Cleft lip and palate
Cleft lip and palate
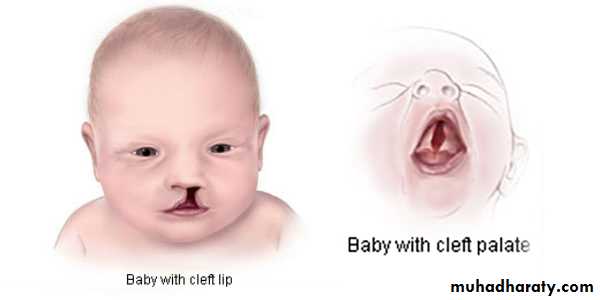
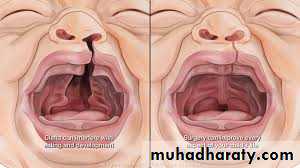
Orofacial clefts include a range of congenital deformities most commonlypresenting as cleft lip with or without cleft palate or isolated cleft palate.
Cleft lip and palate (CLP) is a three-dimensional deformity involving soft and hard tissue that changes with growth and function
Epidemiology
The estimated incidence of CLP ranges from 1:500 live births to 1: 2000 live births, the incidence is highest in Asians (1:500) followed by whites(1:1000) while the lowest incidence is in African-Americans (1:2000), but this racial variation is not observed in cases of isolated cleft palate (CP) with reported incidence of 1:2000 live births.• Isolated cleft lip (CL) is reported in 21%-25% of the cases.
• Isolated CP is reported in 33%-40% of the cases.
• CLP is reported in 35%-46%.
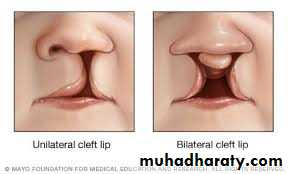
• Unilateral clefts are 9 times more common than bilateral clefts andthey are more frequent on the left side than on the right.
• Males are predominant in CLP population, whereas isolated CP occurs more commonly in females.
• CLP can be associated with syndromes such as Van der Woudesyndrome, hemifacial microsomia , velocardiofacial syndrome orDiGeorge syndrome, ectrodactyly-ectodermal dysplasia-cleftingsyndrome, Stickler syndrome, trisomy 13 and trisomy 18.
Etiology
Clefts can occur as part of a syndrome or as isolated clefts, and they are thought to be of a multifactorial etiology with a number of potential environmental and genetic contributing factors. Multiple genes have been implicated in the etiology of cleft, in addition to disturbances in growth factors or their receptors.The environmental factors during pregnancy that have been established in the etiology of CLP include; smoking, alcohol, anticonvulsants, steroids, folic acid deficiency, hypoxia, retinoid, radiation, viral infections in addition to mechanical factors.
Classification
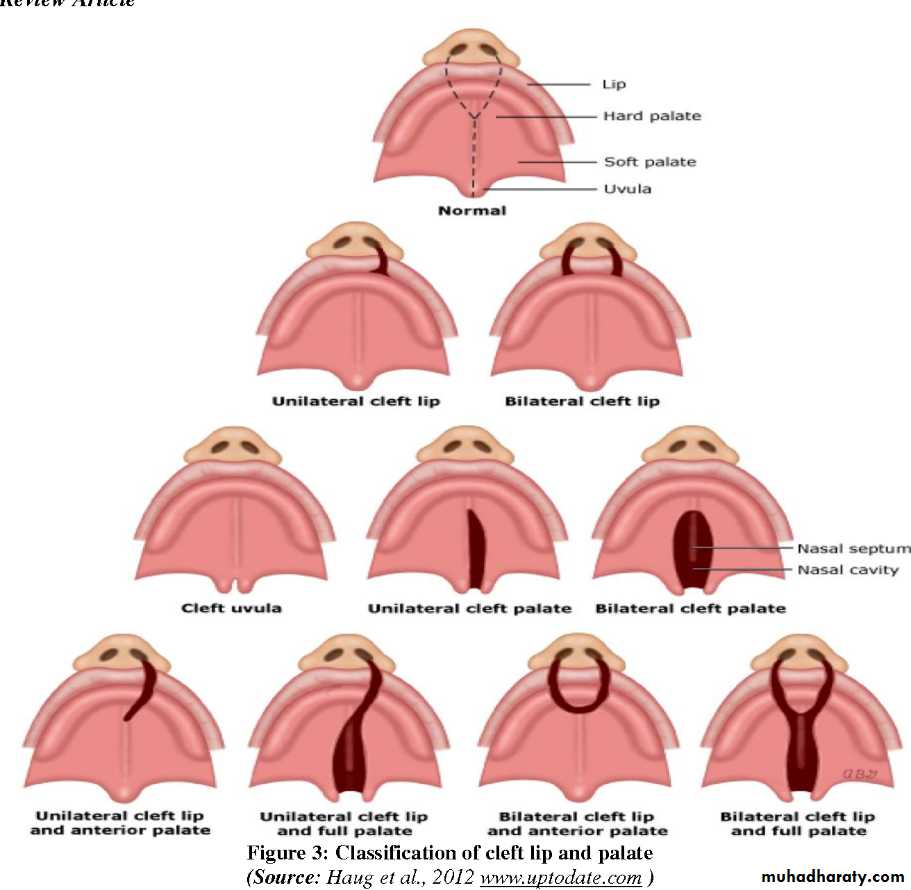
Many classification systems were proposed for CLP starting in 1920s. Clefts need to be described rather than categorized and the description of CLP phenotypes should include:1. The laterality (unilateral/bilateral/median) and severity (complete/
incomplete) of the labial defect.
2. Acknowledgment of an alveolar defect.
3. Morphological characterization of the palatal defect;
• one of the most widely accepted classification of palatal defects is that of Victor Veau introduced in 1931
• Group 1: Cleft of soft palate only.
• Group 2: Cleft of hard and soft palate up to the incisive foramen, involving secondary palate alone.
• Group 3: Complete unilateral cleft, extending from uvula to theincisive foramen in midline, than deviating to one side and usuallyextending through the alveolus at the position of the future lateralincisor tooth.
Group 4: Complete bilateral cleft, same as group 3 with two cleftsextending forward from the incisive foramen through the alveolus
Prenatal diagnosis
Recent advances in ultrasound imaging have revolutionized prenataldiagnosis of facial clefts, ultrasound images of clefts of the lip can be
visualized as early as 12-16 weeks (67%-93% detection rate), whereas
diagnostic images of the palate are more difficult to acquire (7%-22%
detection rate).
Genetic counseling should be offered to parents especially in syndromiccases. The risk of having a second child with CLP is 2-4%, thispercentage increases to about 10% when 2 previous children had CLP.When one parent and one child had CLP the risk of having a second childwith CLP is 17%.
Clinical manifestationsCleft Lip may be microform, incomplete or complete (involving the full vertical height of the lip). Complete cleft lips are often associated with analveolar cleft.
In unilateral CL there is rotation and distortion of the vermillion of Cupid's bow and philtral landmarks on the cleft side.
In bilateral CL, the premaxilla grows independently of the maxillae on either side and may protrude considerably, particularly in complete clefts. The prolabium, consisting of soft tissues of the premaxilla without muscle fibers, also lacks Cupid's bow and philtral columns bilaterally.
The spectrum of CP ranges from a submucous cleft to complete clefting of the primary and secondary palate. CP is primarily characterized by disorientation of palatal muscles which lead to feeding difficulties, velopharyngeal insufficiency, and speech problems.
Management:
Successful management of the child born with CLP requires coordinated care provided by a number of different specialties including oral and maxillofacial surgery, plastic surgery, otolaryngology, genetics, speech therapy, orthodontics, prosthodontics and others.Specific goals of treatment include the following:
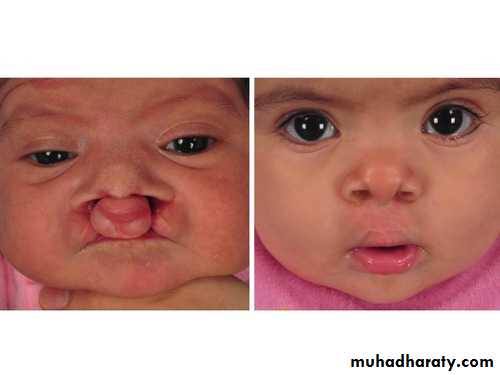
• Normalized esthetic appearance of the lip and nose
• Intact primary and secondary palate
• Normal speech, language, and hearing
• Nasal airway patency
• Class I occlusion with normal masticatory function
• Good dental and periodontal health
• Normal psychosocial development
The management of CLP patients can be divided into:
1. Preoperative management.2. Primary operative management.
3. Secondary operative management
Preoperative management
FeedingOne of the major concerns during this phase of management is feeding, this concerns not very critical in children born with isolated Cl, as they can feed quite well and even have the opportunity to breastfeed in most instances. Infants with cleft palate, on the other hand, can have difficulty in feeding due to the inability to form an adequate seal between the tongue and palate for creation of sufficient negative pressure to suck fluid from a bottle. Specialized nipples and bottles are necessary to improve feeding.
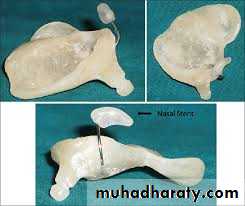
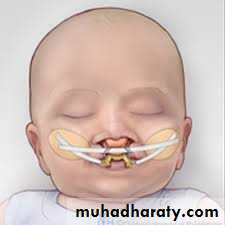
Presurgical orthopedics (PSO)
PSO entails using devices to mold the perioral structures of the infant with a CLP to reposition the nasolabial and axillary segments closer to each other. It is mainly used in the first few weeks after birth and in the months prior to palate repair.The main objectives of PSO are:
• Facilitating intra-oral feeding.• Improving maxillary growth.
• Improving the projection of the nasal tip.
• Reducing nasal deformity.
• Facilitating primary lip, nasal, and alveolar surgeries.
• Retracting and repositioning the premaxilla more posteriorly in patients with bilateral cleft.
PSO treatment can be achieved by intraoral or extraoral devices or appliances or a combination of the two, examples of PSO are:
Alveolar molding
Lip strap/lip taping
Nasoalveolar molding (NAM)
Primary operative management
Treatment planning and timingthe safest time period for Surgery in this population of infants could be outlined simply by using the child was at least 10 weeks old, 10 pounds in weight, and with a minimum hemoglobin value of 10 g/dl.
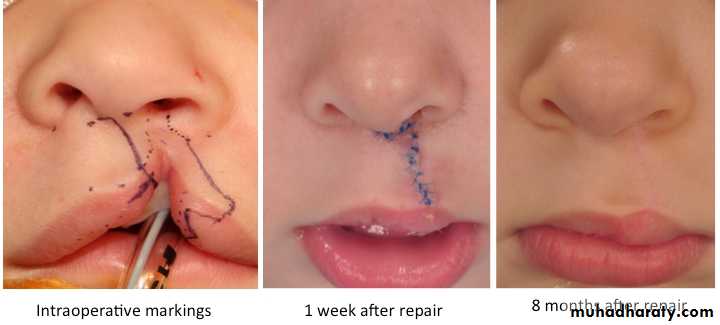
Surgical procedures for CL
The basic premise of the repair is to create a three-layered closure ofskin, muscle, and mucosa that approximates normal tissue and excises
hypoplastic tissue at the cleft margins.
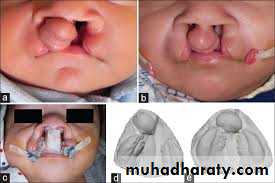
Lip adhesion
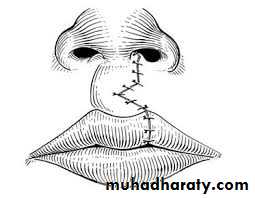
This procedure is carried out in an attempt to surgically approximate the segments of the cleft lip prior to definitive lip repair to achieve a better relationship of both the lip structures and the dental arches. It is usually used in wide bilateral clefts. It is usually completed at 3 months of age while definitive lip repair is 3-9 months later.Straight line repair
Straight line closure, or the Rose-Thompson closure may be indicated for microform clefts and it is rarely used as primary technique for cleft repair as it results in notching of the lip and vertical scar contracture.Tennison-Randall triangular flap repair
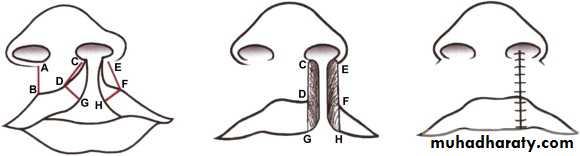
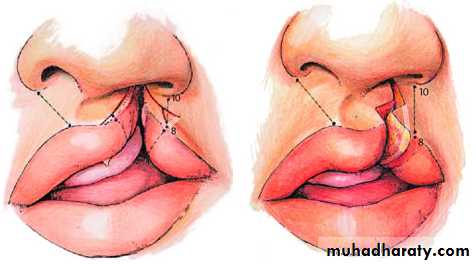
It utilizes the inter-digitation of triangular flaps (geometric design). The concept underlying the technique can be similarly compared to a Z- plasty reconstruction of the lip. This technique is based on careful measurements of specific landmarks.Millard's rotation-advancement flap repair
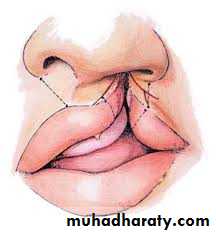
It is the most prevalently used technique in cleft lip repair. The technique utilizes downward rotation of the superiorly displaced medial lip segment with advancement of the lateral lip flap to correct the defect below the nose. Many modifications for the original procedure were described.Bilateral CL repair
Repair of the bilateral CL is often significantly more difficult than the unilateral CL repair due to the presence of the premaxilla and prolabium. The prolabium is oftentimes deficient in muscle and vermillion, is small, and attached to the nasal tip with little or no columella present. The commonly discussed treatment options include; cleft repair that may or may not include a primary rhinoplasty, and a lip adhesion with a delayed lip repair several months later. Infant orthopedics, nasoalveolar molding, and taping of the lip can be considered as an option with any of the techniques described earlier.Surgical procedures for CP
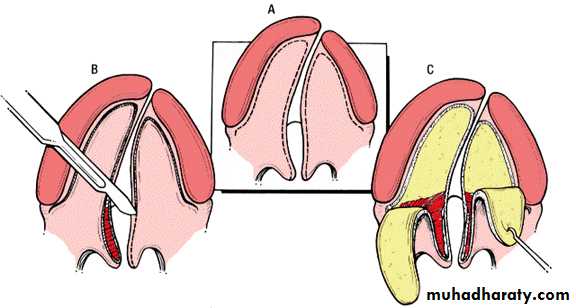
CP repair requires the mobilization of multilayered flaps to reconstructthe defect in a layered fashion by first closing the nasal mucosa and then the oral mucosa, the surgeon must also reconstruct the musculature of the velopharyngeal mechanism. Therefore, the soft palate is closed in three layers by approximating the nasal mucosa, velar musculature, and the oral mucosa.
The hard palate portion is closed in two layers using nasal mucosa flaps and then oral mucosa flaps. Both the hard and soft palate repairs must be done in a tension-free manner to avoid wound breakdown and fistula formation. Many techniques have been described in the literature with many variations, each method having its theoretical advantages and limitations:
The von Langenbeck technique:
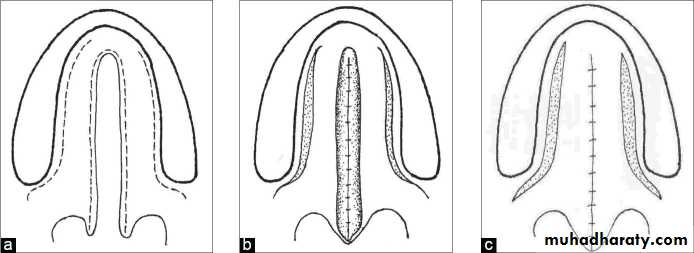
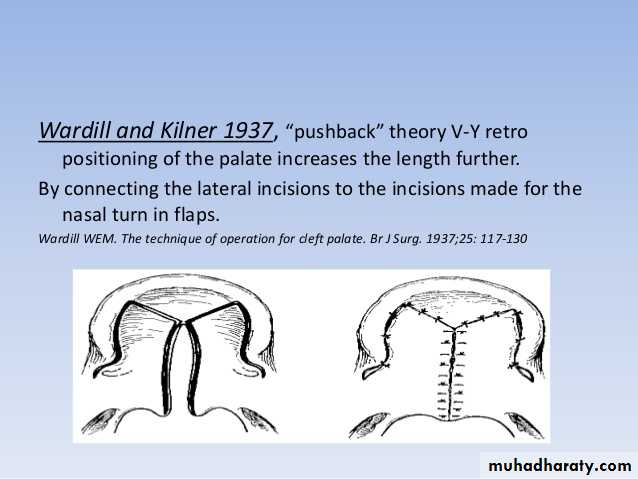
It involves creating bi-pedicled mucoperiosteal flaps on both sides of the cleft. The nasal side of the cleft is closed first, using redundant mucoperiosteum from the incision along the cleft edge. Then the bipedicled flaps are approximated to cover the oral surface of the cleft.V-Y pushback technique
Many authors believed that the von Langenbeck procedure resulted ininsufficient length of the soft palate and advocated the V-Y pushback technique. It has the advantage of lengthening the palate and repositioning the levator muscle in a more favorable position. This technique also has a higher rate of fistula in complete cleft palate.
Two-flap technique
In this procedure a full-thickness mucoperiosteal flap is elevated on each side of the cleft, which preserves the palatal neurovascular bundle.The Furlow technique
It essentially consists of repairing palatal clefts using Z-plasties of theoral and nasal mucosa. The theoretical advantage is that the soft palate may be lengthened while preventing longitudinal scar contracture and palatal shortening.
Postoperative care
Normal feeding can resume as soon as the infant is stable, with the exception that active sucking is to be avoided for at least 2 weeks.
Elbow immobilizers maybe used.
Regular follow-up.
Complications
Immediate postoperative complications include breakdown of the repair due to tension, palatal ischemia, secondary pressure, secondary trauma, or bleeding. It may result in the formation of an oro-nasal fistula which most commonly forms at the junction of the hard and soft palate, The risks of fistula development relate to the type of palate repair, surgical experience, cleft width, cleft type, and even age at closure. Other long-term complications include midface growth deficiency, velopharyngeal incompetence, recurrent fistula, and sleep apnea.Secondary operative management
Alveolar bone graftingGoals of alveolar bone reconstruction
1. To provide bone support and adequate attached gingival width for teeth adjacent to the cleft.
2. To close the remaining oro-nasal fistula.
3. To improve support of the nasal alar base and lip on the affected side(s).
4. To allow normal eruption of the permanent teeth in the cleft area and providing sufficient bone for the placement of dental implants, where needed.
5. To create an appropriate ridge form to allow for optimization of orthodontic care and dental alignment.
6. To allow for stabilization of the premaxillary segment and to provide continuity of the maxilla as a whole.
7. To improve nasal symmetry.
8. To provide support for the upper lip.
Timing of the alveolar bone reconstruction was one of the most controversial issues. Generally it can be grouped according to timing into:
Primary (early) grafting; which was defined as that performed simultaneously with lip repair, performed at younger than 2 years of age is considered primary grafting, or as grafting performed before the palate is repaired.
Secondary (delayed) grafting: which can also be divided into:
Early secondary: before the eruption of the permanent incisor teeth (3-6 years). The literature does not support early secondary grafting.Secondary (mixed dentition): before the eruption of the maxillary canine, (6-12 years), it can also be divided into early (6-8 years) and late secondary (8-12 years).
Ideally the patient is grafted between the ages of 8 and 12 years with a maxillary canine root that is one half to two thirds developed, some authors advocated the early secondary grafting (6-8 years) to preserve the lateral incisor especially if present in the posterior segment.
Late grafting: after 12 or 13 years of age, after the eruption of the permanent canine.
Common presenting problems• Discharge and smell from the nose.
• Oral food/fluids leaking from the nose.
• Poor speech.
• Inability to suck up a straw or low up balloons.
• Poor appearance of the incisor teeth.
• Missing or supernumerary teeth within the cleft area.
• Difficulty cleaning teeth in the cleft area.
• Poor facial appearance
Assessment of the patient
history and clinical examination
radiographic examination panoramic (OPG), occlusal and periapical films are essential for treatment planning. CBCT
Study models
Inter-occlusal acrylic wafer
Orthodontic treatment
Sources of bone graft materials
A variety of autologous, allogeneic, and xenogeneic bone materials;rhBMP; and growth factors have been used for correcting alveolar cleft. Of these, fresh autologous cancellous bone is the ideal bone graft source. Both cortical and cancellous bones can be used for a bone graft, but cancellous bone is known to be better because of the cell transfer and revacularization in osteo-induction and osteoconduction.
lliac crest, is the most commonly used bone in bone grafting because
it is easy to harvest, it can provide a large amount of cancellous bone, and cleft preparation can be performed at the same time. However, the disadvantages of using this bone are possible scar postoperative pain, delayed ambulation, and risk of cutaneous nerve injury- Cranium; it has little resorption, less postoperative pain, and the advantage of a concealed scar. However, a long operative time and serious side effects such as hematoma, seroma, dural tear, dural exposure, and cerebrospinal fluid leakage are possible.
Tibia it results in less bleeding, postoperative pain, operative time, and scarring, as well as faster ambulation and a shorter hospital stay. However, it yields relatively small amounts of bone in adult patients, and it may be necessary to obtain the product from both legs if a large amount is required. Moreover, in children there is possibility of growth disturbance due to injury of the epiphyseal cartilage.
- Mandibular symphysis; the mandible has the same embryonic origin as the maxilla which may contribute to low resorption, surgery is in the same operative field and postoperative discomfort is reduced. However, there is a risk of roots and mental nerve damage, and the amount that can be collected depends on the development of the mandible.
Bone graft substitutes; including demineralized freeze-dried bone (DFDB), freeze-dried bone (FDB), freeze-dried matrix (FDM) hydroxyapatite (HA) or tricalcium phosphate (TCP). Recently the addition of growth factors such as platelet-rich plasma (PRP) and platelet rich fibrin (PRF) with graft materials have used.
Postoperative care
Antibiotics usually start before the incision and continue postoperatively
for 7-10 days along with chlorhexidine mouth wash, excellent oral hygiene and good nutrition are encouraged, patients and parents are instructed to liquid and soft diet for 2-3 weeks and to avoid any trauma to the operative site.
Complications
- Wound dehiscence which is managed by debridement and antimicrobial mouth washes with or without systemic antibiotics.- Infection which is managed by conservative debridement, daily irrigation and packing with oral antibiotics.
- Persistent fistula which may require subsequent procedures.