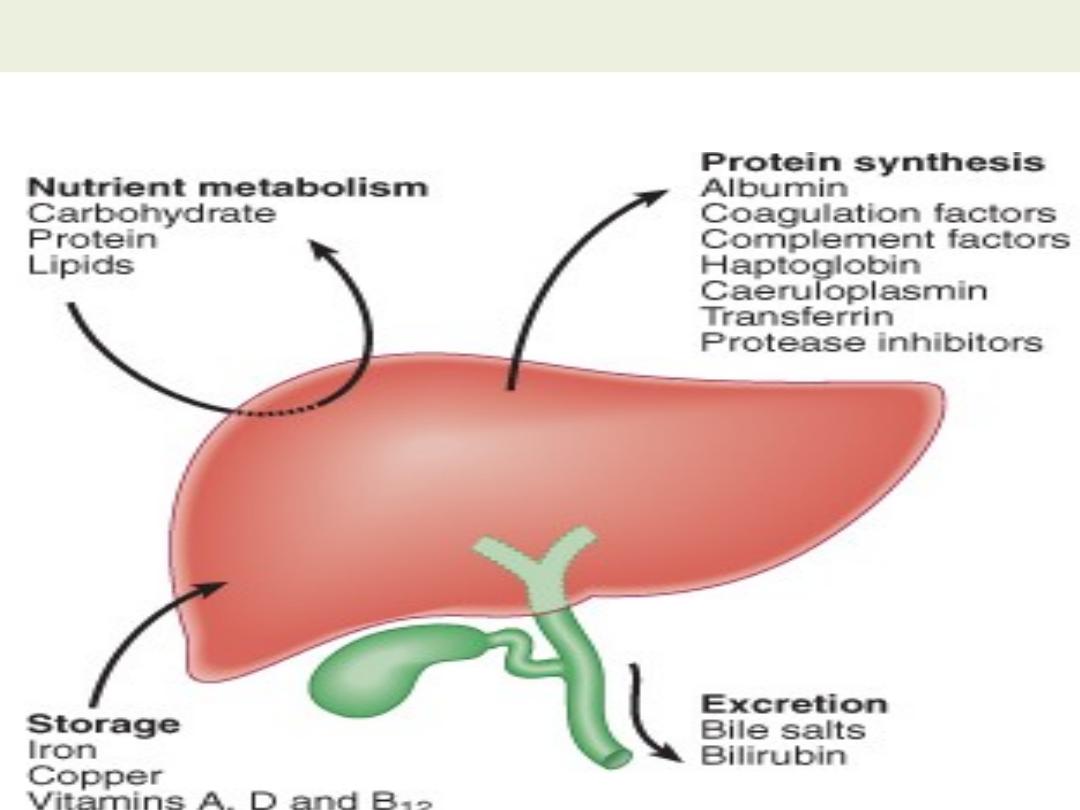
2. Clarify the normal function of the liver.
3. Understand the mechanism of bilirubin
metabolism.
4. Understand the concept of haemolytic jaundice.
5. Recognize the causes of congenital
non-haemolytic hyperbilirubinaemia.
6. Describe the concept of hepatocellular jaundice.
7. Recognize the concept of cholestatic jaundice.
8. List the important investigations of jaundiced
patient.
Learning objectives;
JAUNDICE
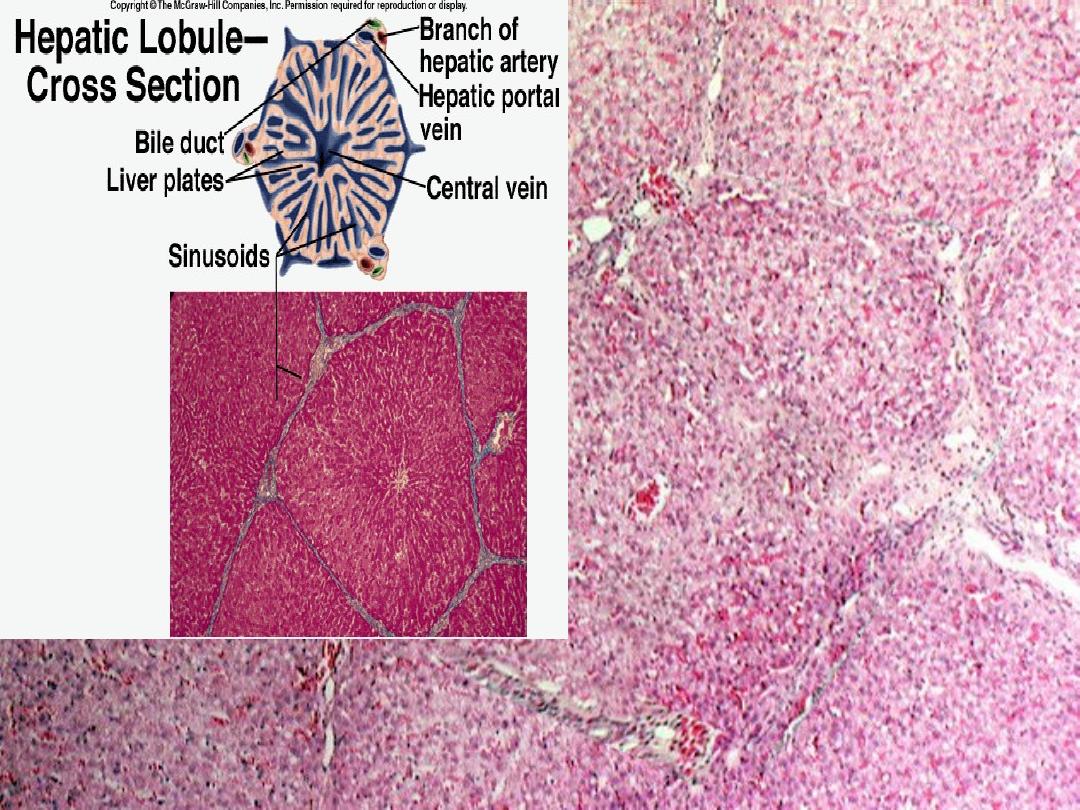
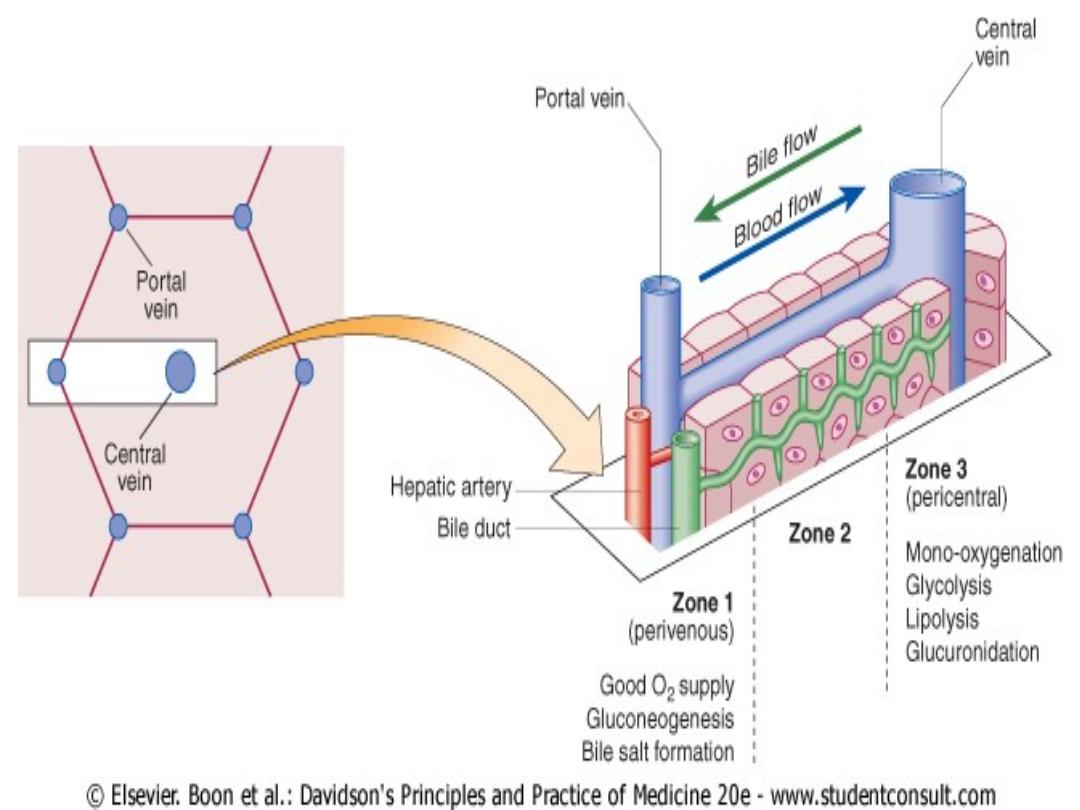
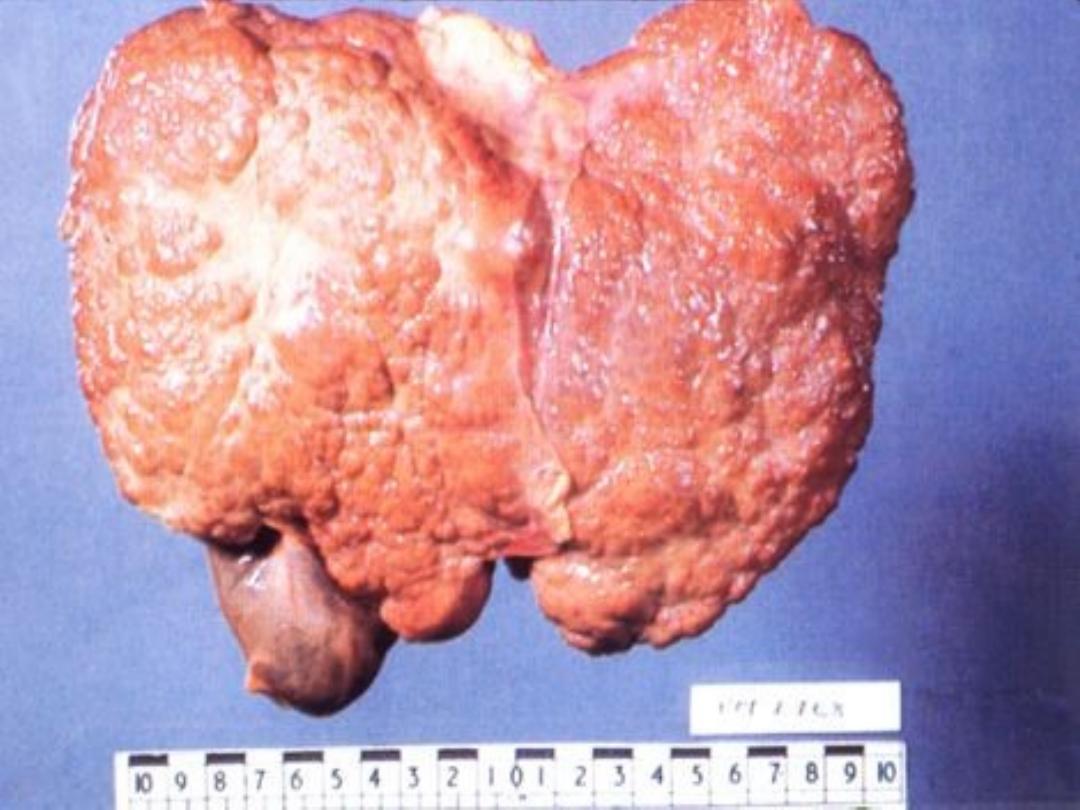
The liver is the largest organ in the body and
performs many important functions.

• weighing 1.2-1.5 kg.---divided into
the left and right lobes --- divided
into a total of eight segments ---
lobules --- The functional unit of
the liver is the hepatic acinus .
LIVER FUNCTION TESTS USED TO
ASSESS LIVER DISEASE
1. Bilirubin
2. Aminotransferases
3. Alkaline phosphatase
4. Gamma-glutamyl transferase
5. Albumin
JAUNDICE
• Jaundice refers to the yellow appearance of the skin,
sclerae and mucous membranes resulting from an
increased bilirubin concentration in the body fluids.
• It is usually detectable clinically when the plasma
bilirubin exceeds 50 μmol/l (∼3 mg/dl). Normal range
(0.5 to 1.0 mg/dl) (5 mmol/l to 17 mmol/l).
• Serum bilirubin are best detected by examining the
sclerae, which have a particular affinity for bilirubin
due to their high elastin content.
• More difficult if the examining room has fluorescent
lighting.
• A second place to examine is underneath the tongue.

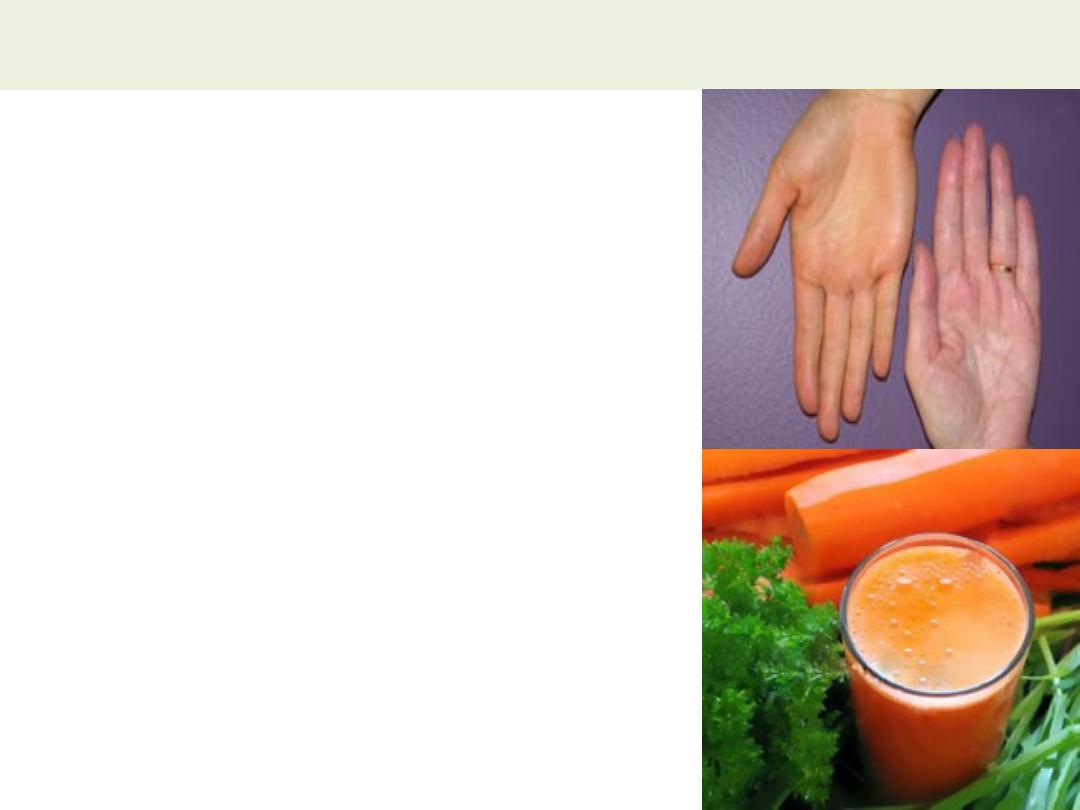
Differential diagnosis for yellowing of the skin
1- Carotenoderma;
Is the
yellow color of skin (but
not sclerae) by the
presence of carotene; it
occurs in healthy
individuals who ingest
excessive amounts of
vegetables and fruits that
contain carotene, such as
carrots, leafy vegetables,
and oranges.
2- Drug;
Quinacrine
3- Excessive exposure to
phenols.
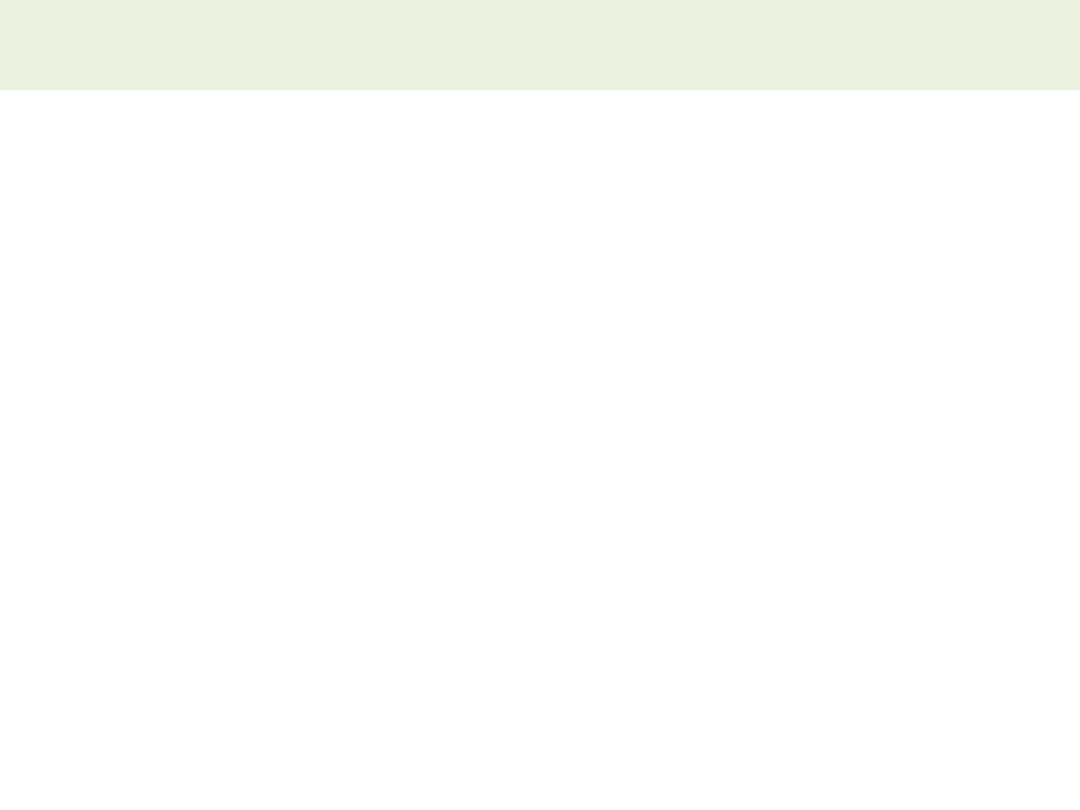
Bilirubin metabolism
• Between 425 and 510 mmol (250-300
mg) of unconjugated bilirubin is
produced from the catabolism of
haem every day
• Bilirubin in the blood is normally
almost all
unconjugated
and,
because it is not water-soluble, is
bound to albumin and does not pass
into the urine.
• Unconjugated bilirubin is
conjugated
by glucuronyl transferase, into
bilirubin mono- and diglucuronide. Is
water-soluble and present in urine.
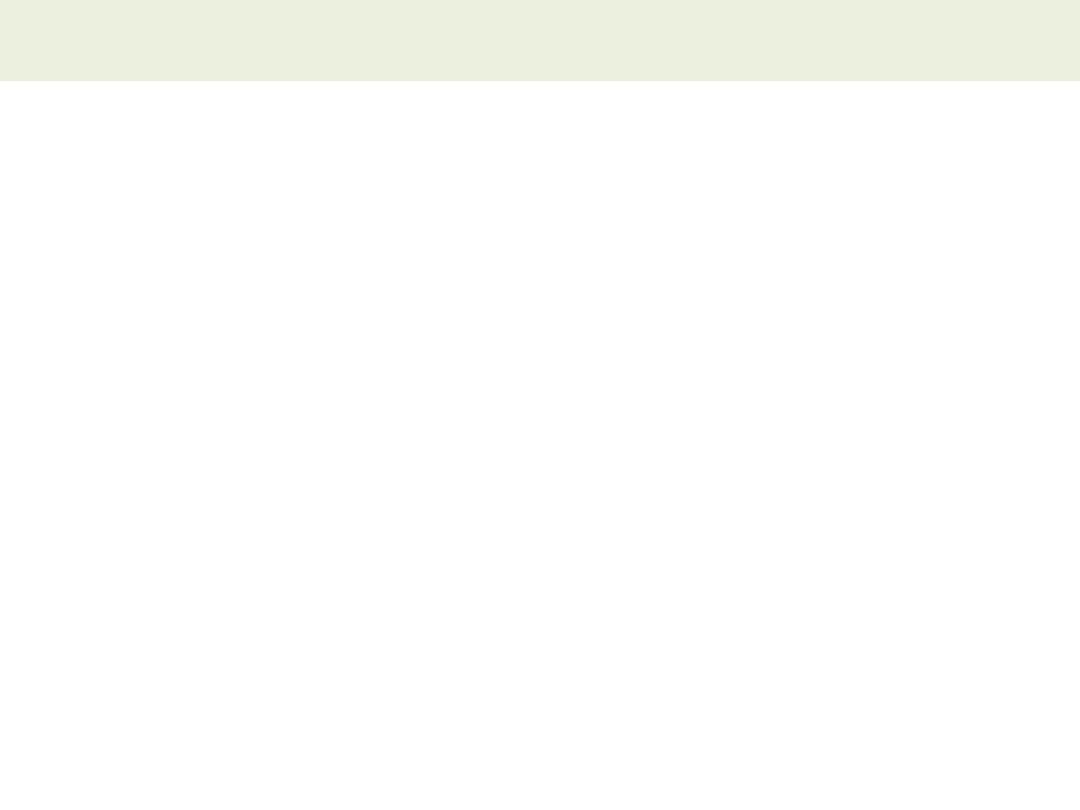
HAEMOLYTIC JAUNDICE
• Results from increased destruction of red blood
cells or their precursors in the marrow.
• Jaundice is usually mild.
• No stigmata of chronic liver disease
• Normal-coloured stools, and urine, but urine to
turn dark on standing as urobilin is formed.
• Pallor due to anaemia, and splenomegaly
• Plasma bilirubin less than 100 μmol/l (∼6 mg/dl)
and the LFTs are normal. Unconjugated
hyperbilirubinaemia
• Blood film show = haemolytic anaemia

CONGENITAL NON-HAEMOLYTIC
HYPERBILIRUBINAEMIA
Syndrome
Inheritance
Abnormality
Clinical
features/treatme
nt
UNCONJUGATED HYPERBILIRUBINAEMIA
Gilbert's
Autosomal
dominant
↓ Glucuronyl
transferase
Mild jaundice,
especially with
fasting
↓ Bilirubin uptake No treatment
necessary
Crigler-Najjar
Type I
Autosomal
recessive
Absent glucuronyl
transferase
Rapid death in
neonate
(kernicterus)
Type II
Autosomal
dominant
↓↓ Glucuronyl
transferase
Presents in
neonate
Phenobarbital,
ultraviolet light or
liver transplant as
treatment
CONJUGATED HYPERBILIRUBINAEMIA
Dubin-Johnson
Autosomal
recessive
↓ Canalicular
excretion of
organic anions
including bilirubin
Mild
No treatment
necessary
Rotor's
Autosomal
dominant
↓ Bilirubin uptake Mild
↓ Intrahepatic
binding
No treatment
necessary
HEPATOCELLULAR JAUNDICE
•
Results from an inability of the liver
to transport bilirubin into the bile,
occurring as a consequence of
parenchymal liver disease
•
The concentrations of both
unconjugated and conjugated
bilirubin in the blood increase.
•
In addition, swelling of cells and
oedema resulting from the disease
itself may cause obstruction of the
biliary canaliculi (sever disease).
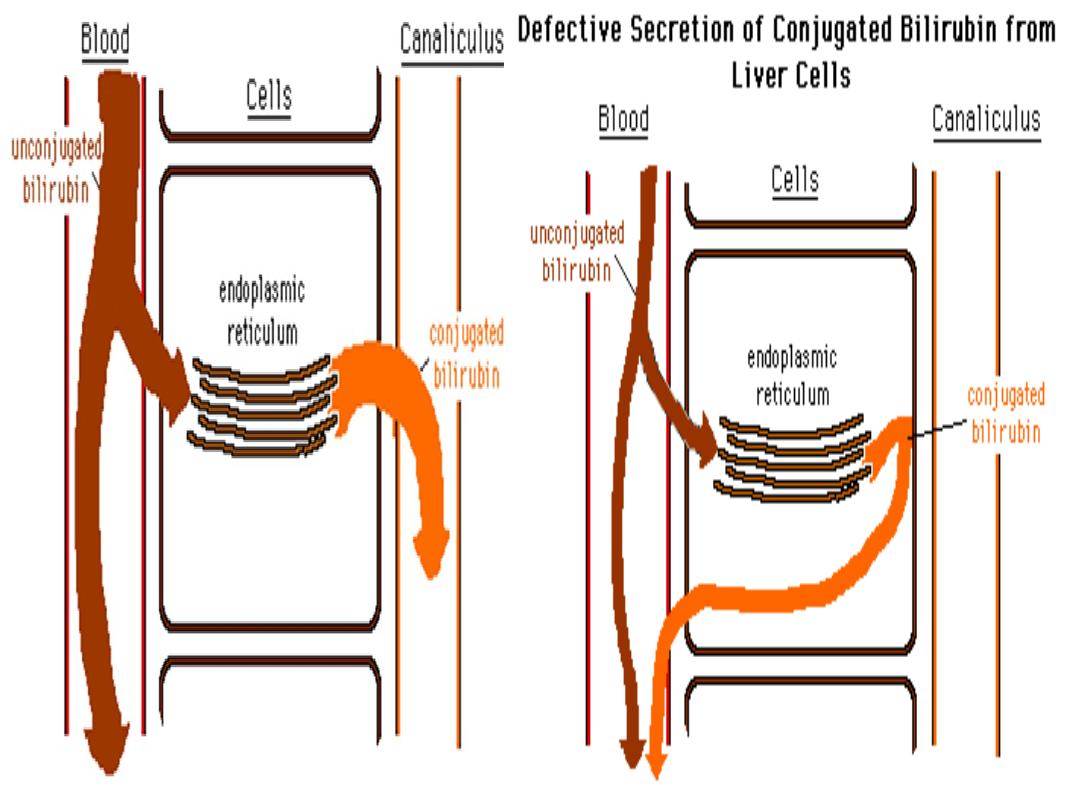
CHOLESTATIC JAUNDICE
1- Intrahepatic;
Primary biliary cirrhosis
Primary sclerosing
cholangitis
Alcohol
Drugs
Viral hepatitis
Autoimmune hepatitis
Cystic fibrosis
Severe bacterial infections
Post-operative
Hodgkin lymphoma
Pregnancy
Benign recurrent
intrahepatic cholestasis
Conjugated bilirubin is unable to enter the bile
canaliculi and passes back into the blood.
Aetiology;
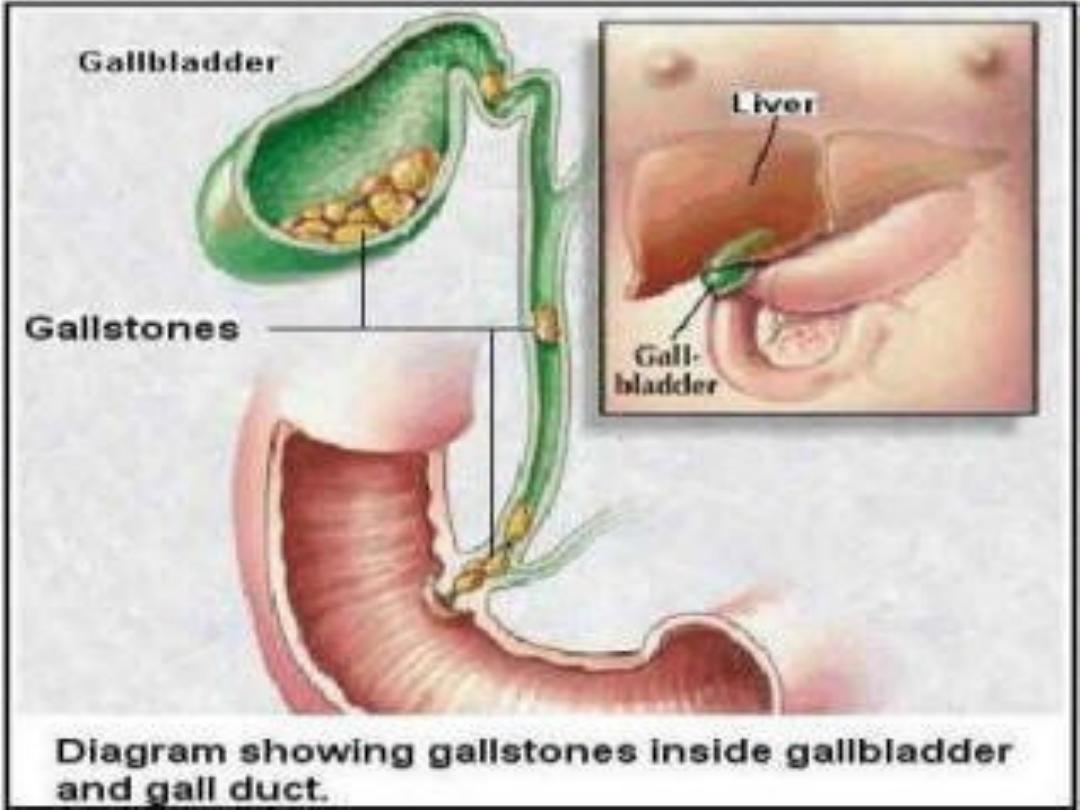
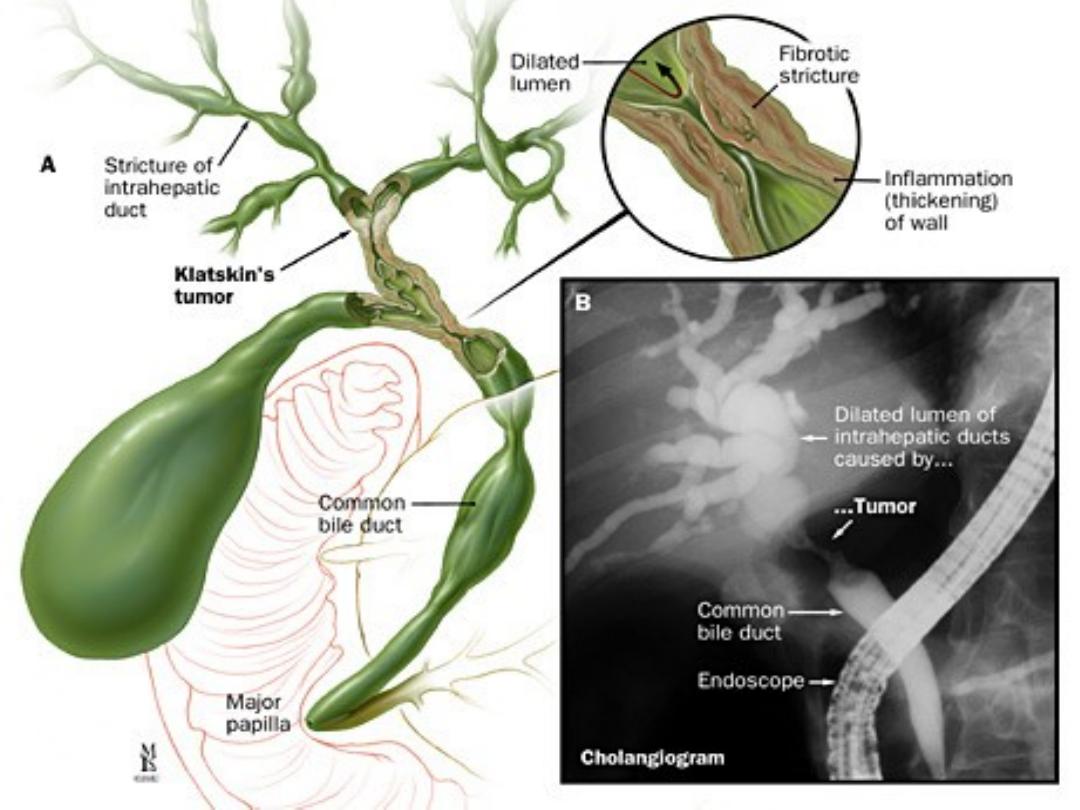
2- Extrahepatic;
Choledocholithiasis
Carcinoma
Ampullary
Pancreatic
Bile duct
(cholangiocarcino
ma)
Secondary
Parasitic
infection
Traumatic biliary
strictures
CLINICAL FEATURES IN CHOLESTATIC JAUNDICE
A- Cholestasis;
1- Early features
• Jaundice
• Dark urine
• Pale stools
• Pruritus
2- Late features
• Xanthelasma and
xanthomas
• Malabsorption
–
Weight loss
–
Steatorrhoea
–
Osteomalacia
–
Bleeding
tendency
B-
Cholangitis;
Charcot's
triad
1. Fever
2. Rigors
3. Right
upper
quadrant
abdomin
al pain.



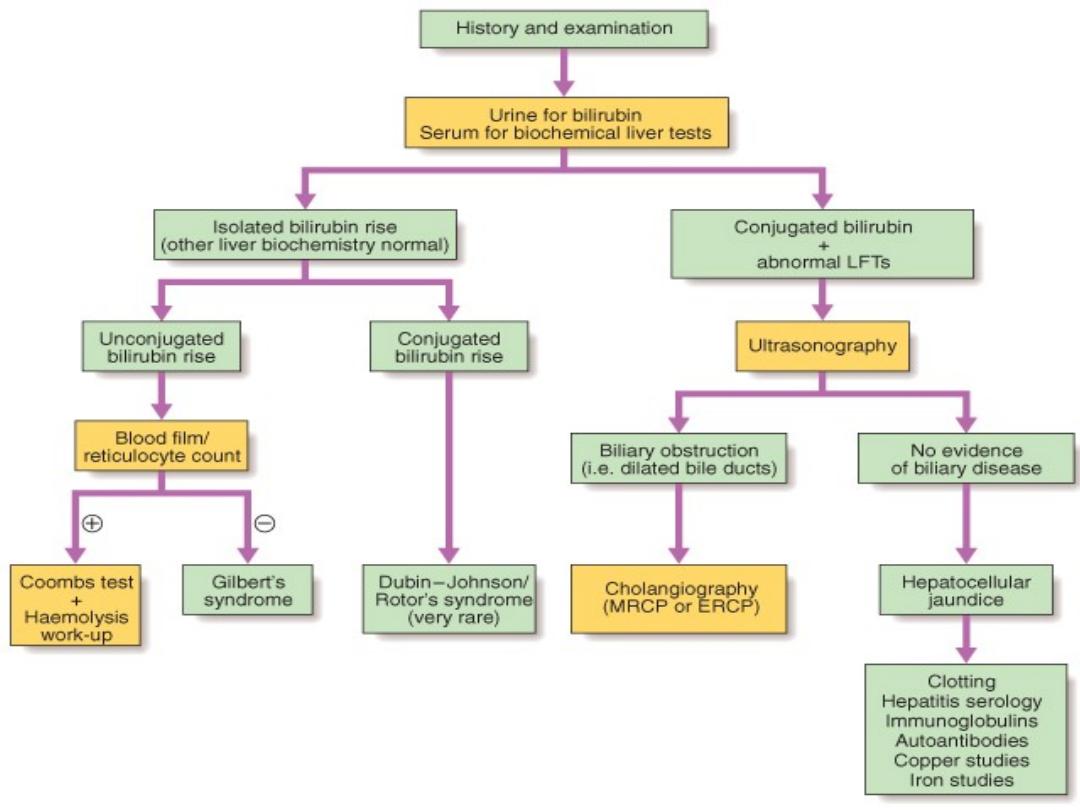
Investigation
of jaundice
'Hepatitic' and
'cholestatic'/'obstructive' LFTs
Pattern
AST/AL
T
GGT
ALP
Biliary
obstruction
↑
↑↑
↑↑↑
Hepatitis
↑↑↑
↑
↑
↑
mild elevation (< twice normal);
↑↑
moderate elevation (2-5 times normal);
↑↑↑
marked elevation (> 5 times normal).

Thanks
