1
Immunoblistering Skin Diseases
Dr. Ahmed Abdulhussein AL-Huchami
Bullous Skin Disorders (BSD)
INTRODUCTIONBSD are skin conditions characterised by blister formation.
A blister is an accumulation of fluid between cells of the epidermis or upper dermis.
Causes of blister could be genetic, physical, inflammatory, immunologic and as a reaction to drugs.
BSDs are mostly autoimmune .
Immunoblistering Skin Diseases
Group of disorders sharing two common features:
• Immunological [Autoimmune] Pathogenesis.
• The primary presenting lesion is a bulla or blister.
• Immunoblistering skin diseases include:
• Pemphigus group (P. vulgaris, P. vegetans, P. foliaceus, P. erythematosus and Paraneoplastic Pemphigus).
• Pemphigoid group (Bullous Pemphigoid, Bullous Pemphigoid of Pregnancy or also known as Herpes gestationis and Cicatricial Pemphigoid).
5
Classification of Immunoblistering Diseases
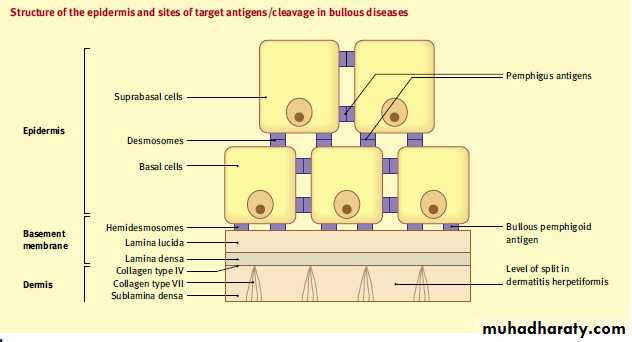
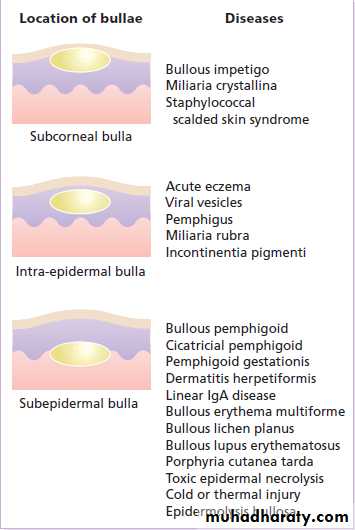
6The bullae result from skin cleavage (splitting) that can occur at any level within the skin with subsequent accumulation of fluid. According to the level of skin cleavage, immunoblistering diseases are classified into:
• Epidermal blistering disorders e.g. Pemphigus group of disorders.
• Dermal blistering disorders in which splitting occurs within or beneath the basement membrane e.g. Pemphigoid group of disorders, DH, Linear IgA disease and CBBDC (Linear IgA disease of Children).
A, these lesions.
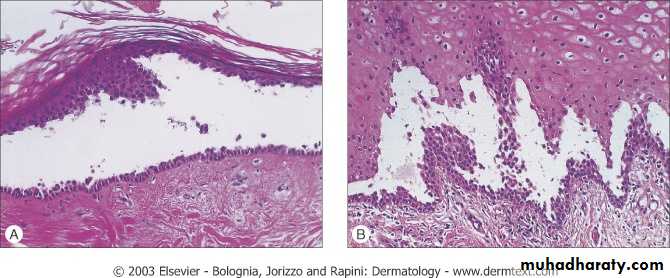
Levels of blister formationA, Subcorneal (as in pemphigus foliaceus).
B, Suprabasal (as in pemphigus vulgaris).C, Subepidermal (as in bullous pemphigoid & dermatitis herpetiformis).
Assessment of the levels of epidermal separation forms the basis of the initial differential diagnosis of these lesions.
Pemphigus داء الفقــــــاع
An autoimmune intraepidermal blistering disease.Relatively uncommon disease.
Often severe and can be life-threatening.
It presents as flaccid bullae and painful erosions.
According to the level of splitting within the epidermis Pemphigus can be divided into:
• Superficial types: characterized by subcorneal cleavage e.g. P. foliaceus and its variant P. erythematosus.
• Deep type: characterized by suprabasal cleavage e.g. P. vulgaris and its variant P. vegetans.
• A rare variant of Pemphigus which is usually associated with an underlying malignancy (Thymoma or Carcinoma) is called Paraneoplastic Pemphigus.
9
A, Subcorneal (as in pemphigus foliaceus).
.Levels of blister formation
Pathogenesis
Circulating Antidesmosomal IgG autoantibodies + desmosomesAg-Ab complexes Keratinocytes
Plasminogen activatorPlasminogen Plasmin (Proteolytic enzyme)
Acantholysis
Bullae
11
Stimulate
Pemphigus vulgaris داء الفقاع الخبيث
Clinical PictureUsually affects middle age group [40-60 years].
Both sexes are equally affected.
Incidence is higher among Jews.
Presentation
Flaccid bullae that easily and rapidly rupture leaving oozy painful erosions and later crusted lesions (bullae may not be seen at presentation because of their flaccid and fragile nature). The bullae are not hemorrhagic.
The rash is not pruritic and there is no grouping of lesions.
Nikolsky’s sign and Bulla spread sign are positive.
12
+ ve Nikolski’s Sign
Nikolsky Sign : Dislodging of epidermis by lateral finger pressure in the vicinity of lesions, which leads to an erosion.
Shearing stresses on normal skin can cause new erosions to form
Pemphigus vulgaris داء الفقاع الخبيث
P. vulgaris usually has generalized distribution, however the predilection sites are the scalp, trunk, itertriginous areas (axillae and groins).
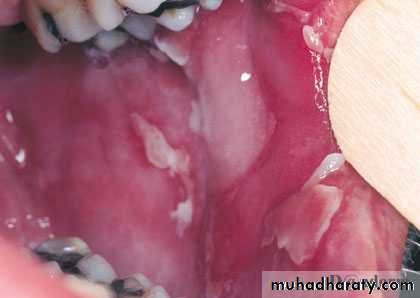
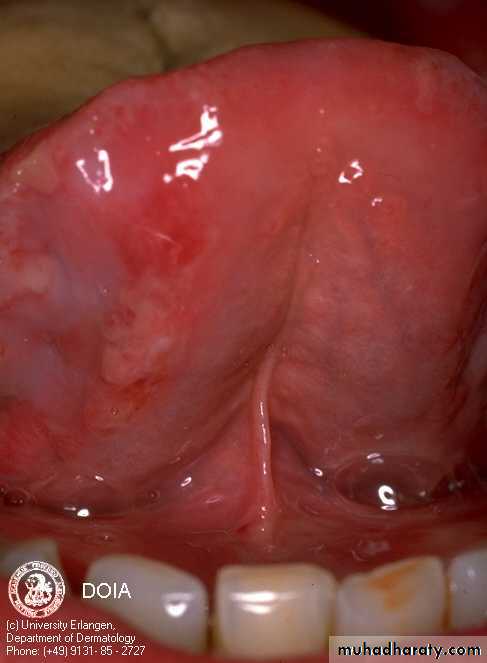
Mucous membranes of the mouth, pharynx and larynx may be involved and cause painful oral erosions, dysphagia and hoarseness of the voice respectively. Oral lesions (Painful erosions and ulcerations) are the presenting feature in about 50% of the patient and oral involvement occurs in almost all patients during the whole course of the disease.
The course of the disease is usually chronic with a high mortality rate (100% before steroid era and about 10-30% after corticosteroid introduction), however with careful management many patients can live relatively normal life with occasional exacerbations.
14
P. Vulgaris involving the trunk with painful erosions
15
Bullae are flaccid and fragile in P. vulgaris, they rupture easily and rapidly leaving painful erosions and later crustations.
16
Pemphigus vulgaris: Bullae are transient in this disorder; erosion is more characteristic.
17
18
Upper lip
Lower lipInner Cheek
Tongue
PV of the oral mucous membranes
Pemphigus vulgaris
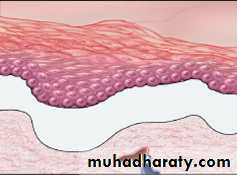
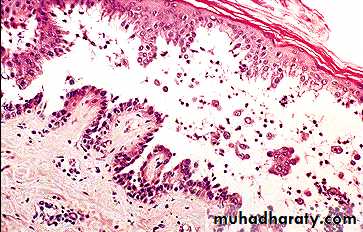
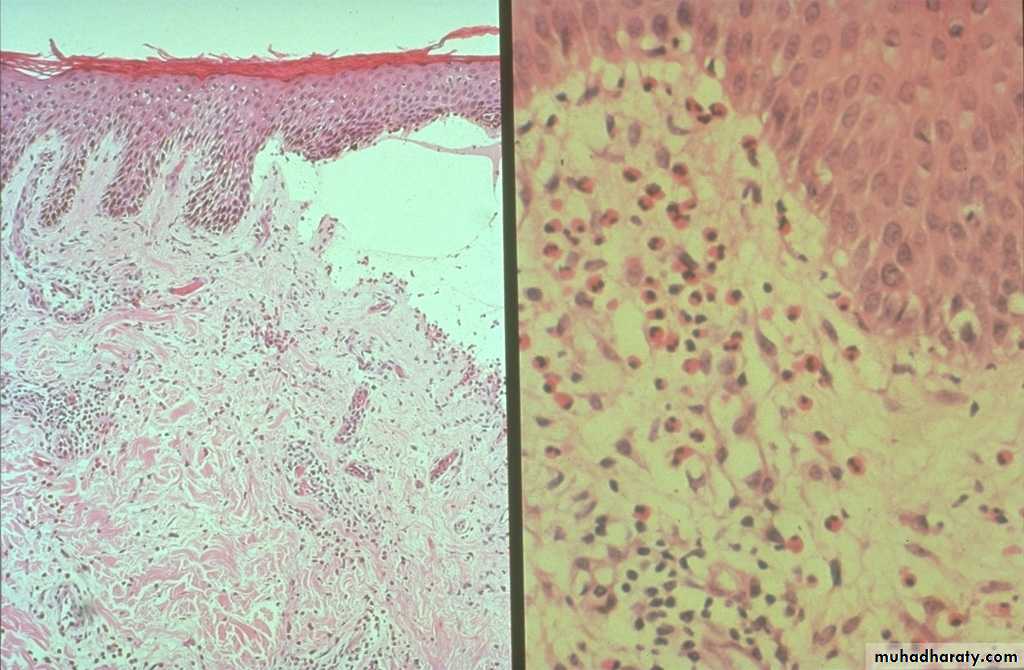
Suprabasal acantholysis results in an intraepidermal blister containing rounded keratinocytes that are separating from their neighbors. Initially, a single row of basal cells is present on the floor of the blister with dermal papillomatosis (tombstone effect). Follicular involvement by acantholysis is also common.
Binding of Abs to the adhesion molecules loss of cell-cell adhesion acantholysis
Pemphigus vulgaris داء الفقاع الخبيث
Complications of P. vulgaris• Infections such as septicemia, chest infection… etc.
• Fluid and electrolyte loss due to widespread denudation of the skin and mucous membranes.
• Side effects of treatment with corticosteroids and other immunosuppressive agents.
21
These side effects are inevitable and now considered as the leading cause of death in patients with P. vulgaris.
Investigations
• Tzanck Smear: Scrape the floor of an intact blister and stain with Giemsa stain, it shows large rounded acantholytic keratinocytes with hyperchromatic nuclei.• Skin Biopsy
3. Immunoflourescence studies: is used to detect tissue-fixed antibodies (local antibodies) and circulating antibodies (serum antibodies) through:
• Direct Immunoflourescence technique (DIF)
• Indirect Immunoflourescence technique (IIF)
22
Investigations
Skin Biopsy
Take an intact early blister from the skin or oral mm and stain it with H-E stain.
Suprabasal acantholysis and intraepidermal bullae containing large round acantholytic cells and some polymorphs & eosinophils
23
P. foliaceus: Subcorneal Acantholysis
P. vulgaris: Suprabasilar Acantholysis
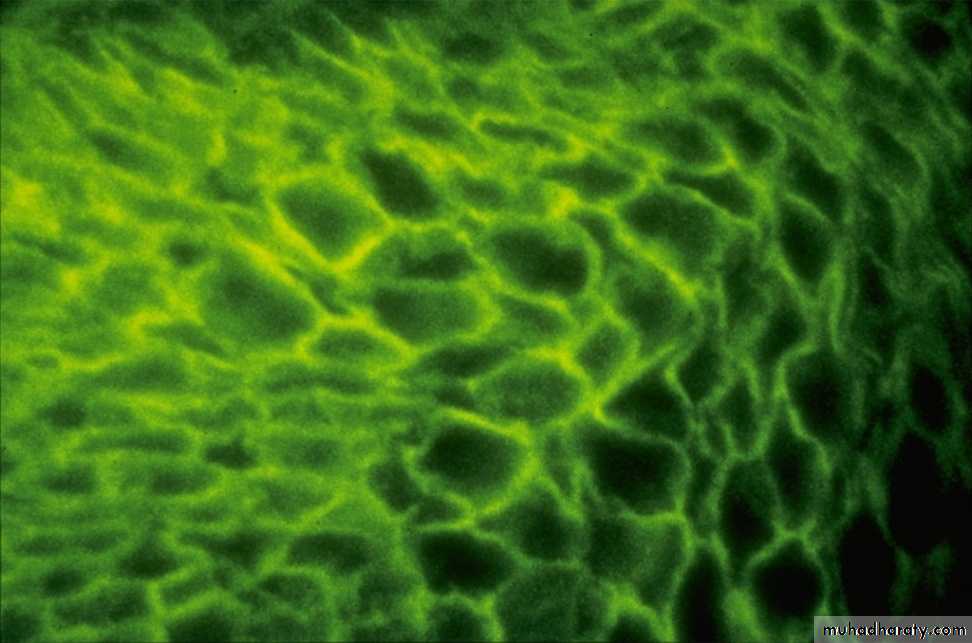
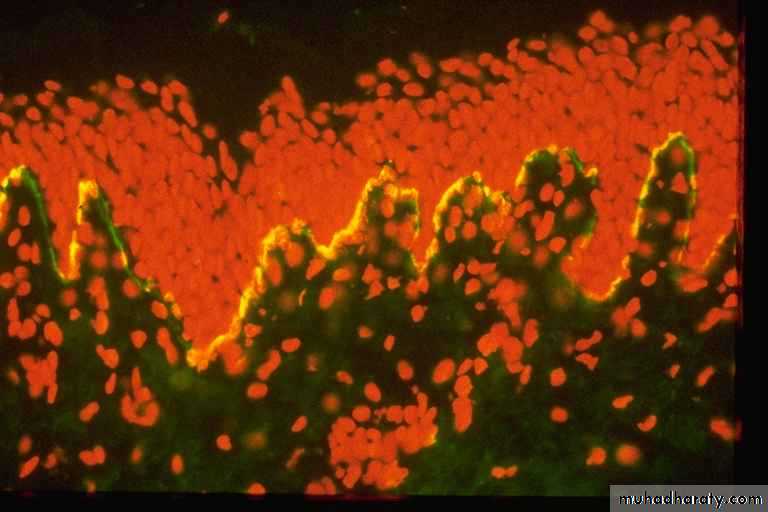
Investigations• DIF Technique:
• A peri-lesional skin from the patient is stained with a fluorescen-labeled Anti-IgG and Anti-C3 Abs to detect tissue fixed autoantibodies. It shows IgG and C3 deposition in epidermal intercellular spaces around the keratinocytes i.e. Desmosomal Antibodies.
24
Investigations
• Indirect Immunoflourescence Technique:
• IgG anti-Desmosomal Abs can be detected in the serum of about 90% of patients with P. vulgaris.
• Technique: Incubate Patient’s serum with monkey’s esophageal mucosa and then stain it with a fluorescen-labeled Anti-IgG. Positive test shows IgG deposition in epidermal intercellular spaces around the keratinocytes i.e. Desmosomal Antibodies. This technique:
• Is useful in detecting circulating autoantibodies.
• Can be used to measure disease activity in P. vulgaris (through measuring Ab titer by serial dilution of the patient serum). It is useful in the follow-up of patient on corticosteroid therapy as the Ab titer correlates with the disease activity in patients with P. vulgaris.
25
Management of P. vulgaris
• Admission to the hospital.• Give supportive therapy (iv fluids, antibiotics) if needed.
• Start Immunosuppressive therapy:
• Corticosteroids:
• Considered as the first line treatment unless there is a contraindication.
• Start with 80-120 mg Prednisolone per day in divided doses (higher doses may be needed in more severe cases).
• Start to taper the dose gradually over weeks when the disease is controlled (Control is reached when no new lesions appear and disappearance of old lesions) until reaching a minimal possible maintenance dose (Usually in the range of 5-15 mg per day).
26
Management of P. vulgaris
B. Cytotoxics: Used as Steroid-sparing Agents (Used in combination with steroid to decrease the dose of steroid) or as Steroid alternatives in cases of corticosteroid contraindications. These agents act through suppressing immunity and hence decrease autoantibody production. Examples of these agents:Azothioprine (Immuran®): 150 mg per day
Cyclophosphamide (Cytoxan®): 2 mg per Kg per day
Cyclosporine
Mycophenolate moefetil
C. Gold: Gold therapy (oral or parenteral “im”) may be useful in some cases of P. vulgaris.
D. Plasmapheresis: Rarely used, however it may be reserved for very severe and refractory cases.
27
TREATMENT
Systemic steroid ;
2 to 3 mg/kg of prednisolone until cessation of new blister formation and disappearance of Nikolsky sign.
Concomitant Immunosuppressive Therapy(steroid sparing agents)
such as Azathioprine , 2–3 mg/kg
Methotrexate , either orally or IM at doses of 25 to 35 mg/week.
cyclophosphamide or mycophenylate mofetil
High-dose intravenous immunoglobulin (HIVIg) ;
(2 g/kg every 3–4 weeks) may help gain quick control whilst waiting for other drugs to work.Rituximab ( Anti-CD20 monoclonal antibody) has been reported to help multidrug resistance, IV , once a week for 4 weeks.
Rx is usually prolong and need regular follow up
Dosage should be dropped only when new blisters stop appearingBullous Pemphigoid شبيه داء الفقاع
Clinical PictureBP is an autoimmune subepidermal blistering disease.
More prevalent in western countries (BP>PV), whereas the reverse occurs in Iraqi people (PV>BP).
Usually affects old people (60-80 years).
Both sexes are equally affected.
BP is often pruritic.
Characterized by tense bullae that may arise from normal-appearing skin or from an urticarial or eczematous areas.
The bullae are tense (not flaccid because they are subepidermal and covered with an intact epidermis).
29
Bullous Pemphigoid
The bullae may be hemorrhagic and may rupture leaving erosions and crustations.The lesions usually heal without scar formation.
Nikolsky's sign is negative.
Predilection areas:
1. Extremities (esp. inner thighs and flexor aspects of upper arms).
2. Trunk (especially axillae, groins & lower abdomen).
Mucous membrane involvement is occasional (20-30%) and is rarely being the initial presenting feature of BP.
30
Bullous Pemphigoid Tense bullae and hemorrhagic scabs
31
Thigh
Bullous Pemphigoid
32
BP mimicking Pompholyx
Tense bullaBullous Pemphigoid
33
Bullous Pemphigoid
34Tense bullae
Bullous pemphigoid
A, these lesions.
Levels of blister formation, Subepidermal (as in bullous pemphigoid
Pathogenesis of BP
IgG autoantibodies Complement systemBP Ag (in LL of BMZ) Chemotactic factors
Ag-Ab complex Proteolytic enzymesSubepidermal bullae Separation of LL
37Binds
Activates
Produces+
Investigations
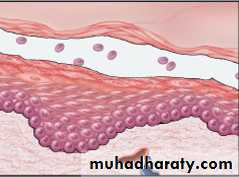
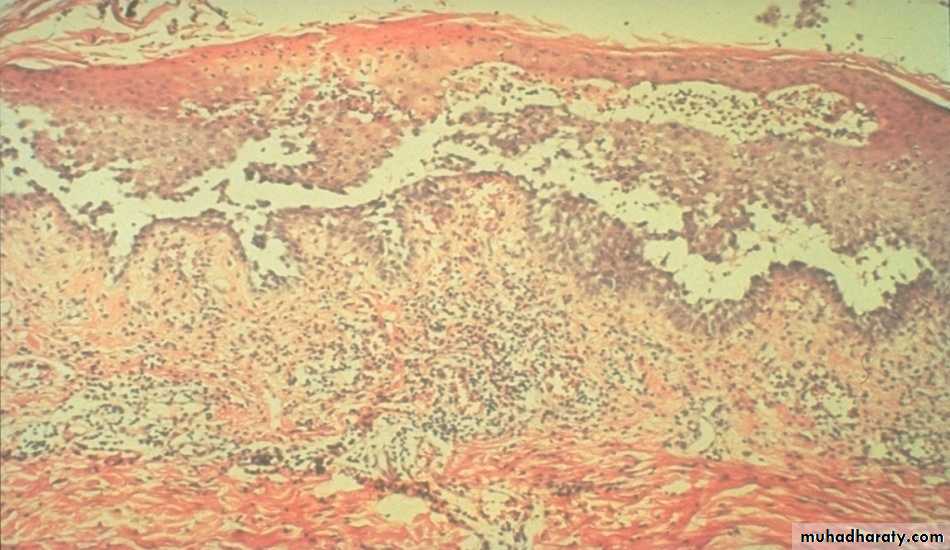
• Skin Biopsy: shows subepidermal unilocular bullae, often filled with eosinophils and some neutrophils.38
Subepidermal bulla
EosinophilsInvestigations
2. Immunoflourescent Studies• DIF: Shows linear IgG and C3 deposition along the Basement Membrane Zone.
• IIF: Circulating IgG antibodies can be detected in about 70% of patients. The titer of antibodies dose not correlate with the disease activity i.e. it is not useful in the follow up of the patients.
39
DIF
DIF
DIF: Linear IgG deposits in the BMZ in BP
40
Treatment of BP
Treatment• Prednisolone: start with 40-60 mg per day and after control state taper the dose to the minimum possible maintenance dose or even in some cases treatment may stopped.
• Dapsone: 2 mg per kg per day may be useful in some cases.
Course of BP is often self-limiting and treatment can often be stopped after one or few years of treatment.
Remission of BP may be spontaneous or treatment-induced.
Complications of BP are similar but milder and to lesser extent than those of PV (less mortality rate).
41
DIFF BTW PEMPHIGUS AND PEMPHIGOID
Pemphigus• Usually affects the middle age
• Acute and non itchy
• Seen on the trunk, flexures and scalp
• Mouth Blister is common
• Nature of blister is superficial and flaccid
Circulating Ab is IgG to intracellular adhesion proteins
Serum Ab Titer correlate with clinical disease activity.
Acantholysis
Nikolsky sign is positive
Pemphigoid
• Elderly patients
• Chronic and itchy
• Usually flexural
• Mouth Blister is Rare
• Blister is tense and bloody
IgG to BM region
Serum Ab Titer does not correlate with clinical disease activity.
No acantholysis
Nikolsky sign is negative
43